The Association of the Global Climate Crisis with Environmental Risks and the Impact of Heat Stress on Occupational Safety, Health, and Hygiene †
Abstract
:1. Introduction
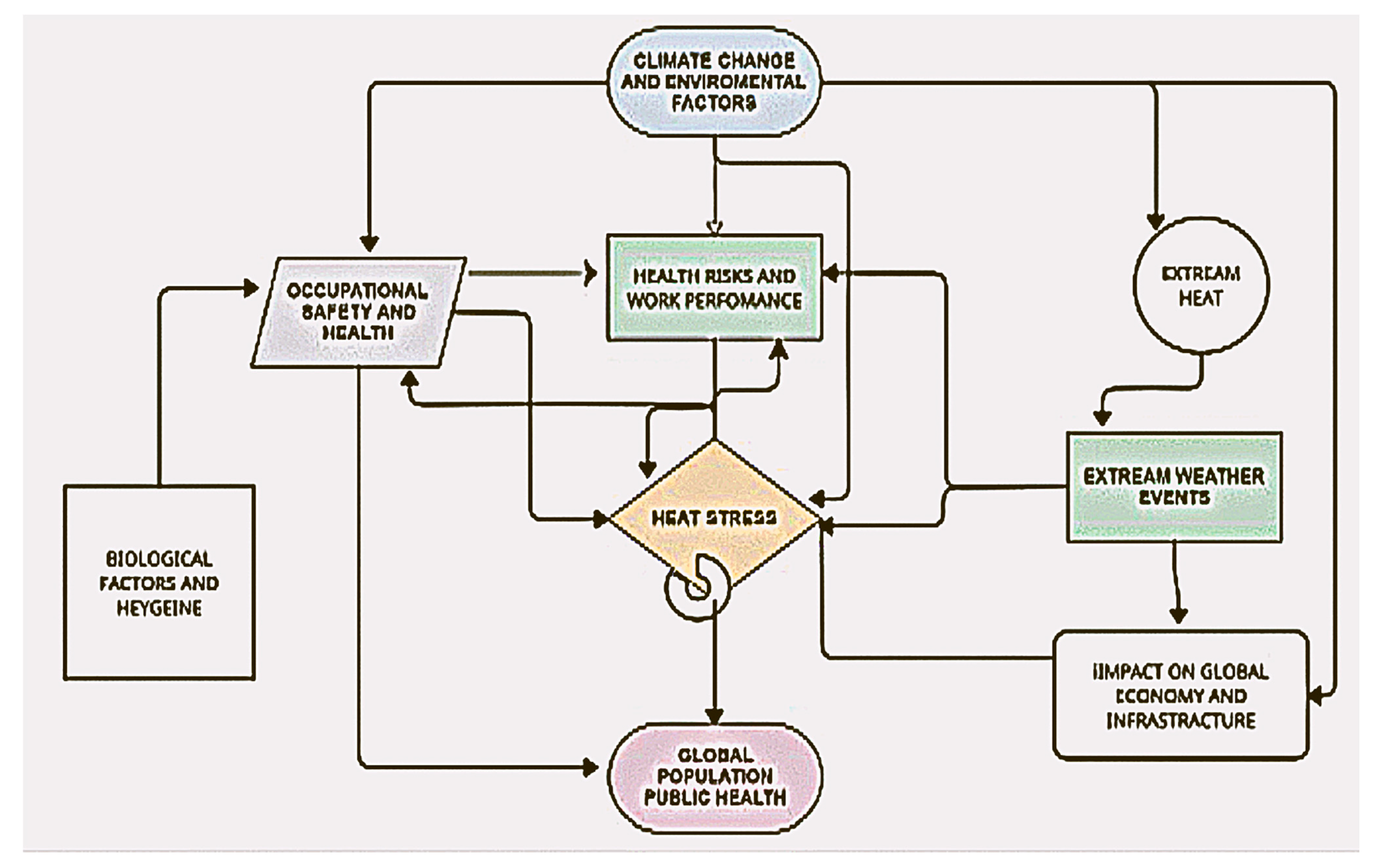
1.1. Climate Change and Occupational Health Risks
- Increased exposure to vector-borne diseases (e.g., malaria, dengue) in tropical and subtropical regions due to expanding insect populations [7].
- Respiratory diseases caused by air pollution and wildfire smoke, leading to higher rates of chronic lung conditions among outdoor workers [8].
- Physical injuries from extreme weather events (e.g., hurricanes, floods, and wildfires), increasing workplace accident rates and mortality [9].
