Current Perspective of Metaverse Application in Medical Education, Research and Patient Care
Abstract
:1. Introduction
Metaverse
2. Significance of the Metaverse in Healthcare Systems
2.1. Applications in Education for Healthcare
2.2. Applications in Research
2.3. Applications in Patient Care
3. Limitations and Challenges
4. Future Direction and Recommendation
5. Summary
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Types | Pros | Cons |
|---|---|---|
| Virtual reality (VR) therapy [44] VR can be used as a therapeutic tool to help patients with a range of conditions, including anxiety, phobias, post-traumatic stress disorder (PTSD), and pain management. | i. Controlled Environment: VR allows therapists to create a controlled and safe environment in which patients can confront their fears and anxieties. ii. Customizable: VR experiences can be customized to suit individual needs, making the therapy more effective. iii. Being Immersed: VR creates an immersive experience that can be more effective than traditional therapy methods in treating conditions such as phobias and PTSD. iv. Accessibility: VR therapy is more accessible to patients who may not be able to participate in traditional exposure therapy due to physical limitations or fears of leaving the house. | i. Cost: VR equipment can be expensive, making it less accessible to some patients. ii. Limited Research: The use of VR for treating anxiety, phobias, and PTSD is still in the early stages of development and there is limited research on its long-term effects. iii. Unrealistic: Some patients may not respond well to VR therapy because they perceive the experience as unrealistic or too artificial. |
| Virtual consultations [35] The metaverse can be used to facilitate virtual consultations between patients and healthcare providers, allowing patients to access care from anywhere. This can be particularly useful for patients in remote or underserved areas, or for those who have mobility issues. | i. Accessibility: Virtual consultations can increase access to healthcare for patients who may have difficulty traveling to see a healthcare provider in person, such as those with mobility issues or who live in rural areas. ii. Convenience: Virtual consultations can be more convenient for both patients and healthcare providers as they can be done from the comfort of one’s own home or office. iii. Timesaving: Virtual consultations can save time compared to traditional in-person consultations as they eliminate the need for traveling. iv. Reduced costs: Virtual consultations can potentially reduce costs associated with travel and parking. | i. Technical issues: Virtual consultations can be disrupted by technical issues such as poor internet connectivity or equipment malfunctions. ii. Reduced personal interaction: Virtual consultations may lack the personal interaction and human touch that can be important in building a therapeutic relationship between a healthcare provider and patient. iii. Limited examination: Virtual consultations may limit the examination that can be performed compared to an in-person consultation, as the healthcare provider may not be able to physically touch or observe the patient. iv. Data security: Virtual consultations may raise concerns about the security of personal and medical information, as it is transmitted electronically. |
| Telerehabilitation [46] The metaverse can be used to deliver rehabilitation services to patients remotely, enabling them to complete therapy exercises at home or in other locations. | i. Increased access to rehabilitation services: Telerehabilitation with the metaverse can increase access to rehabilitation services for patients who may not have access to traditional rehabilitation facilities due to geographic or mobility limitations. ii. Improved outcomes: The systematic review by de Araújo et al. found that VR rehabilitation was effective in improving outcomes such as motor function, balance, and activities of daily living in individuals with spinal cord injuries. iii. Customized and immersive rehabilitation experience: The metaverse allows healthcare providers to create customized virtual environments that simulate real-world scenarios, providing a