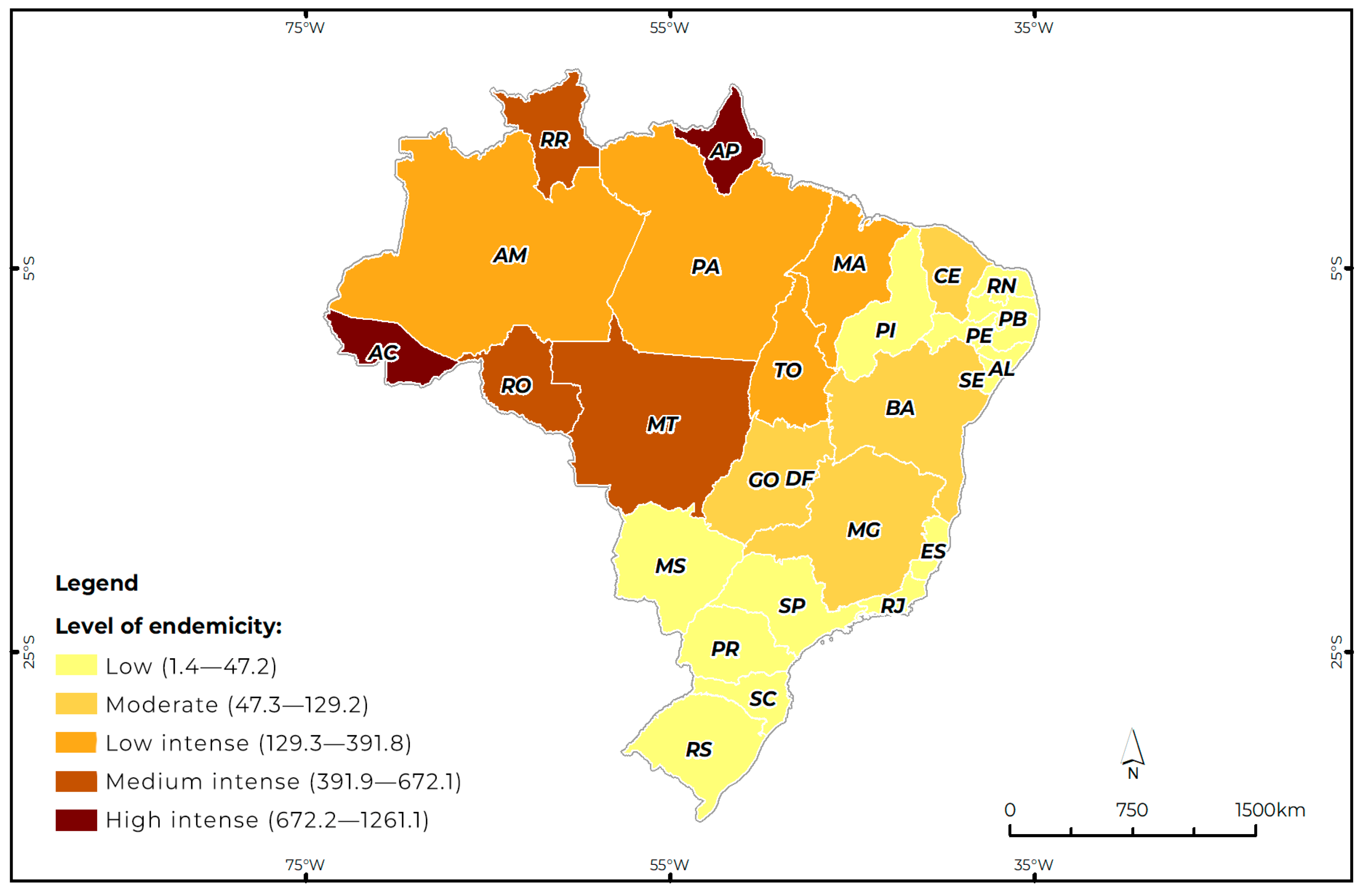
Different Levels of Endemicity of Cutaneous Leishmaniasis in Brazil
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Location
2.3. Data Source
2.4. Variables Used
- (a)
- Municipality of notification;
- (b)
- State of notification;
- (c)
- Sex (male/female);
- (d)
- Ethnicity (brown/white/black/indigenous/Asian/ignored);
- (e)
- Level of education (illiterate, incomplete 1st to 4th grade of elementary school, complete 4th grade of elementary school, incomplete 5th to 8th grade of elementary school, complete elementary school, incomplete high school, complete high school, incomplete higher education, complete higher education, not applicable, ignored);
- (f)
- Age group (under 1 year, 1 to 4 years, 5 to 9 years, 10 to 14 years, 15 to 19 years, 20 to 39 years, 40 to 59 years, 60 to 64 years, and over 65 years);
- (g)
- Gestational condition (yes, no, ignored).
