Effects of Strength Training Assessed by Anthropometry and Muscle Ultrasound
Abstract
1. Introduction
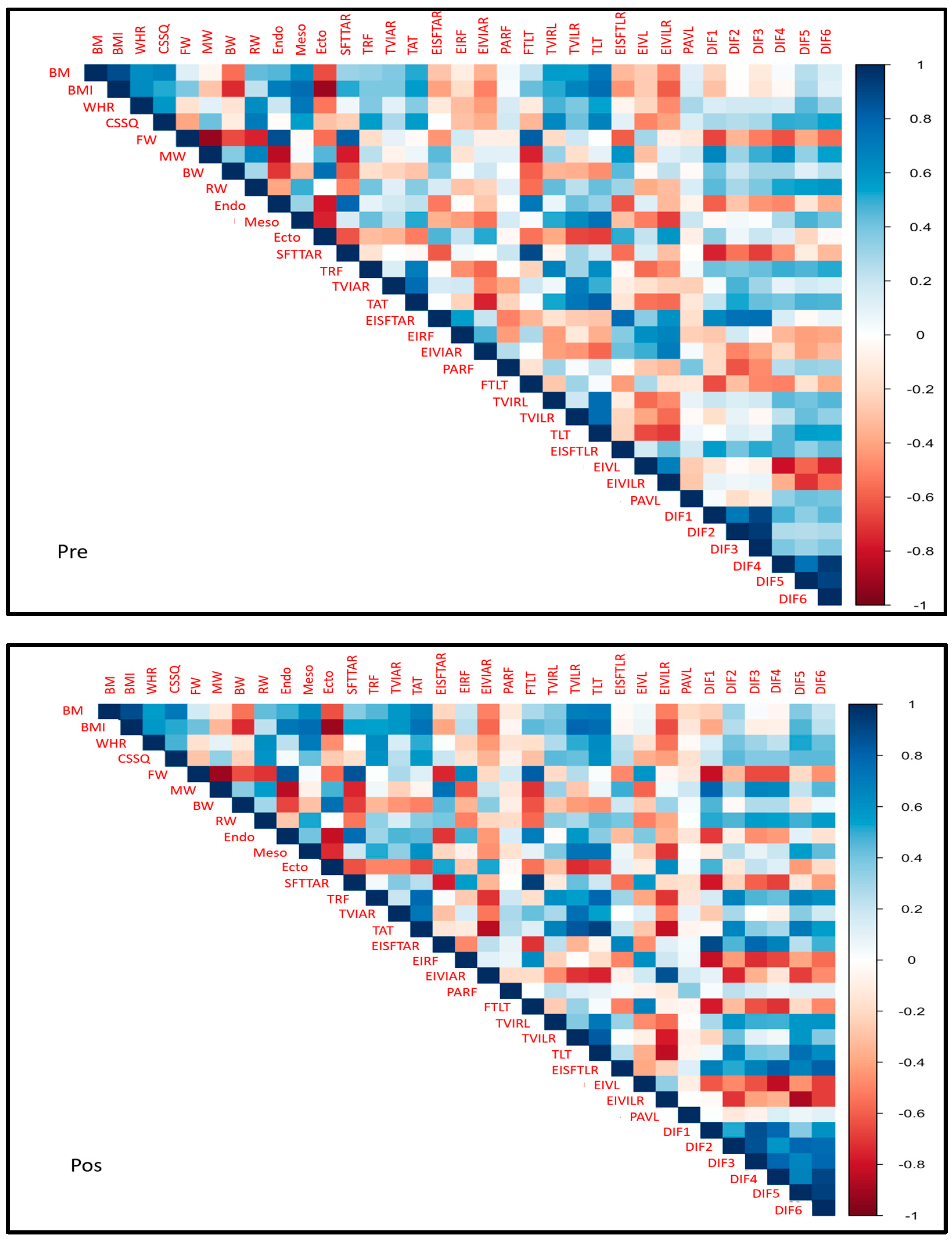
2. Results
3. Discussion
4. Materials and Methods
4.1. Participants
4.2. Procedure
4.3. Strength Training
4.4. Anthropometric Measurements
4.5. Description of the Taking of the Main Anthropometric Measurements
4.6. Ultrasound Measurements
4.7. Statistical Analysis
5. Conclusions
5.1. Limitations
5.2. Suggestions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| 1RM | One-repetition maximum |
| BM | Body mass |
| BMI | Body mass index |
| BW | Bone weight |
| CSSQ | Cross-sectional section of the quadriceps |
| DAM | Median absolute deviation |
| Dif1 | Anterior fat EI minus RF EI |
| Dif2 | Anterior fat EI minus anterior VI EI |
| Dif3 | Anterior fat EI minus the average of RF EI + anterior VI EI |
| Dif4 | Lateral fat EI minus VL EI |
| Dif5 | Anterior fat EI minus lateral VI EI |
| Dif6 | Lateral fat EI minus the average of VL EI + lateral VI EI |
| Ecto | Ectomorphy |
| EI | Echo-intensity |
| EIRF | EI of the RF |
| EISFTAR | EI of subcutaneous fat tissue in the anterior region |
| EISFTLR | EI of subcutaneous fat tissue in the lateral region |
| EIVIAR | EI of the VI in the anterior region |
| EIVILR | EI of the VI in the lateral region |
| EIVL | EI of the VL |
| Endo | Endomorphy |
| FTLT | Fat thickness in the lateral region |
| FW | Fat weight |
| M | Mean |
| Meso | Mesomorphy |
| MRI | Magnetic resonance imaging |
| MW | Muscle weight |
| n | Sample size |
| PARF | Pennation angle of the RF |
| PAVL | Pennation angle of the VL |
| RW | Residual weight |
| SD | Standard deviation |
| SFTTAR | Subcutaneous fat tissue thickness in the anterior region |
| T | Tomography |
| TAT | Total anterior thickness |
| TLT | Total lateral thickness |
| TRF | Thickness of the RF |
| TVIAR | Thickness of the VI in the anterior region |
| TVILR | Thickness of the VI in the lateral region |
| TVL | Thickness of the VL |
| US | Ultrasound |
| WHO | World Health Organization |
| WHR | Waist-to-hip ratio |
References
- Hyde, P.N.; Kendall, K.L.; Fairman, C.M.; Coker, N.A.; Yarbrough, M.E.; Rossi, S.J. Use of B-Mode Ultrasound as a Body Fat Estimate in Collegiate Football Players. J. Strength Cond. Res. 2016, 30, 3525–3530. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sarto, F.; Spörri, J.; Fitze, D.P.; Quinlan, J.I.; Narici, M.V.; Franchi, M.V. Implementing Ultrasound Imaging for the Assessment of Muscle and Tendon Properties in Elite Sports: Practical Aspects, Methodological Considerations and Future Directions. Sports Med. 2021, 51, 1151–1170. [Google Scholar] [CrossRef]
