Pachydermoperiostosis Mimicking Inflammatory Arthritis: Case Description and Narrative Review
Abstract
1. Introduction
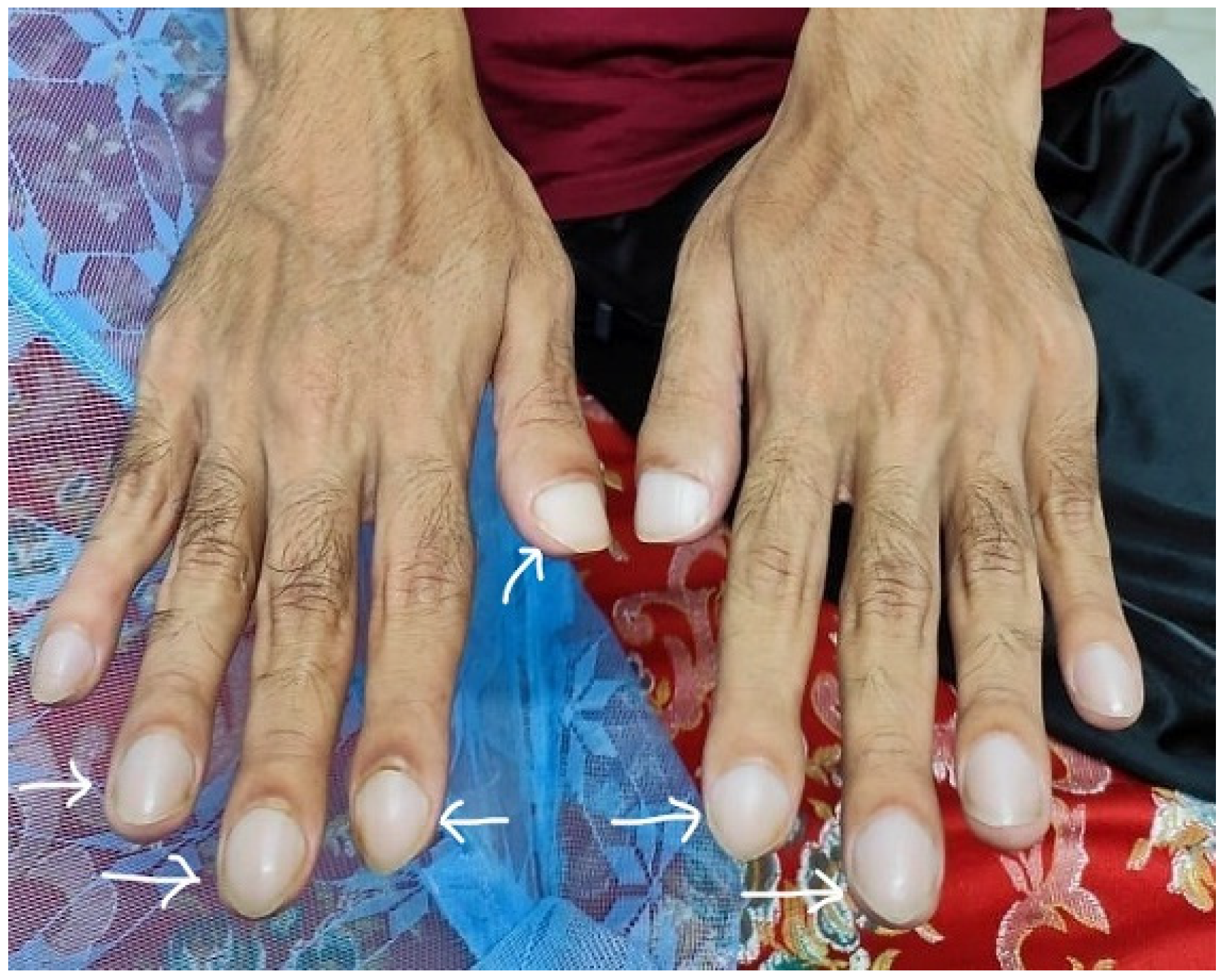
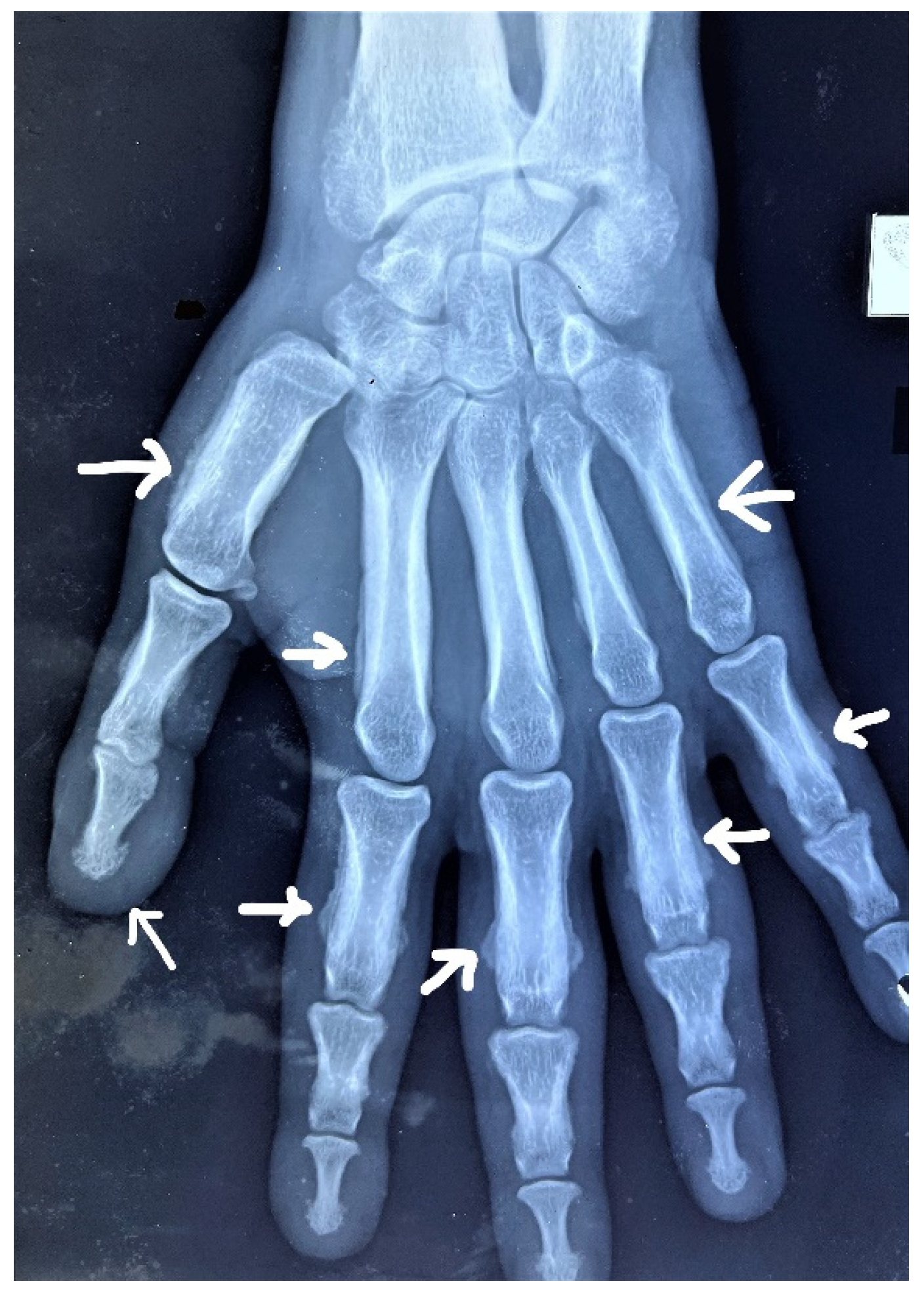
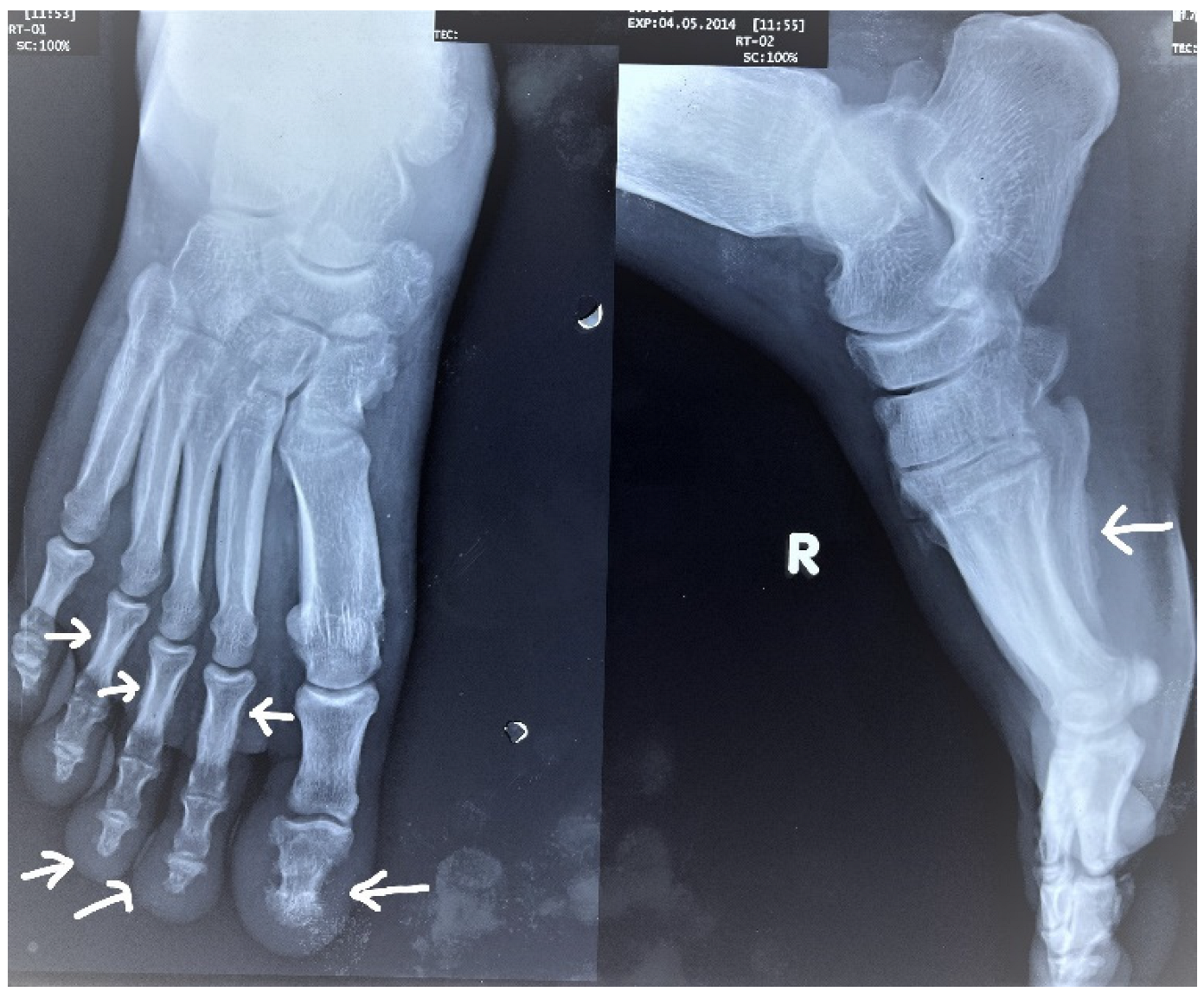
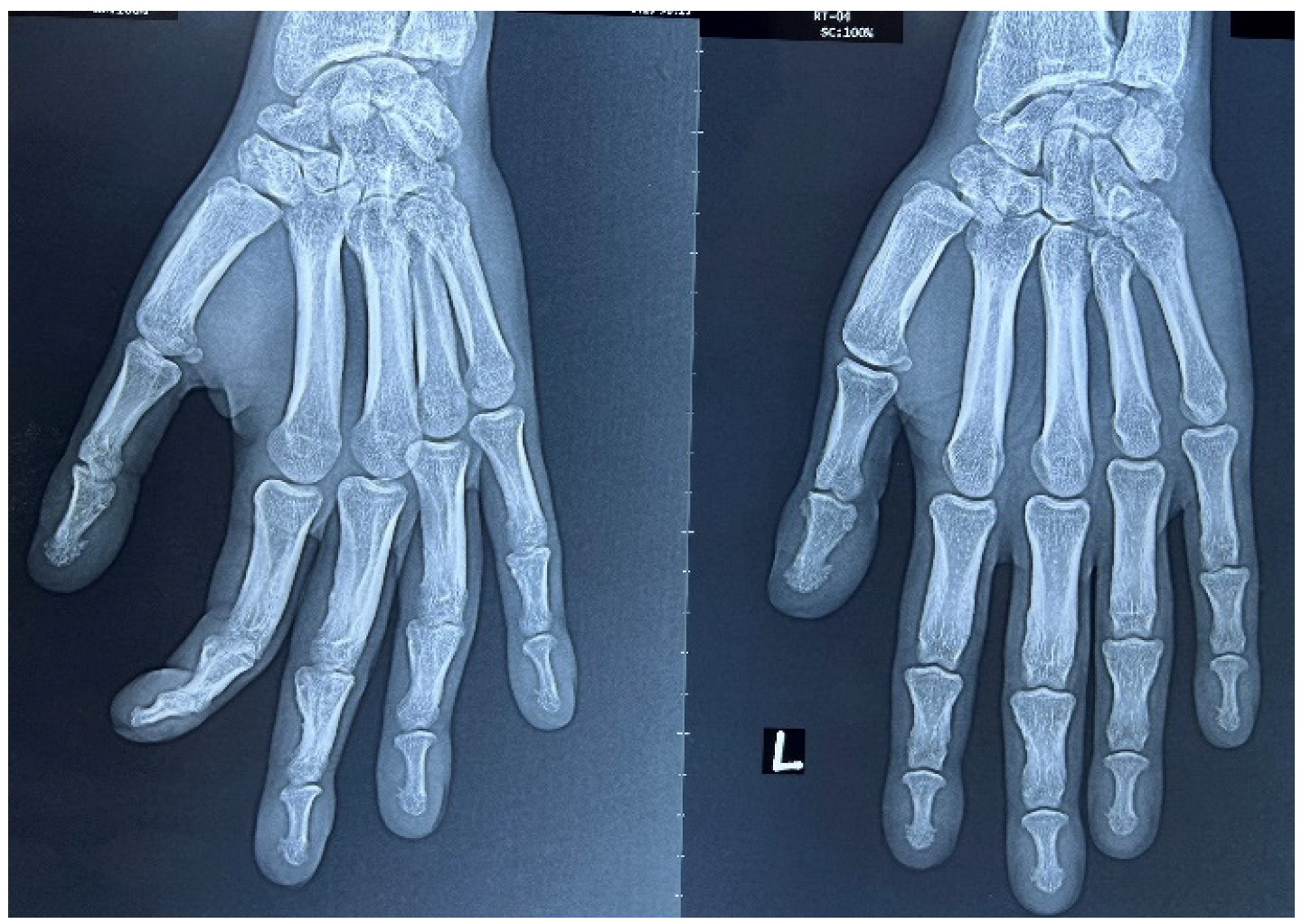
2. Case Report
3. Discussion
3.1. Pathophysiology
3.2. Differential Diagnoses
3.3. Clinical Symptoms and Signs
3.4. Treatment
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Friedreich, N. Hyperostose des gesammten Skelettes. Virchows Arch. 1868, 43, 83–87. [Google Scholar] [CrossRef]
- Touraine, A.; Solente, G.; Gole, L. Un syndrome osteodermopathique: La pachydermie plicaturee avec pachyperiostose des extremités. Presse Med. 1935, 43, 1820–1824. [Google Scholar]
- Castori, M.; Sinibaldi, L.; Mingarelli, R.; Lachman, R.S.; Rimoin, D.L.; Dallapiccola, B. Pachydermoperiostosis: An update. Clin. Genet. 2005, 68, 477–486. [Google Scholar] [CrossRef] [PubMed]
- Ahmmed, M.F.; Shazzad, M.N.; Ferdous, S.; Azad, A.K.; Haq, S.A. Polyarthritis is a Rare Manifestation of Pachydermoperiostosis: A Case Report. Mymensingh Med. J. 2017, 26, 939–943. [Google Scholar]
- Younes, M.; Touzi, M.; Béjia, I.; Zrour-Hassen, S.; Amara, N.; Hammouda, M.B.; Bergaoui, N. Primary hypertrophic osteoarthropathy with bilateral destructive hip arthritis. Jt. Bone Spine 2006, 73, 477–479. [Google Scholar] [CrossRef]