1.2. Research Hypothesis
1.3. Study Objectives and Scope
- Analyze the relationship between climate change-induced environmental hazards and occupational health outcomes.
- Evaluate the effectiveness of existing workplace safety measures in mitigating climate-induced risks.
- Identify policy gaps in occupational safety frameworks and propose evidence-based improvements.
- Develop a structured risk assessment framework to assess the interaction between climate change, occupational health risks, and labor productivity.
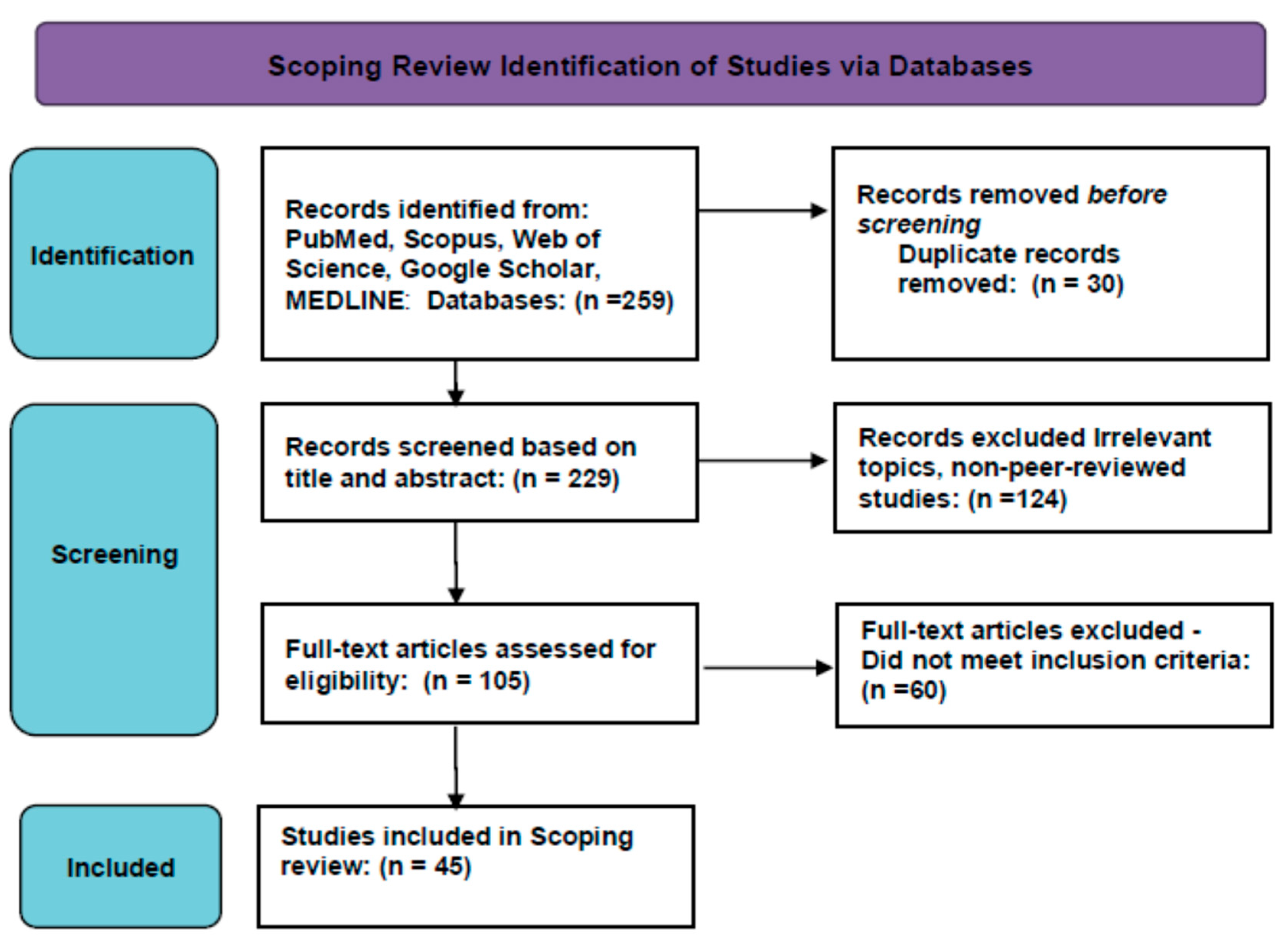
2. Materials and Methods
2.1. Study Design
2.2. Data Sources and Search Strategy
- (“Climate Change” OR “Global Warming”) AND (“Occupational Health” OR “Heat Stress” OR “Workplace Safety”);
- (“Extreme Weather Events”) AND (“Public Health Inspectors” OR “Workplace Regulations”);
- (“Air Pollution” OR “Heat-Related Illnesses”) AND (“Occupational Risks”).
