Abstract
The chaperone system (CS) is emerging as a key multistage participant in carcinogenesis. The CS chief components are the molecular chaperones (some of which are named heat shock proteins or Hsp), which are typically cytoprotective but if abnormal in structure, location, or quantity, can become etiopathogenic and cause diseases, known as chaperonopathies, including some cancers. For example, abnormal Hsp90 expression is associated with tumorigenesis and poor prognosis. Hsp90 is positioned at the center of several key oncogenic pathways by stabilizing and activating oncogenic kinases responsible for driving cell proliferation and survival. Consequently, inhibition of Hsp90 is being investigated as a possible anti-cancer strategy and some results are encouraging. However, the 5-year survival rate for patients suffering from salivary gland carcinomas is still unsatisfactory. Because of the rarity of these malignancies, they may have been overlooked and understudied and, thus, novel therapies (e.g., inhibition of CS components like Hsp90 and others) are urgently needed. In this review, we also summarize the histopathological quantitative patterns and the intra- and extra-cellular location characteristics of Hsp90 in tumors of salivary glands, pointing to their potential for differential diagnosis, prognostication, and patient monitoring.
1. Introduction
Salivary glands are part of the body’s exocrine system because they secrete their biological product, the saliva, through a system of ducts. The salivary glands are in the oral cavity and are classified into two groups: major and minor. The major salivary glands occur in pairs and are grouped based on their anatomical location in the oral cavity and on their size, with the parotid gland (PG) being the largest followed by the submandibular gland (SMG) and the sublingual being the smallest [1,2,3]. Despite being smaller than the parotid, the submandibular gland accounts for 70% of the saliva output. The minor glands consist of hundreds of small clusters of glands scattered throughout the mucosa of the aerodigestive tract being more concentrated along the buccal, labial, and lingual mucosae, soft and hard palates, and mouth floor [2,4]. The acini are the secretory units of the salivary glands, containing secretory granules that produce the saliva (Figure 1). Although saliva is formed in the acini, it undergoes several physiological and chemical processes along its passage through the ductal system to become the final product that is secreted in the buccal cavity.
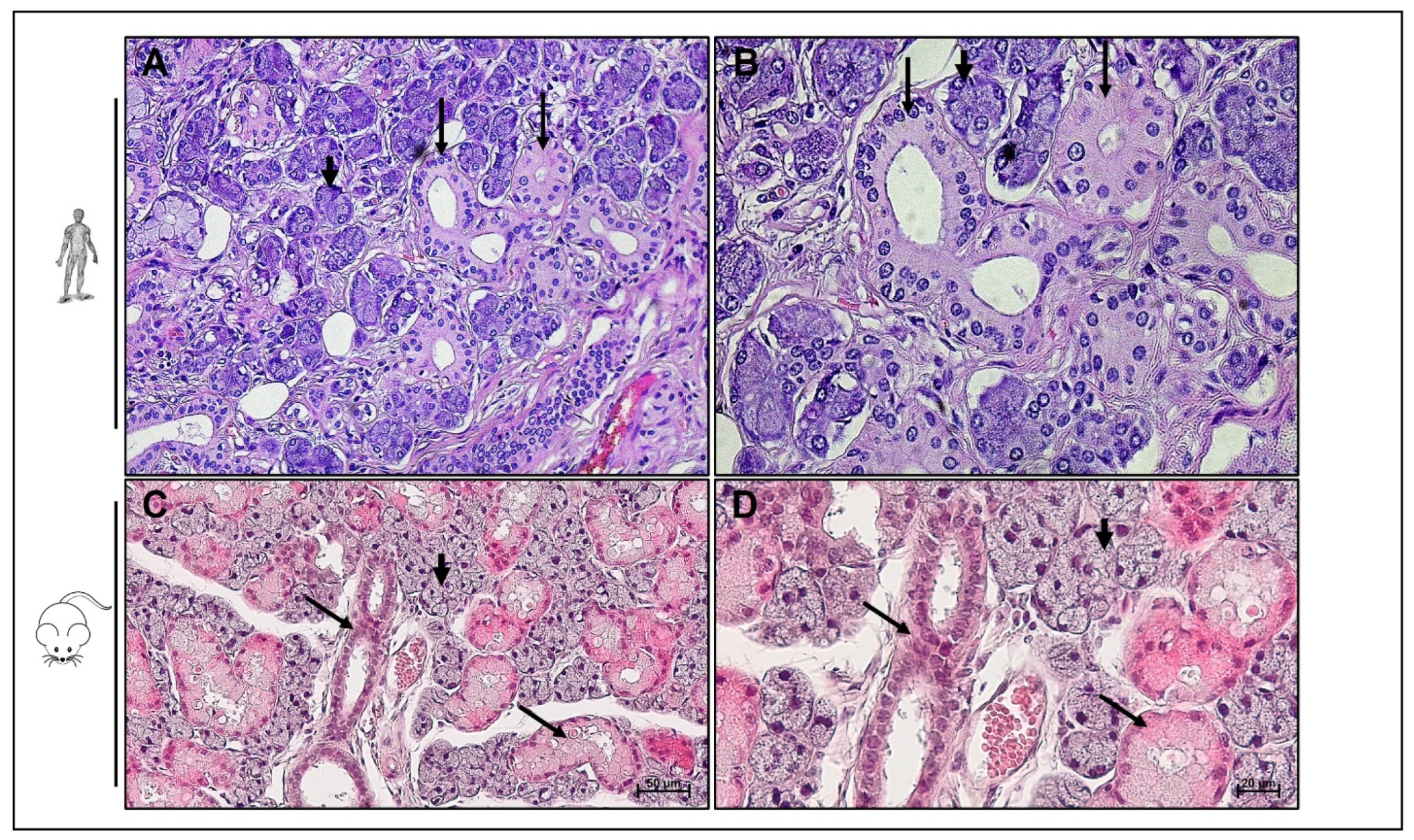
Figure 1.
Histological structure of salivary glands. Hematoxilin and eosin staining of adult human (upper panel) and adult mouse (lower panel) submandibular gland. Acini (short arrow) and ducts (long arrow) are featured in both human and mouse submandibular glands. (A,C) Bar 50 µm. (B,D) Bar 20 µm.