- (a)
- Month of notification (January, February, March, April, May, June, July, August, September, October, November, December);
- (b)
- Year of notification (2014, 2015, 2016, 2017, 2018, 2019, 2020, 2021, 2022, 2023, 2024);
- (c)
- Confirmation criterion (laboratory, clinical-epidemiological);
- (d)
- Clinical form (cutaneous, mucosal).
2.5. Procedures Used
2.6. Data Analysis
2.7. Ethical Considerations
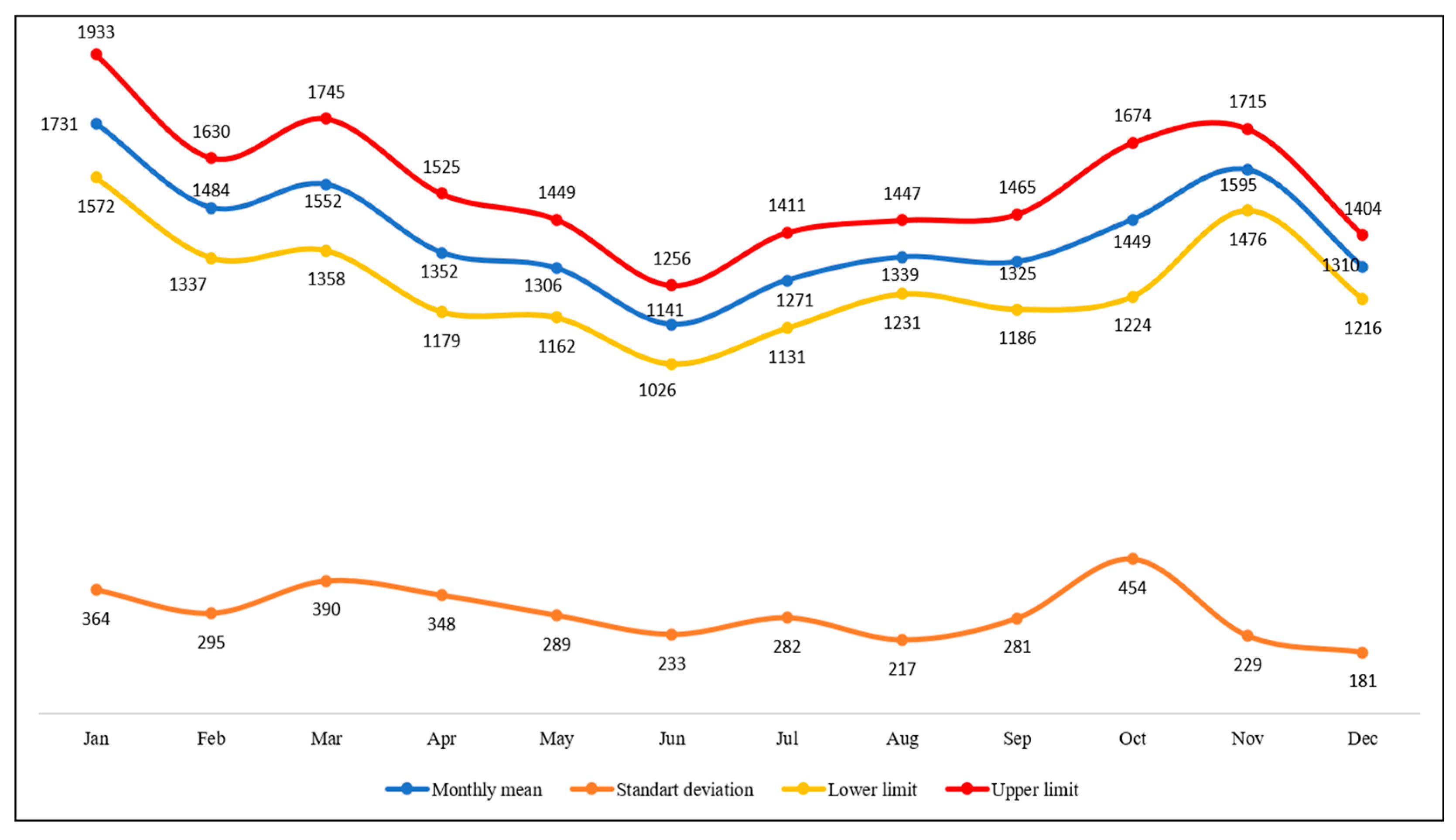
3. Results
4. Discussion
5. Conclusions and Recommendations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rangel, E.F.; Lainson, R. Proven and putative vectors of American cutaneous leishmaniasis in Brazil: Aspects of their biology and vectorial competence. Mem. Inst. Oswaldo Cruz 2009, 104, 937–954. [Google Scholar] [CrossRef]
- Anversa, L.; Tiburcio, M.G.S.; Richini-Pereira, V.B.; Ramirez, L.E. Human leishmaniasis in Brazil: A general review. Rev. Assoc. Med. Bras. 2018, 64, 281–289. [Google Scholar] [CrossRef]
- Silva, A.F.; Latorre, M.R.D.O.; Galati, E.A.B. Fatores relacionados à ocorrência de leishmaniose tegumentar no Vale do Ribeira. Rev. Soc. Bras. Med. Trop. 2010, 43, 46–51. [Google Scholar] [CrossRef] [PubMed]
- Mann, S.; Frasca, K.; Scherrer, S.; Henao-Martínez, A.F.; Newman, S.; Ramanan, P.; Suarez, J.A. A Review of Leishmaniasis: Current Knowledge and Future Directions. Curr. Trop. Med. Rep. 2021, 8, 121–132. [Google Scholar] [CrossRef]
- Hotez, P.J.; Woc-Colburn, L.; Bottazzi, M.E. Neglected tropical diseases in Central America and Panama: Review of their prevalence, populations at risk and impact on regional development. Int. J. Parasitol. 2014, 44, 597–603. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Chan, J.V.; Valenzuela, J.; Dumonteil, E. Leishmaniasis in the Americas. In Neglected Tropical Diseases—Latin America and the Caribbean; Franco-Paredes, C., Santos-Preciado, J., Eds.; Neglected Tropical Diseases; Springer: Vienna, Austria, 2015. [Google Scholar] [CrossRef]
- Marcos-Marcos, J.; Olry de Labry-Lima, A.; Toro-Cardenas, S.; Lacasaña, M.; Degroote, S.; Ridde, V.; Bermudez-Tamayo, C. Impact, economic evaluation, and sustainability of integrated vector management in urban settings to prevent vector-borne diseases: A scoping review. Infect. Dis. Poverty 2018, 7, 83. [Google Scholar] [CrossRef] [PubMed]
- Claborn, D.M. The biology and control of leishmaniasis vectors. J. Glob. Infect. Dis. 2010, 2, 127–134. [Google Scholar] [CrossRef]