2.3. Inclusion and Exclusion Criteria
2.3.1. Inclusion Criteria
- Publication Type: Peer-reviewed articles, systematic reviews, and meta-analyses.
- Population: Studies analyzing workers in heat-intensive environments (e.g., agriculture, construction, and emergency response).
- Language: Articles published in English.
- Study Period: Research published between 2014 and 2024.
2.3.2. Exclusion Criteria
- Studies without full-text access.
- Articles focused solely on general climate change effects without occupational health aspects [18].
- Research on non-human subjects or laboratory-based experiments.
- Duplicates or preliminary studies without peer review.
2.4. Data Extraction and Analysis
- Study Location: Geographic region.
- Sample Size: Number of participants.
- Key Findings: Major conclusions.
- Statistical Methods: Analytical techniques applied [19].
2.5. Mathematical Models for Heat Stress Assessment
Wet Bulb Globe Temperature (WBGT) Index
- Formula for Indoor Workplaces (Without Solar Radiation):
- ⭘
- = Natural wet bulb temperature;
- ⭘
- = Globe temperature.
- Formula for Outdoor Workplaces (Including Solar Radiation):
- ⭘
- = Air temperature (insulated from direct radiation) [23].
3. Results
- Identified key occupational health risks associated with climate change.
- Summarized and categorized different workplace hazards.
- Provided insights into policy gaps and future research directions.
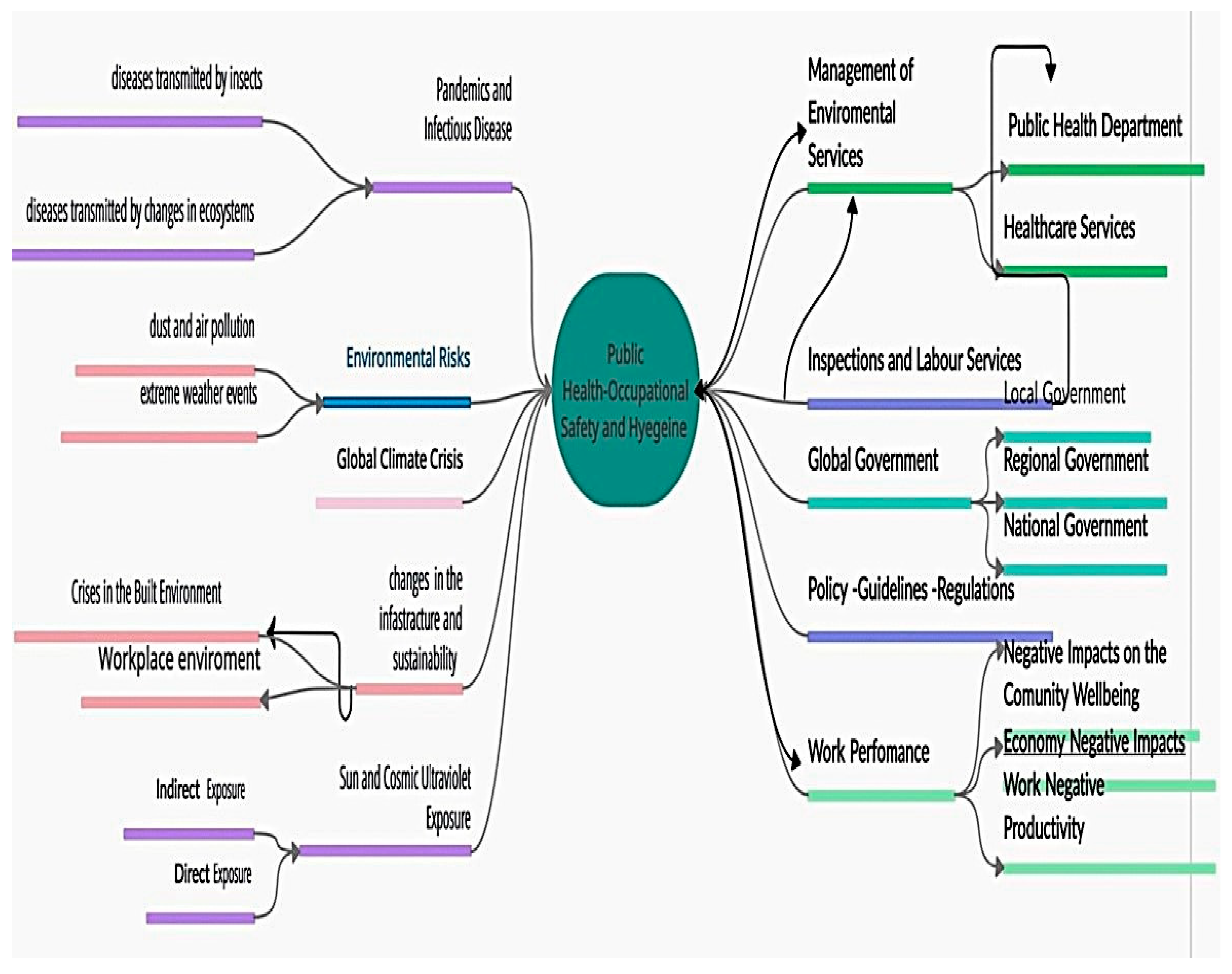
3.1. Categories of Climate-Related Occupational Hazards
- Dust and air pollution → Respiratory diseases and lung damage [26].