Saliva is composed of 99.5% water and 0.5% glycoproteins, mucus, electrolytes, enzymes, immunoglobulins, and antibacterial composites [5]. Saliva composition is detailed in Table 1. As food enters the mouth, digestion is initiated by salivary α-amylase that catalyzes the breakdown of starch into glucose and maltose. Saliva has other physiological functions including: (1) mouth lubrication for facilitating speech and mastication, (2) protection of teeth from cavities, (3) antibacterial activity, (4) enhancing taste sensation, (5) hormonal activity, and (6) generation of the food bolus, enabling its swallowing for further processing [1,2,3,6,7].

Table 1.
Saliva composition.
Hsp90 (Heat shock protein 90) is recognized as a crucial player in various aspects of cellular function, including protein folding, stabilization, and degradation. Its role in cancer, including salivary gland tumorigenesis, has been an area of active research.
Hsp90 functions as a chaperone protein, assisting in the correct folding and maturation of other proteins that are involved in key signaling pathways regulating cell growth, survival, and proliferation [8]. In cancer, the overexpression and increased activity of Hsp90 have been observed in several tumor types, including salivary gland tumors [8]. This increased expression is thought to support the folding and stabilization of oncogenic client proteins, enabling the survival and proliferation of cancer cells.
Researchers in many laboratories (including ours) have explored Hsp90 as a potential therapeutic target for cancer treatment. By inhibiting Hsp90’s activity, the stabilization of oncogenic proteins could be disrupted, leading to the degradation of these proteins and impairing tumor growth [8]. Several Hsp90 inhibitors have been investigated in preclinical studies and clinical trials for various cancers, including some types of salivary gland tumors [8].
2. Salivary Glands Cancer: Epidemiology and Pathogenesis
The epidemiology and pathogenesis of salivary gland cancer have been subjects of ongoing research. Here is an overview of the general understanding to date. Salivary gland cancer can occur at any age, but it is most commonly diagnosed in individuals between the ages of 50 and 70. Salivary gland tumors are very heterogenous and histologically diverse; more than 30 distinct pathological types of salivary gland tumors have been categorized [9]. Typically, salivary gland tumors are classified based on cytologic, histopathologic, and immunohistochemical characteristics. Although these established parameters for identifying and classifying salivary glands tumors are still considered the gold standard, lately genetic features have been added to their definition [10]. In their latest edition of the classification of tumors of head and neck published in 2022, the world health organization (WHO) has added six new entities [10]. Salivary gland cancers are a heterogeneous group of tumors that can arise from different cell types within the salivary glands. The exact pathogenesis can vary depending on the specific subtype of salivary gland cancer. Some common subtypes include: (1) mucoepidermoid carcinoma (MUC): this is the most common subtype and is believed to arise from ductal or glandular cells. Genetic alterations, such as gene fusions involving MAML2 and CRTC1 genes, have been implicated in the development of mucoepidermoid carcinoma. (2) Adenoid cystic carcinoma (ACC): this subtype is thought to arise from the myoepithelial cells of the salivary glands. Chromosomal translocations involving the MYB and NFIB genes have been identified in many cases of adenoid cystic carcinoma. (3) Acinic cell carcinoma: this subtype arises from the acinar cells of the salivary glands. Specific genetic alterations, including rearrangements of the genes ETV6 and NTRK3, have been associated with acinic cell carcinoma. (4) Polymorphous adenocarcinoma: the pathogenesis of this subtype is not fully understood, but it is believed to originate from the terminal duct cells of the salivary glands. Research into the molecular and genetic basis of salivary gland cancer has advanced our understanding of its pathogenesis, and ongoing studies aim to identify potential therapeutic targets for these tumors.
Despite being considered rare, a significant increase in salivary gland tumors incidence has occurred. Salivary gland cancers accounted for 6.3% of all head and neck carcinomas (HNC) in 1974–1976 and increased to 8.1% in 1998–1999 [11]. Statistical studies conducted in Europe in 2013 estimate that salivary gland malignancies represent 8.5% of all HNC [4]. Major salivary gland malignant neoplasia increased by 54% from 1973 to 2009 [12]. The etiology of salivary gland tumors remains largely unknown, although several risk factors have been established, with irradiation being the most dangerous. Advances in the medical field and the use of modern tools for diagnosis and for routine screening at medical and dental clinics have increased our daily exposure to ionizing radiation and may have played a role in the increase of salivary gland tumor occurrence [11]. Other risk factors have been associated with salivary gland cancer development, including: (1) gender: certain subtypes of salivary gland cancer, such as mucoepidermoid carcinoma and adenoid cystic carcinoma, tend to have a higher incidence in females. (2) Age: the risk of salivary gland cancer tends to increase with age. (3) Occupational exposures: occupational exposure to certain substances, such as asbestos and nickel refining, has been suggested as a potential risk factor for salivary gland cancer. (4) Prior benign tumors: some benign salivary gland tumors, such as pleomorphic adenomas, may have an increased risk of developing into malignant tumors.
3. Salivary Gland Cancer Treatment and Patient Management
Salivary gland cancer treatment and patient management depend on various factors, including the tumor type, stage, location, and the patient’s overall health. The management often involves a multidisciplinary approach, with a team of specialists collaborating to create a personalized treatment plan. The primary treatment options for salivary gland cancer include surgery, radiation therapy, and in some cases, chemotherapy or targeted therapy. Here is a summary of the common treatment approaches and patient management strategies:
- (1)
- Surgery: Surgery is the primary treatment for most salivary gland cancers. The extent of surgery depends on the tumor size, location, and whether it has spread to nearby lymph nodes or other tissues. The goal of surgery is to remove the tumor while preserving as much healthy tissue and salivary gland function as possible.
- (2)
- Radiation therapy: Radiation therapy may be used as the primary treatment for small tumors, in combination with surgery, or after surgery to destroy any remaining cancer cells. External beam radiation delivers focused radiation to the tumor site while sparing surrounding healthy tissues.
- (3)
- Chemotherapy: Chemotherapy is not commonly used for all types of salivary gland cancer but may be considered for certain aggressive or advanced cases. It involves the use of drugs to kill cancer cells or stop their growth.
- (4)
- Targeted therapy: Targeted therapy is a newer approach that focuses on specific molecular targets within cancer cells. It is used in some salivary gland cancers that have specific genetic mutations or alterations.
