1. Introduction
Orofacial anatomy is a pillar of knowledge for medical and dental education [
1,
2]. It provides the framework for future health professionals to develop their clinical skills and performance. Additionally, it supports human identification issues in the forensic context [
3].
The orofacial region has a particular property of resilience and resistance to extreme forensic conditions [
1]. Orofacial anatomy, namely dental anatomy, is recording along individual life by health professionals into the clinical record. The goal of orofacial practice requires the understanding of the two-dimensional (2D) and three-dimensional (3D) morpho-anatomy of the stomatognathic system [
1,
2,
3,
4,
5]. Normal anatomy allows for the comparative assumption to define the abnormal condition [
1,
3]. Orofacial discrepancies and their heterogeneous anatomical traits include different and distinct orofacial and dental characteristics. For example, orofacial cleft (OFC) is the leading congenital disability in the craniofacial region [
6]. The OCF phenotypes are broadly divided into three types: isolated cleft lip, isolated cleft palate, and simultaneous cleft lip and palate [
7]. OFC is associated with the supernumerary maxillary primary lateral incisor or agenesis, which can also occur in permanent dentition [
6]. This pathology prevalence differs by geographical region, ranging from 2.9 to 23.9 per 10,000 [
8], concerning its discriminating power in anatomical identification [
9,
10]. The discriminatory power for each piece of evidence is referring the number of possible candidates (identities) that can be excluded on that basis [
10]. Anormal features correlated to a lower frequency have significantly more discriminatory power than normal or usual features [
9,
10,
11]. This assumption in transversal is used in human identification for forensic purposes under genotyping methodology [
9,
11]. Orofacial surgery aims to correct facial skeletal discrepancies. Dental rehabilitation’s goal is to correct dental disharmony and pathological functions. These rehabilitations are based on objective evaluation and complementary diagnostic exams, such as photography and radiological exams. These exams are a database of individual anatomical information for prospective analysis.
The identification procedure in a forensic scenario includes comparing and analyzing data [
1]. The first line of the procedure’s orofacial analysis consists of details of tissues, soft and hard, and clinical features. The facial soft tissues analysis corresponds to the definition of shape, proportionality, and symmetry. The facial hard tissues analysis corresponds to the record of morphological and anatomical features. These analyses should be performed concerning standard guidelines and anatomical references [
1]. Positive identification is the goal of the global process, with an impact on legal issues, such as death certificates, insurance proceeds, estate transfers, settlement of probate, execution of wills, remarriage, and child custody [
1,
2,
10,
11].
Anatomy teaching is associated with studying human identification within the scope of the missing and unidentified person. The study of human identification has its first line of action: dactyloscopy, visual or visual, anthropological, and dental methods. They are immediate and more economical than genotyping. They integrate the general medical examiner’s knowledge of human anatomy and mass disaster team skills. Both areas are part of the Professional Qualifications Directive’s requirement and the Bologna Declaration’s guidelines [
12,
13,
14,
15].
This manuscript intends to correlate anatomical changes following orofacial iatrogenic interventions and their impact on forensic human identification within an educational approach.
2. Materials and Methods
An observational and retrospective cohort study was performed on cephalography and photographic exams of patient records of the Clinical Academic Center of Coimbra (CACC), in line with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) methodology. The CACC is a consortium between the University and Hospital Center of Coimbra and the Faculty of Medicine at the University of Coimbra (FMUC), Portugal.
The inclusion criteria were as follows: clinical record in national health service; Class III Angle diagnosis as the record of orofacial, dental, and/or facial anatomy discrepancies; orthognathic surgery the scope of orofacial rehabilitation; events between January 2017 and May 2019; and an adult population. Medical reports with systemic diseases and aesthetic surgery goals were excluded.
Informed consent was provided in compliance with the Faculty of Medicine Ethics Committee (process number 23-CE-2017).
A team dentist performed the victim’s exam with a forensic odontologist from the Laboratory of Forensic Dentistry at the University of Coimbra, Portugal. The research team had up to 15 years of experience in medico-legal expertise and anatomy education. The sample selected in the CACC database included patients (n = 30) aged between 18 and 26 years.
