A Preliminary Predictive Model for Proliferative Lupus Nephritis in Juvenile Systemic Lupus Erythematosus
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Pre-Processing
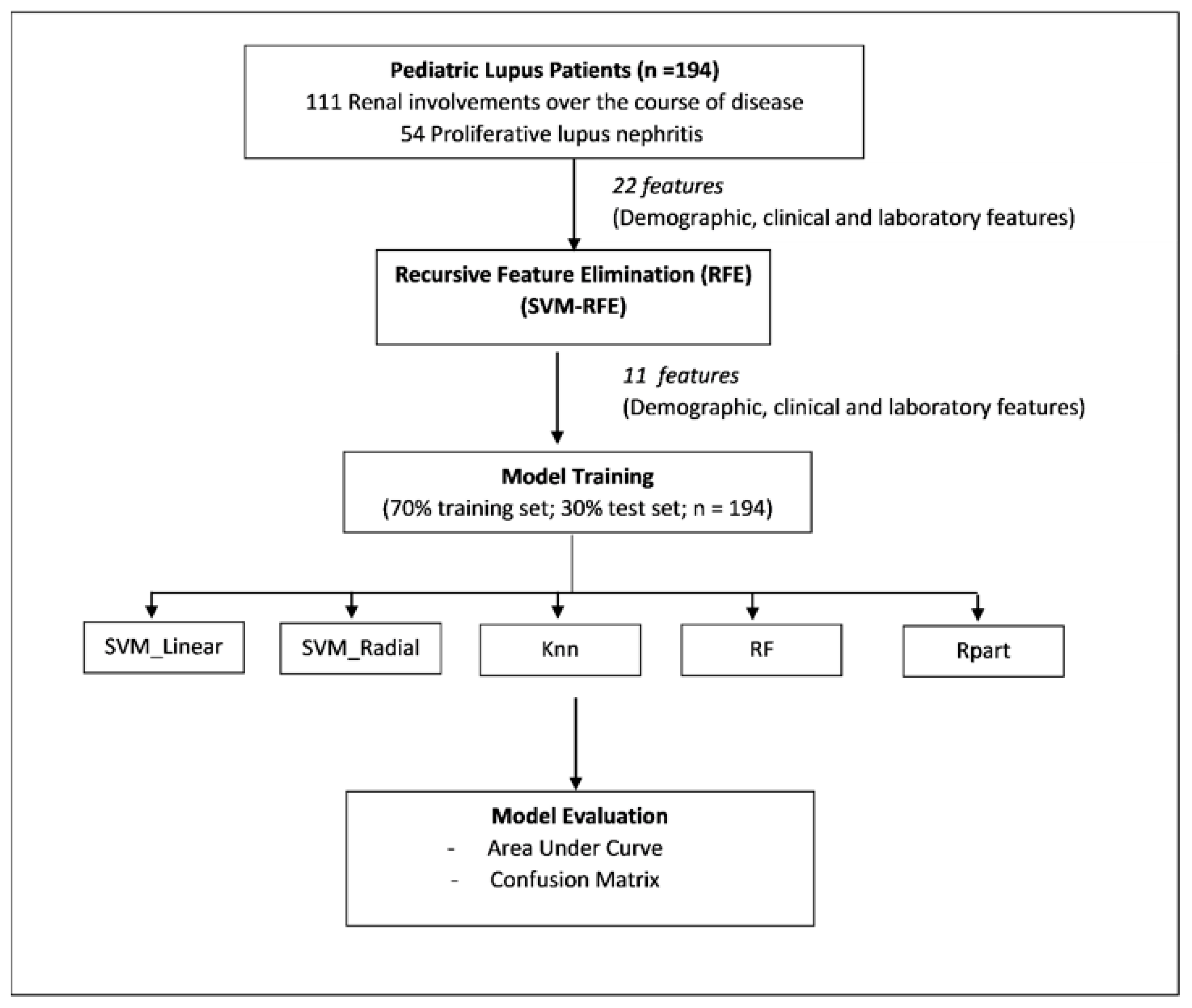
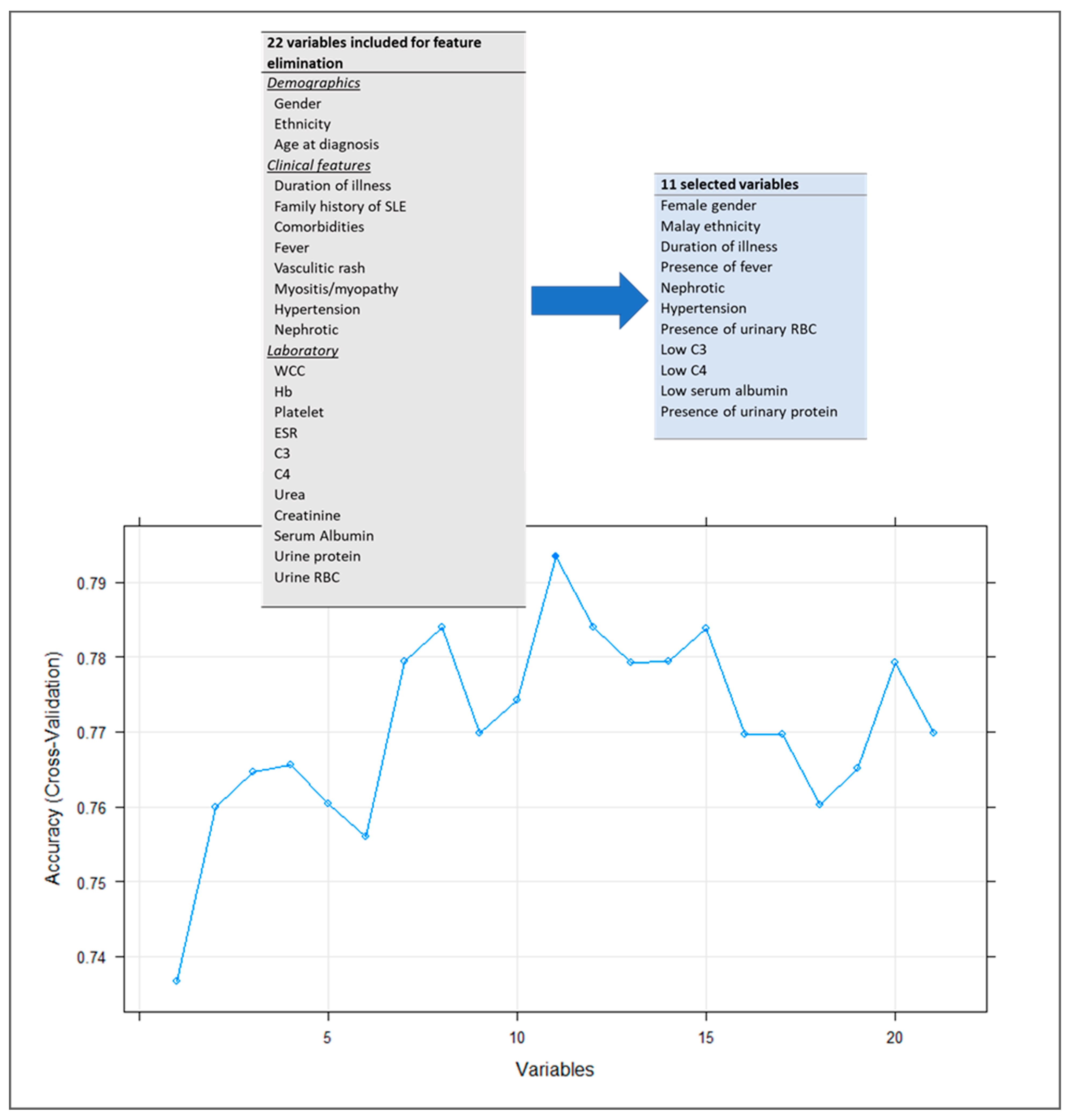
2.2. Feature Selection: Support Vector Machine Classification (SVM)-Recursive Feature Elimination (RFE)
2.3. Model Training and Parameter Tuning
2.4. Model Evaluation
3. Results
3.1. Demographic and Characteristic of Study Population
3.2. Clinical Features and Major Organ Manifestations at Presentation
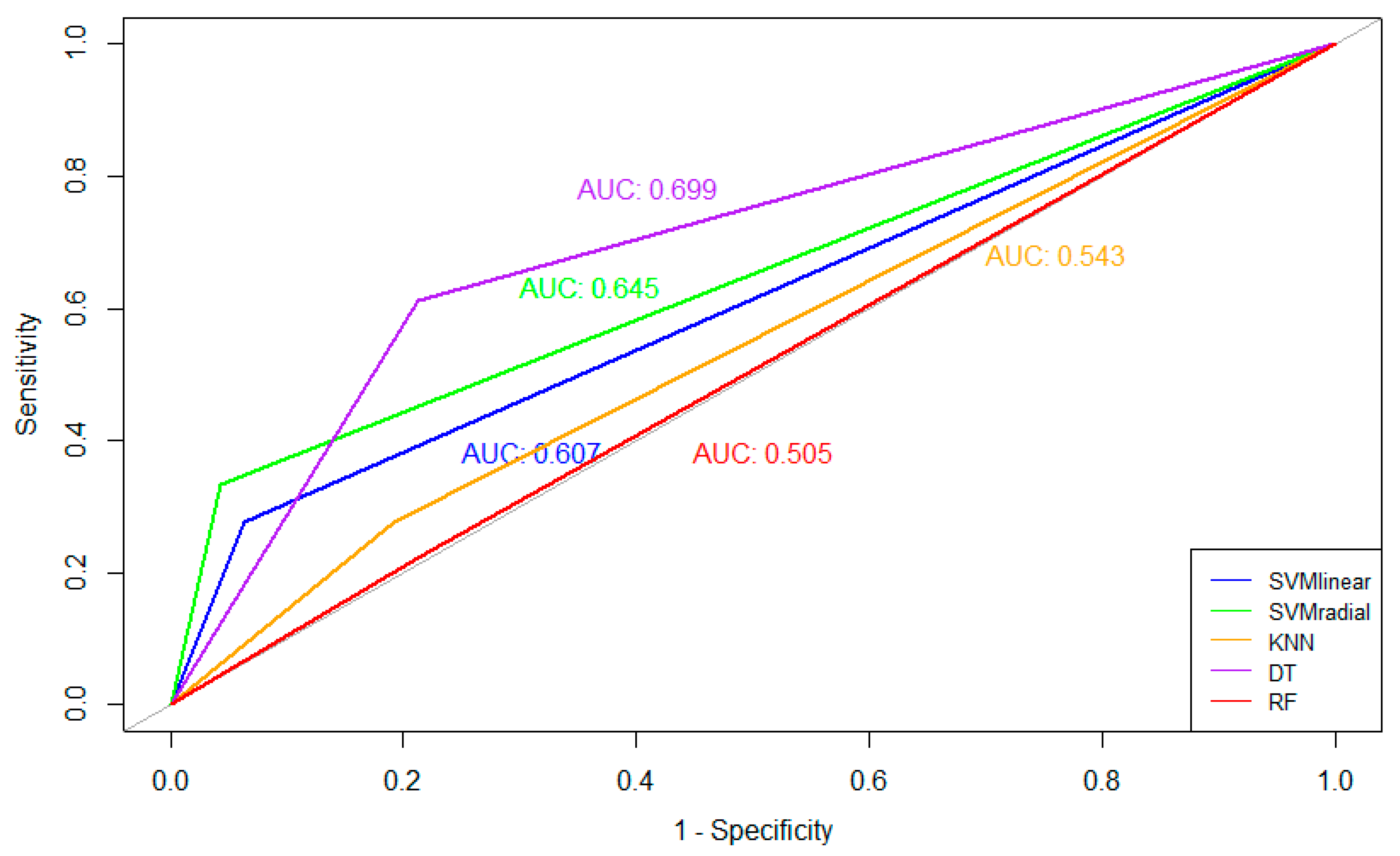
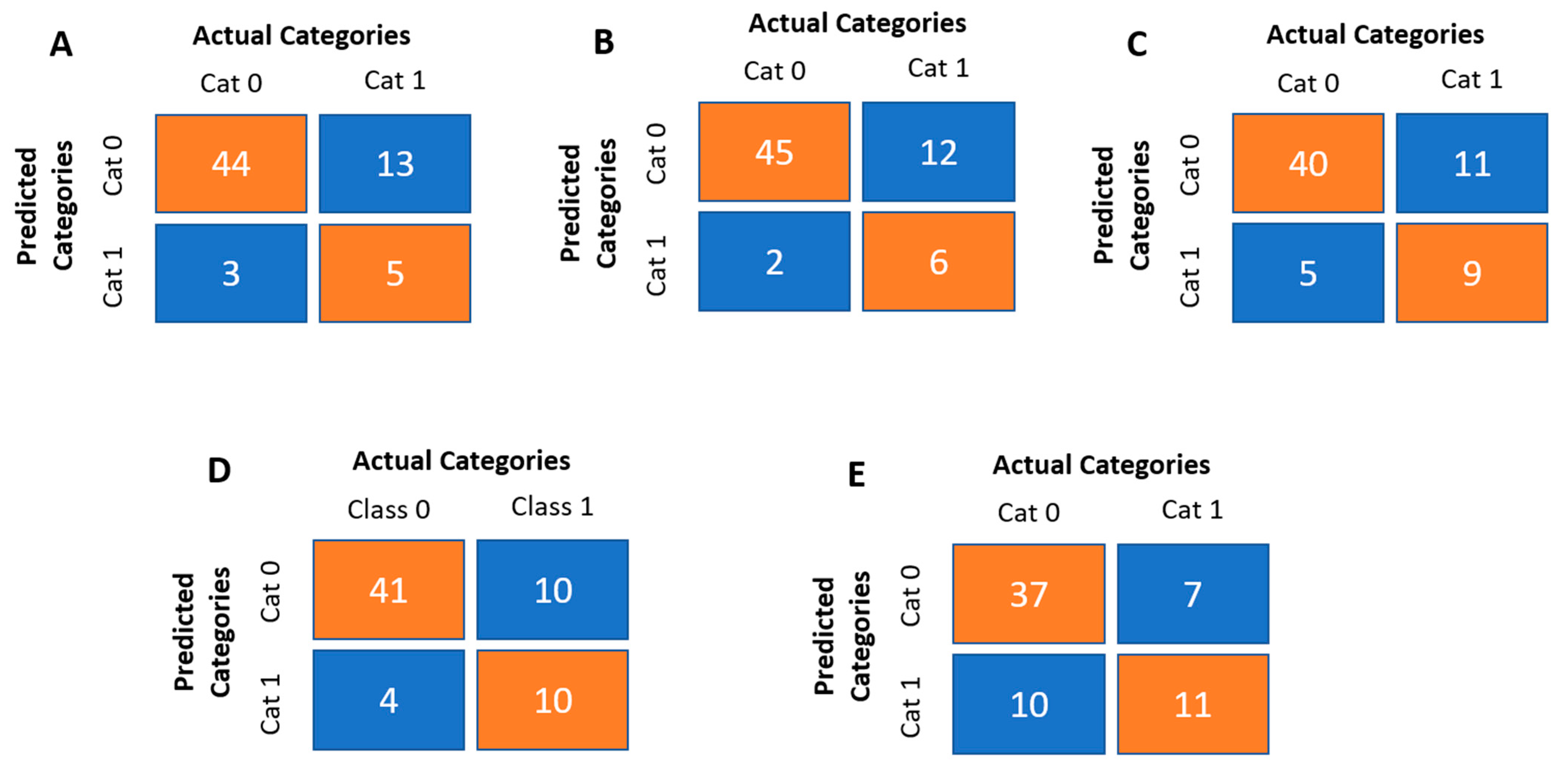
3.3. Determination of Variables That Could Predict Proliferative Lupus Nephritis among the jSLE Cases
4. Discussion
4.1. Strengths
4.2. Limitations
4.3. Recommendations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hiraki, L.T.; Benseler, S.M.; Tyrrell, P.N.; Hebert, D.; Harvey, E.; Silverman, E.D. Clinical and Laboratory Characteristics and Long-Term Outcome of Pediatric Systemic Lupus Erythematosus: A Longitudinal Study. J. Pediatr. 2008, 152, 550–556. [Google Scholar] [CrossRef]
- Levy, D.M.; Kamphuis, S. Systemic Lupus Erythematosus in Children and Adolescents. Pediatr. Clin. N. Am. 2012, 59, 345–364. [Google Scholar] [CrossRef] [PubMed]
- Kamphuis, S.; Silverman, E.D. Prevalence and burden of pediatric-onset systemic lupus erythematosus. Nat. Rev. Rheumatol. 2010, 6, 538–546. [Google Scholar] [CrossRef] [PubMed]
- Watson, L.; Leone, V.; Pilkington, C.; Tullus, K.; Rangaraj, S.; McDonagh, J.E.; Gardner-Medwin, J.; Wilkinson, N.; Riley, P.; Tizard, J.; et al. Disease activity, severity, and damage in the UK juvenile-onset systemic lupus erythematosus cohort. Arthritis Rheum. 2012, 64, 2356–2365. [Google Scholar] [CrossRef]