- (5)
- Immunotherapy: Immunotherapy is being explored in clinical trials for some salivary gland cancers. It involves boosting the patient’s immune system to recognize and attack cancer cells more effectively.
- (6)
- Adjuvant and neoadjuvant therapies: Adjuvant therapy refers to additional treatment after the primary treatment (surgery or radiation) to reduce the risk of cancer recurrence. Neoadjuvant therapy is given before the main treatment to shrink the tumor and improve the chances of successful surgery or radiation.
- (7)
- Palliative care: For advanced or metastatic cases where a cure may not be possible, palliative care focuses on improving the patient’s quality of life. It aims to manage symptoms, alleviate pain, and provide emotional and psychological support to both the patient and their family.
- (8)
- Patient management also includes regular follow-up visits with the medical team to monitor treatment response, assess for any recurrence, and manage potential side effects. Supportive care, including speech and swallowing therapy, nutrition counseling, and psychological support, is vital for patients dealing with the effects of treatment on salivary gland function and overall well-being.
Overall, the treatment and management of salivary gland cancer require a comprehensive and individualized approach to optimize the chances of successful outcomes while minimizing potential side effects and maintaining the patient’s quality of life. As research continues to advance, more targeted and personalized treatments are likely to emerge, improving the outlook for patients with this rare form of cancer.
The rarity of salivary gland tumors and their variety are probably the reason of the scarcity of pertinent animal models and cell lines, which in turn slows down progress in the understanding of carcinogenic mechanisms and, consequently, blocks development of efficacious treatments. Therefore, no protocol for salivary gland tumor treatment and management has yet been standardized [13,14]. Generally, salivary gland tumors are surgically excised, which may be accompanied by adjuvant radiotherapy (RT) or chemotherapy (CT) [13]. Because of its low efficiency, CT is usually considered the last resort, palliative, in locally recurrent or metastatic salivary gland cancers that are not amenable to further surgery and irradiation [13]. For diagnosis, ultrasound-guided fine needle aspiration cytology or core biopsy is applied. [15]. For benign tumors, excision of the SMG in a supracapsular plane is the recommended therapeutic approach, while for PG, a partial or radical excision with the facial nerve is usually recommended. RT is not recommended in most benign tumor cases, especially for younger patients, except for intra-operative tumor spillage, where it may be considered after a long-term follow up. For malignant tumors of SMG, wide excision is recommended with a 2 cm margin of healthy tissue, with neck dissection for patients with clinical metastasis in the neck. Elective neck dissection should be considered in high-grade tumors of SMG more than 4 cm in size in addition to a 6-week post-operative adjuvant RT. Primary radiotherapy should be considered for specific cases in which surgical treatments cannot be applied. For malignant tumors of PG, conservative or partial parotidectomy is recommended as the method of treatment, the latter for low-grade tumors (<1.5 cm). If the facial nerve is properly functioning pre-operatively, it is recommended that a direct microsurgical repair or primary nerve graft be performed within a year of the surgery. Neck dissection should be performed if clinical or radiological evidence of nodal diseases is found. In high-grade tumors, a selective/prophylactic neck dissection may be applied and, finally, radiotherapy may be applied to tumors that are >4 cm in size [15].
4. Hsp90 in Cancer
Recent advances in cancerology have encompassed various areas of research, including genetic inheritance, RNA varieties and roles (including diagnostic and therapeutic applications), drug design and delivery, extracellular vesicles, and chaperonology [16]. The latter pertains to the study of the chaperone system (CS), a physiological system akin to other systems, e.g., the immune system [17]. The CS is composed of molecular chaperones, chaperone co-factors, co-chaperones, chaperone interactors, and receptors. The molecular chaperones are the chief components of the CS and are typically cytoprotective, under physiologically normal conditions and under stress. However, when abnormal, molecular chaperones or any of the other CS components can become etiopathogenic and cause diseases, i.e., chaperonopathies [18,19]. These diseases have been classified like many other disorders into genetic and acquired, with the former caused by a change in a gene encoding a CS member, and the latter caused by post-transcriptional or post-translational modifications of the gene’s product. Molecular chaperones are the chief members of the CS, but they typically do not act alone and form teams and networks. This is exemplified by the chaperone Hsp90, which forms teams and networks with various other components of the CS [8,18]. Hsp90 represents a group of molecular chaperones that have been named heat shock proteins (Hsp) accompanied by a number which is its molecular weight (e.g., 90 kDa for Hsp90). We have been studying the CS in the salivary glands, mapping some of its components in normal and pathological, including cancerous, tissues [8,20,21,22,23]. Heat shock proteins are molecular chaperones that maintain protein integrity and function to counteract the effects of stressors such as a heat shock, irradiation, inflammation, heavy metals, antibiotics, alcohols, oxidation, pH change, osmotic alteration, and mechanical trauma [8,22]. Under physiological conditions, molecular chaperones maintain protein homeostasis by promoting folding of newly synthesized proteins into their functional conformation [22]. Thus, the canonical role of the CS is maintaining protein homeostasis, which, for some functions requires interaction with the ubiquitin–proteasome system (UPS) and/or with the chaperone-mediated autophagy (CMA) machinery. Apart from their canonical role, molecular chaperones have other non-canonical functions and for this they may interact with the immune system [23,24,25]. For instance, some Hsp mediate immune reactions by binding to antigenic peptides and chaperone them towards MHC class I molecules at the cell surface for presentation to lymphocytes, a process known as cross-presentation [23]. As tumors develop and grow, protein synthesis is increased and thus the demand for molecular chaperones, including Hsp90, increases and neoplasms become “chaperone addicted” [8].
Hsp90 is the master regulator of various growth, inflammation, and survival pathways [8]. Pronounced expression of Hsp90 in several cancer types has been reported [26,27,28,29,30]. Hsp90 has been proposed as a potential biomarker because its increased expression in neoplastic tissue correlates with clinically advanced stages and poor prognosis [31,32,33,34,35,36]. As reported for other Hsp, Hsp90 pattern of expression can be tissue-specific as shown by a decrease in Hsp90 tissue levels in infiltrative lobular carcinoma [37].
Hsp90-targeted therapy has gained considerable attention as a non-invasive alternative/adjuvant intervention for cancer treatment [8]. Several natural and synthetic compounds have been assessed for their efficacy against cancer. For instance, Hsp90 inhibitors are considered promising candidates for use to abate cancer progression and some of them have entered stage III clinical trials [8].