The horizontal subdivision and proportionality of the face were performed in photography and cephalometry. Following Arnett’s study [
16], there are several landmarks in face analysis procedure: (1) upper one-third of the face, between triquio (Tri) and glabella (Gl) soft tissue points; (2) medium one-third of the face, between Gl and sub nasale (SN) soft tissue points; and (3) lower one-third of the face, between Sn and menton (Me) soft tissue points. The horizontal proportionality is achieved when the three portions have the same size. The vertical subdivision of the face was performed regarding the DMV Atlas [
17] regarding the medium sagittal line, allowing for analyzing the left and right proportion. For example, the breadth of the nasal bridge in the middle portion of the nasal bridge in frontal view: narrow, average, or broad; or the form of the chin contour or its shape: round, square, or pointed [
17].
Cone-Beam Computed Tomography (CBCT) guidelines are well defined following clinical procedure [
2]. Photographic standards are well defined and discussed in several medical fields, for example, plastic surgery and orthodontics. Digital photography was performed following institutional guidelines and widespread use in clinical documentation. The patient’s head should be aligned to the Frankfort horizontal line for the frontal view. The focal point and center of the picture is the intersection between the Frankfort horizontal line and the midline of the face. The patient should look straight, and the interpupillary line should be horizontal. No rotation in the vertical axis should occur. Lips should be relaxed with a visible inter-labial gap if it exists. By enlargement, the following close-up views can be achieved of the full-face front view: front view of eyes, front view of lower face and jaw, front view of the nose, and front view of auricles.
The reports were randomly selected according to previous inclusion, and exclusion criteria were reviewed and interpreted according to the anatomical features in the thirds of the face compared to pre- and post-surgery intervention in the oral rehabilitation plan for identification purposes. Descriptive analysis was performed, and intra- and inter-observer errors were analyzed by the Technical Measurement Error test.
3. Results
The anatomical analysis was performed in two periods: before and after orthognathic surgery regarding the Class III Angle previous diagnostic of 30 patients in homogeneous sex distribution. Intra- and inter-observer errors were nonsignificant.
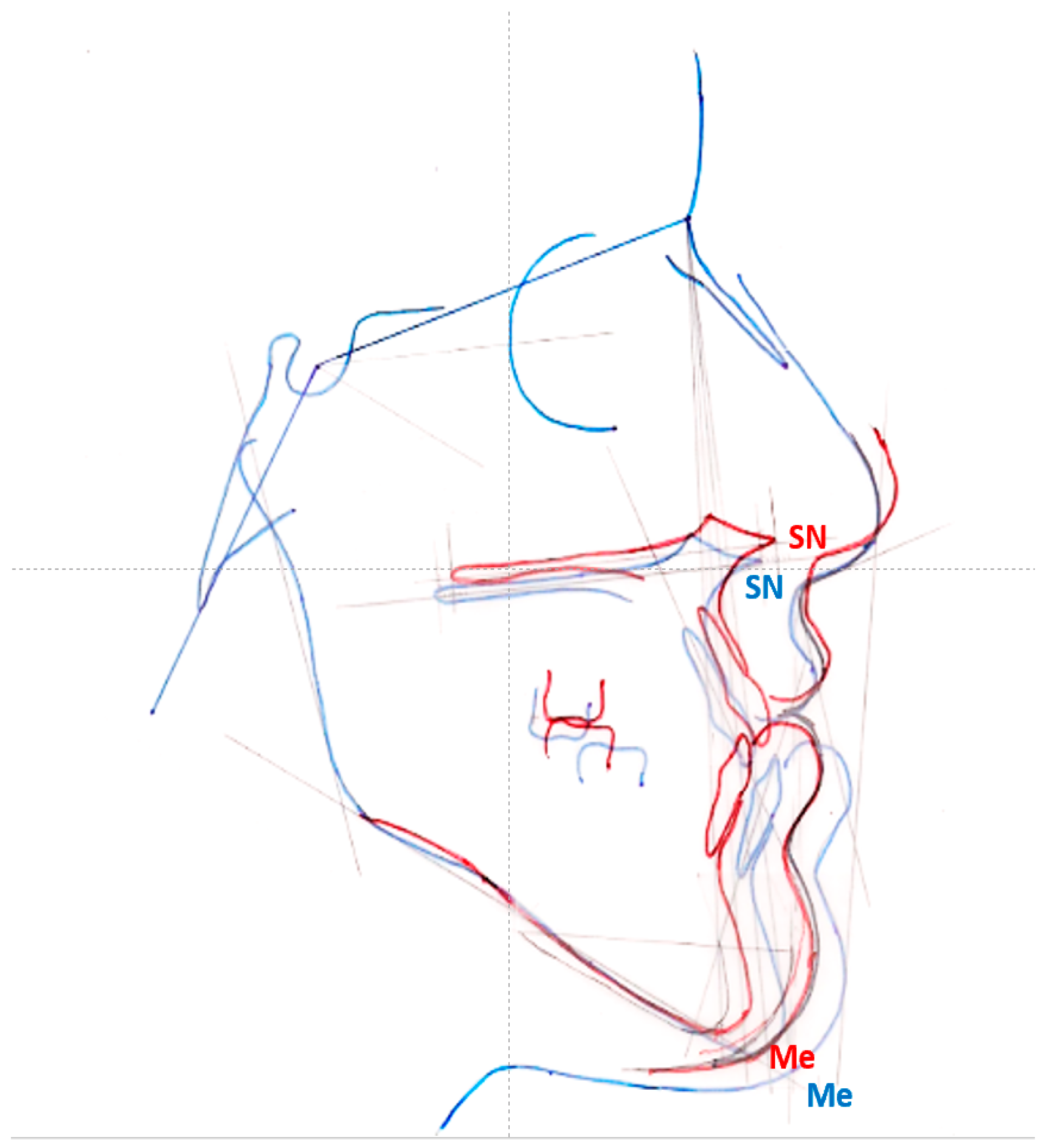