- Herbert, D.A.; Fessel, W.J. Idiopathic hypertrophic osteoarthropathy (pachydermoperiostosis). West. J. Med. 1981, 134, 354–357. [Google Scholar]
- Rodriguez, N.G.; Ruan, J.I.; Perez, M.G. Primary hypertrophic osteoarthropathy (pachydermoperiostosis). Report of two familial cases and literature review. Reum. Clin. 2009, 5, 259–263. (In Spanish) [Google Scholar] [CrossRef]
- Zhang, Z.; Zhang, C.; Zhang, Z. Primary hypertrophic osteoarthropathy: An update. Front. Med. 2013, 7, 60–64. [Google Scholar] [CrossRef]
- Callemeyn, J.; Van Haecke, P.; Peetermans, W.E.; Blockmans, D.E. Clubbing and hypertrophic osteoarthropathy: Insights in diagnosis, pathophysiology, and clinical significance. Acta Clin. Belg. 2016, 71, 123–130. [Google Scholar] [CrossRef]
- Honório, M.L.P.; Bezerra, G.H.; Costa, V.L.D.C. Complete form of pachydermoperiostosis. An. Bras. Dermatol. 2019, 95, 98–101. [Google Scholar] [CrossRef]
- Tanese, K.; Niizeki, H.; Seki, A.; Otsuka, A.; Kabashima, K.; Kosaki, K.; Kuwahara, M.; Miyakawa, S.-I.; Miyasaka, M.; Matsuoka, K.; et al. Pathological characterization of pachydermia in pachydermoperiostosis. J. Dermatol. 2015, 42, 710–714. [Google Scholar] [CrossRef]