5. Hsp90 in Salivary Gland Tumors
Studies have revealed that Hsp90 is often overexpressed in salivary gland tumors, promoting the correct folding, stability, and activity of oncogenic client proteins [38,39,40]. This activity allows cancer cells to survive, proliferate, and resist apoptosis (cell death), leading to tumor growth and progression. The overexpression of Hsp90 has been associated with more aggressive tumor behavior and poorer prognosis in some cases.
Researchers have investigated Hsp90 as a potential therapeutic target for salivary gland tumors. By inhibiting Hsp90’s chaperone function, it is possible to disrupt the stabilization of oncogenic proteins, leading to their degradation and hindering tumor growth. Hsp90 inhibitors have been studied in cell models as a potential treatment strategy for salivary gland cancers as an initial step that precedes preclinical models and clinical trials with the hope of improving patient outcomes and developing more effective therapies.
Hsp90 histopathological expression and role in pathophysiology has been studied in a range of cancers but not as much in those of the salivary glands. In this section, we present findings retrieved from the literature about Hsp90 in salivary glands tumors. A study investigated the pattern of distribution and expression of a panel of Hsp (Hsp27, Hsp60, Hsp84, and Hsp86) in 81 specimens of salivary gland tumors [38]. Benign tumors encompassed adenolymphoma, mixed tumors and others while malignant tumors included ACC, MUC, and others. The spatial distribution of Hsp84 and Hsp86, members of the Hsp90 family, was mainly confined to the cytoplasmic portion of the epithelium of the tumors and partly expressed in the nucleus [38]. Semi-quantitative analysis showed that Hsp84 and Hsp86 levels were pronounced in both malignant and benign tumors while being higher in malignant tumors [38]. In benign tumors, Hsp84 and Hsp86 showed higher levels in mixed tumors than in adenolymphoma [38]. Hsp86 immunopositivity intensity was positively correlated with neural invasion, metastasis, malignant grading, tumor site, and proliferation index [38]. Two similar studies assessed the immunohistochemical levels of Hsp27 and Hsp60 as well as Hsp10 and Hsp90 in 20 and 66 cases of salivary gland tumors, respectively [20,21]. Illustrative images of chaperone Hsp90 in tumor tissues from salivary glands are shown in Figure 2. Warthin’s tumor (WT) and pleomorphic adenoma (PA) represent the benign tumors while ACC, MUC and ex-pleomorphic adenoma (EX-PA) illustrate the malignant lesions. The panel of the aforementioned molecular chaperones was distributed in the cytoplasmic portion of the epithelium in all specimens [20]. The results reported corroborate the findings that were discussed in the previous study [38]. Hsp90 levels, unlike Hsp10, Hsp27, and Hsp60, were significantly increased in ACC, MUC, and EX-PA and significantly diminished in WT and PA when compared to healthy salivary glands [20]. In the previous study [38], a comparison of the Hsp90 levels in the tumors with those in healthy salivary glands was not reported, therefore, insights on the clinical applicability of Hsp90 measurements as a diagnostic marker to differentiate between healthy and neoplastic salivary glands and also to differentiate between benign and malignant tumors were not obtained. Another group examined Hsp90 molecular expression in benign and malignant tumors of the salivary glands and their findings are in accordance with the immunohistological data highlighted above as Hsp90 mRNA levels are prominent in both tissue types [39].
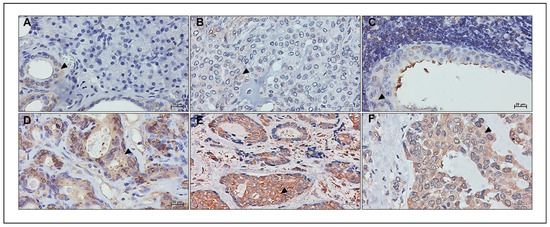
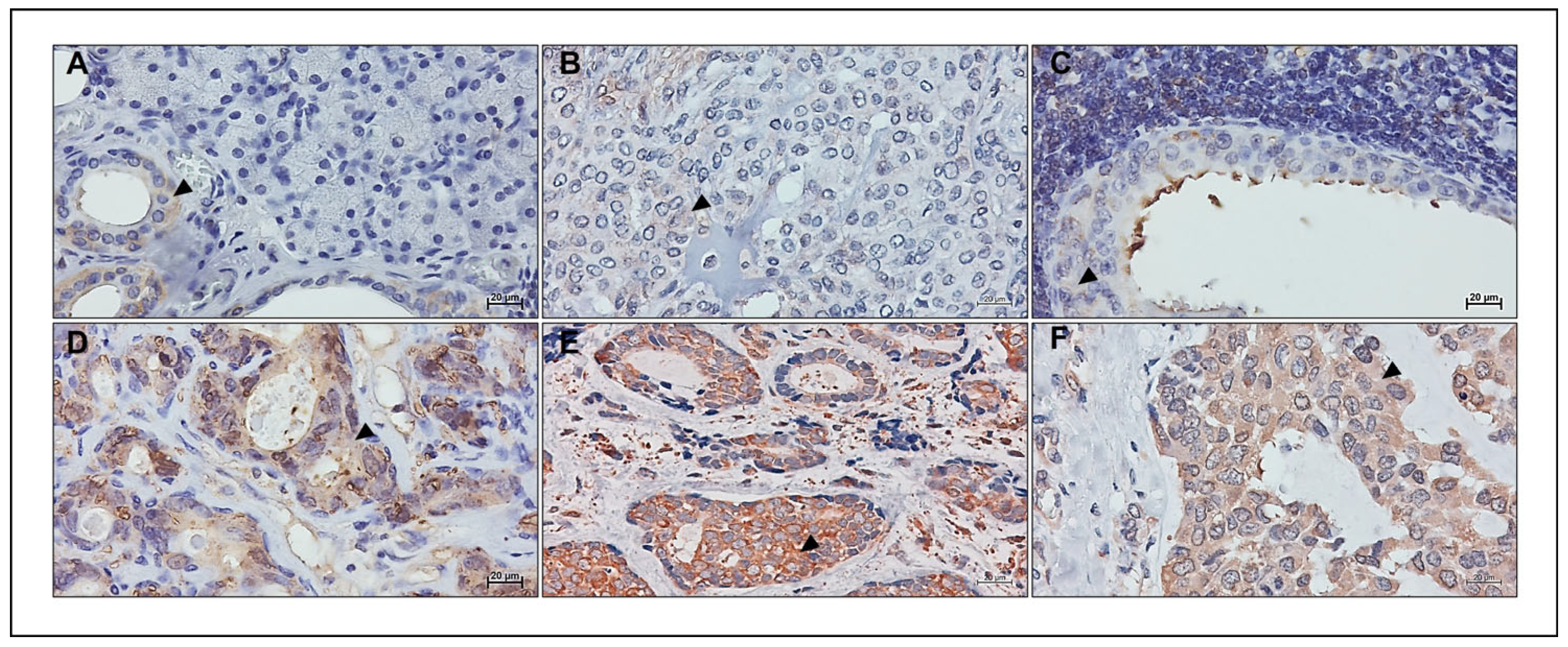
Figure 2.