- Arkachaisri, T. Pediatric Rheumatology in Southeast Asia: Insights from the Singapore Experience. Curr. Rheumatol. Rep. 2010, 13, 117–122. [Google Scholar] [CrossRef]
- Huang, J.L.; Yao, T.C.; See, L.-C. Prevalence of pediatric systemic lupus erythematosus and juvenile chronic arthritis in a Chinese population: A nation-wide prospective population-based study in Taiwan. Ann. Rheum. Dis. 2005, 22, 776–780. [Google Scholar]
- Mackie, F.E.; Kainer, G.; Adib, N.; Boros, C.; Elliott, E.; Fahy, R.; Munro, J.; Murray, K.; Rosenberg, A.; Wainstein, B.; et al. The national incidence and clinical picture of SLE in children in Australia—A report from the Australian Paediatric Surveillance Unit. Lupus 2014, 24, 66–73. [Google Scholar] [CrossRef]
- Hiraki, L.T.; Benseler, S.M.; Tyrrell, P.N.; Harvey, E.; Hebert, D.; Silverman, E.D. Ethnic Differences in Pediatric Systemic Lupus Erythematosus. J. Rheumatol. 2009, 36, 2539–2546. [Google Scholar] [CrossRef]
- Danchenko, N.; Satia, J.A.; Anthony, M.S. Epidemiology of systemic lupus erythematosus: A comparison of worldwide disease burden. Lupus 2006, 15, 308–318. [Google Scholar] [CrossRef]
- Levy, D.M.; Peschken, C.; Tucker, L.; Chédeville, G.; Huber, A.M.; Pope, J.; the Canadian Network for Improved Outcomes in SLE 1000 Faces Investigators; Silverman, E.D. Influence of ethnicity on childhood-onset systemic lupus erythematosus: Results from a multiethnic multicenter Canadian cohort. Arthritis Care Res. 2012, 65, 152–160. [Google Scholar] [CrossRef]
- Tucker, L.; Uribe, A.; Fernández, M.; Vilá, L.; McGwin, G.; Apte, M.; Fessler, B.; Bastian, H.; Reveille, J.; Alarcón, G. Adolescent onset of lupus results in more aggressive disease and worse outcomes: Results of a nested matched case–control study within LUMINA, a multiethnic US cohort (LUMINA LVII). Lupus 2008, 17, 314–322. [Google Scholar] [CrossRef] [PubMed]
