1. Introduction
Burning Mouth Syndrome (BMS) is a chronic orofacial pain condition characterized by a persistent or recurrent burning sensation of the oral mucosa, occurring in the absence of clinically evident lesions or laboratory abnormalities [
1]. The condition predominantly affects women, particularly during peri- and postmenopausal periods, and is frequently accompanied by xerostomia, dysgeusia, and paraesthetic symptoms [
2]. BMS significantly impairs quality of life, contributing to psychological distress, functional limitations, and social isolation [
3].
Despite increased clinical awareness, BMS remains a diagnostic challenge. The diagnosis is fundamentally one of exclusion, necessitating the elimination of local, systemic, and psychological factors [
4]. This complexity contributes to a notable diagnostic delay, with reported averages ranging from one to three years in various populations [
5,
6,
7]. During this period, patients often seek multiple appointments with different doctors, undergo unnecessary investigations, and receive inappropriate treatments, which can exacerbate psychological and physical distress [
5].
The etiology of BMS is multifactorial, with contributions from peripheral and central neuropathic mechanisms, hormonal fluctuations, and psychosocial factors [
1,
4]. Psychiatric comorbidities such as anxiety and depression are frequently reported, and the empirical prescription of psychotropic medications is common in clinical management [
4]. Stress is also frequently identified as a precipitating or aggravating factor [
6]. Emerging evidence suggests that age, education level, and previous psychiatric history may be predictive of longer diagnostic delays [
7].
Given the significant burden of BMS and the implications of diagnostic delay on treatment outcomes, this study aims to characterize diagnostic delays and associated clinical features—including psychotropic drug use and patient-reported triggers—within a Portuguese cohort. This work forms part of a broader doctoral research project.
2. Materials and Methods
A retrospective analysis was conducted using clinical records from 300 patients diagnosed with primary BMS at the Integrated Oral Medicine Clinic (CIMO) in Lisbon. Inclusion criteria included a diagnosis of primary BMS based on the International Classification of Orofacial Pain (ICOP) criteria [
1], age ≥18 years, and complete clinical documentation. Patients with secondary BMS due to local or systemic causes were excluded.
Data collected included sex, age at diagnosis, diagnostic delay (defined as the time from symptom onset to definitive diagnosis), use of psychotropic medications, and self-reported triggering factors. When available, the number of prior appointments and previous diagnoses was also recorded.
Descriptive statistics were used to summarize demographic and clinical characteristics. Associations between variables were assessed using chi-square tests, t-tests, and analysis of variance (ANOVA). A significance threshold of p < 0.05 was adopted for inferential analyses.
3. Results and Discussion
Among the 300 patients, 82.0% were female. The mean age at diagnosis was 60.3 years for women and 56.6 years for men; this difference was not statistically significant (
p = 0.075). The overall prevalence of psychotropic drug use was 33.7%, with a significantly higher prevalence among women (42.7%), compared to men (17.8%;
p = 0.002)—
Table 1.