Hsp90 tissue levels help discern between different physiological and pathological states of salivary glands. (A) Healthy tissue from the periphery of a Warthin’s tumor. Benign tumors pleomorphic adenoma (PA) (B) and Warthin’s tumor (WT) (C). Hsp90 tissue levels assessed by immunohistochemistry show the highest signal intensity and cellular positivity (arrowhead) in the malignant epithelial cells of mucoepidermoid carcinoma (MUC) (D), adenoid cystic carcinoma (ACC) (E), and ex-pleomorphic adenoma (EX-PA) (F) when compared with A, B, and C. Hsp90 levels confined to the ducts of healthy salivary glands show a higher positivity and intensity than the neoplastic epithelium of both PA and WT. Bar 20 µm. Image (B) was reproduced from Ref. [20] under the terms and conditions of the Creative Commons Attribution License (CC BY 4.0).
Hsp90 plays a major role in promoting the activity of the PI3K-Akt proliferation pathway and the NF-kB inflammatory pathway, both pathways being upregulated in cancer, Figure 3 [8]. Hsp90 inhibition in ACC has been assessed in vitro for its potential anti-cancer properties. Hsp90 inhibition via ganetespib, the most potent second generation Hsp90 inhibitor, diminished cellular viability, proliferation, and migration while exacerbating apoptosis [20]. Hsp90-targeted inhibition further altered the activation of PI3K-Akt and NF-kB pathways by up-regulating the activity of Akt and down-regulating NF-kB protein levels [20]. Although ganetespib promoted cytotoxicity in ACC cells via apoptosis, cleaved caspase-3 levels were not altered, suggesting that in this instance apoptosis may not be mediated through the mitochondrial pathway. Oncogenic kinases are intrinsically unstable [40]. Hsp90 interaction with its co-chaperone, Cdc37, is essential for the stabilization of the targeted kinases and is required for their oncogenic activity. C-myc is an oncogene prevalent in many cancers [40]. C-myc was expressed in vivo in rodents, using a mouse mammary tumor virus-c-myc (MMTV-c-myc) transgenic mouse model. Mammary adenocarcinomas formed after ectopic expression of c-myc [40]. The introduction of double transgenic MMTV-Cdc37/c-myc mice increased the number of mammary adenocarcinomas and simultaneously induced salivary gland adenocarcinomas formation [40]. Despite their anti-cancer effect, no Hsp90 inhibitor has yet been FDA approved, because they trigger a regulatory feedback loop in the form of a “heat shock response” (HSR) promoting cellular survival [41,42]. This brings the need for higher doses to maintain the inhibitory effect of the drug which is accompanied by increased toxicity. Efforts are being re-directed into exploring isoform-specific Hsp90 inhibition. This is expected to circumvent the drawback of HSR and potentially offer less toxicity than conventional Hsp90 “pan” inhibitors [41,43,44]. One of those drugs, Pimitespib (TAS-116), has recently entered phase III clinical trials [44]. Although, as this is a rather new area of research, more time is needed for novel drugs to be synthesized and tested. Isoform-specific Hsp90 inhibitors may prove to be potent drugs for cancer treatment, especially for salivary glands as chemotherapy in this case has not been effective.
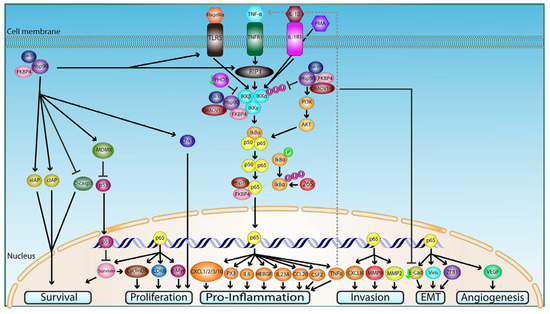
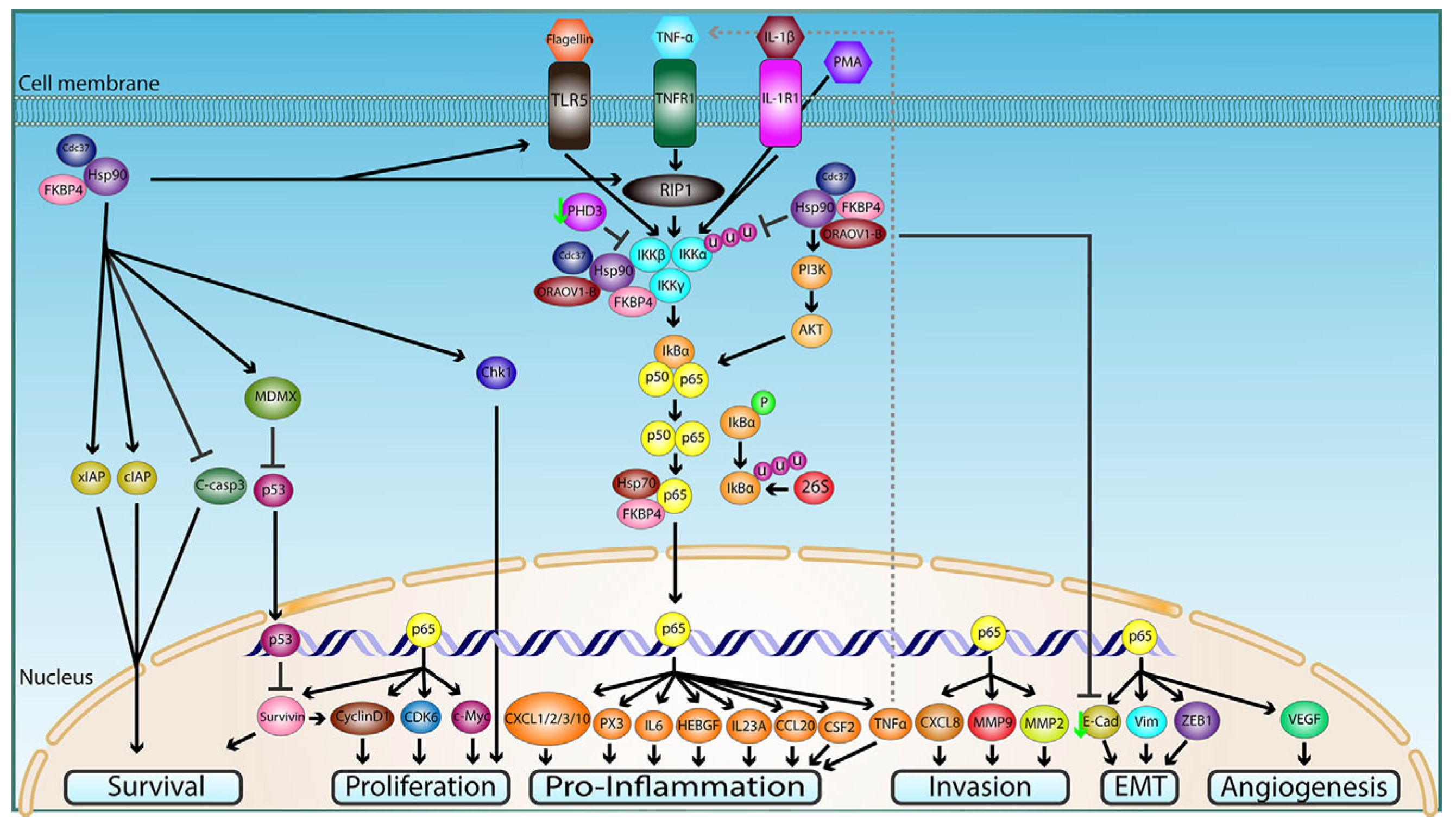
Figure 3.
Hsp90 molecular mechanisms and regulation of the NF-kB signaling pathway in cancer. This diagram captures the various signal transduction cascades through which Hsp90 modulates NF-kB activity in tumorous cells and tissue to promote growth, progression, invasion, and metastasization. For the detailed figure caption, please refer to Ref. [8]. This figure is reproduced from Ref. [8] under the terms and conditions of the Creative Commons Attribution License (CC BY 4.0).
As research in this field continues, a deeper understanding of the specific mechanisms by which Hsp90 influences salivary gland tumorigenesis is likely to emerge. Targeting Hsp90 and its associated signaling pathways may offer promising avenues for novel and targeted therapies to combat these rare tumors.