- Sun and UV exposure → Skin cancer and vision impairment [27].
- Infectious diseases → Higher incidence of vector-borne illnesses [28].
- Vector-related disease transmission → Expansion of insect-borne illnesses [29].
- Industrial diseases → Aggravated by climate-driven environmental shifts [30].
- Extreme weather → Increased workplace accidents and fatalities [31].
- Built environment risks → Infrastructure instability due to climate stress [32].
3.2. Public Health and Workplace Regulations
4. Discussion
4.1. Study Limitations and Future Research Directions
4.2. Future Research Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Schulte, P.A.; Chun, H. Climate change and occupational safety and health: Establishing a preliminary framework. J. Occup. Environ. Hyg. 2009, 6, 542–554. [Google Scholar] [CrossRef]
- Lucas, R.A.I.; Epstein, Y.; Kjellstrom, T. Excessive occupational heat exposure: A significant ergonomic challenge and health risk for current and future workers. Extrem. Physiol. Med. 2014, 3, 14. [Google Scholar] [CrossRef]
- Kjellstrom, T.; Lemke, B.; Otto, M. Mapping occupational heat exposure and effects in South-East Asia: Ongoing time trends 1980–2011 and future estimates to 2050. Ind. Health 2013, 51, 56–67. [Google Scholar] [CrossRef]
- Jay, O.; Bain, A.R.; Deren, T.M.; Sacheli, M.; Cramer, M.N. Large differences in peak oxygen uptake do not independently alter changes in core temperature and sweating during exercise. Am. J. Physiol-Regul. Integ Comp. Physiol. 2011, 301, R832–R841. [Google Scholar] [CrossRef]
- Zander, K.K.; Moss, S.; Garnett, S.T. Climate Change–Related Heat Stress and Subjective Well-Being in Australia. Weather. Clim. Soc. 2019, 11, 505–520. [Google Scholar] [CrossRef]
- Parsons, K. Human Thermal Environments: The Effects of Hot, Moderate, and Cold Environments on Human Health, Comfort and Performance, 2nd ed.; CRC Press: London, UK, 2002. [Google Scholar] [CrossRef]