- Mina, R.; Brunner, H.I. Pediatric Lupus—Are There Differences in Presentation, Genetics, Response to Therapy, and Damage Accrual Compared with Adult Lupus? Rheum. Dis. Clin. N. Am. 2010, 36, 53–80. [Google Scholar] [CrossRef]
- Glidden, R.S.; Mantzouranis, E.C.; Borel, Y. Systemic lupus erythematosus in childhood: Clinical manifestations and improved survival in fifty-five patients. Clin. Immunol. Immunopathol. 1983, 29, 196–210. [Google Scholar] [CrossRef] [PubMed]
- Mina, R.; Brunner, H.I. Update on differences between childhood-onset and adult-onset systemic lupus erythematosus. Thromb. Haemost. 2013, 15, 218. [Google Scholar] [CrossRef] [PubMed]
- Brunner, H.I.; Gladman, D.D.; Ibañez, D.; Urowitz, M.D.; Silverman, E.D. Difference in disease features between childhood-onset and adult-onset systemic lupus erythematosus. Arthritis Rheum. 2008, 58, 556–562. [Google Scholar] [CrossRef]
- Artim-Esen, B.; Şahin, S.; Çene, E.; Şahinkaya, Y.; Barut, K.; Adrovic, A.; Ozluk, Y.; Kılıçaslan, I.; Omma, A.; Gül, A.; et al. Comparison of Disease Characteristics, Organ Damage, and Survival in Patients with Juvenile-onset and Adult-onset Systemic Lupus Erythematosus in a Combined Cohort from 2 Tertiary Centers in Turkey. J. Rheumatol. 2017, 44, 619–625. [Google Scholar] [CrossRef]
- Gheith, R.E.; El-Gazzar, I.I.; El Fishawy, H.S.; El-Din, A.M.N.; Bahgat, D.M.; Gheita, T.A. Juvenile and juvenile-onset systemic lupus erythematosus patients: Clinical characteristics, disease activity and damage. Egypt. Pediatr. Assoc. Gaz. 2017, 65, 49–53. [Google Scholar] [CrossRef]
- Lee, P.-Y.; Yeh, K.-W.; Yao, T.-C.; Lee, W.-I.; Lin, Y.-J.; Huang, J.-L. The outcome of patients with renal involvement in pediatric-onset systemic lupus—A 20-year experience in Asia. Lupus 2013, 22, 1534–1540. [Google Scholar] [CrossRef]