- Budzynski-Seymour, E.; Fisher, J.; Giessing, J.; Gentil, P.; Steele, J. Relationships and Comparative Reliability of Ultrasound Derived Measures of Upper and Lower Limb Muscle Thickness and Estimates of Muscle Area from Anthropometric Measures. SportRxiv 2019. preprint. [Google Scholar] [CrossRef]
- Sizoo, D.; de Heide, L.J.M.; Emous, M.; van Zutphen, T.; Navis, G.; van Beek, A.P. Measuring Muscle Mass and Strength in Obesity: A Review of Various Methods. Obes. Surg. 2021, 31, 384–393. [Google Scholar] [CrossRef] [PubMed]
- Bazzocchi, A.; Filonzi, G.; Ponti, F.; Albisinni, U.; Guglielmi, G.; Battista, G. Ultrasound: Which role in body composition? Eur. J. Radiol. 2016, 85, 1469–1480. [Google Scholar] [CrossRef]
- Fischer, A.; Anwar, M.; Hertwig, A.; Hahn, R.; Pesta, M.; Timmermann, I.; Siebenrock, T.; Liebau, K.; Hiesmayr, M. Ultrasound method of the USVALID study to measure subcutaneous adipose tissue and muscle thickness on the thigh and upper arm: An illustrated step-by-step guide. Clin. Nutr. Exp. 2020, 32, 38–73. [Google Scholar] [CrossRef]
- Harris-Love, M.O.; Seamon, B.A.; Teixeira, C.; Ismail, C. Ultrasound estimates of muscle quality in older adults: Reliability and comparison of Photoshop and ImageJ for the grayscale analysis of muscle echogenicity. PeerJ 2016, 4, e1721. [Google Scholar] [CrossRef] [PubMed]
- Hill, J.C.; San Millán, I. Validation of Musculoskeletal Ultrasound to Assess and Quantify Muscle Glycogen Content. A Novel Approach. Phys. Sportsmed. 2014, 42, 45–52. [Google Scholar] [CrossRef]
- Moreno Pascual, C.; Manonelles Marqueta, P.; Federación Española de Medicina del Deporte. Manual de Cineantropometría; Nexus Médica: Badalona, Spain, 2011. [Google Scholar]
- American College of Sports Medicine. ACSM´s Guidelines for Exercise Testing and Prescription; Williams & Wilkins: Philadelphia, PA, USA, 2000. [Google Scholar]
- Housh, D.J.; Housh, T.J.; Weir, J.P.; Weir, L.L.; Johnson, G.O.; Stout, J.R. Anthropometric estimation of thigh muscle cross-sectional area. Med. Sci. Sports Exerc. 1995, 27, 784–791. [Google Scholar] [CrossRef]