- Adamopoulos, I.; Syrou, N.; Lamnisos, D.; Boustras, G. Cross-sectional nationwide study in occupational safety & health: Inspection of job risks context, burn out syndrome and job satisfaction of public health Inspectors in the period of the COVID-19 pandemic in Greece. Saf. Sci. 2023, 158, 105960. [Google Scholar] [CrossRef]
- Adamopoulos, I.P. Job Satisfaction in Public Health Care Sector, Measures Scales and Theoretical Background. Eur. J. Environ. Public Health 2022, 6, em0116. [Google Scholar] [CrossRef]
- Adamopoulos, I.; Lamnisos, D.; Syrou, N.; Boustras, G. Public health and work safety pilot study: Inspection of job risks, burn out syndrome and job satisfaction of public health inspectors in Greece. Saf. Sci. 2022, 147, 105592. [Google Scholar] [CrossRef]
- Adamopoulos, I.; Frantzana, A.; Syrou, N. Climate Crises Associated with Epidemiological, Environmental, and Ecosystem Effects of a Storm: Flooding, Landslides, and Damage to Urban and Rural Areas (Extreme Weather Events of Storm Daniel in Thessaly, Greece). Med. Sci. Forum 2024, 25, 7. [Google Scholar] [CrossRef]
- Adamopoulos, I.; Frantzana, A.; Adamopoulou, J.; Syrou, N. Climate Change and Adverse Public Health Impacts on Human Health and Water Resources. Environ. Sci. Proc. 2023, 26, 178. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- NIOSH. NIOSHcriteria for a Recommended Standard: Occupational Exposure to Heat Hot Environments; Jacklitsch, B., Williams, W.J., Musolin, K., Coca, A., Kim, J.-H., Turner, N., Cincinnati, O.H., Eds.; U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, DHHS (NIOSH) Publication: Cincinnati, OH, USA, 2016; p. 106. [Google Scholar]
- Lemke, B.; Kjellstrom, T. Calculating workplace WBGT from meteorological data: A tool for climate change assessment. Ind. Health 2012, 50, 267–278. [Google Scholar] [CrossRef] [PubMed]
- Parsons, K. Occupational health impacts of climate change: Current and future ISO standards for the assessment of heat stress. Ind. Health 2013, 51, 86–100. [Google Scholar] [CrossRef]
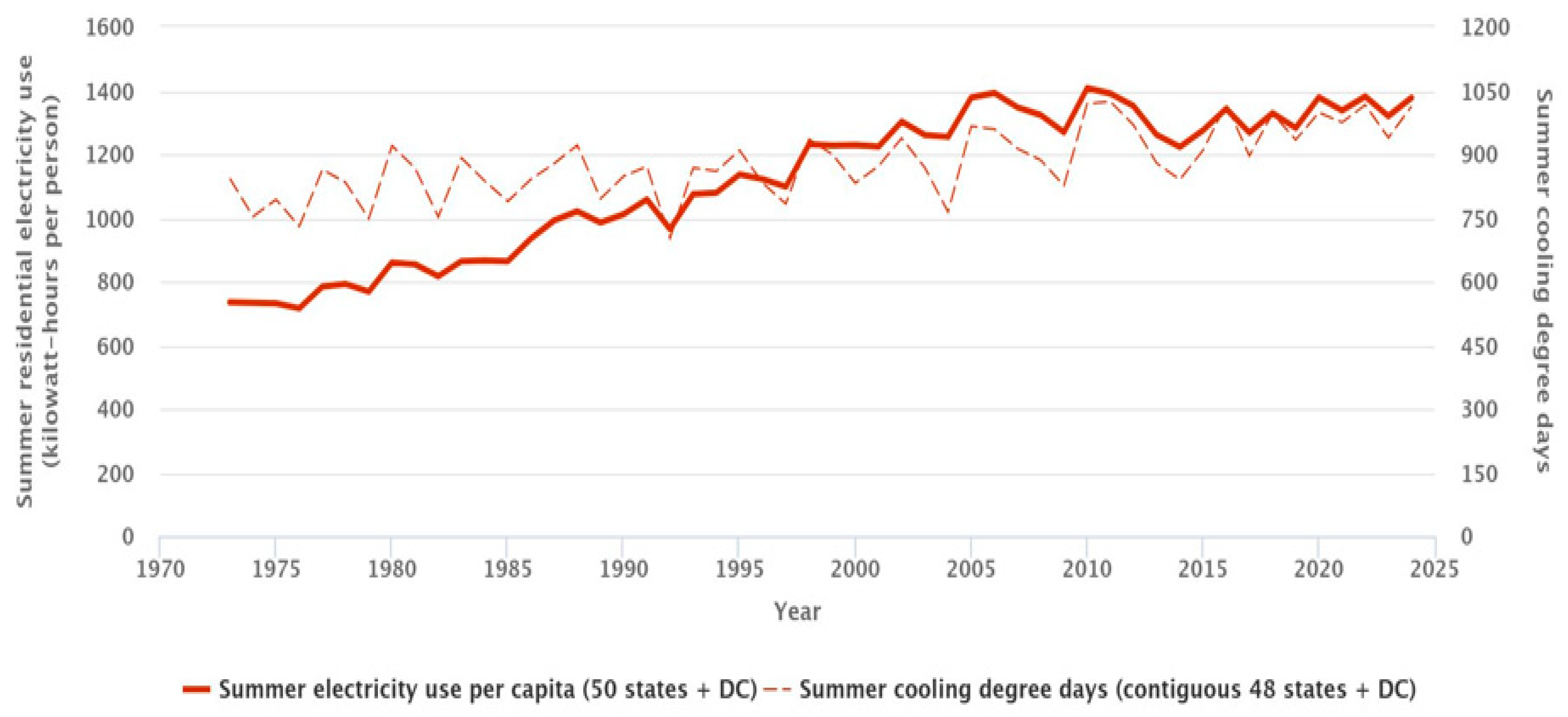
- Climate Change Indicators: Residential Energy Use. Available online: https://www.epa.gov/climate-indicators/climate-change-indicators-residential-energy-use (accessed on 20 May 2025).