- Pluchinotta, F.R.; Schiavo, B.; Vittadello, F.; Martini, G.; Perilongo, G.; Zulian, F. Distinctive clinical features of pediatric systemic lupus erythematosus in three different age classes. Lupus 2007, 16, 550–555. [Google Scholar] [CrossRef]
- Lim, S.C.; Chan, W.L.E.; Tang, S.P. Clinical features, disease activity and outcomes of Malaysian children with paediatric systemic lupus erythematosus: A cohort from a tertiary centre. Lupus 2020, 29, 1106–1114. [Google Scholar] [CrossRef]
- Brunner, H.I.; Silverman, E.D.; To, T.; Bombardier, C.; Feldman, B.M. Risk factors for damage in childhood-onset systemic lupus erythematosus: Cumulative disease activity and medication use predict disease damage. Arthritis Rheum. 2002, 46, 436–444. [Google Scholar] [CrossRef] [PubMed]
- Tang, S.; Lim, S.; Arkachaisri, T. Childhood-Onset Systemic Lupus Erythematosus: Southeast Asian Perspectives. J. Clin. Med. 2021, 10, 559. [Google Scholar] [CrossRef] [PubMed]
- Wenderfer, S.E.; Ruth, N.M.; Brunner, H.I. Advances in the care of children with lupus nephritis. Pediatr. Res. 2016, 81, 406–414. [Google Scholar] [CrossRef]
- Oni, L.; Wright, R.D.; Marks, S.; Beresford, M.W.; Tullus, K. Kidney outcomes for children with lupus nephritis. Pediatr. Nephrol. 2020, 36, 1377–1385. [Google Scholar] [CrossRef]
- Anders, H.-J.; Rovin, B. A pathophysiology-based approach to the diagnosis and treatment of lupus nephritis. Kidney Int. 2016, 90, 493–501. [Google Scholar] [CrossRef] [PubMed]
- Yap, D.Y.; Tang, C.S.; Ma, M.K.; Lam, M.F.; Chan, T.M. Survival analysis and causes of mortality in patients with lupus nephritis. Nephrol. Dial. Transplant. 2012, 27, 3248–3254. [Google Scholar] [CrossRef]