- Bamorovat, M.; Sharifi, I.; Agha Kuchak Afshari, S.; Ghasemi Nejad Almani, P. Mutual Role of Patients and the Healthcare System in the Control of Cutaneous Leishmaniasis. Transbound. Emerg. Dis. 2023, 2023, 7814940. [Google Scholar] [CrossRef]
- Wermelinger, E.D. Reflections on vector control in Brazil. Rev. Soc. Bras. Med. Trop. 2020, 53, e20190385. [Google Scholar] [CrossRef]
- Abraão, L.S.O.; José, B.M.P.A.; Gomes, C.B.S.; Nunes, P.C.S.; dos Santos, D.R.; Varela, A.P.A.S.; Lima, C.S. Perfil epidemiológico dos casos de leishmaniose tegumentar americana no estado do Pará, Brasil, entre 2008 e 2017. Rev. Pan-Amaz. Saúde 2020, 11, e202000612. [Google Scholar] [CrossRef]
- Gonçalves, L.P.; Santos, T.V.d.; Campos, M.B.; Lima, L.V.d.R.; Ishikawa, E.A.Y.; Silveira, F.T.; Ramos, P.K.S. Further insights into the eco-epidemiology of American cutaneous leishmaniasis in the Belem metropolitan region, Pará State, Brazil. Rev. Soc. Bras. Med. Trop. 2020, 53, e20200255. [Google Scholar] [CrossRef]
- Gontijo, B.; Carvalho, M.d.L.R.d. Leishmaniose tegumentar americana. Rev. Soc. Bras. Med. Trop. 2003, 36, 71–80. [Google Scholar] [CrossRef]
- Almeida, A.P.; Paulo, P.F.M.; Pereira Júnior, A.M.; Gujanwski, C.A.; Ferreira, V.; Costa, G.D.S.; Rodrigues, M.M.S.; Ferreira, R.G.M.; Medeiros, J.F. Occurrence of Leishmania infection in the immediate geographic region of Ji-Paraná, Rondônia State, Brazil. Rev. Soc. Bras. Med. Trop. 2021, 54, e02122021. [Google Scholar] [CrossRef]
- Santos, G.; Kückelhaus, S.; Roselino, A.; Chaer, W.; Sampaio, R. Leishmania (Viannia) braziliensis is the main species causing cutaneous leishmaniasis in the Federal District of Brazil. J. Venom. Anim. Toxins Incl. Trop. Dis. 2012, 18, 340–343. [Google Scholar] [CrossRef]
- Ferreira Ede, C.; Cruz, I.; Cañavate, C.; de Melo, L.A.; Pereira, A.A.; Madeira, F.A.; Valério, S.A.; Cunha, H.M.; Paglia, A.P.; Gontijo, C.M. Mixed infection of Leishmania infantum and Leishmania braziliensis in rodents from endemic urban area of the New World. BMC Vet. Res. 2015, 11, 71. [Google Scholar] [CrossRef] [PubMed]
- Cosma, C.; Maia, C.; Khan, N.; Infantino, M.; Del Riccio, M. Leishmaniasis in Humans and Animals: A One Health Approach for Surveillance, Prevention and Control in a Changing World. Trop. Med. Infect. Dis. 2024, 9, 258. [Google Scholar] [CrossRef]