- Melaku, C.; Abere, G.; Zele, Y.T.; Mamaye, Y.; Mekonen, T.A.; Bezie, A.E.; Tesfaye, A.H.; Worede, E.A. The Occupational Heat Exposure-related Symptoms prevalence and Associated Factors among Hospitality Industry Kitchen Workers in Ethiopia: Wet Bulb Globe Temperature. Saf. Health Work. 2024, 15, 472–480. [Google Scholar] [CrossRef]
- The US Department of Labor. Campaign to Prevent Heat Illness in Outdoor Workers. 2011. Available online: https://www.osha.gov/SLTC/heatillness/index.html (accessed on 7 October 2024).
- Levy; Barry, S.; Cora, R. Impacts of Climate Change on Workers’ Health and Safety. In Oxford Research Encyclopedia of Global Public Health; Oxford University Press: Oxford, UK, 2019; Available online: https://oxfordre.com/publichealth/view/10.1093/acrefore/9780190632366.001.0001/acrefore-9780190632366-e-39 (accessed on 12 October 2024).
- Butler-Dawson, J.; Erlandson, G.; Jaramillo, D.; Calvimontes, L.; Pilloni, D.; Seidel, J.; Castro, C.; Villarreal Hernandez, K.; Krisher, L.; Brindley, S.; et al. Concurrent Particulate Matter and Heat Exposure in Working and Non-Working Women in Rural Guatemala. Atmosphere 2024, 15, 1175. [Google Scholar] [CrossRef]
- Xiang, J.; Hansen, A.; Pisaniello, D.; Bi, P. Perceptions of Workplace Heat Exposure and Controls among Occupational Hygienists and Relevant Specialists in Australia. PLoS ONE 2015, 10, e0135040. [Google Scholar] [CrossRef]
- Jessel, S.; Sawyer, S.; Hernández, D. Energy, Poverty, and Health in Climate Change: A Comprehensive Review of an Emerging Literature. Front. Public Health 2019, 7, 357. [Google Scholar] [CrossRef]
- Manisalidis, I.; Stavropoulou, E.; Stavropoulos, A.; Bezirtzoglou, E. Environmental and Health Impacts of Air Pollution: A Review. Front. Public Health 2020, 8, 14. [Google Scholar] [CrossRef]
- Spector, J.T.; Sheffield, P.E. Re-evaluating Occupational Heat Stress in a Changing Climate. Ann. Occup. Hyg. 2014, 58, 936–942. [Google Scholar] [CrossRef]
- Idris, M.A.; Markham, C.; Mena, K.D.; Perkison, W.B. Examining Management and Employees’ Perceptions of Occupational Heat Exposure and the Effectiveness of a Heat Stress Prevention Intervention on Safety and Well-Being among Natural Gas Construction Workers: A Qualitative Field-Based Study. Int. J. Environ. Res. Public Health 2024, 21, 1255. [Google Scholar] [CrossRef]
- World Health Organization. Climate Change and Health. 2018. Available online: https://www.who.int/news-room/fact-sheets/detail/climate-change-and-health (accessed on 10 October 2024).
- Wunderlich, K.; Suppa, M.; Gandini, S.; Lipski, J.; White, J.M.; Del Marmol, V. Risk Factors and Innovations in Risk Assessment for Melanoma, Basal Cell Carcinoma, and Squamous Cell Carcinoma. Cancers 2024, 16, 1016. [Google Scholar] [CrossRef] [PubMed]
- Intergovernmental Panel on Climate Change (IPCC). Climate Change 2014: Impacts, Adaptation, and Vulnerability; Fifth Assessment Report; IPCC: Geneva, Switzerland, 2014. [Google Scholar]
- Smith, K.R.; Frumkin, H.; Balakrishnan, K.; Butler, C.D.; Chafe, Z.A.; Fair, K.; Kinney, P. Energy and human health. Annu. Rev. Public health 2016, 37, 139–154. [Google Scholar] [CrossRef]
- World Health Organization. Ambient (Outdoor) Air Quality and Health. 2018. Available online: https://www.who.int/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health (accessed on 9 October 2024).