- Atencia Pérez, E.A.; Ricardo Paternina, D.A.; Vergara Villa, J.D. Relación del Nivel de Actividad Física con Variables Asociadas a la Composición Corporal en Estudiantes de Primer Ingreso del Programa Ciencias del Deporte y la Actividad Física; CECAR—Corporación Universitaria del Caribe: Sincelejo, Colombia, 2021; Available online: https://repositorio.cecar.edu.co/server/api/core/bitstreams/4e9b459a-0067-4217-b5cf-46587f95a879/content (accessed on 9 March 2025).
- Aravena-Sagardia, P.; García-Sandoval, A.; Herrera-Valenzuela, T.; Magnani Branco, B.; Vargas-Vitoria, R.; Valdés-Badilla, P. Efectos de un programa de entrenamiento muscular sobre la composición corporal y fuerza máxima en estudiantes universitarios según su índice de masa corporal inicial. Nutr. Clínica Y Dietética Hosp. 2021, 41, 194–200. [Google Scholar] [CrossRef]
- Cardozo, L.C. Body fat percentage and prevalence of overweight—Obesity in college students of sports performance in Bogotá, Colombia. Nutr. Clínica Y Dietética Hosp. 2016, 36, 68–75. [Google Scholar] [CrossRef]
- Pirazán Rodríguez, M.J.; Pirazán Rodríguez, M.J.; Rivera Santisteban, M.E.; Anzola Martínez, F. Efectos de un programa de entrenamiento concurrente sobre el perfil antropométrico y la fuerza muscular en un grupo de jóvenes universitarios. Rev. Digit. Act. Física Y Deporte 2020, 6, 14–31. [Google Scholar] [CrossRef]
- Coratella, G.; Beato, M.; Milanese, C.; Longo, S.; Limonta, E.; Rampichini, S.; Cè, E.; Bisconti, A.V.; Schena, F.; Esposito, F. Specific Adaptations in Performance and Muscle Architecture After Weighted Jump-Squat vs. Body Mass Squat Jump Training in Recreational Soccer Players. J. Strength Cond. Res. 2018, 32, 921–929. [Google Scholar] [CrossRef]
- Correa, C.S.; LaRoche, D.P.; Cadore, E.L.; Reischak-Oliveira, A.; Bottaro, M.; Kruel, L.M.; Tartaruga, M.P.; Radaelli, R.; Wilhelm, E.N.; Lacerda, F.C.; et al. 3 Different Types of Strength Training in Older Women. Int. J. Sports Med. 2012, 33, 962–969. [Google Scholar] [CrossRef]
- Franchi, M.V.; Monti, E.; Carter, A.; Quinlan, J.I.; Herrod, P.J.J.; Reeves, N.D.; Narici, M.V. Bouncing Back! Counteracting Muscle Aging with Plyometric Muscle Loading. Front. Physiol. 2019, 10, 178. [Google Scholar] [CrossRef]
- Simó-Servat, A.; Ibarra, M.; Libran, M.; Escobar, L.; Perea, V.; Quirós, C.; Puig-Jové, C.; Barahona, M.-J. Prospective Study to Evaluate Rectus Femoris Muscle Ultrasound for Body Composition Analysis in Patients Undergoing Bariatric Surgery. J. Clin. Med. 2024, 13, 3763. [Google Scholar] [CrossRef] [PubMed]
