Heat Waves and Cardiovascular Events in Milan, Italy: A Geospatial Case-Crossover Approach Using Data from Emergency Medical Services †
Abstract
1. Introduction
2. Methodology
2.1. Data
2.2. Statistical Methods
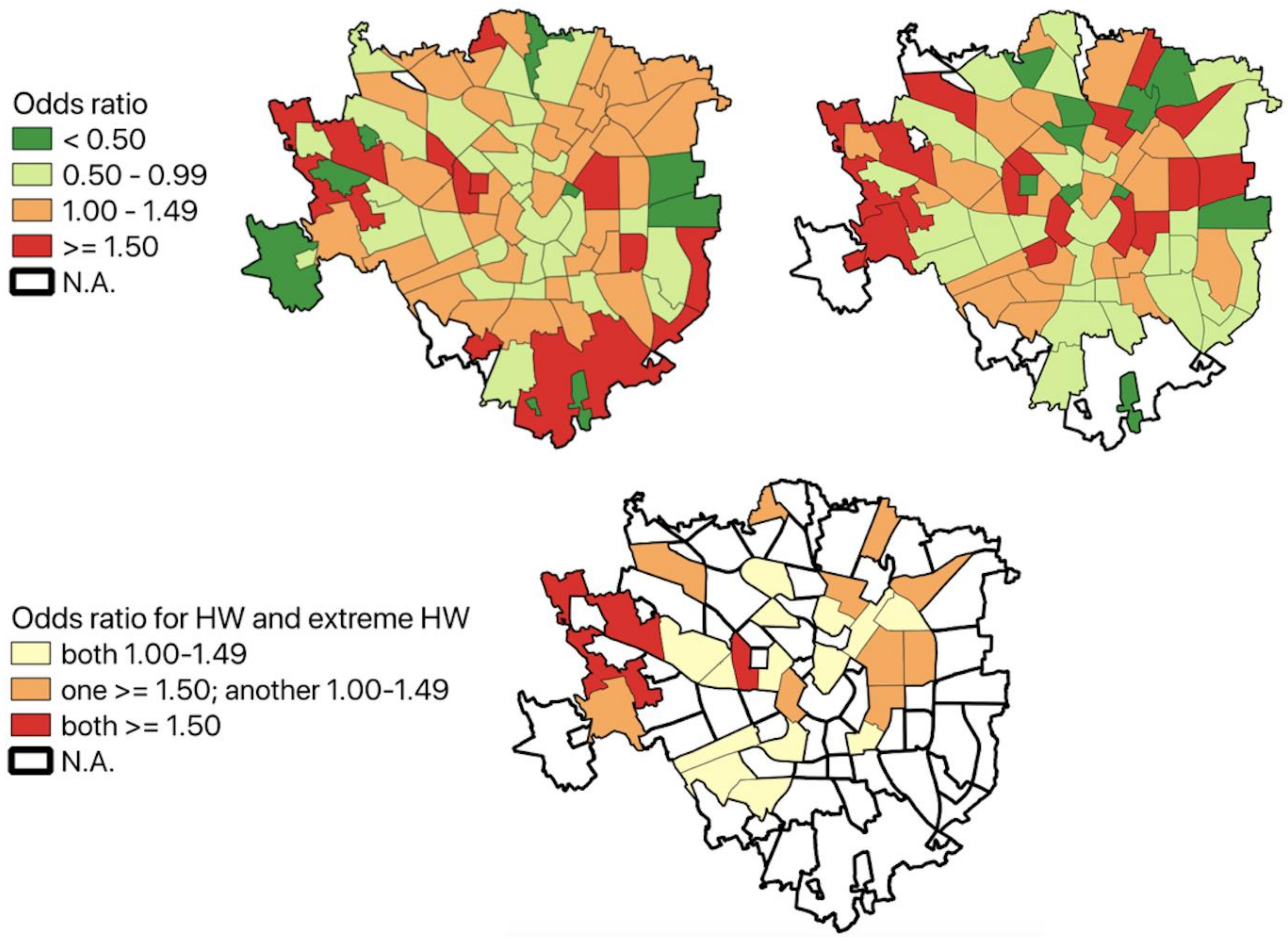
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Xing, Q.; Sun, Z.; Tao, Y.; Zhang, X.; Miao, S.; Zheng, C.; Tong, S. Impacts of urbanization on the temperature-cardiovascular mortality relationship in Beijing, China. Environ. Res. 2020, 191, 110234. [Google Scholar] [CrossRef] [PubMed]
- Peters, A.; Schneider, A. Cardiovascular risks of climate change. Nat. Rev. Cardiol. 2021, 18, 1–2. [Google Scholar] [CrossRef]
- Åström, D.O.; Forsberg, B.; Edvinsson, S.; Rocklöv, J. Acute fatal effects of short- lasting extreme temperatures in Stockholm, Sweden: Evidence across a century of change. Epidemiology 2013, 24, 820–829. [Google Scholar] [CrossRef] [PubMed]
- Cheng, X.; Su, H. Effects of climatic temperature stress on cardiovascular diseases. Eur. J. Intern. Med. 2010, 21, 164–167. [Google Scholar] [CrossRef]
- Nastos, P.T.; Matzarakis, A. The effect of air temperature and human thermal indices on mortality in Athens, Greece. Theor. Appl. Climatol. 2012, 108, 591–599. [Google Scholar] [CrossRef]
- Song, X.; Wang, S.; Hu, Y.; Yue, M.; Zhang, T.; Liu, Y.; Shang, K. Impact of ambient temperature on morbidity and mortality: An overview of reviews. Sci. Total Environ. 2017, 586, 241–254. [Google Scholar] [CrossRef]
- Lubczyńska, M.J.; Christophi, C.A.; Lelieveld, J. Heat-related cardiovascular mortality risk in Cyprus: A case-crossover study using a distributed lag non-linear model. Environ. Health 2015, 14, 1–11. [Google Scholar] [CrossRef]