- Cardoso, D.T.; de Souza, D.C.; de Castro, V.N.; Geiger, S.M.; Barbosa, D.S. Identification of priority areas for surveillance of cutaneous leishmaniasis using spatial analysis approaches in Southeastern Brazil. BMC Infect. Dis. 2019, 19, 318. [Google Scholar] [CrossRef]
- Reis, E.S.D.; Paz, W.S.; Santos Ramos, R.E.; Nunes Ribeiro, C.J.; Biano, L.S.; Bezerra-Santos, M.; de Oliveira, C.I.; Lipscomb, M.W.; de Moura, T.R. Spatial and temporal modeling of the global burden of Cutaneous Leishmaniasis in Brazil: A 21-year ecological study. PLoS Negl. Trop. Dis. 2024, 18, e0012668. [Google Scholar] [CrossRef] [PubMed]
- Bezerra, J.M.T.; de Araújo, V.E.M.; Barbosa, D.S.; Martins-Melo, F.R.; Werneck, G.L.; Carneiro, M. Burden of leishmaniasis in Brazil and federated units, 1990-2016: Findings from Global Burden of Disease Study 2016. PLoS Negl. Trop. Dis. 2018, 12, e0006697. [Google Scholar] [CrossRef]
- Teresinha Schröder, N.; Fraga Da Silveira, E.; Thomasi Janhke Botton, L.; Périco, E. Neglected diseases in Brazil: Space-temporal trends and public policies. In Neglected Tropical Diseases—Unsolved Debts for the One Health Approach; IntechOpen: London, UK, 2023. [Google Scholar] [CrossRef]
- Tomasella, J.; do Amaral Cunha, A.M.; Zeri, M.; Costa, L.C.O. Changes in the aridity index across Brazilian biomes. Sci. Total Environ. 2025, 989, 179869. [Google Scholar] [CrossRef]
- Pinheiro, M.P.G.; Silva-Inacio, C.L.; Silva, M.M.M.; Araújo, P.S.F.; Ximenes, M.F.F.M. Potential vectors of Leishmania spp. in an Atlantic Forest conservation unit in northeastern Brazil under anthropic pressure. Parasites Vectors 2021, 14, 38. [Google Scholar] [CrossRef]
- Sousa Júnior, A.S.; Gonçalves, N.V.; Miranda, C.S.C.; Santos, B.O.; de Oliveira, R.A.C.; da Costa, R.J.F.; Noguchi, S.K.d.T.; Oliveira, J.S.d.S.; Matsumura, E.S.S.; Palácios, V.R.d.C.M. Cutaneous leishmaniasis spatial distribution and epidemiological and environmental risk factors in Cametá, state of Pará, Brazil. Braz. J. Infect. Dis. 2020, 24, 330–336. [Google Scholar] [CrossRef] [PubMed]
- Instituto Brasileiro de Geografia e Estatística (IBGE). Cidades e Estados, Censo. 2022. Available online: https://www.ibge.gov.br/cidades-e-estados (accessed on 1 May 2025).
- Brasil Ministério da Saúde, Secretaria de Vigilância em Saúde. Manual de Vigilância da Leishmaniose Tegumentar Americana; Ministério da Saúde: Brasília, Brazil, 2017. Available online: https://bvsms.saude.gov.br/bvs/publicacoes/manual_vigilancia_leishmaniose_tegumentar.pdf (accessed on 2 May 2025).