- Tanese, K.; Niizeki, H.; Seki, A.; Nakabayashi, K.; Nakazawa, S.; Tokura, Y.; Kawashima, Y.; Kubo, A.; Ishiko, A. Infiltration of mast cells in pachydermia of pachydermoperiostosis (letter to the editor). J. Dermatol. 2017, 44, 1320–1335. [Google Scholar] [CrossRef]
- Hong, C.; Devic, N.; Zavareh, A.; Desai, A.; Ng, N. Pachydermoperiostosis: The Elephant Skin Disease. J. Rheumatol. 2017, 44, 1680–1681. [Google Scholar] [CrossRef]
- Mittal, A.; Gupta, N.; Soneja, M. Touraine-Solente-Gole syndrome. BMJ Case Rep. 2019, 12, e232238. [Google Scholar] [CrossRef]
- Marques, P.; Stelmachowska-Banas, M.; Collier, D.; Wernig, F.; Korbonits, M. Pachydermoperiostosis mimicking the acral abnormalities of acromegaly. Endocrine 2020, 67, 499–500. [Google Scholar] [CrossRef]
- Baykan, E.K.; Türkyilmaz, A. Differential diagnosis of acromegaly: Pachydermoperiostosis two new cases, turkey. J. Clin. Res. Pediatr. Endocrinol. 2022, 14, 350–355. [Google Scholar] [CrossRef]
- Joshi, A.; Nepal, G.; Shing, Y.K.; Panthi, H.P.; Baral, S. Pachydermoperiostosis (Touraine–Solente–Gole syndrome): A case report. J. Med. Case Rep. 2019, 13, 1–6. [Google Scholar] [CrossRef]
- Chakraborty, P.P.; Bhattacharjee, R.; Mukhopadhyay, S.; Chowdhury, S. Pseudoacromegaly in pachydermoperiostosis. BMJ Case Rep. 2016, 2016, bcr2016214624. [Google Scholar] [CrossRef]