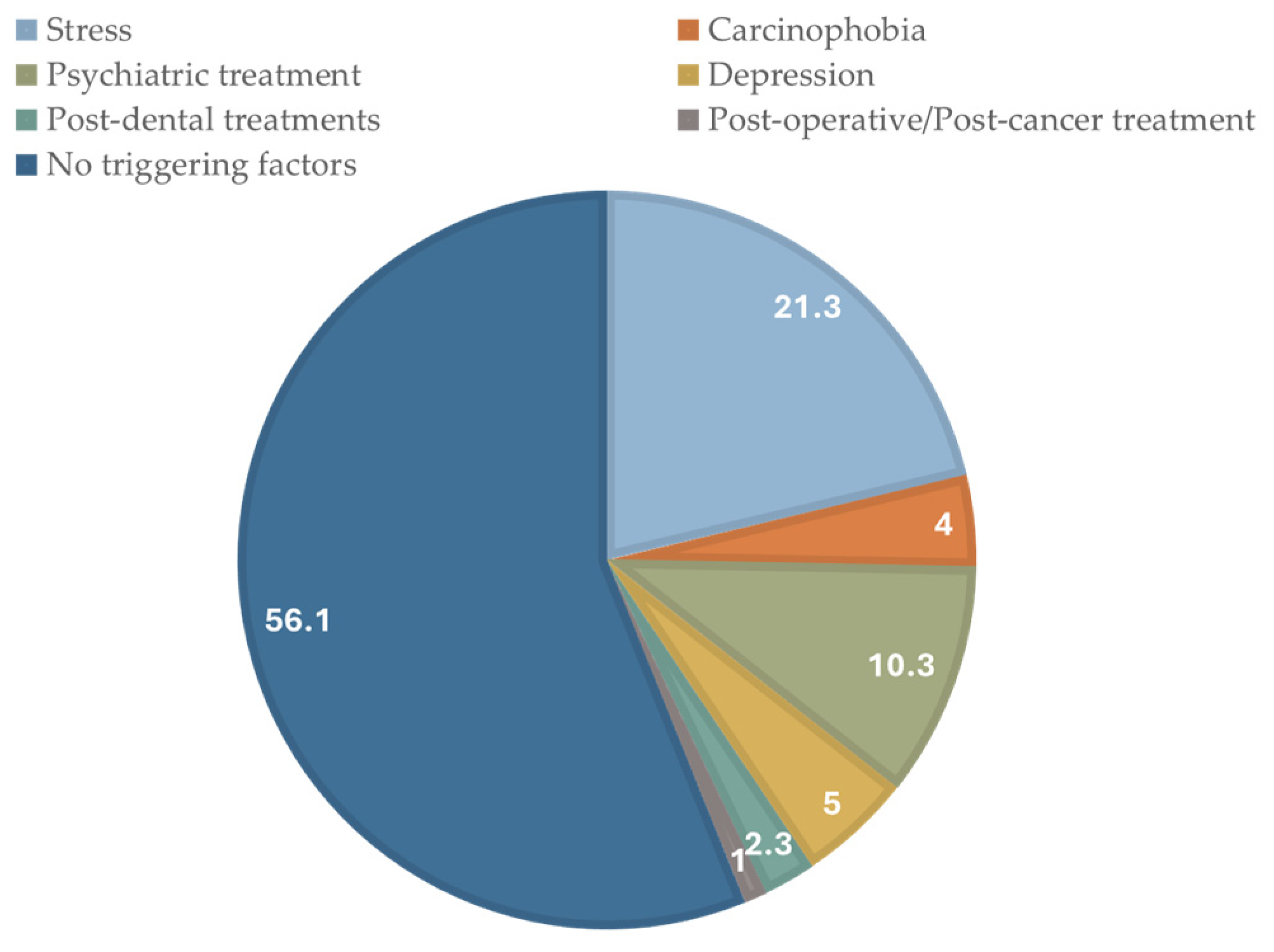
Stress was the most commonly reported trigger (21.3%)—
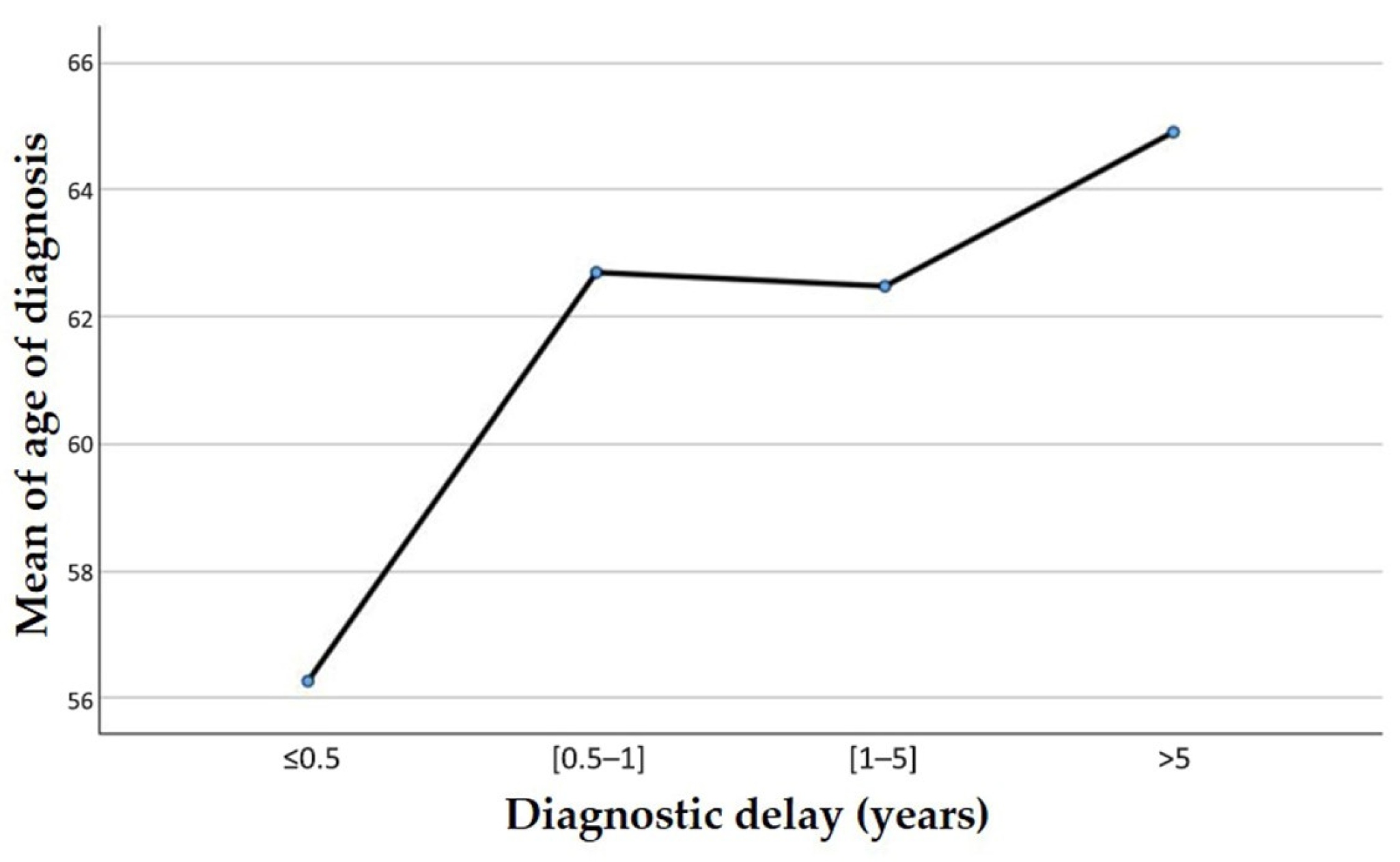
Figure 1. The mean age at diagnosis—
Figure 2—was significantly higher in patients taking psychotropic medications (62.9 years) compared to those not medicated (58.9 years;
p = 0.009).
Age was inversely associated with diagnostic delay: younger patients were more likely to receive an earlier diagnosis (p = 0.021).