- Brilhante, A.F.; Melchior, L.A.K.; Nunes, V.L.B.; Cardoso, C.O.; Galati, E.A.B. Epidemiological aspects of American cutaneous leishmaniasis (ACL) in an endemic area of forest extractivist culture in western Brazilian Amazonia. Rev. Inst. Med. Trop. São Paulo 2017, 59, e12. [Google Scholar] [CrossRef]
- Medina-Morales, D.A.; Machado-Duque, M.E.; Machado-Alba, J.E. Epidemiology of Cutaneous Leishmaniasis in a Colombian Municipality. Am. J. Trop. Med. Hyg. 2017, 97, 1503–1507. [Google Scholar] [CrossRef] [PubMed]
- Solomon, M.; Fuchs, I.; Glazer, Y.; Schwartz, E. Gender and Cutaneous Leishmaniasis in Israel. Trop. Med. Infect. Dis. 2022, 7, 179. [Google Scholar] [CrossRef] [PubMed]
- Jansen, A.; Stark, K.; Schneider, T.; Schoneberg, I. Diferenças sexuais na leptospirose clínica na Alemanha: 1997–2005. Clin. Infect. Dis. 2007, 44, e69–e72. [Google Scholar] [CrossRef]
- Schlagenhauf, P.; Chen, L.H.; Wilson, M.E.; Freedman, D.O.; Tcheng, D.; Schwartz, E.; Pandey, P.; Weber, R.; Nadal, D.; Berger, C.; et al. Sex and gender differences in travel-associated disease. Clin. Infect. Dis. 2010, 50, 826–832. [Google Scholar] [CrossRef]
- Lockard, R.D.; Wilson, M.E.; Rodríguez, N.E. Sex-related differences in the immune response symptomatic manifestations to infection with Leishmania species. J. Immunol. Res. 2019, 2019, 4103819. [Google Scholar] [CrossRef]
- Veiga Gonçalves, N.; Miranda, C.D.S.C.; Costa, R.J.F.D.; Guedes, J.A.; Matsumura, E.S.S.; Costa, S.B.N.D.; Noguchi, S.K.D.T.; Guimarães, L.H.R.; Coelho de Oliveira, R.A.; Simone Alves Tavares, L.; et al. Cutaneous leishmaniasis: Spatial distribution and environmental risk factors in the state of Pará, Brazilian Eastern Amazon. J. Infect. Dev. Ctries. 2019, 13, 939–944. [Google Scholar] [CrossRef]
- Oliveira, R.S.; Pimentel, K.B.A.; Moura, M.L.; Aragão, C.F.; Guimarães-e-Silva, A.S.; Bezerra, J.M.T.; Melo, M.N.; Pinheiro, V.C.S. Clinical, epidemiological and climatic factors related to the occurrence of cutaneous leishmaniasis in an endemic area in northeastern Brazil. Braz. J. Biol. 2021, 81, 557–565. [Google Scholar] [CrossRef]
- Gonçalves, N.V.; Alcântara, R.C.C.; Sousa, A.S.; Pereira, A.L.R.R.; Miranda, C.S.C.; Oliveira, J.S.S.; Melo, A.C.B.V.; Guedes, J.A.; Costa, R.J.F.; Costa, S.B.N.; et al. Leprosy in an administrative district of Belém, Pará State, Brazil: Relations between territory, socioeconomics, and public health policy, 2007–2013. Rev. Pan-Amaz. Saúde 2018, 9, 2176–6223. [Google Scholar] [CrossRef]
- Lima, C.C.M.; Grisotti, M.; Santos, F.S. Os desafios no controle das leishmanioses no contexto da cidade de Montes Claros (MG). Rev. Unimontes Científica 2017, 18, 131–147. [Google Scholar]
- Morgan, D.J.; Guimaraes, L.H.; Machado, P.R.; D’OLiveira, A., Jr.; Almeida, R.P.; Lago, E.L.; Faria, D.R.; Tafuri, W.L.; Dutra, W.O.; Carvalho, E.M. Cutaneous leishmaniasis during pregnancy: Exuberant lesions and potential fetal complications. Clin. Infect. Dis. 2007, 45, 478–482. [Google Scholar] [CrossRef] [PubMed]
- Santa Catarina, Secretaria Estadual de Saúde, Superintendência de Vigilância em Saúde. Guia de Orientação da Vigilância da Leishmaniose Tegumentar; Superintendência de Vigilância em Saúde: Florianópolis, Brazil, 2021. [Google Scholar]