- Escárcega, R.O.; Garcia-Carrasco, M.; Jara, L.J.; Cervera, R. Accelerated Atherosclerosis in Systemic Lupus Erythematosus: Perspectives towards Decreasing Cardiovascular Morbidity and Mortality. Lupus 2009, 18, 383–386. [Google Scholar] [CrossRef]
- Sule, S.; Fivush, B.; Neu, A.; Furth, S. Increased Hospitalizations and Death in Patients with ESRD Secondary to Lupus. Lupus 2012, 21, 1208–1213. [Google Scholar] [CrossRef]
- Hachiya, A.; Karasawa, M.; Imaizumi, T.; Kato, N.; Katsuno, T.; Ishimoto, T.; Kosugi, T.; Tsuboi, N.; Maruyama, S. The ISN/RPS 2016 classification predicts renal prognosis in patients with first-onset class III/IV lupus nephritis. Sci. Rep. 2021, 11, 1525. [Google Scholar] [CrossRef]
- Weening, J.J.; D’Agati, V.D.; Schwartz, M.M.; Seshan, S.V.; Alpers, C.E.; Appel, G.B.; Balow, J.E.; Bruijn, J.A.; Cook, T.; Ferrario, F.; et al. The Classification of Glomerulonephritis in Systemic Lupus Erythematosus Revisited. J. Am. Soc. Nephrol. 2004, 15, 241–250. [Google Scholar] [CrossRef]
- Houssiau, F.A.; Lauwerys, B.R. Current management of lupus nephritis. Best Pract. Res. Clin. Rheumatol. 2013, 27, 319–328. [Google Scholar] [CrossRef]
- Ramachandran, R.; Sulaiman, S.; Chauhan, P.; Ulasi, I.; Onu, U.; Villaneuva, R.; Alam, M.R.; Akhtar, F.; Vincent, L.; Aulakh, G.S.; et al. Challenges in Diagnosis and Management of Glomerular Disease in Resource-Limited Settings. Kidney Int. Rep. 2022, 7, 2141–2149. [Google Scholar] [CrossRef]
- Htay, H.; Alrukhaimi, M.; Ashuntantang, G.E.; Bello, A.K.; Bellorin-Font, E.; Gharbi, M.B.; Braam, B.; Feehally, J.; Harris, D.C.; Jha, V.; et al. Global access of patients with kidney disease to health technologies and medications: Findings from the Global Kidney Health Atlas project. Kidney Int. Suppl. 2018, 8, 64–73. [Google Scholar] [CrossRef] [PubMed]