- Buonocore, J.J. The health impacts of energy consumption and air pollution. J. Air Waste Manag. Assoc. 2016, 66, 649–676. [Google Scholar]
- Adamopoulos, I.P.; Frantzana, A.A.; Syrou, N.F. Epidemiological surveillance and environmental hygiene, SARS-CoV-2 infection in the community, urban wastewater control in Cyprus, and water reuse. J. Contemp. Stud. Epidemiol. Public Health 2023, 4, ep23003. [Google Scholar] [CrossRef]
- Adamopoulou, J.P.; Frantzana, A.A.; Adamopoulos, I.P. Addressing water resource management challenges in the context of climate change and human influence. Eur. J. Sustain. Dev. Res. 2023, 7, em0223. [Google Scholar] [CrossRef]
- Adamopoulos, I.; Syrou, N.; Lamnisos, D.; Dounias, G. Public Health Inspectors Classification and Assessment of Environmental, Psychosocial, Organizational Risks and Workplace Hazards in the Context of the Global Climate Crisis. Preprints 2024. [Google Scholar] [CrossRef]
- Adamopoulos, I.P.; Syrou, N.F.; Adamopoulou, J.P. Greece’s current water and wastewater regulations and the risks they pose to environmental hygiene and public health, as recommended by the European Union Commission. Eur. J. Sustain. Dev. Res. 2024, 8, em0251. [Google Scholar] [CrossRef]
- Adamopoulos, I.P.; Lamnisos, D.; Syrou, N.F.; Boustras, G. Inspection of job risks, burn out syndrome and job satisfaction of Greek public health inspectors. Saf. Health Work 2022, 13, S294. [Google Scholar] [CrossRef]
- Adamopoulos, I.P.; Bardavouras, A.N.; Syrou, N.F. Occupational safety, policy, and management in public health organizations and services. Eur. J. Environ. Public Health 2023, 7, em0122. [Google Scholar] [CrossRef]
- Abokhashabah, T.; Jamoussi, B.; Summan, A.S.; Abdelfattah, E.; Ahmad, I. Effects of Heat Stress Exposure and Climate Change on Health and Safety of Outdoor Workers. Curr. World Environ. 2021, 16, 836–847. [Google Scholar] [CrossRef]
- Patil, M.; Jeffery, K.J. What does climate change mean for occupational health professionals? Occup. Med. 2020, 70, 386–388. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7566748/ (accessed on 12 October 2024). [CrossRef] [PubMed]
- Smith, K.R.; Corvalan, C.F.; Kjellstrom, T. How much global ill health is attributable to environmental factors? Epidemiology 1999, 10, 573–584. [Google Scholar] [CrossRef] [PubMed]
- Park, C.Y.; Lee, D.K.; Hyun, J.H. The Effects of Extreme Heat Adaptation Strategies under Different Climate Change Mitigation Scenarios in Seoul, Korea. Sustainability 2019, 11, 3801. [Google Scholar] [CrossRef]
- Meier, B.M.; Bustreo, F.; Gostin, L.O. Climate Change, Public Health and Human Rights. Int. J. Environ. Res. Public Health 2022, 19, 13744. [Google Scholar] [CrossRef]
- El Khayat, M.; Halwani, D.A.; Hneiny, L.; Alameddine, I.; Haidar, M.A.; Habib, R.R. Impacts of Climate Change and Heat Stress on Farmworkers’ Health: A Scoping Review. Front. Public Health 2022, 10, 782811. [Google Scholar] [CrossRef]
- OSHA Heat: Prevention. Water. Rest. Shade. Available online: https://www.osha.gov/heat-exposure/water-rest-shade (accessed on 2 October 2024).