Surgical interventions caused differences in the individual’s facial features after the intervention. Orthognathic surgery was the cause for these differences detected on the lower one-third of the face. The anatomical measure (SN and Me), or the height of the lower one-third height, is highlighted as a change measurement (67%) (
Figure 1 and
Table 1), detected on frontal and lateral views on photographic and cephalometric analysis. The anteroposterior analysis (between the craniometric and cutaneous points) performed on cephalometric exams was also highlighted as a changed measurement (
Table 1).
Regarding the differences with the professional intervention, a positive value indicates the decrease between the two records for the same individual, and a negative value indicates the opposite (
Table 1). A positive result means that the starting value is greater than the ending value. Differences were highlighted in horizontal proportionally, in height, and in anteroposterior analysis.
Left and right asymmetry, or vertical proportionality analysis, was performed in the frontal analysis of the face, and a symmetry in 87% of the sample was achieved under the initial diagnosis of facial disharmony. No changes were detected in 13% of the sample.
4. Discussion
Professional interventions that interfere with hard and soft tissue orofacial anatomical features have potential outcomes in biometric data and should be discussed regarding their impact in the forensic scope, such as identity. Asserting one’s identity is a universal right.
Orthognathic surgery introduces changes in the anatomy of the face and, consequently, in the individual’s visual aspect and identity profile. Our findings highlight anatomical changes in the lower one-third of the face. The results relate interdental relations between lower and upper dental arches under maxilla and mandible surgery [
18]. These relations within the stomatognathic system emphasize the bone and dental support of the soft tissues, impacting the anatomy of the lips and chin.
The challenge of human identification consists of undocumented person situations. Science must follow the moment’s needs in the practical impact of its outcomes. This is a current and relevant topic in the context of natural disasters and armed conflicts and human migration flows [
9]. This technical note intends to adjust the visual recognition methodology, namely orofacial data comparison, as it corresponds to the first line of action in human identification. International forensic experts use morphological or anatomic analysis to compare missing and unidentified data as an identification procedure [
11]. Biometric data in visual and dental methodologies lead to a consistent evaluation of anatomical features [
11] based on integrated and complementary analysis using photo and radiological exams.