- Kloppenburg, M.; Dijkmans, B.A.C.; Rasker, J.J. Effect of therapy for thyroid dysfunction on musculoskeletal symptoms. Clin. Rheumatol. 1993, 12, 341–345. [Google Scholar] [CrossRef]
- Kabi, F.; Mkinsi, O.; Janani, S.; Raissouni, N. Pachydermoperiostosis. A case report. J. Intern. Med. 2006, 27, 710–712. [Google Scholar]
- Prevo, R.L.; Rasker, J.J.; Kruijsen, M.W.M. Sternoclavicular Hyperostosis or Pustulotic Arthroosteitis. J. Rheumatol. 1989, 16, 1602–1605. [Google Scholar] [PubMed]
- Tabatabaei, S.A.; Masoumi, A.; Soleimani, M.; Rafizadeh, S.M.; Salabati, M.; Ahmadraji, A.; Bohrani, B.; Ghahvehchian, H.; Nozarian, Z. Pachydermoperiostosis: A clinicopathological description. J. Curr. Ophthalmol. 2019, 31, 450–453. [Google Scholar] [CrossRef] [PubMed]
- Weerasooriya, N.; Amarasinghe, A.; Punniyamoorthy, L.; Karunatilake, H.; Jayanaga, A. Complete primary pachydermoperiostosis. Ceylon Med. J. 2020, 65, 118. [Google Scholar] [CrossRef] [PubMed]
- Matucci-Cerinic, M.; Fattorini, L.; Gerini, G.; Lombardi, A.; Pignone, A.; Petrini, N.; Lotti, T. Colchicine treatment in a case of pachydermoperiostosis with acroosteolysis. Rheumatol. Int. 1988, 8, 185–188. [Google Scholar] [CrossRef]