- Kwon, O.C.; Park, J.H.; Park, H.-C.; Jung, S.M.; Lee, S.-W.; Song, J.J.; Park, Y.-B.; Park, M.-C. Non-histologic factors discriminating proliferative lupus nephritis from membranous lupus nephritis. Thromb. Haemost. 2020, 22, 138. [Google Scholar] [CrossRef]
- Petri, M.; Orbai, A.-M.; Alarcón, G.S.; Gordon, C.; Merrill, J.T.; Fortin, P.R.; Bruce, I.N.; Isenberg, D.; Wallace, D.J.; Nived, O.; et al. Derivation and validation of the Systemic Lupus International Collaborating Clinics classification criteria for systemic lupus erythematosus. Arthritis Rheum. 2012, 64, 2677–2686. [Google Scholar] [CrossRef]
- Kuan, W.; Li, E.; Tam, L.-S. Lupus organ damage: What is damaged in Asian patients? Lupus 2010, 19, 1436–1441. [Google Scholar] [CrossRef]
- Sit, J.K.K.; Chan, W.K.Y. Risk factors for damage in childhood-onset systemic lupus erythematosus in Asians: A case control study. Pediatr. Rheumatol. 2018, 16, 56. [Google Scholar] [CrossRef]
- Abujam, B.; Gupta, A.; Suri, D.; Rawat, A.; Singh, S. Trends and predictors of mortality in childhood onset lupus in a single North-Indian centre over 23 years: A retrospective study. Ann. Rheum. Dis. 2016, 34, 554–559. [Google Scholar]
- Mina, R.; Von Scheven, E.; Ardoin, S.P.; Eberhard, B.A.; Punaro, M.; Ilowite, N.; Hsu, J.; Klein-Gitelman, M.; Moorthy, L.N.; Muscal, E.; et al. Consensus treatment plans for induction therapy of newly diagnosed proliferative lupus nephritis in juvenile systemic lupus erythematosus. Arthritis Care Res. 2011, 64, 375–383. [Google Scholar] [CrossRef]
- Sule, S.D.; Moodalbail, D.G.; Burnham, J.; Fivush, B.; Furth, S.L. Predictors of Kidney Disease in a Cohort of Pediatric Patients with Lupus. Lupus 2015, 24, 862–868. [Google Scholar] [CrossRef]