Orofacial identification, according to Pretty and Sweet, 2001, is based on anatomical features like the maxillary sinus (size, shape, foreign bodies, and relationship to teeth), anterior nasal spine, mandibular canal, coronoid and condylar processes, and temporomandibular joint [
1]. Atlas of these morphological details must be a standard procedure, and it must comprise part of professional education, because the selection of reference planes is the most relevant in anatomical evaluation. The evaluation of hard and soft tissues and their anatomy can be performed by bi- or three-dimensional analysis, namely CBCT technology [
19]. Soft tissue landmarks, namely Sn (the point at which columella merges with the upper lip in the midsagittal plane) and Me (the lowest median landmark on the lower border of the chin) [
19], can be identified in photography as well as in CBCT reconstruction. The digital technologies associated with photography and radiological software allow for a realistic metrics analysis (related with minimum distortion) of the horizontal and vertical, proportionally allowing for a positive coordinate evaluation of the sample.
In the present study, the results (
Table 1) follow and reinforce the differences in facial profiles following the surgical intervention. The vertical proportionally was performed using a vertical plane for a qualitative analysis of facial asymmetry [
17,
19,
20,
21]. The photographic CBCT records highlight hard tissue landmarks to construct the reference plane following the Hwang study [
19]. The advantage of using soft tissue landmarks under hard tissue landmarks is that the hard and soft tissue can be evaluated simultaneously, enabling us to assess the hard and soft tissue interrelationship more accurately and overcome the potential difference in thickness under specific population groups following anatomical regions, such as the lips [
19]. The standardized anatomical planes for hard and soft tissue evaluation will simplify the analysis procedure. This general procedure in clinical practice further contributes to the broader use of 3D image analysis in everyday practice. Concerning the right and left bone anatomical discrepancies, it is not fully reflected in soft tissue because it is compensated or masked by muscle and/or skin tissue, which significantly impacts achieving symmetry after bone surgery. The present study emphasizes midline landmarks to overcome the discrepancy between right and left anatomical landmarks. Regarding a methodology for asymmetry evaluation, it highlights that the mandible is a mobile structure compared to the maxilla, connecting to the adjacent structures and adjusting to outcomes of surgical intervention following Severt and Proffit [
20].
Anatomical discrepancies compared to regular anatomy can be an essential feature in identity. In the scope of human identification, an orofacial anatomy study (radiographic study of orofacial and dental anomalies) is a population-based feature. The findings specific to the population overcome unbiased comparison in forensic procedures—these clinical conditions spotlight clinical and complementary exams as tools for a forensic report and prospective identity procedure.
The purpose of health professional intervention is to correct abnormalities and functions, such as orthognathic surgery’s purpose to overcome the anatomical discrepancies to achieve a stable or normal condition. The technological advances to improve the patient’s esthetic and functional clinical condition can alter anatomical relationships and deviate from the predictable anatomy of the face, regarding the present results. The match between clinical data is a condition for overlapping the anatomical region in the comparison between pre- and post-surgery for identification purposes. Positive identification is achieved under the match between orofacial features, and negative identification is achieved under a no match. There is a medico-legal impact of a no match condition. The legal impact of the result is related with legal, civil, religious, and cultural reasons.
The victim’s medical history should be considered in this procedure to overcome an incorrect result and its medico-legal impact. The clinical record assessment is relevant knowledge for the discriminating diagnosis and has real value for correct identification.
Standards for individual records in clinical practice should be in accordance with identification analysis for a forensic purpose [
21]. Anatomical features discussed in photographs and complementary exams are essential for pre- and post-operative documentation [
21]. These planning data illustrate the purpose of the surgical intervention for the patient and its consistent documentation, which is demanded in medico-legal cases. In addition, these records support anatomical education as well as a scientific study.
This analysis is included in the multimodal pedagogical process in anatomy education, performed using two tools, photography and imagology, and namely CBCT technology, that sequentially complement the student’s skills [
2]. The integration of CBCT technology corresponds to the anatomical interpretation of multiplanar medical images and multiplied 2D slices in 3D reconstructions or 3D models, spotlighting external and internal anatomical details and their relations, whose dynamics positively attracted the students’ attention [
2,
5]. The Master’s degree corresponds to integrated education, and anatomy knowledge should be related to legal medicine or forensic issues with an impact on hot topics, such as identification in human traffic and migration flow [
9].
Plastic and reconstructive surgery is a particular intervention and topic related to the identity process that was not considered in this manuscript.