- Chen, X.; Yang, C.; Zhang, L.; Hu, Q. Rare gastric manifestations in primary pachydermoperiostosis. Rheumatology 2021, 60, 5481–5482. [Google Scholar] [CrossRef]
- Shin, K.C.; Chung, W.J.; Lee, K.Y.; Shin, M.S.; Kim, S.H.; Jo, Y.J.; Park, Y.M.; Ahn, T.H.; Choi, I.S.; Shin, E.K. Pachydermoperiostosis accompanied by heart failure. J. Cardiovasc. Ultrasound 2009, 17, 135–137. [Google Scholar] [CrossRef]
- Pineda, C.; Martinez-Lavin, M.; Goobar, J.; Sartoris, D.; Clopton, P.; Resnick, D. Periostitis in hypertrophic osteoarthropathy: Relationship to disease duration. Am. J. Roentgenol. 1987, 148, 773–778. [Google Scholar] [CrossRef]
- Jagdish, R.K.; Bhatnagar, M.K.; Malhotra, A.; Aggarwal, R.; Shailly. Bisphosphonates use in Pachydermoperiostosis. J. Assoc. Physicians India 2019, 67, 87–90. [Google Scholar]
- Zhang, H.; Yang, B. Successful treatment of pachydermoperiostosis patients with etoricoxib, aescin, and arthroscopic synovectomy. Medicine 2017, 96, e8865. [Google Scholar] [CrossRef]
- Li, S.-S.; He, J.-W.; Fu, W.-Z.; Liu, Y.-J.; Hu, Y.-Q.; Zhang, Z.-L. Clinical, Biochemical, and Genetic Features of 41 Han Chinese Families With Primary Hypertrophic Osteoarthropathy, and Their Therapeutic Response to Etoricoxib: Results From a Six-Month Prospective Clinical Intervention. J. Bone Miner. Res. 2017, 32, 1659–1666. [Google Scholar] [CrossRef]