- Vasconcelos, J.M.; Gomes, C.G.; Sousa, A.; Teixeira, A.B.; Lima, J.M. Leishmaniose tegumentar americana: Perfil epidemiológico, diagnóstico e tratamento. Rev. Bras. Análises Clínicas 2018, 50, 221–227. [Google Scholar]
- Almeida ANFde Nascimento Lde CSdo Sousa ESMde, M.; de Oliveira, A.J.D.; de Sena, M.G.; de Resende, B.M.; Chaves, R.C.G.; Garcez, L.M. Vigilância da leishmaniose cutânea em amostras clínicas: Distribuição da Leishmania guyanensis no estado do Amapá, 2018. Epidemiol. Serv. Saúde 2020, 29, e2018504. [Google Scholar] [CrossRef]
- Santos, M.F.D.; Lorenz, C.; Chiaravalotti-Neto, F.; Lima-Camara, T.N. Spatial analysis of American cutaneous leishmaniasis in the state of Amazonas. Rev. Saude Publica 2024, 58, 11. [Google Scholar] [CrossRef]
- Rodgers, M.S.M.; Bavia, M.E.; Eichold, B.; Shipman, C.; Owen, N.; Winstanley, H.; Gordon, M.; Karapetyan, M.; Silva, M.M.N.; Carneiro, D.D.M.T.; et al. Environmental risk factors of leishmaniasis in Bahia State, Brazil using NASA Earth observation satellites. Rev. Inst. Adolfo Lutz 2018, 77, e1775. [Google Scholar] [CrossRef]
- Yarzon RMde, G.B.; Dorval, M.E.C.; Freitas HGde Oshiro, E.T. Leishmaniose Tegumentar Americana (LTA) em Mato Grosso do Sul. Rev. Soc. Bras. Med. Trop. 2003, 36, 41–42. [Google Scholar] [CrossRef]
- Temponi, A.O.D.; de Brito, M.G.; Ferraz, M.L.; Diniz, S.d.A.; Silva, M.X.; da Cunha, T.N. Ocorrência de casos de leishmaniose tegumentar americana: Uma análise multivariada dos circuitos espaciais de produção, Minas Gerais, Brasil, 2007 a 2011. Cad Saúde Pública 2018, 34, e00165716. [Google Scholar] [CrossRef]
- Lana, R.S.; Michalsky, E.M.; Fortes-Dias, C.L.; França-Silva, J.C.; Lara-Silva, F.O.; Lima, A.C.V.M.R.; de Avelar, D.M.; Martins, J.C.D.; Dias, E.S. Phlebotomine sand fly fauna and Leishmania infection in the vicinity of the Serra do Cipó National Park, a natural Brazilian heritage site. BioMed Res. Int. 2015, 2015, 385493. [Google Scholar] [CrossRef]
- Osmari, V.; Fernandes, F.D.; Tatto, M.; Souza, G.D.; Ratzlaff, F.R.; Vasconcellos, J.S.d.P.; Botton, S.d.A.; Machado, D.W.N.; Vogel, F.S.F.; Sangioni, L.A. Fauna and seasonality of sand flies (Diptera: Psychodidae: Phlebotominae) from a leishmaniasis transmission area in the central region of Rio Grande do Sul, Brazil. Rev. Bras. Parasitol. Vet. 2024, 33, e000824. [Google Scholar] [CrossRef]
- Pereira, N.C.L.; Michalsky, E.M.; Lara-Silva, F.O.; Lana, R.S.; Paula, A.J.V.; Pereira, D.M.; Lopes, J.V.; Fortes-Dias, C.L.; Dias, E.S. Ecology of phlebotomine sand flies in a Brazilian area with recent leishmaniasis transmission (Itaúna, in Minas Gerais state). Rev. Soc. Bras. Med. Trop. 2020, 53, e20190538. [Google Scholar] [CrossRef] [PubMed]
- Pedrosa Fde, A.; Ximenes, R.A. Sociodemographic and environmental risk factors for American cutaneous leishmaniasis (ACL) in the State of Alagoas, Brazil. Am. J. Trop. Med. Hyg. 2009, 81, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Dires, A.; Gedamu, S.; Kumar, P.; Yimam, W.; Ademe, S.; Dires, T. Determinants of cutaneous leishmaniasis among students in Delanta district, Northeast Ethiopia: A case-control study. Health Sci. Rep. 2022, 5, e917. [Google Scholar] [CrossRef] [PubMed]
- de Vries, H.J.C.; Schallig, H.D. Cutaneous Leishmaniasis: A 2022 Updated Narrative Review into Diagnosis and Management Developments. Am. J. Clin. Dermatol. 2022, 23, 823–840. [Google Scholar] [CrossRef]