- Bethel, J.W.; Harger, R. Heat-related illness among Oregon farmworkers. Int. J. Environ. Res. Public Health 2014, 11, 9273–9285. [Google Scholar] [CrossRef]
- Mix, J.; Elon, L.; Vi Thien Mac, V.; Flocks, J.; Economos, E.; Tovar-Aguilar, A.J.; Hertzberg, V.S.; McCauley, L.A. Hydration Status, Kidney Function, and Kidney Injury in Florida Agricultural Workers. J. Occup. Environ. Med. 2018, 60, e253–e260. [Google Scholar] [CrossRef]
- Spector, J.T.; Krenz, J.; Blank, K.N. Risk Factors for Heat-Related Illness in Washington Crop Workers. J. Agromed. 2015, 20, 349–359. [Google Scholar] [CrossRef]
- Arcury, T.A.; Summers, P.; Talton, J.W.; Chen, H.; Sandberg, J.C.; Spears Johnson, C.R.; Quandt, S.A. Heat Illness Among North Carolina Latino Farmworkers. J. Occup. Environ. Med. 2015, 57, 1299–1304. [Google Scholar] [CrossRef]
- Riccò, M.; Vezzosi, L.; Bragazzi, N.L.; Balzarini, F. Heat-Related Illnesses among Pesticide Applicators in North-Eastern Italy (2017). J. Agromed. 2020, 25, 52–64. [Google Scholar] [CrossRef]
- Han, S.R.; Wei, M.; Wu, Z.; Duan, S.; Chen, X.; Yang, J.; Borg, M.A.; Lin, J.; Wu, C.; Xiang, J. Perceptions of workplace heat exposure and adaption behaviors among Chinese construction workers in the context of climate change. BMC Public Health 2021, 21, 2160. [Google Scholar] [CrossRef] [PubMed]
- Glaser, J.; Hansson, E.; Weiss, I.; Wesseling, C.; Jakobsson, K.; Ekström, U.; Apelqvist, J. Preventing kidney injury among sugarcane workers: Promising evidence from enhanced workplace interventions. Occup. Environ. Med. 2020, 77, 527–534. [Google Scholar] [CrossRef]
- Butler-Dawson, J.; Krisher, L.; Yoder, H.; Dally, M.; Sorensen, C.; Johnson, R.J.; Asensio, C. Evaluation of heat stress and cumulative incidence of acute kidney injury in sugarcane workers in Guatemala. Int. Arch. Occup. Environ. Health 2019, 92, 977–990. [Google Scholar] [CrossRef]
- Luque, J.S.; Becker, A.; Bossak, B.H.; Grzywacz, J.G.; Tovar-Aguilar, J.A.; Guo, Y. Knowledge and Practices to Avoid Heat-Related Illness among Hispanic Farmworkers along the Florida-Georgia Line. J. Agromed. 2020, 25, 190–200. [Google Scholar] [CrossRef]
- Wegman, D.H.; Apelqvist, J.; Bottai, M.; Ekström, U.; García-Trabanino, R.; Glaser, J.; Hogstedt, C. Intervention to diminish dehydration and kidney damage among sugarcane workers. Scand. J. Work. Environ. Health 2018, 44, 16–24. [Google Scholar] [CrossRef]
- Kearney, G.D.; Hu, H.; Xu, X.; Hall, M.B.; Balanay, J.A.G. Estimating the Prevalence of Heat-Related Symptoms and Sun Safety-Related Behavior among Latino Farmworkers in Eastern North Carolina. J. Agromed. 2016, 21, 15–23. [Google Scholar] [CrossRef]
- Gao, C.; Kuklane, K.; Östergren, P.O.; Kjellstrom, T. Occupational heat stress assessment and protective strategies in the context of climate change. Int. J. Biometeorol. 2018, 62, 359–371. [Google Scholar] [CrossRef]
- Adamopoulos, I.; Valamontes, A.; Tsirkas, P.; Dounias, G. Predicting Workplace Hazard, Stress and Burnout Among Public Health Inspectors: An AI-Driven Analysis in the Context of Climate Change. Eur. J. Investig. Health Psychol. Educ. 2025, 15, 65. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adamopoulos, I.; Syrou, N.; Mpourazanis, G.; Constantinidis, T.C.; Dounias, G. The Association of the Global Climate Crisis with Environmental Risks and the Impact of Heat Stress on Occupational Safety, Health, and Hygiene. Med. Sci. Forum 2025, 33, 2. https://doi.org/10.3390/msf2025033002
Adamopoulos I, Syrou N, Mpourazanis G, Constantinidis TC, Dounias G. The Association of the Global Climate Crisis with Environmental Risks and the Impact of Heat Stress on Occupational Safety, Health, and Hygiene. Medical Sciences Forum. 2025; 33(1):2. https://doi.org/10.3390/msf2025033002
Chicago/Turabian StyleAdamopoulos, Ioannis, Niki Syrou, George Mpourazanis, Theodoros C. Constantinidis, and George Dounias. 2025. "The Association of the Global Climate Crisis with Environmental Risks and the Impact of Heat Stress on Occupational Safety, Health, and Hygiene" Medical Sciences Forum 33, no. 1: 2. https://doi.org/10.3390/msf2025033002
APA StyleAdamopoulos, I., Syrou, N., Mpourazanis, G., Constantinidis, T. C., & Dounias, G. (2025). The Association of the Global Climate Crisis with Environmental Risks and the Impact of Heat Stress on Occupational Safety, Health, and Hygiene. Medical Sciences Forum, 33(1), 2. https://doi.org/10.3390/msf2025033002