- Li, Z.; Yang, Q.; Yang, Y.; Wang, D.; Wang, S. Successful treatment of pachydermoperiostosis with etoricoxib in a patient with a homozygous splice-site mutation in the SLCO2A1 gene. Br. J. Dermatol. 2019, 180, 682–688. [Google Scholar] [CrossRef]
- da Costa, F.V.; Fialho, S.C.D.M.S.; Zimmermann, A.F.; Neves, F.S.; de Castro, G.R.W.; Pereira, I.A. Infliximab Treatment in Pachydermoperiostosis. Am. J. Clin. Oncol. 2010, 16, 183–184. [Google Scholar] [CrossRef]
- Vaidya, B.; Baral, R.; Baral, H.; Nakarmi, S. Inflammatory variant of pachydermoperiostosis responding to methotrexate: A report of two cases. Oxf. Med. Case Rep. 2019, 2019, omy128. [Google Scholar] [CrossRef]
- Yadav, N.; Yanamandra, U. Primary Hypertrophic Osteoarthropathy. N. Engl. J. Med. 2022, 386, e22. [Google Scholar] [CrossRef]
- Guyot-Drouot, M.H.; Solau-Gervais, E.; Cortet, B.; Deprez, X.; Chastanet, P.; Cotten, A.; Delcambre, B.; Flipo, R.M. Rheumatologic manifestations of pachydermoperiostosis and preliminary experience with bisphosphonates. J. Rheumatol. 2000, 27, 2418–2423. [Google Scholar]