6. Conclusions
Diagnosis, treatment, and patient follow up of benign and malignant tumors, including those of the salivary glands discussed here, can now benefit from the advances in our understanding of the chaperone system (CS) and its participation in carcinogenesis. Differential patterns of expression of Hsp90 (a major component of the CS) in salivary gland tissue may be used in clinical pathology to discern between healthy, benign, and malignant specimens. Hsp90 tissue levels could be used by pathologists as markers to enhance diagnosis and identification of salivary gland tumors. Interaction of Hsp90 with another member of the CS, Cdc37, is emerging as a driving factor behind salivary gland tissue transformation and progression via stabilizing and activating oncogenic kinases.
Author Contributions
Conceptualization, C.A.B.; methodology, C.A.B.; software, C.A.B.; validation, I.H.H.; formal analysis, C.A.B.; investigation, C.A.B.; resources, C.A.B.; data curation, A.J.L.M. and E.C.d.M.; writing—original draft preparation, C.A.B. and A.L.; writing—review and editing, A.J.L.M. and E.C.d.M.; visualization, A.L.; supervision, A.R.J.; project administration, F.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Acknowledgments
A.J.L.M. and E.C.d.M. were partially supported by IEMEST and IMET.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Holmberg, K.V.; Hoffman, M.P. Anatomy, biogenesis and regeneration of salivary glands. Monogr. Oral Sci. 2014, 24, 1–13. [Google Scholar] [PubMed]
- Kessler, A.T.; Bhatt, A.A. Review of the Major and Minor Salivary Glands, Part 1: Anatomy, Infectious, and Inflammatory Processes. J. Clin. Imaging Sci. 2018, 8, 47. [Google Scholar] [CrossRef] [PubMed]
- Holsinger, F.C.; Bui, D.T. Anatomy, Function, and Evaluation of the Salivary Glands. In Salivary Gland Disorders; Myers, E.N., Ferris, R.L., Eds.; Springer: Berlin/Heidelberg, Germany, 2007; pp. 1–16. [Google Scholar]
- Gatta, G.; Guzzo, M.; Locati, L.D.; McGurk, M.; Prott, F.J. Major and minor salivary gland tumours. Crit. Rev. Oncol. Hematol. 2020, 152, 102959. [Google Scholar] [CrossRef] [PubMed]
- Radha, R.; John Blesswin, A.; Selva Mary, G. A Simple Innovative Approach DNA-Based Saliva Security System for User Authentication. Indian J. Sci. Technol. 2016, 9, 1–6. [Google Scholar] [CrossRef]
- Zolotukhin, S. Metabolic hormones in saliva: Origins and functions. Oral Dis. 2013, 19, 219–229. [Google Scholar] [CrossRef]
- Gröschl, M. The Physiological Role of Hormones in Saliva. BioEssays 2009, 31, 843–852. [Google Scholar] [CrossRef]
- Basset, C.A.; Conway de Macario, E.; Leone, L.G.; Macario, A.J.L.; Leone, A. The chaperone system in cancer therapies: Hsp90. J. Mol. Histol. 2023, 54, 105–118. [Google Scholar] [CrossRef]
- Lin, H.H.; Limesand, K.H.; Ann, D.K. Current State of Knowledge on Salivary Gland Cancers. Crit. Rev. Oncog. 2018, 23, 139–151. [Google Scholar] [CrossRef]
- Skálová, A.; Hyrcza, M.D.; Leivo, I. Update from the 5th Edition of the World Health Organization Classification of Head and Neck Tumors: Salivary Glands. Head Neck Pathol. 2022, 16, 40–53. [Google Scholar] [CrossRef]
- Guzzo, M.; Locati, L.D.; Prott, F.J.; Gatta, G.; McGurk, M.; Licitra, L. Major and minor salivary gland tumors. Crit. Rev. Oncol. Hematol. 2010, 74, 134–148. [Google Scholar] [CrossRef]
- Del Signore, A.G.; Megwalu, U.C. The Rising incidence of major salivary gland cancer in the United States. Ear Nose Throat J. 2017, 96, E13–E16. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Luo, Y.; Li, M.; Yan, H.; Sun, M.; Fan, T. Management of salivary gland carcinomas—A review. Oncotarget 2017, 8, 3946–3956. [Google Scholar] [CrossRef] [PubMed]
- Geiger, J.L.; Ismaila, N.; Beadle, B.; Caudell, J.J.; Chau, N.; Deschler, D.; Glastonbury, C.; Kaufman, M.; Lamarre, E.; Lau, H.Y.; et al. Management of Salivary Gland Malignancy: ASCO Guideline. J. Clin. Oncol. 2021, 39, 1909–1941. [Google Scholar] [CrossRef]