more engaging and motivating rehabilitation experience for patients. iv. Increased safety: VR rehabilitation provides a controlled and safe setting for patients to practice and improve their skills, minimizing the risk of further injury. | i. Access to technology: Not all patients may have access to the necessary technology and equipment for telerehabilitation with the metaverse, such as VR headsets. ii. Cost: The cost of technology and equipment for telerehabilitation with the metaverse can be a barrier for some patients and healthcare providers. iii. Technical difficulties: Technical difficulties or malfunctions of the equipment can disrupt the rehabilitation experience and may require additional support. iv. Limited ability to assess physical performance: The virtual environment may not fully replicate real-world scenarios, making it difficult for healthcare providers to accurately assess physical performance. |
| Telemedicine [35] The metaverse could be used to provide remote medical consultations, allowing patients to see a doctor or specialist in a virtual environment. This could be especially useful for people living in remote or underserved areas. | i. Convenient for patients: Telemedicine enables patients to access healthcare services from the comfort of their homes, saving them time and effort in traveling to see a doctor. ii. Improved access to care: Telemedicine can provide healthcare services to patients in remote and underserved areas, improving access to care. iii. Increased efficiency: Telemedicine can reduce wait times for appointments and improve the efficiency of the healthcare system. iv. Cost-effective: Telemedicine can be a more cost-effective solution compared to traditional in-person visits. v. Better continuity of care: Telemedicine can improve the continuity of care for patients, as they can easily communicate with their healthcare provider between appointments. | i. Technical challenges: Telemedicine can be limited by technology and may require patients to have access to reliable internet, a computer or smartphone, and other necessary equipment. ii. Quality of care concerns: The quality of care provided through telemedicine may not be as high as in-person visits, as certain physical exams and procedures cannot be performed remotely. iii. Limited patient-provider interaction: Telemedicine may not provide the same level of patient–provider interaction as in-person visits, as patients may feel less connected to their healthcare provider. iv. Privacy and security risks: Telemedicine can also pose privacy and security risks, as personal health information may be vulnerable to hacking and cyberattacks. v. Reimbursement issues: Telemedicine may also face reimbursement issues, as insurance companies may not cover all telemedicine services. |
| Patient education [47] The metaverse can be used to provide interactive, immersive patient education experiences, which can be more engaging and effective than traditional methods. | i. Improving rehabilitation outcomes: The study focuses on the use of VR as a rehabilitation tool after knee surgery. By incorporating VR exercises into the rehabilitation process, patients can improve their physical performance, balance, and gait, resulting in a faster recovery and better outcomes. ii. Increased patient satisfaction: Patients in the study reported a high level of satisfaction with VR-based rehabilitation compared to traditional physical therapy. iii. Personalized rehabilitation: The study found that the level of difficulty of the VR exercises had a significant impact on patient outcomes. By tailoring the exercises to the patient’s specific abilities and progress, the rehabilitation program can be personalized to meet each patient’s unique needs. | i. Potential for technological limitations: The use of VR technology for rehabilitation may be limited by the availability and accessibility of the equipment, as well as the technical skills required to operate it. Patients may also experience discomfort or motion sickness while using VR, which could limit the feasibility of this approach for some patients. |