- Hisham, F.A.; Tharwat, S.; Samra, N.E.; Mostafa, N.; Nassar, M.K.; El-Desoky, M.M. High Mobility Group Box Protein 1 (HMGB1) Serum and Urinary Levels and Gene Polymorphism in Egyptian Patients with Systemic Lupus Erythematosus: A Possible Relation to Lupus Nephritis. Lupus 2022, 31, 1777–1785. [Google Scholar] [CrossRef]
- Kwon, O.C.; Lee, J.S.; Ghang, B.; Kim, Y.-G.; Lee, C.-K.; Yoo, B.; Hong, S. Predicting eventual development of lupus nephritis at the time of diagnosis of systemic lupus erythematosus. Semin. Arthritis Rheum. 2018, 48, 462–466. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | No. of Participating Patients, n = 194 (%) |
|---|---|
| Gender | |
| Female | 165 (85.5) |
| Female: Male Ratio | 5.5:1 |
| Female: Male Ratio based on age: | |
| 0–5 years old | 2.7:1 |
| 6–12 years old | 7.8:1 |
| 13–18 years old | 23.4:1 |
| Median age (years, IQR) | |
| At diagnosis | 11.7 (9.0–15.3) |
| At data collection | 15.0 (13.4–20.0) |
| Duration of illness, median | |
| Onset of symptoms to diagnosis (months, IQR) | 2 (0–64) |
| Diagnosis to data collection (years, IQR) | 3 (0–13) |
| Ethnicity | |
| Malay | 133 (68.9) |
| Chinese | 45 (23.3) |
| Indians | 10 (5.2) |
| Others | 5 (2.6) |
| SLICC index at diagnosis | |
| Median (range) score | 20 (1–61) |
| Characteristics | Our Cohort n = 194 (%) |
|---|---|
| Clinical features | |
| Fever | 172 (89.1) |
| Lethargy | 132 (68.4) |
| LOA | 124 (64.2) |
| LOW | 97 (50.3) |
| Alopecia | 80 (41.4) |
| Vasculitic rash | 133 (68.9) |
| Livedo Reticularis | 10 (5.2) |
| Myositis/Myopathy | 53 (27.5) |
| Headache | 37 (19.2) |
| Eye manifestation | 18 (9.3) |
| Hypertension | 52 (26.9) |
| Nephrotic Syndrome | 32 (16.6) |
| Nephritic Syndrome | 21 (10.9) |
| Characteristics | Our Cohort n = 194 (%) |
|---|---|
| Clinical and laboratory features | |
| Acute cutaneous lupus | 124 (64.2) |