- Sood, S.; McGurk, M.; Vaz, F. Management of Salivary Gland Tumours: United Kingdom National Multidisciplinary Guidelines. J. Laryngol. Otol. 2016, 130, S142–S149. [Google Scholar] [CrossRef]
- Macario, A.J.L.; Conway de Macario, E. Chaperonins in Cancer: Expression, function, and migration in extracellular vesicles. Semin. Cancer Biol. 2022, 86, 26–35. [Google Scholar] [CrossRef] [PubMed]
- Macario, A.J.L.; Conway de Macario, E. Chaperone Proteins and Chaperonopathies. In Stress: Physiology, Biochemistry, and Pathology; Fink, G., Ed.; Academic Press: Cambridge, MA, USA, 2019; Volume 3, pp. 135–152. [Google Scholar] [CrossRef]
- Johnson, J.L. Mutations in Hsp90 Cochaperones Result in a Wide Variety of Human Disorders. Front. Mol. Biosci. 2021, 8, 787260. [Google Scholar] [CrossRef] [PubMed]
- Macario, A.J.L.; Conway de Macario, E. Sick chaperones, cellular stress, and disease. N. Engl. J. Med. 2005, 353, 1489–1501. [Google Scholar] [CrossRef]
- Basset, C.A.; Rappa, F.; Barone, R.; Florena, A.M.; Porcasi, R.; Conway de Macario, E.; Macario, A.J.L.; Leone, A. The Chaperone System in Salivary Glands: Hsp90 Prospects for Differential Diagnosis and Treatment of Malignant Tumors. Int. J. Mol. Sci. 2022, 23, 9317. [Google Scholar] [CrossRef]
- Basset, C.A.; Rappa, F.; Lentini, V.L.; Barone, R.; Pitruzzella, A.; Unti, E.; Cappello, F.; Conway de Macario, E.; Macario, A.J.L.; Leone, A. Hsp27 and Hsp60 in human submandibular salivary gland: Quantitative patterns in healthy and cancerous tissues with potential implications for differential diagnosis and carcinogenesis. Acta Histochem. 2021, 123, 151771. [Google Scholar] [CrossRef]
- Basset, C.A.; Cappello, F.; Rappa, F.; Lentini, V.L.; Jurjus, A.R.; Conway de Macario, E.; Macario, A.J.L.; Leone, A. Molecular Chaperones in Tumors of Salivary Glands. J. Mol. Histol. 2020, 51, 109–115. [Google Scholar] [CrossRef]
- Basset, C.A.; Cappello, F.; Rappa, F.; Jurjus, A.R.; Conway de Macario, E.; Macario, A.J.L.; Leone, A. Chaperonin Hsp60 and Cancer Therapies. In Heat Shock Proteins in Human Disease; Asea, A.A.A., Kaur, P., Eds.; Springer: Cham, Switzerland, 2020; Volume 21, pp. 31–52. [Google Scholar]
- Fouani, M.; Basset, C.A.; Mangano, G.D.; Leone, L.G.; Lawand, N.B.; Leone, A.; Barone, R. Heat Shock Proteins Alterations in Rheumatoid Arthritis. Int. J. Mol. Sci. 2022, 23, 2806. [Google Scholar] [CrossRef] [PubMed]
- Macario, A.J.L.; Conway de Macario, E. The chaperone system in autoimmunity, inflammation, and virus-induced diseases: Role of chaperonins. In Stress: Immunology and Inflammation; Fink, G., Ed.; Elsevier/Academic Press: San Diego, CA, USA, 2023; Volume 5, pp. 119–128. [Google Scholar]
- Caruso Bavisotto, C.; Cipolla, C.; Graceffa, G.; Barone, R.; Bucchieri, F.; Bulone, D.; Cabibi, D.; Campanella, C.; Marino Gammazza, A.; Pitruzzella, A.; et al. Immunomorphological Pattern of Molecular Chaperones in Normal and Pathological Thyroid Tissues and Circulating Exosomes: Potential Use in Clinics. Int. J. Mol. Sci. 2019, 20, 4496. [Google Scholar] [CrossRef]
- Rappa, F.; Sciume, C.; Lo Bello, M.; Caruso Bavisotto, C.; Marino Gammazza, A.; Barone, R.; Campanella, C.; David, S.; Carini, F.; Zarcone, F.; et al. Comparative analysis of Hsp10 and Hsp90 expression in healthy mucosa and adenocarcinoma of the large bowel. Anticancer Res. 2014, 34, 4153–4160. [Google Scholar] [PubMed]
- Barone, R.; Caruso Bavisotto, C.; Rappa, F.; Gargano, M.L.; Macaluso, F.; Paladino, L.; Vitale, A.M.; Alfano, S.; Campanella, C.; Gorska, M.; et al. JNK pathway and heat shock response mediate the survival of C26 colon carcinoma bearing mice fed with the mushroom Pleurotus eryngii Var. eryngii without affecting tumor growth or cachexia. Food Funct. 2021, 12, 3083–3095. [Google Scholar] [CrossRef]
- Gorska-Ponikowska, M.; Kuban-Jankowska, A.; Marino Gammazza, A.; Daca, A.; Wierzbicka, J.M.; Zmijewski, M.A.; Luu, H.H.; Wozniak, M.; Cappello, F. The Major Heat Shock Proteins, Hsp70 and Hsp90, in 2-Methoxyestradiol-Mediated Osteosarcoma Cell Death Model. Int. J. Mol. Sci. 2020, 21, 616. [Google Scholar] [CrossRef] [PubMed]