| Social support [44] The metaverse can be used to connect patients with similar conditions and provide a sense of community and social support. | i. Greater control: Virtual reality exposure therapy (VRET) provides the therapist with greater control over the patient’s exposure to anxiety-provoking stimuli, allowing them to carefully tailor the treatment to the patient’s specific needs and progress at a pace that they can handle. ii. Increased engagement and motivation: VRET provides a highly immersive and engaging experience, which can increase patient motivation to participate in therapy and adhere to treatment plans. iii. Safe and controlled environment: VRET allows patients to confront anxiety-provoking stimuli in a safe and controlled environment, without the risks associated with exposure in real-life situations. iv. Efficacy: VRET has been found to be effective in reducing symptoms of anxiety disorders, with some studies reporting results that are comparable to traditional in vivo exposure therapy. | i. Limited generalizability: VRET may not always generalize to real-life situations, as the stimuli presented in VR may differ from those encountered in the real world. This can limit the effectiveness of the therapy in some cases. ii. Technical limitations: The quality of the VR experience can be impacted by technical limitations, such as the quality of the graphics or the performance of the hardware. This can potentially detract from the effectiveness of the therapy. iii. Cost: VRET can be expensive to implement, as it requires specialized equipment and software. This can limit its accessibility to some patients who may not have access to the necessary resources. |
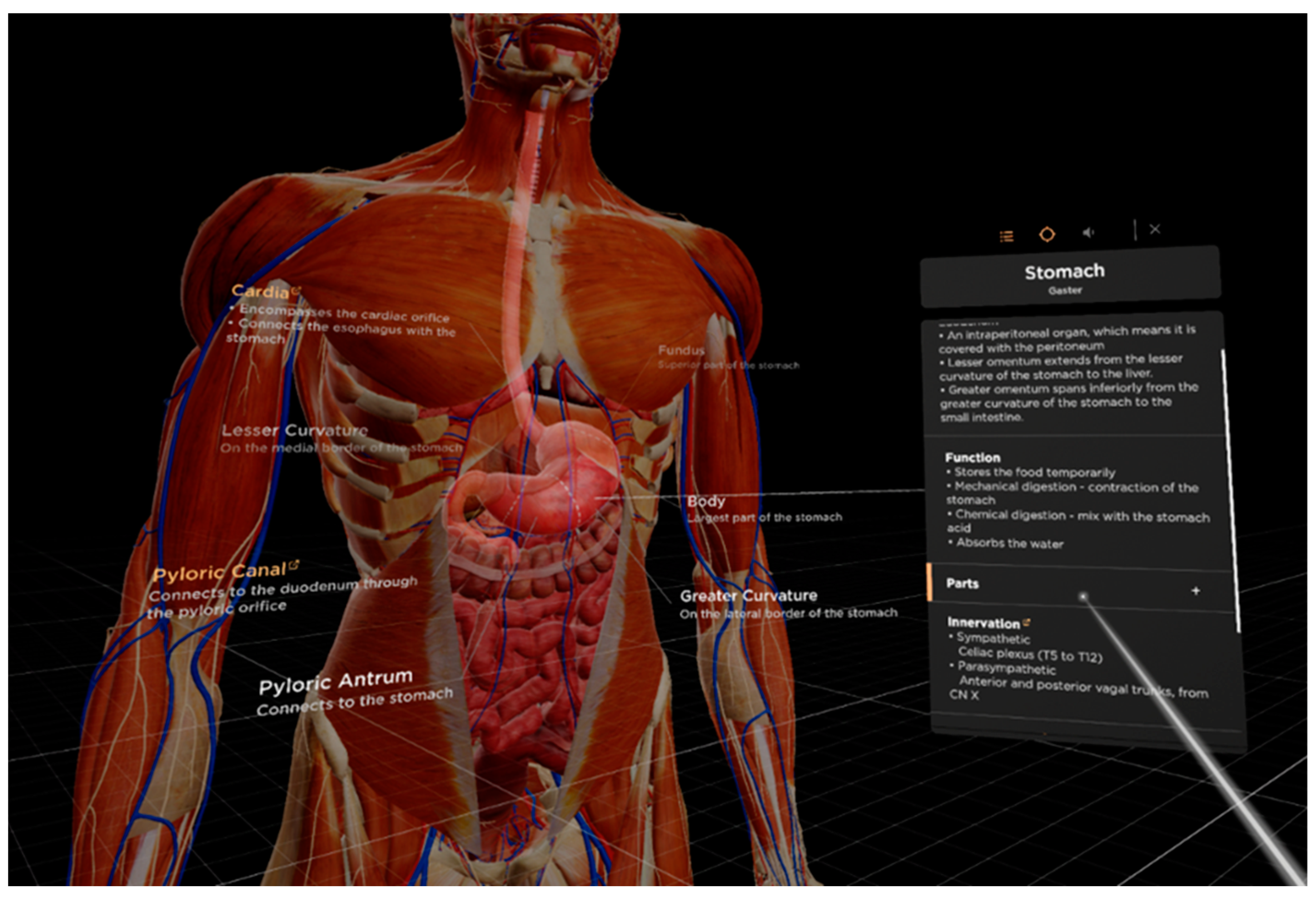
| Medical Visualization [39] The metaverse could be used to create interactive 3D visualizations of medical data, such as CT scans, MRI images, and microscopic samples. This could make it easier for doctors and researchers to understand and analyze medical data and could also be used to create VR experiences that help patients understand their diagnosis and treatment. | i. Improved understanding of medical data: By creating interactive 3D visualizations of medical data, doctors and researchers can better understand and analyze complex medical data. This can lead to more accurate diagnoses and better treatment decisions. ii. Enhanced patient education: Using VR experiences, patients can better understand their diagnosis and treatment, which can improve their engagement in the treatment process and their overall outcomes. iii. Greater efficiency: Medical visualization can help doctors and researchers process complex medical data more efficiently, leading to faster diagnoses and treatment decisions. iv. Reduced risk: Using VR to visualize medical data can reduce the need for invasive procedures or surgeries, which can reduce the risk of complications and speed up recovery times. | i. Cost: Developing high-quality, interactive VR visualizations can be expensive, which may limit their availability to certain institutions or patients. ii. Technical challenges: Creating 3D visualizations of medical data requires specialized technical expertise and resources, which may be a barrier to adoption. iii. Limited accessibility: VR technology may not be accessible to all patients, particularly those with certain disabilities or conditions that make it difficult to use. iv. Ethical concerns: There may be ethical concerns around the use of VR to visualize sensitive medical data, particularly if there are privacy or confidentiality risks. |
| Mental Health treatment [44] This could be used for providing virtual therapy sessions, creating virtual support groups, and providing VR exposure therapy for people suffering from anxiety and post-traumatic stress disorder (PTSD). | i. Increased access to care: Virtual therapy sessions and virtual support groups can be more accessible and convenient for people who may have difficulty accessing in-person mental health services due to geographical, financial, or other barriers. ii. Greater anonymity: Virtual therapy and support groups can provide a greater sense of anonymity and privacy, which may make it easier for people to share about their mental health struggles. iii. More engaging and immersive therapy: VR