- Simó-Servat, A.; Ibarra, M.; Libran, M.; Quirós, C.; Puértolas, N.; Alonso, N.; Perea, V.; Simó, R.; Barahona, M. Usefulness of Ultrasound in Assessing the Impact of Bariatric Surgery on Body Composition: A Pilot Study. Obes. Surg. 2023, 33, 1211–1217. [Google Scholar] [CrossRef]
- Rustani, K.; Kundisova, L.; Capecchi, P.L.; Nante, N.; Bicchi, M. Ultrasound measurement of rectus femoris muscle thickness as a quick screening test for sarcopenia assessment. Arch. Gerontol. Geriatr. 2019, 83, 151–154. [Google Scholar] [CrossRef]
- Mechelli, F.; Arendt-Nielsen, L.; Stokes, M.; Agyapong-Badu, S. Validity of Ultrasound Imaging Versus Magnetic Resonance Imaging for Measuring Anterior Thigh Muscle, Subcutaneous Fat, and Fascia Thickness. Methods Protoc. 2019, 2, 58. [Google Scholar] [CrossRef]
- Prado, C.M.M.; Heymsfield, S.B. Lean Tissue Imaging. J. Parenter. Enter. Nutr. 2014, 38, 940–953. [Google Scholar] [CrossRef]
- Pineau, J.C.; Bouslah, M. Prediction of body fat in male athletes from ultrasound and anthropometric measurements versus DXA. J. Sports Med. Phys. Fit. 2020, 60, 251–256. [Google Scholar] [CrossRef]
- Miclos-Balica, M.; Muntean, P.; Schick, F.; Haragus, H.G.; Glisici, B.; Pupazan, V.; Neagu, A.; Neagu, M. Reliability of body composition assessment using A-mode ultrasound in a heterogeneous sample. Eur. J. Clin. Nutr. 2021, 75, 438–445. [Google Scholar] [CrossRef] [PubMed]
- Stock, M.S.; Thompson, B.J. Echo intensity as an indicator of skeletal muscle quality: Applications, methodology, and future directions. Eur. J. Appl. Physiol. 2021, 121, 369–380. [Google Scholar] [CrossRef]
- Bali, A.U.; Harmon, K.K.; Burton, A.M.; Phan, D.C.; Mercer, N.E.; Lawless, N.W.; Stock, M.S. Muscle strength, not age, explains unique variance in echo intensity. Exp. Gerontol. 2020, 139, 111047. [Google Scholar] [CrossRef] [PubMed]
- Wong, V.; Spitz, R.W.; Bell, Z.W.; Viana, R.B.; Chatakondi, R.N.; Abe, T.; Loenneke, J.P. Exercise induced changes in echo intensity within the muscle: A brief review. J. Ultrasound 2020, 23, 457–472. [Google Scholar] [CrossRef]
- Vasenina, C.; Kataoka, R.; Hammert, W.B.; Ibrahim, A.H.; Dankel, S.J.; Buckner, S.L. Examination of Changes in Echo Intensity Following Resistance Exercise among Various Regions of Interest. Clin. Physiol. Funct. Imaging 2022, 42, 23–28. [Google Scholar] [CrossRef]
- Schoenfeld, B.J. The Mechanisms of Muscle Hypertrophy and Their Application to Resistance Training. J. Strength Cond. Res. 2010, 24, 2857–2872. [Google Scholar] [CrossRef]