- Aronson, N.; Herwaldt, B.L.; Libman, M.; Pearson, R.; Lopez-Velez, R.; Weina, P.; Carvalho, E.M.; Ephros, M.; Jeronimo, S.; Magill, A. Diagnosis and Treatment of Leishmaniasis: Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA) and the American Society of Tropical Medicine and Hygiene (ASTMH). Clin. Infect. Dis. 2016, 63, e202–e264. [Google Scholar] [CrossRef]
| Variables | Cases | Percentage |
|---|---|---|
| n | % | |
| Sex | ||
| Male | 133,816 | 73.2 |
| Female | 48,851 | 26.8 |
| Ethnicity | ||
| Brown | 118,678 | 65.0 |
| White | 34,419 | 18.8 |
| Black | 14,865 | 8.1 |
| Indigenous | 6791 | 3.8 |
| Asian | 1415 | 0.8 |
| Ignored | 6321 | 3.5 |
| Age Group (Years) | ||
| <1 | 2332 | 1.4 |
| 1 to 4 | 3631 | 2.1 |
| 5 to 9 | 6000 | 3.6 |
| 10 to14 | 10,750 | 6.5 |
| 15 to 19 | 16,945 | 10.1 |
| 20 to 39 | 69,773 | 41.5 |
| 40 to 59 | 48,816 | 29.1 |
| 60 to 64 | 7954 | 4.7 |
| >65 | 1693 | 1.0 |
| Level of education | ||
| Ignored | 43,043 | 23.6 |
| Illiterate | 8117 | 4.5 |
| Incomplete 1st to 4th grade of elementary school | 29,318 | 16.0 |
| Complete 4th grade of elementary school | 13,114 | 7.2 |
| Incomplete 5th to 8th grade of elementary school | 30,404 | 16.7 |
| Complete elementary school | 11,154 | 6.1 |
| Incomplete high school | 13,028 | 7.1 |
| Complete high school | 20,484 | 11.2 |
| Incomplete higher education | 1674 | 0.9 |
| Complete higher education | 4031 | 2.2 |
| Not applicable | 8122 | 4.5 |
| Gestational condition | ||
| No | 32,151 | 91.8 |
| Yes | 614 | 1.8 |
| Ignored | 2244 | 6.4 |
| Confirmation criteria | ||
| Laboratory | 145,978 | 80.0 |
| Clinical-epidemiological | 36,511 | 20.0 |
| Clinical form | ||
| Cutaneous | 171,293 | 94.0 |
| Mucosal | 11,118 | 6.0 |
| Municipalities | Cases | Population | Land Area * | Demographic Density ** | Prevalence |
|---|---|---|---|---|---|
| Manaus—AM | 5619 | 2063,689 | 11,401,002 | 181.01 | 272.2 |
| Presidente Tancredo Neves—BA | 4527 | 27,134 | 441,820 | 62.17 | 166.3 |
| Rio Branco—AC | 2246 | 364,756 | 8,834,831 | 41.28 | 615.7 |
| Macapá—AP | 1970 | 442,933 | 6,563,849 | 62.48 | 444.7 |
| Porto Velho—RO | 1697 | 460,434 | 34,091,146 | 13.51 | 368.5 |
| Presidente Figueiredo—AM | 1688 | 30,668 | 331,354 | 6.98 | 5503.1 |
| Belo Horizonte—MG | 1674 | 2,315,560 | 5,687,037 | 6988.18 | 72.2 |
| Boa Vista—RR | 1661 | 413,986 | 5,090,238 | 72.91 | 401.7 |
| Santarém—PA | 1554 | 306,942 | 17,829,220 | 18.55 | 468.1 |
| Cuiabá—MT | 1434 | 650,819 | 430,340 | 150.91 | 220.3 |
| Valença—RJ | 1342 | 68,088 | 1,300,622 | 52.34 | 1970.9 |
| Rio Preto da Eva—AM | 1256 | 24,936 | 5,815,622 | 4.29 | 5197.3 |
| Laranjal do Jari—AP | 1255 | 44,858 | 30,542,284 | 1.14 | 3594.0 |
| Vilhena—RO | 1240 | 95,832 | 11,708,519 | 8.19 | 1308.5 |
| Uruará—PA | 1201 | 43,558 | 10,791,400 | 4.04 | 2289.9 |
| Montes Claros—MG | 1196 | 414,240 | 3,589,811 | 115.39 | 288.6 |
| Medicilândia—PA | 1195 | 27,094 | 8,292,629 | 3.28 | 4414.2 |
| Boral—PA | 1174 | 62,503 | 25,386,158 | 2.46 | 1911.2 |
| Monte Alegre—PA | 1171 | 60,012 | 18,151,323 | 3.31 | 1951.2 |
| Altamira—PA | 1166 | 126,279 | 159,533,306 | 0.79 | 923.3 |
| Sex | Low Endemicity | Medium Endemicity | High Endemicity | |||
|---|---|---|---|---|---|---|
| n | p-Value | n | p-Value | n | p-Value | |