- Ebi, K.L.; Capon, A.; Berry, P.; Broderick, C.; de Dear, R.; Havenith, G.; Jay, O. Hot weather and heat extremes: Health risks. Lancet 2021, 398, 698–708. [Google Scholar] [CrossRef]
- Kang, S.H.; Oh, I.Y.; Heo, J.; Lee, H.; Kim, J.; Lim, W.H.; Oh, S. Heat, heat waves, and out-of-hospital cardiac arrest. Int. J. Cardiol. 2016, 221, 232–237. [Google Scholar] [CrossRef]
- Schulte, F.; Roosli, M.; Ragettli, M.S. Heat-related cardiovascular morbidity and mortality in Switzerland: A clinical perspective. Swiss Med. Wkly. 2021, 151, w30013. [Google Scholar] [CrossRef]
- Murage, P.; Kovats, S.; Sarran, C.; Taylor, J.; McInnes, R.; Hajat, S. What individual and neighbourhood-level factors increase the risk of heat-related mortality? A case- crossover study of over 185,000 deaths in London using high-resolution climate datasets. Environ. Int. 2020, 134, 105292. [Google Scholar] [CrossRef]
- Comune di Milano. Available online: https://dati.comune.milano.it/dataset/ds205-sociale-caratteristiche-demografiche-territoriali-quartiere (accessed on 19 July 2022).
- Peel, M.C.; Finlayson, B.L.; McMahon, T.A. Updated world map of the Köppen-Geiger climate classification. Hydrol. Earth Syst. Sci. 2007, 11, 1633–1644. [Google Scholar] [CrossRef]
- Agenzia Regionale per la Protezione Dell’ambiente. Available online: https://www.arpalombardia.it/Pages/Meteorologia/Richiesta-dati-misurati.aspx (accessed on 19 July 2022).
- Boots, B.; Sugihara, K.; Chiu, S.N.; Okabe, A. Spatial Tessellations: Concepts and Applications of Voronoi Diagrams, 2nd ed.; Wiley: New York, NY, USA, 2009. [Google Scholar]
- World Health Organization: International Classification of Diseases: [9th] Ninth Revision, Basic Tabulation List with Alphabetic Index; World Health Organization: Geneva, Switzerland, 1978.
- Regione Lombardia. Available online: https://dati.lombardia.it/ (accessed on 19 July 2022).