- Wernbom, M.; Augustsson, J.; Thomeé, R. The Influence of Frequency, Intensity, Volume and Mode of Strength Training on Whole Muscle Cross-Sectional Area in Humans. Sports Med. 2007, 37, 225–264. [Google Scholar] [CrossRef] [PubMed]
- Schoenfeld, B.J. Science and Development of Muscle Hypertrophy; Human Kinetics: New York, NY, USA, 2020. [Google Scholar]
- Suchomel, T.J.; Nimphius, S.; Stone, M.H. The Importance of Muscular Strength in Athletic Performance. Sports Med. 2016, 46, 1419–1449. [Google Scholar] [CrossRef]
- Franchi, M.V.; Reeves, N.D.; Narici, M.V. Skeletal Muscle Remodeling in Response to Eccentric vs. Concentric Loading: Morphological, Molecular, and Metabolic Adaptations. Front. Physiol. 2017, 8, 447. [Google Scholar] [CrossRef]
- Proske, U.; Morgan, D.L. Muscle damage from eccentric exercise: Mechanism, mechanical signs, adaptation and clinical applications. J. Physiol. 2001, 537, 333–345. [Google Scholar] [CrossRef] [PubMed]
- Kraemer, W.J.; Ratamess, N.A. Fundamentals of Resistance Training: Progression and Exercise Prescription. Med. Sci. Sports Exerc. 2004, 36, 674–688. [Google Scholar] [CrossRef]
- Zatsiorsky, V.M.; Kraemer, W.J.; Fry, A.C. Science and Practice of Strength Training; Human Kinetics: New York, NY, USA, 2020. [Google Scholar]
- Benavides-Villanueva, J.; Ramirez-Campillo, R. Entrenamiento con sobrecarga, duración de la repetición e hipertrofia: Una revisión de la literatura. Rev. Cienc. De La Act. Física 2022, 23, 1–13. [Google Scholar] [CrossRef]
- Wilk, M.; Gepfert, M.; Krzysztofik, M.; Golas, A.; Mostowik, A.; Maszczyk, A.; Zajac, A. The Influence of Grip Width on Training Volume During the Bench Press with Different Movement Tempos. J. Hum. Kinet. 2019, 68, 49–57. [Google Scholar] [CrossRef] [PubMed]
- Mazzetti, S.A.; Kraemer, W.J.; Volek, J.S.; Duncan, N.D.; Ratamess, N.A.; Gomez, A.L.; Newton, R.U.; Hakkinen, K.; Fleck, S.J. The influence of direct supervision of resistance training on strength performance. Med. Sci. Sports Exerc. 2000, 32, 1175–1184. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Waist Circumference and Waist-Hip Ratio: Report of a WHO Expert Consultation; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Zermeño-Ugalde, P.; Gallegos-García, V.; Ramírez, R.A.C.; Gaytán-Hernández, D. Relación del índice cintura-estatura (ICE) con circunferencia cintura e índice de cintura cadera como predictor para obesidad y riesgo metabólico en adolescentes de secundaria. Rev. Salud Pública Nutr. 2020, 19, 19–27. [Google Scholar]