exposure therapy can create a more immersive and realistic experience for people receiving treatment for anxiety and PTSD, which may lead to more effective therapy outcomes. iv. Customizable experiences: Virtual technology can be used to create personalized and customizable therapy experiences, such as virtual environments that are tailored to a person’s specific fears or triggers. | i. Technical issues: Virtual technology may be subject to technical issues that could disrupt therapy sessions, such as internet connectivity problems, hardware failures, or software glitches. ii. Lack of personal connection: Virtual therapy and support groups may lack the personal connection and face-to-face interactions that some people may prefer in traditional therapy settings. iii. Potential for distractions: Virtual therapy sessions may be more susceptible to distractions from the person’s environment, such as notifications from their phone or other digital devices. iv. Ethical and legal concerns: Virtual therapy may raise ethical and legal concerns related to privacy, security, and informed consent. For example, ensuring that personal health information is kept confidential and secure may be more challenging in a virtual environment. |
References
- Flavián, C.; Ibáñez-Sánchez, S.; Orús, C. The impact of virtual, augmented and mixed reality technologies on the customer experience. J. Bus. Res. 2019, 100, 547–560. [Google Scholar] [CrossRef]
- Ramesh, P.V.; Joshua, T.; Ray, P.; Devadas, A.K.; Raj, P.M.; Ramesh, S.V.; Ramesh, M.K.; Rajasekaran, R. Holographic elysium of a 4D ophthalmic anatomical and pathological metaverse with extended reality/mixed reality. Indian J. Ophthalmol. 2022, 70, 3116–3121. [Google Scholar] [CrossRef] [PubMed]
- Iwanaga, J.; Muo, E.C.; Tabira, Y.; Watanabe, K.; Tubbs, S.J.; D’Antoni, A.V.; Rajaram-Gilkes, M.; Loukas, M.; Khalil, M.K.; Tubbs, R.S. Who really needs a Metaverse in anatomy education? A review with preliminary survey results. Clin. Anat. 2023, 36, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Mystakidis, S. Metaverse. Encyclopedia 2022, 2, 486–497. [Google Scholar] [CrossRef]
- Qiu, C.S.; Majeed, A.; Khan, S.; Watson, M. Transforming health through the metaverse. J. R. Soc. Med. 2022, 115, 484–486. [Google Scholar] [CrossRef] [PubMed]
- Morgado, L.; Allison, C.; Beck, D.; Penicheiro, F. Immersive Learning Research. J. Univers. Comput. Sci. 2018, 24, 70–71. [Google Scholar] [CrossRef]
- Hilty, D.M.; Alverson, D.C.; Alpert, J.E.; Tong, L.; Sagduyu, K.; Boland, R.J.; Mostaghimi, A.; Leamon, M.L.; Fidler, D.; Yellowlees, P.M. Virtual reality, telemedicine, web and data processing innovations in medical and psychiatric education and clinical care. Acad. Psychiatry 2006, 30, 528–533. [Google Scholar] [CrossRef]
- Cook, A.; Erwin, P.J.; Triola, M.M. Computerized Virtual Patients in Health Professions Education: A Systematic Review and Meta-Analysis. Acad. Med. 2019, 85, 1589–1602. [Google Scholar] [CrossRef] [Green Version]
- Sandrone, S. Medical education in the metaverse. Nat. Med. 2022, 28, 2456–2457. [Google Scholar] [CrossRef]
- A Whole New World: Education Meets the Metaverse. Available online: https://www.brookings.edu/research/a-whole-new-world-education-meets-the-metaverse/ (accessed on 20 February 2023).
- Kye, B.; Han, N.; Kim, E.; Park, Y.; Jo, S. Educational applications of metaverse: Possibilities and limitations. J. Educ. Eval. Health Prof. 2020, 18, 32. [Google Scholar] [CrossRef]
- Chang, E.; Kim, H.T.; Yoo, B. Virtual Reality Sickness: A Review of Causes and Measurements. Int. J. Hum.-Comput. Interact. 2020, 36, 1658–1682. [Google Scholar] [CrossRef]
- Lombardi, J.; Lombardi, M. Opening the Metaverse. In Online Worlds: Convergence of the Real and the Virtual; Human-Computer Interaction Series; Bainbridge, W., Ed. Springer: London, UK, 2010; pp. 111–122. [Google Scholar] [CrossRef]
- Nevelsteen, K.J. Virtual world defined from a technological perspective and applied to video games mixed reality and the metaverse. Comput. Animat. Virtual Worlds 2018, 29, e1752. [Google Scholar] [CrossRef] [Green Version]
- Virtual Life Support™, Created by VR Lab. Available online: virtuallifesupport.eu (accessed on 15 March 2023).