| Male | 10,492 | 0.000 * | 28,258 | 0.000 * | 95,085 | 0.001 * |
| Female | 5474 | 17,958 | 25,433 | |||
| Ethnicity | ||||||
| Brown | 6325 | <2.2 × 10−16 * | 29,385 | <2.2 × 10−16 * | 83,040 | <2.2 × 10−16 * |
| White | 7391 | 8294 | 18,854 | |||
| Black | 1024 | 5519 | 8338 | |||
| Indigenous | 202 | 502 | 5650 | |||
| Asian | 192 | 292 | 952 | |||
| Ignored | 835 | 2245 | 3253 | |||
| Age group (Years) | ||||||
| <1 | 135 | <2.2 × 10−16 * | 590 | <2.2 × 10−16 * | 1607 | <2.2 × 10−16 * |
| 1 to 4 | 259 | 1174 | 1979 | |||
| 5 to 9 | 496 | 1946 | 3560 | |||
| 10 to 14 | 719 | 2886 | 7150 | |||
| 15 to 19 | 847 | 3332 | 12,769 | |||
| 20 to 39 | 4300 | 12,897 | 52,607 | |||
| 40 to 59 | 5277 | 13,441 | 30,105 | |||
| 60 to 64 | 1189 | 2870 | 3898 | |||
| >65 | 2744 | 7090 | 6611 | |||
| Level of education | ||||||
| Ignored | 4723 | 0.000 * | 12,705 | 0.000 * | 25,713 | 0.004 * |
| Illiterate | 764 | 2761 | 4611 | |||
| Incomplete 1st to 4th grade of elementary school | 2138 | 8654 | 18,502 | |||
| Complete 4th grade of elementary school | 1108 | 2925 | 9096 | |||
| Incomplete 5th to 8th grade of elementary school | 1950 | 6457 | 22,021 | |||
| Complete elementary school | 1122 | 2078 | 7969 | |||
| Incomplete high school | 910 | 2336 | 9796 | |||
| Complete high school | 1912 | 4418 | 14,180 | |||
| Incomplete higher education | 186 | 376 | 1115 | |||
| Complete higher education | 618 | 1032 | 2391 | |||
| Not applicable | 557 | 2495 | 5071 | |||
| Gestational condition | ||||||
| Yes | 68 | 0.009 * | 143 | 0.004 * | 369 | 0.281 |
| No | 3626 | 9792 | 16,884 | |||
| Confirmation criteria | ||||||
| Laboratory | 9098 | 0.001 * | 28,234 | 0.000 * | 105,553 | 0.000 * |
| Clinical-epidemiological | 6629 | 14,910 | 14,972 | |||
| Clinical form | ||||||
| Cutaneous | 13,653 | <2.2 × 10−16 * | 43,038 | <2.2 × 10−16 * | 114,602 | <2.2 × 10−16 * |
| Mucosal | 2020 | 3195 | 5903 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tolentino Júnior, D.S.; Silva, H.T.d.; Ribeiro, A.M.; Amador, A.M.R.; Silva, B.O.S.e.; Guimarães, B.M.; Nogueira, M.B.L.; Teixeira, H.K.C.; Assis, E.M.d. Different Levels of Endemicity of Cutaneous Leishmaniasis in Brazil. Zoonotic Dis. 2025, 5, 28. https://doi.org/10.3390/zoonoticdis5040028
Tolentino Júnior DS, Silva HTd, Ribeiro AM, Amador AMR, Silva BOSe, Guimarães BM, Nogueira MBL, Teixeira HKC, Assis EMd. Different Levels of Endemicity of Cutaneous Leishmaniasis in Brazil. Zoonotic Diseases. 2025; 5(4):28. https://doi.org/10.3390/zoonoticdis5040028
Chicago/Turabian StyleTolentino Júnior, Dilceu Silveira, Heberson Teixeira da Silva, Alessandro Martins Ribeiro, Ana Mécia Ribeiro Amador, Bruno Oliveira Souza e Silva, Bárbara Mendes Guimarães, Manuella Botelho Laure Nogueira, Hellen Karine Campos Teixeira, and Eliseu Miranda de Assis. 2025. "Different Levels of Endemicity of Cutaneous Leishmaniasis in Brazil" Zoonotic Diseases 5, no. 4: 28. https://doi.org/10.3390/zoonoticdis5040028
APA StyleTolentino Júnior, D. S., Silva, H. T. d., Ribeiro, A. M., Amador, A. M. R., Silva, B. O. S. e., Guimarães, B. M., Nogueira, M. B. L., Teixeira, H. K. C., & Assis, E. M. d. (2025). Different Levels of Endemicity of Cutaneous Leishmaniasis in Brazil. Zoonotic Diseases, 5(4), 28. https://doi.org/10.3390/zoonoticdis5040028