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic; Report of a WHO consultation; World Health Organization Technical Report Series; WHO: Geneva, Switzerland, 2000; Volume 894, p. i253. [Google Scholar]
- Young, H.; Jenkins, N.T.; Zhao, Q.; Mccully, K.K. Measurement of intramuscular fat by muscle echo intensity. Muscle Nerve 2015, 52, 963–971. [Google Scholar] [CrossRef]
- Wu, J.S.; Darras, B.T.; Rutkove, S.B. Assessing spinal muscular atrophy with quantitative ultrasound. Neurology 2010, 75, 526–531. [Google Scholar] [CrossRef]
| Descriptive Statistics | Data |
|---|---|
| n 1 | 31 |
| Age (years) (M ± SD) 1 | 22.3 ± 4.14 |
| Height (meters) (M ± SD) 1 | 1.73 ± 0.08 |
| Body Mass (Kg)(Mediana ± DAM) 1 | 69 ± 13.64 |
| BMI (Kg/m2) (Mediana ± DAM) 1 | 23.54 ± 3.34 |
| Anthropometry (% Fat) | Pre- n (%) | Post- n (%) | p-Value |
|---|---|---|---|
| Media | 21 (67.74) | 14 (45.16) | 0.0302 1 |
| Good | 1 (3.2) | 7 (22.6) | |
| Excellent | 9 (29.03) | 10 (32.25) | |
| Total | 31 (100) | 31 (100) |
| Anthropometry | Before | After | p Value * | Size of the Effect | ||
|---|---|---|---|---|---|---|
| Medium | DAM | Medium | DAM | |||
| BM | 69.00 | 13.64 | 70.00 | 13.34 | 0.27 | 0.19 |
| BMI | 23.54 | 3.34 | 23.13 | 3.76 | 0.27 | 0.19 |
| WHR | 0.82 | 0.06 | 0.83 | 0.04 | 0.78 | 0.051 |
| CSSQ | 74.88 | 7.61 | 72.24 | 10.16 | 0.05 | 0.34 |
| FW | 14.04 | 5.84 | 14.25 | 5.92 | 0.21 | 0.22 |
| MW | 46.49 | 4.05 | 46.27 | 4.12 | 0.39 | 0.15 |
| BW | 15.53 | 2.42 | 15.66 | 2.27 | 0.26 | 0.20 |
| RW | 24.10 | 0.00 | 24.10 | 0.00 | n.a. | n.a. |
| Endo | 5.30 | 1.33 | 5.50 | 1.78 | 0.13 | 0.27 |
| Meso | 4.70 | 1.63 | 4.80 | 1.48 | 0.47 | 0.13 |
| Ecto | 1.80 | 1.48 | 1.90 | 1.48 | 0.29 | 0.19 |
| Ultrasound | Medium | DAM | Medium | DAM | p Value * | Size of the Effect |
|---|---|---|---|---|---|---|
| Pre | Post | |||||
| SFTTAR | 5.120 | 3.050 | 5.690 | 3.560 | 0.827 | 0.041 |
| TRF | 25.930 | 4.050 | 27.370 | 5.460 | 0.004 ** | 0.500 |
| TVIAR | 20.450 | 2.940 | 21.000 | 3.460 | 0.158 | 0.255 |
| TAT | 48.060 | 6.910 | 49.080 | 7.410 | 0.005 ** | 0.484 |
| EISFTAR | 155.220 | 17.010 | 157.160 | 11.970 | 0.111 | 0.289 |
| EIRF | 116.290 | 18.160 | 112.050 | 9.610 | 0.182 | 0.243 |
| EIVIA | 90.050 | 15.880 | 90.380 | 13.670 | 0.999 | 0.000 |
| PARF | 15.120 | 4.560 | 17.000 | 2.620 | 0.055 | 0.345 |