- Akrout, R.; Bendjemaa, S.; Fourati, H.; Ezzeddine, M.; Hachicha, I.; Baklouti, S. Hypertrophy of the feet and ankles presenting in primary hypertrophic osteoarthropathy or pachydermoperiostosis: A case report. J. Med. Case Rep. 2012, 6, 31. [Google Scholar] [CrossRef]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kamruzzaman, A.; Farzana, M.; Sohel, M.M.; Kaiser, E.; Chowdhury, N.; Rahman, M.H.; Haq, S.A.; Rasker, J.J. Pachydermoperiostosis Mimicking Inflammatory Arthritis: Case Description and Narrative Review. Rheumato 2023, 3, 98-105. https://doi.org/10.3390/rheumato3010008
Kamruzzaman A, Farzana M, Sohel MM, Kaiser E, Chowdhury N, Rahman MH, Haq SA, Rasker JJ. Pachydermoperiostosis Mimicking Inflammatory Arthritis: Case Description and Narrative Review. Rheumato. 2023; 3(1):98-105. https://doi.org/10.3390/rheumato3010008
Chicago/Turabian StyleKamruzzaman, AKM, Maisha Farzana, Md Mainuddin Sohel, Emrul Kaiser, Nobendu Chowdhury, Md Hafizur Rahman, Syed Atiqul Haq, and Johannes J. Rasker. 2023. "Pachydermoperiostosis Mimicking Inflammatory Arthritis: Case Description and Narrative Review" Rheumato 3, no. 1: 98-105. https://doi.org/10.3390/rheumato3010008
APA StyleKamruzzaman, A., Farzana, M., Sohel, M. M., Kaiser, E., Chowdhury, N., Rahman, M. H., Haq, S. A., & Rasker, J. J. (2023). Pachydermoperiostosis Mimicking Inflammatory Arthritis: Case Description and Narrative Review. Rheumato, 3(1), 98-105. https://doi.org/10.3390/rheumato3010008