- Kamm, A.; Przychodzeń, P.; Kuban-Jankowska, A.; Marino Gammazza, A.; Cappello, F.; Daca, A.; Żmijewski, M.A.; Woźniak, M.; Górska-Ponikowska, M. 2-Methoxyestradiol and Its Combination with a Natural Compound, Ferulic Acid, Induces Melanoma Cell Death via Downregulation of Hsp60 and Hsp90. J. Oncol. 2019, 2019, 9293416. [Google Scholar] [CrossRef]
- Ansa-Addo, E.A.; Thaxton, J.; Hong, F.; Wu, B.X.; Zhang, Y.; Fugle, C.W.; Metelli, A.; Riesenberg, B.; Williams, K.; Gewirth, D.T.; et al. Clients and Oncogenic Roles of Molecular Chaperone gp96/grp94. Curr. Top. Med. Chem. 2016, 16, 2765–2778. [Google Scholar] [CrossRef]
- Chiu, C.C.; Lin, C.Y.; Lee, L.Y.; Chen, Y.J.; Lu, Y.C.; Wang, H.M.; Liao, C.T.; Chang, J.T.C.; Cheng, A.J. Molecular chaperones as a common set of proteins that regulate the invasion phenotype of head and neck cancer. Clin. Cancer Res. 2011, 17, 4629–4641. [Google Scholar] [CrossRef]
- Chen, Y.; Chen, C.; Ma, C.; Sun, S.; Zhang, J.; Sun, Y. Expression of heat-shock protein gp96 in gallbladder cancer and its prognostic clinical significance. Int. J. Clin. Exp. Pathol. 2015, 8, 1946–1953. [Google Scholar]
- Feng, J.; Xie, G.; Zhan, Y.; Lu, J.; Xu, L.; Fan, S.; Wang, W. Elevated HSP90 associates with expression of HIF-1α and p-AKT and is predictive of poor prognosis in nasopharyngeal carcinoma. Histopathology 2019, 75, 202–212. [Google Scholar] [CrossRef]
- Maddalena, F.; Simeon, V.; Vita, G.; Bochicchio, A.; Possidente, L.; Sisinni, L.; Lettini, G.; Condelli, V.; Matassa, D.S.; Li Bergolis, V.; et al. TRAP1 protein signature predicts outcome in human metastatic colorectal carcinoma. Oncotarget 2017, 8, 21229–21240. [Google Scholar] [CrossRef] [PubMed]
- Pick, E.; Kluger, Y.; Giltnane, J.M.; Moeder, C.; Camp, R.L.; Rimm, D.L.; Kluger, H.M. High HSP90 expression is associated with decreased survival in breast cancer. Cancer Res. 2007, 67, 2932–2937. [Google Scholar] [CrossRef] [PubMed]
- Zagouri, F.; Sergentanis, T.; Nonni, A.; Papadimitriou, C.; Pazaiti, A.; Michalopoulos, N.V.; Safioleas, P.; Lazaris, A.; Theodoropoulos, G.; Patsouris, E.; et al. Decreased Hsp90 expression in infiltrative lobular carcinoma: An immunohistochemical study. BMC Cancer 2010, 10, 409. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.; Gu, X.; Chen, L.; Wang, Y.; Cao, B.; Qun, E. Comparison of the expression of 5 heat shock proteins in benign and malignant salivary gland tumor tissues. Oncol. Lett. 2013, 5, 1363–1369. [Google Scholar] [CrossRef]
- Shigeishi, H.; Sugiyama, M.; Tahara, H.; Ono, S.; Bhawal, U.K.; Okura, M.; Kogo, M.; Shinohara, M.; Shindoh, M.; Shintani, S.; et al. Increased telomerase activity and hTERT expression in human salivary gland carcinomas. Oncol. Lett. 2011, 2, 845–850. [Google Scholar] [CrossRef]
- Stepanova, L.; Finegold, M.; DeMayo, F.; Schmidt, E.V.; Harper, J.W. The oncoprotein kinase chaperone CDC37 functions as an oncogene in mice and collaborates with Both c-Myc and cyclin D1 in transformation of multiple tissues. Mol. Cell Biol. 2000, 20, 4462–4473. [Google Scholar] [CrossRef]
- Sanchez, J.; Carter, T.R.; Cohen, M.S.; Blagg, B.S.J. Old and New Approaches to Target the Hsp90 Chaperone. Curr. Cancer Drug Targets 2019, 20, 253–270. [Google Scholar] [CrossRef]
- Wang, L.; Zhang, L.; Li, L.; Jiang, J.; Zheng, Z.; Shang, J.; Wang, C.; Chen, W.; Bao, Q.; Xu, X.; et al. Small-molecule inhibitor targeting the Hsp90-Cdc37 protein-protein interaction in colorectal cancer. Sci. Adv. 2019, 5, eaax2277. [Google Scholar] [CrossRef]
- Blair, L.J.; Genest, O.; Mollapour, M. The multiple facets of the Hsp90 machine. Nat. Struct. Mol. Biol. 2019, 26, 92–95. [Google Scholar] [CrossRef]
- Honma, Y.; Kurokawa, Y.; Sawaki, A.; Naito, Y.; Iwagami, S.; Baba, H.; Komatsu, Y.; Nishida, T.; Doi, T. Randomized, double-blind, placebo (PL)-controlled, phase III trial of pimitespib (TAS-116), an oral inhibitor of heat shock protein 90 (HSP90), in patients (Pts) with advanced gastrointestinal stromal tumor (GIST) refractory to imatinib (IM), sunitinib (SU) and regorafenib (REG). J. Clin. Oncol. 2021, 39, 11524. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).