| FTLT | 5.060 | 3.230 | 5.600 | 3.290 | 0.812 | 0.044 |
| TVL | 24.320 | 4.180 | 25.120 | 4.040 | 0.035 * | 0.377 |
| TVILR | 20.400 | 4.630 | 19.510 | 4.370 | 0.820 | 0.042 |
| TLT | 47.590 | 7.990 | 48.580 | 6.520 | 0.003 ** | 0.516 |
| EISFTLR | 151.590 | 10.900 | 155.480 | 9.980 | 0.135 | 0.271 |
| EIVL | 119.740 | 18.020 | 117.390 | 10.780 | 0.157 | 0.257 |
| EIVILR | 78.470 | 14.620 | 80.030 | 19.120 | 0.399 | 0.155 |
| PAVL | 16.130 | 3.590 | 15.650 | 3.190 | 0.961 | 0.011 |
| Dif1 | 33.000 | 15.540 | 41.170 | 18.320 | <0.0001 ** | 0.686 |
| Dif2 | 67.170 | 15.400 | 71.730 | 21.280 | 0.224 | 0.222 |
| Dif3 | 49.110 | 14.060 | 55.630 | 13.730 | 0.002 ** | 0.524 |
| Dif4 | 30.780 | 24.940 | 37.920 | 19.890 | 0.001 ** | 0.560 |
| Dif5 | 79.520 | 13.800 | 84.100 | 23.020 | 0.854 | 0.035 |
| Dif6 | 56.650 | 19.270 | 59.770 | 21.540 | 0.157 | 0.257 |
| Stage | Days | % 1RM | Series | Repetitions | Reference |
|---|---|---|---|---|---|
| 1 | 1–6 | 60–70 | 4–5 | 10–12 | Bompa and Carrera (2015) [16] |
| 2 | 7–9 | 70–80% | 4–5 | 8–10 | Schoenfeld (2010) [8] |
| 3 | 10–12 | 80–90% | 5–6 | 5–6 | Zatsiorsky and Kraemer (2020) [15] |
| 4 | 13–18 * | 85–95% | 4–5 | 4–5 | Verkhoshansky (2009) [17] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giraldo García, J.C.; Ruiz Rengifo, G.M.; Cardona Nieto, D.; Echeverri Chica, J.; Arcila Arango, J.C.; Campuzano Zuluaga, G.; Ramos-Álvarez, O. Effects of Strength Training Assessed by Anthropometry and Muscle Ultrasound. Muscles 2025, 4, 11. https://doi.org/10.3390/muscles4020011
Giraldo García JC, Ruiz Rengifo GM, Cardona Nieto D, Echeverri Chica J, Arcila Arango JC, Campuzano Zuluaga G, Ramos-Álvarez O. Effects of Strength Training Assessed by Anthropometry and Muscle Ultrasound. Muscles. 2025; 4(2):11. https://doi.org/10.3390/muscles4020011
Chicago/Turabian StyleGiraldo García, Juan Carlos, Gloria María Ruiz Rengifo, Donaldo Cardona Nieto, Julián Echeverri Chica, Juan Cancio Arcila Arango, German Campuzano Zuluaga, and Oliver Ramos-Álvarez. 2025. "Effects of Strength Training Assessed by Anthropometry and Muscle Ultrasound" Muscles 4, no. 2: 11. https://doi.org/10.3390/muscles4020011
APA StyleGiraldo García, J. C., Ruiz Rengifo, G. M., Cardona Nieto, D., Echeverri Chica, J., Arcila Arango, J. C., Campuzano Zuluaga, G., & Ramos-Álvarez, O. (2025). Effects of Strength Training Assessed by Anthropometry and Muscle Ultrasound. Muscles, 4(2), 11. https://doi.org/10.3390/muscles4020011