- Pearce, N. What does the odds ratio estimate in a case-control study? Int. J. Epidemiol. 1993, 22, 1189–1192. [Google Scholar] [CrossRef]
- Maclure, M. The case-crossover design: A method for studying transient effects on the risk of acute events. Am. J. Epidemiol. 1991, 133, 144–153. [Google Scholar] [CrossRef]
- Breslow, N.E. Statistics in epidemiology: The case-control study. J. Am. Stat. Assoc. 1996, 91, 14–28. [Google Scholar] [CrossRef]
- Zhang, Z. Case-crossover design and its implementation in R. Ann. Transl. Med. 2016, 4, 341. [Google Scholar] [CrossRef]
- Kouis, P.; Kakkoura, M.; Ziogas, K.; Paschalidou, A.Κ.; Papatheodorou, S.I. The effect of ambient air temperature on cardiovascular and respiratory mortality in Thessaloniki, Greece. Sci. Total Environ. 2019, 647, 1351–1358. [Google Scholar] [CrossRef]
- Schechtman, E. Odds ratio, relative risk, absolute risk reduction, and the number needed to treat—Which of these should we use? Value Health 2002, 5, 431–436. [Google Scholar] [CrossRef]
- Aklilu, D.; Wang, T.; Amsalu, E.; Feng, W.; Li, Z.; Li, X.; Guo, X. Short-term effects of extreme temperatures on cause specific cardiovascular admissions in Beijing, China. Environ. Res. 2020, 186, 109455. [Google Scholar] [CrossRef]
- Lin, S.; Luo, M.; Walker, R.J.; Liu, X.; Hwang, S.A.; Chinery, R. Extreme high temperatures and hospital admissions for respiratory and cardiovascular diseases. Epidemiology 2009, 738–746. [Google Scholar] [CrossRef]
- Michelozzi, P.; Accetta, G.; De Sario, M.; D’Ippoliti, D.; Marino, C.; Baccini, M.; Perucci, C.A. High temperature and hospitalizations for cardiovascular and respiratory causes in 12 European cities. Am. J. Respir. Crit. Care Med. 2009, 179, 383–389. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, J.; Samet, J.M.; Patz, J.A. Hospital admissions for heart disease: The effects of temperature and humidity. Epidemiology 2004, 15, 755–761. [Google Scholar] [CrossRef] [PubMed]
- Bauer, F.; Lindtke, J.; Seibert, F.; Rohn, B.; Doevelaar, A.; Babel, N.; Westhoff, T.H. Impact of weather changes on hospital admissions for hypertension. Sci. Rep. 2022, 12, 5716. [Google Scholar] [CrossRef] [PubMed]
- Koken, P.J.; Piver, W.T.; Ye, F.; Elixhauser, A.; Olsen, L.M.; Portier, C.J. Temperature, air pollution, and hospitalization for cardiovascular diseases among elderly people in Denver. Environ. Health Perspect. 2003, 111, 1312–1317. [Google Scholar] [CrossRef]
- Qiu, H.; Tak-sun Yu, I.; Tse, L.A.; Tian, L.; Wang, X.; Wong, T.W. Is greater temperature change within a day associated with increased emergency hospital admissions for heart failure? Circ. Heart Fail. 2013, 6, 930–935. [Google Scholar] [CrossRef]
- Li, N.; Ma, J.; Liu, F.; Zhang, Y.; Ma, P.; Jin, Y.; Zheng, Z.J. Associations of apparent temperature with acute cardiac events and subtypes of acute coronary syndromes in Beijing, China. Sci. Rep. 2021, 11, 15229. [Google Scholar] [CrossRef]
- Guo, S.; Niu, Y.; Cheng, Y.; Chen, R.; Kan, J.; Kan, H.; Cao, J. Association between ambient temperature and daily emergency hospitalizations for acute coronary syndrome in Yancheng, China. Environ. Sci. Pollut. Res. 2020, 27, 3885–3891. [Google Scholar] [CrossRef]