- Reulay, Inc. Available online: www.reulay.com (accessed on 15 March 2023).
- VictoryXR. Available online: www.victoryxr.com (accessed on 16 March 2023).
- University of Nebraska Medical Center- Lincoln College of Nursing and SimX. Available online: www.simxvr.com (accessed on 23 March 2023).
- Center for Systems Science and Engineering (CSSE) at Johns Hopkins University. COVID-19 Dashboard. Available online: https://coronavirus.jhu.edu/map.html (accessed on 20 January 2023).
- Wong, M.Y.Z.; Gunasekeran, D.V.; Nusinovici, S.; Sabanayagam, C.; Yeo, K.K.; Cheng, C.Y.; Tham, Y.C. Telehealth demand trends during the COVID-19 pandemic in the top 50 most affected countries: Infodemiological evaluation. JMIR Public Health Surveill. 2021, 7, e24445. [Google Scholar] [CrossRef] [PubMed]
- Kala, N. Revolutionizing Medical Education with Metaverse. Int. J. Sci. Res. Comput. Sci. Eng. Inf. Technol. 2022, 8, 26–32. [Google Scholar] [CrossRef]
- Metaverse: The Next Frontier for Health 4.0. Available online: https://www.netscribes.com/metaverse-in-healthcare/ (accessed on 22 January 2023).
- Jnr, A.B. Integrating telemedicine to support digital health care for the management of COVID-19 pandemic. Int. J. Healthc. Manag. 2021, 14, 280–289. [Google Scholar] [CrossRef]
- Vergara, D.; Rubio, M.P.; Lorenzo, M. On the design of virtual reality learning environments in engineering. Multimodal. Technol. Interact. 2017, 1, 11. [Google Scholar] [CrossRef] [Green Version]
- Rahaman, T. Into the Metaverse—Perspectives on a New Reality. Med. Ref. Serv. Q. 2022, 41, 330–337. [Google Scholar] [CrossRef]
- Zhang, X.; Chen, Y.; Hu, L.; Wang, Y. The metaverse in education: Definition, framework, features, potential applications, challenges, and future research topics. Front. Psychol. 2022, 13, 1016300. [Google Scholar] [CrossRef]
- Bansal, G.; Rajgopal, K.; Chamola, V.; Xiong, Z.; Niyato, D. Healthcare in Metaverse: A Survey on Current Metaverse Applications in Healthcare. IEEE Access 2022, 10, 119914–119946. [Google Scholar] [CrossRef]
- Chan, E.; Foster, S.; Sambell, R.; Leong, P. Clinical efficacy of virtual reality for acute procedural pain management: A systematic review and meta-analysis. PLoS ONE 2018, 27, 13. [Google Scholar] [CrossRef] [Green Version]
- Ahmadpour, N.; Randall, H.; Choksi, H.; Gao, A.; Vaughan, C.; Poronnik, P. Virtual Reality interventions for acute and chronic pain management. Int. J. Biochem. Cell Biol. 2019, 114, 105568. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Lin, W.; Zheng, Y.; Xue, T.; Chen, C.; Chen, G. Application of Active Learning Strategies in Metaverse to Improve Student Engagement: An Immersive Blended Pedagogy Bridging Patient Care and Scientific Inquiry in Pandemic. SSRN Electron. J. 2022. [Google Scholar] [CrossRef]
- Al-Elq, A.H. Simulation-based medical teaching and learning. J. Fam. Community Med. 2010, 17, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Thomason, J. MetaHealth—How will the Metaverse Change Health Care? J. Metaverse 2021, 1, 13–16. [Google Scholar]
- [33]Medical Augmented Intelligence (MAI) Is a Pioneer in the Field of Medical VR Innovations Creating the Google Maps of the Human Body. Available online: www.mai.ai/bodymap/ (accessed on 16 March 2023).