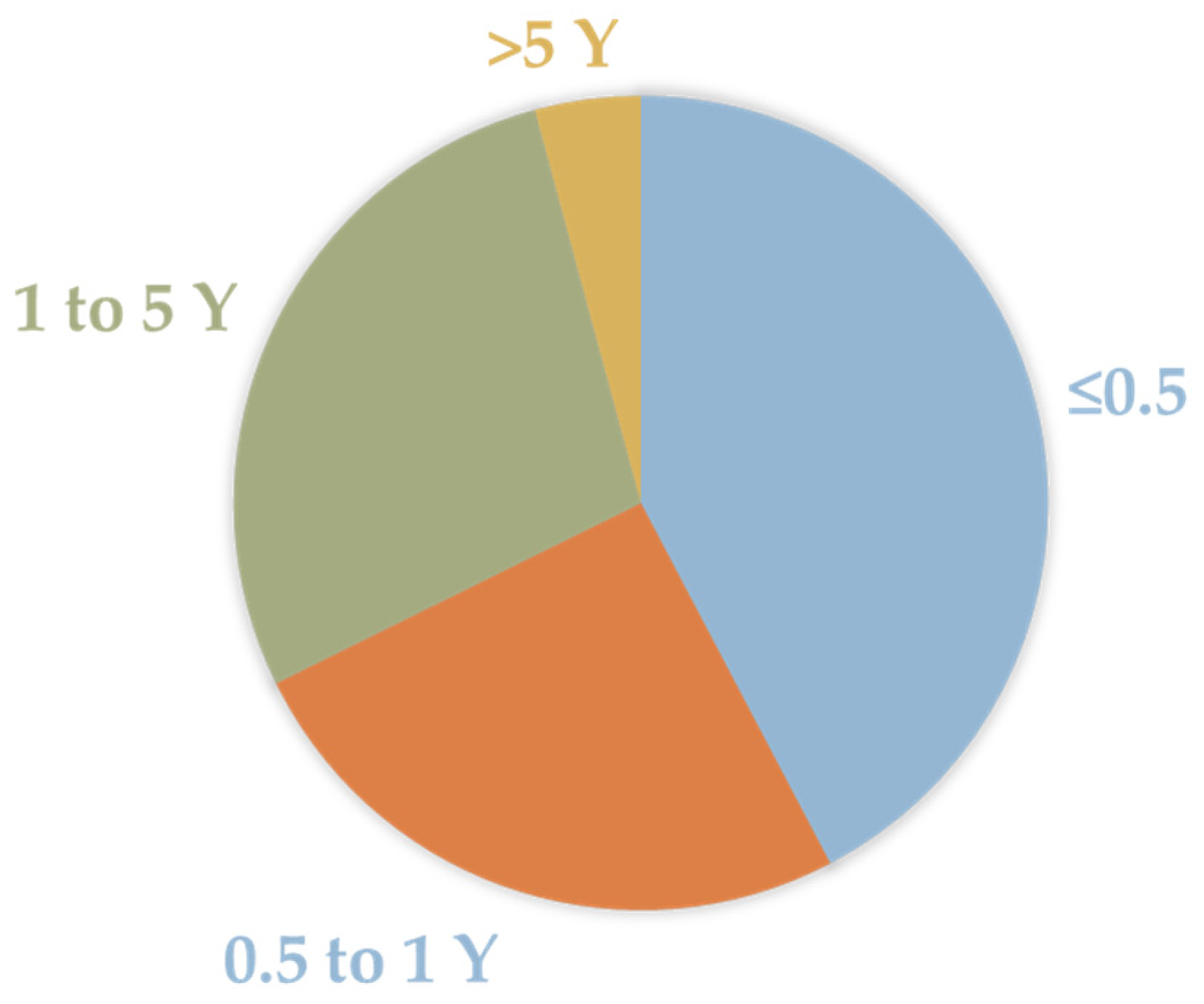
Also, of the 300 patients, 42.31% had a diagnostic delay of under a year and a half (≤0.5 Y). However, most of them had a diagnostic delay of up to 5 years (0.5 to 5 Y)—
Figure 3.
The findings of this preliminary study align with international literature, highlighting a considerable delay in the diagnosis of BMS and frequent misdiagnoses along the diagnostic pathway [
5,
6,
7]. This delay remains a significant clinical challenge, as BMS presents with non-specific symptoms that overlap with other oral and systemic conditions [
3]. A lack of training and awareness among general physicians and dentists, coupled with the exclusion-based nature of the diagnosis, contributes to diagnostic uncertainty and delays [
4]. Additionally, psychotropic medications are commonly prescribed to manage the psychological burden or as part of empirical treatment, although their use often precedes a definitive diagnosis.