- Panagiotakos, D.B.; Chrysohoou, C.; Pitsavos, C.; Nastos, P.; Anadiotis, A.; Tentolouris, C.; Paliatsos, A. Climatological variations in daily hospital admissions for acute coronary syndromes. Int. J. Cardiol. 2004, 94, 229–233. [Google Scholar] [CrossRef]
- Sohail, H.; Kollanus, V.; Tiittanen, P.; Schneider, A.; Lanki, T. Heat, heatwaves and cardiorespiratory hospital admissions in Helsinki, Finland. Int. J. Environ. Res. Public Health 2020, 17, 7892. [Google Scholar] [CrossRef]
- Mohammadi, R.; Soori, H.; Alipour, A.; Bitaraf, E.; Khodakarim, S. The impact of ambient temperature on acute myocardial infarction admissions in Tehran, Iran. J. Therm. Biol. 2018, 73, 24–31. [Google Scholar] [CrossRef]
- Fisher, J.A.; Jiang, C.; Soneja, S.I.; Mitchell, C.; Puett, R.C.; Sapkota, A. Summertime extreme heat events and increased risk of acute myocardial infarction hospitalizations. J. Expo. Sci. Environ. Epidemiol. 2017, 27, 276–280. [Google Scholar] [CrossRef]
- Kwon, B.Y.; Lee, E.; Lee, S.; Heo, S.; Jo, K.; Kim, J.; Park, M.S. Vulnerabilities to temperature effects on acute myocardial infarction hospital admissions in South Korea. Int. J. Environ. Res. Public Health 2015, 12, 14571–14588. [Google Scholar] [CrossRef]
- Loughnan, M.E.; Nicholls, N.; Tapper, N.J. The effects of summer temperature, age and socioeconomic circumstance on acute myocardial infarction admissions in Melbourne, Australia. Int. J. Health Geogr. 2010, 9, 41. [Google Scholar] [CrossRef]
- Liu, X.; Kong, D.; Fu, J.; Zhang, Y.; Liu, Y.; Zhao, Y.; Fan, Z. Association between extreme temperature and acute myocardial infarction hospital admissions in Beijing, China: 2013–2016. PLoS ONE 2018, 13, e0204706. [Google Scholar] [CrossRef]
- Wichmann, J.; Ketzel, M.; Ellermann, T.; Loft, S. Apparent temperature and acute myocardial infarction hospital admissions in Copenhagen, Denmark: A case-crossover study. Environ. Health 2012, 11, 19. [Google Scholar] [CrossRef]
- Empana, J.P.; Sauval, P.; Ducimetiere, P.; Tafflet, M.; Carli, P.; Jouven, X. Increase in out-of-hospital cardiac arrest attended by the medical mobile intensive care units, but not myocardial infarction, during the 2003 heat wave in Paris, France. Crit. Care Med. 2009, 37, 3079–3084. [Google Scholar] [CrossRef]
- García-Lledó, A.; Rodríguez-Martín, S.; Tobías, A.; Alonso-Martín, J.; Ansede-Cascudo, J.C.; de Abajo, F.J. Heat waves, ambient temperature, and risk of myocardial infarction: An ecological study in the Community of Madrid. Rev. Española De Cardiol. (Engl. Ed.) 2020, 73, 300–306. [Google Scholar]
- Dang, T.A.T.; Wraith, D.; Bambrick, H.; Dung, N.; Truc, T.T.; Tong, S.; Dunne, M.P. Short-term effects of temperature on hospital admissions for acute myocardial infarction: A comparison between two neighboring climate zones in Vietnam. Environ. Res. 2019, 175, 167–177. [Google Scholar] [CrossRef]
- Bai, L.; Li, Q.; Wang, J.; Lavigne, E.; Gasparrini, A.; Copes, R.; Chen, H. Hospitalizations from hypertensive diseases, diabetes, and arrhythmia in relation to low and high temperatures: Population-based study. Sci. Rep. 2016, 6, 30283. [Google Scholar] [CrossRef]
- Sheehy, S.; Fonarow, G.C.; Holmes, D.N.; Lewis, W.R.; Matsouaka, R.A.; Piccini, J.P.; Bhatt, D.L. Seasonal Variation of Atrial Fibrillation Admission and Quality of Care in the United States. J. Am. Heart Assoc. 2022, 11, e023110. [Google Scholar] [CrossRef]