- Javaid, M.; Haleem, A. Virtual reality applications toward medical field. Clin. Epidemiol. Glob. Health 2020, 8, 600–605. [Google Scholar] [CrossRef] [Green Version]
- Bhugaonkar, K.; Bhugaonkar, R.; Masne, N. The Trend of Metaverse and Augmented & Virtual Reality Extending to the Healthcare System. Cureus 2022, 12, e29071. [Google Scholar] [CrossRef]
- Krijn, M.; Emmelkamp, P.M.G.; Olafsson, R.P.; Biemond, R. Virtual reality exposure therapy of anxiety disorders: A review. Clin. Psychol. Rev. 2004, 24, 259–281. [Google Scholar] [CrossRef]
- Spiers, H.J.; Maguire, E.A. Neural substrates of driving behaviour. NeuroImage 2007, 36, 245–255. [Google Scholar] [CrossRef] [Green Version]
- State-of-the-Art Human-Computer-Interaction in Metaverse. Available online: https://think.taylorandfrancis.com/special_issues/international-journal-human-computer-interaction-metaverse/ (accessed on 21 January 2023).
- Zhao, Y.; Jiang, J.; Chen, Y.; Liu, R.; Yang, Y.; Xue, X.; Chen, S. Metaverse: Perspectives from graphics, interactions and visualization. Vis. Inform. 2022, 6, 56–67. [Google Scholar] [CrossRef]
- Chengoden, R.; Victor, N.; Huynh-The, T.; Yenduri, G.; Jhaveri, R.H.; Alazab, M.; Gadekallu, T.R. Metaverse for Healthcare: A Survey on Potential Applications, Challenges and Future Directions. IEEE Access 2023, 11, 12765–12795. [Google Scholar] [CrossRef]
- Halbig, A.; Babu, S.K.; Gatter, S.; Latoschik, M.E.; Brukamp, K.; von Mammen, S. Opportunities and challenges of virtual reality in healthcare–a domain experts’ inquiry. Front. Virtual Real. 2022, 3, 837616. [Google Scholar] [CrossRef]
- Petrigna, L.; Musumeci, G. The Metaverse: A New Challenge for the Healthcare System: A Scoping Review. J. Funct. Morphol. Kinesiol. 2022, 7, 63. [Google Scholar] [CrossRef] [PubMed]
- Sandrone, S.; Carlson, C.E. Future of Neurology & Technology: Virtual and Augmented Reality in Neurology and Neuroscience Education Applications and Curricular Strategies. Neurology 2021, 97, 740–744. [Google Scholar] [CrossRef]
- Carl, E.; Stein, A.T.; Levihn-Coon, A.; Pogue, J.R.; Rothbaum, B.; Emmelkamp, P.; Powers, M.B. Virtual reality exposure therapy for anxiety and related disorders: A meta-analysis of randomized controlled trials. J. Anxiety Disord. 2019, 61, 27–36. [Google Scholar] [CrossRef]
- Metaverse Continuum. Available online: https://www.accenture.com/us-en/services/metaverse-index?c=acn (accessed on 14 March 2023).
- de Araújo, A.V.L.; Neiva, J.F.O.; Monteiro, C.B.M.; Magalhães, F.H. Efficacy of Virtual Reality Rehabilitation after Spinal Cord Injury: A Systematic Review. Biomed. Res. Int. 2019, 13, 7106951. [Google Scholar] [CrossRef]
- Lee, M.; Suh, D.; Son, J.; Kim, J.; Eun, S.D.; Yoon, B. Patient perspectives on virtual reality-based rehabilitation after knee surgery: Importance of level of difficulty. J. Rehabil. Res. Dev. 2016, 53, 239–252. [Google Scholar] [CrossRef]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Suh, I.; McKinney, T.; Siu, K.-C. Current Perspective of Metaverse Application in Medical Education, Research and Patient Care. Virtual Worlds 2023, 2, 115-128. https://doi.org/10.3390/virtualworlds2020007
Suh I, McKinney T, Siu K-C. Current Perspective of Metaverse Application in Medical Education, Research and Patient Care. Virtual Worlds. 2023; 2(2):115-128. https://doi.org/10.3390/virtualworlds2020007
Chicago/Turabian StyleSuh, Irene, Tess McKinney, and Ka-Chun Siu. 2023. "Current Perspective of Metaverse Application in Medical Education, Research and Patient Care" Virtual Worlds 2, no. 2: 115-128. https://doi.org/10.3390/virtualworlds2020007
APA StyleSuh, I., McKinney, T., & Siu, K.-C. (2023). Current Perspective of Metaverse Application in Medical Education, Research and Patient Care. Virtual Worlds, 2(2), 115-128. https://doi.org/10.3390/virtualworlds2020007