| Chronic cutaneous lupus | 25 (13) |
| Oral ulcers | 87 (45.1) |
| Nonscarring alopecia | 78 (40.4) |
| Synovitis | 66 (34.2) |
| Serositis | 32 (16.6) |
| Renal disorder | 66 (34.2) |
| Neurologic | 53 (27.5) |
| Hemolytic anemia | 40 (20.7) |
| Leukopenia or Lymphopenia | 101 (52.3) |
| Thrombocytopenia | 77 (39.9) |
| Immunological features | |
| Anti-nuclear Antibodies | 190 (98.4) |
| Anti-dsDNA antibodies | 141 (73.1) |
| Anti-smith antibodies | 60 (31.1) |
| Low complement | 171 (88.6) |
| Direct Coombs tests | 148 (76.7) |
| Models | Sensitivity (%) | Specificity (%) | Accuracy (%) |
|---|---|---|---|
| SVM-Linear | 93.62 | 27.78 | 75.38 |
| SVM-Radial | 95.74 | 33.33 | 78.46 |
| Knn | 88.89 | 45.00 | 75.38 |
| RF | 91.11 | 50.00 | 78.46 |
| Rpart | 78.72 | 61.11 | 73.85 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lim, S.C.; Chan, E.W.L.; Mandal, S.S.; Tang, S.P. A Preliminary Predictive Model for Proliferative Lupus Nephritis in Juvenile Systemic Lupus Erythematosus. Rheumato 2023, 3, 86-97. https://doi.org/10.3390/rheumato3010007
Lim SC, Chan EWL, Mandal SS, Tang SP. A Preliminary Predictive Model for Proliferative Lupus Nephritis in Juvenile Systemic Lupus Erythematosus. Rheumato. 2023; 3(1):86-97. https://doi.org/10.3390/rheumato3010007
Chicago/Turabian StyleLim, Sern Chin, Elaine Wan Ling Chan, Shikriti Suprakash Mandal, and Swee Ping Tang. 2023. "A Preliminary Predictive Model for Proliferative Lupus Nephritis in Juvenile Systemic Lupus Erythematosus" Rheumato 3, no. 1: 86-97. https://doi.org/10.3390/rheumato3010007
APA StyleLim, S. C., Chan, E. W. L., Mandal, S. S., & Tang, S. P. (2023). A Preliminary Predictive Model for Proliferative Lupus Nephritis in Juvenile Systemic Lupus Erythematosus. Rheumato, 3(1), 86-97. https://doi.org/10.3390/rheumato3010007