Our findings further support the association between older age, psychotropic drug use, and prolonged diagnostic delay, in line with other international reports [
7]. The data also suggest that younger patients may be more rapidly diagnosed, potentially due to more proactive help-seeking behavior or a higher index of suspicion among clinicians for atypical pain syndromes in younger populations.
Diagnostic delay in BMS not only impacts timely management but is also associated with worsened psychological outcomes and reduced responsiveness to interventions [
3]. Patients often express dissatisfaction with their healthcare experiences, reflecting a gap in the delivery of integrated, patient-centered care [
5]. Improving diagnostic timelines requires increased education and awareness among healthcare providers, particularly in primary and dental care settings. Early identification protocols and interdisciplinary referral pathways are critical. Patient education and psychological support should also be integrated into routine care for individuals with BMS [
6].
4. Conclusions
This study confirms a significant diagnostic delay in Portuguese patients with BMS, particularly among older individuals and those using psychotropic medications. These findings underscore the importance of timely recognition and the need for targeted educational strategies among healthcare professionals. A multidisciplinary approach involving dental, medical, and mental health practitioners is essential to improve outcomes, reduce diagnostic delay, and enhance the quality of life for individuals living with BMS.
Author Contributions
Conceptualization, C.Z. and A.M.A.; methodology, M.V.M.; software, L.P.; validation, C.Z., A.M.A. and P.F.T.; formal analysis, L.P.; investigation, M.V.M.; resources, A.M.A. and P.F.T.; data curation, L.P.; writing—original draft preparation, M.V.M.; writing—review and editing, P.F.T., J.G.E. and A.M.A.; visualization, M.V.M.; supervision, A.M.A.; project administration, C.Z.; funding acquisition, M.V.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study due to its retrospective design. All data were fully anonymized, and patients had been previously informed that their clinical information could be used for research purposes.
Informed Consent Statement
Patient consent was waived due to the retrospective nature of the study. All clinical data were analyzed anonymously, and patients had previously been informed that their data could be used for clinical and research purposes.
Data Availability Statement
The datasets presented in this article are not readily available because the data are part of an ongoing study. Requests to access the datasets should be directed to the corresponding authors.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- International Headache Society. International Classification of Orofacial Pain, 1st edition (ICOP). Cephalalgia 2020, 40, 129–221. [Google Scholar] [CrossRef] [PubMed]
- Ni Riordain, R.; O’Dwyer, S.; McCreary, C. Burning mouth syndrome—A diagnostic dilemma. Br. Dent. J. 2019, 226, 835–840. [Google Scholar] [CrossRef] [PubMed]
- Mignogna, M.D.; Fedele, S.; Lo Russo, L.; Adamo, D.; Satriano, R.A. Burning mouth syndrome: A review on diagnosis and management. Oral. Dis. 2022, 28, 5–16. [Google Scholar] [CrossRef]
- Galli, F.; Lodi, G.; Sardella, A.; Macchiarelli, G.; Manfredi, M.; Fedele, S.; Carrara, G.; Rossi, R.; Tarsitani, L. Psychological factors in burning mouth syndrome: A systematic review. J. Oral. Rehabil. 2023, 50, 679–692. [Google Scholar] [CrossRef]
- Adamo, D.; Calabria, E.; Canfora, F.; Coppola, N.; Pecoraro, G.; D’Aniello, L.; Aria, M.; Mignogna, M.D.; Leuci, S. Burning mouth syndrome: Analysis of diagnostic delay in 500 patients. Oral. Dis. 2024, 30, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Patil, S.; Patil, P. Burning mouth syndrome: A review. J Family Med. Prim Care 2021, 10, 2751–2756. [Google Scholar] [CrossRef]
- McMillan, R.; Forssell, H.; Buchanan, J.A.; Glenny, A.M.; Zakrzewska, J.M.; Aggarwal, V.R. Interventions for treating burning mouth syndrome. Cochrane Database Syst Rev. 2016, 11, CD002779. [Google Scholar] [CrossRef] [PubMed]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).