- Comelli, I.; Ferro, J.; Lippi, G.; Comelli, D.; Sartori, E.; Cervellin, G. Incidence of acute-onset atrial fibrillation correlates with air temperature. Results of a nine-year survey. J. Epidemiol. Glob. Health 2014, 4, 151–157. [Google Scholar] [CrossRef] [PubMed]
- Lim, Y.H.; Hong, Y.C.; Kim, H. Effects of diurnal temperature range on cardiovascular and respiratory hospital admissions in Korea. Sci. Total Environ. 2012, 417, 55–60. [Google Scholar] [CrossRef] [PubMed]
- Onozuka, D.; Hagihara, A. Spatiotemporal variation in heat-related out-of-hospital cardiac arrest during the summer in Japan. Sci. Total Environ. 2017, 583, 401–407. [Google Scholar] [CrossRef] [PubMed]
- Borghei, Y.; Moghadamnia, M.T.; Sigaroudi, A.E.; Ghanbari, A. Association between climate variables (cold and hot weathers, humidity, atmospheric pressures) with out-of- hospital cardiac arrests in Rasht, Iran. J. Therm. Biol. 2020, 93, 102702. [Google Scholar] [CrossRef] [PubMed]
- Ferrini, F.; Fini, A.; Mori, J.; Gori, A. Role of vegetation as a mitigating factor in the urban context. Sustainability 2020, 12, 4247. [Google Scholar] [CrossRef]
- Mariani, L.; Parisi, S.G.; Cola, G.; Lafortezza, R.; Colangelo, G.; Sanesi, G. Climatological analysis of the mitigating effect of vegetation on the urban heat island of Milan, Italy. Sci. Total Environ. 2016, 569, 762–773. [Google Scholar] [CrossRef]
- Taleghani, M. Outdoor thermal comfort by different heat mitigation strategies—A review. Renew. Sustain. Energy Rev. 2018, 81, 2011–2018. [Google Scholar] [CrossRef]
- Arbuthnott, K.; Hajat, S.; Heaviside, C.; Vardoulakis, S. Changes in population susceptibility to heat and cold over time: Assessing adaptation to climate change. Environ. Health 2016, 15, 73–93. [Google Scholar] [CrossRef]
- Bobb, J.F.; Peng, R.D.; Bell, M.L.; Dominici, F. Heat-related mortality and adaptation to heat in the United States. Environ. Health Perspect. 2014, 122, 811–816. [Google Scholar] [CrossRef]
| Non-Heat Days | Heat Wave (Incl. Extreme Heat Wave) Days | Extreme Heat Wave Days | |
|---|---|---|---|
| Count | 21.3 °C | 27.1 °C | 28.9 °C |
| Mean | 3.06 °C | 1.15 °C | 0.84 °C |
| Standard deviation | 12.9 °C | 25.7 °C | 28.0 °C |
| Minimum | 19.2 °C | 26.3 °C | 28.3 °C |
| 25% | 21.8 °C | 26.8 °C | 28.4 °C |
| 50% | 23.7 °C | 27.9 °C | 29.7 °C |
| 75% | 25.8 °C | 30.5 °C | 30.5 °C |
| Maximum | 21.3 °C | 27.1 °C | 28.9 °C |
| Non-Heat Days | Heat Wave (Incl. Extreme Heat) Days | Extreme Heat Wave Days | Total | |
|---|---|---|---|---|
| Gender | ||||
| Female | 8305 (54%) | 2525 (53%) | 488 (53%) | 10,830 (53%) |
| Male | 7199 (46%) | 2237 (47%) | 436 (47%) | 9436 (47%) |
| Age | ||||
| <65 | 6997 (45%) | 2222 (47%) * | 438 (47%) | 9219 (45%) |
| >=65 | 8507 (55%) | 2540 (53%) * | 486 (53%) | 11,047 (55%) |
| Place | ||||
| Home | 11,583 (75%) | 3353 (70%) * | 639 (69%) * | 14,936 (74%) |
| Street | 1286 (8%) | 479 (10%) * | 102 (11%) * | 1765 (9%) |
| Other | 2635 (17%) | 930 (20%) * | 183 (20%) * | 3565 (18%) |
| Hour | ||||
| Night (00-08) | 3385 (22%) | 1051 (22%) | 192 (21%) | 4436 (22%) |
| Day (09-23) | 12,119 (78%) | 3711 (78%) | 732 (79%) | 15,830 (78%) |
| Total | 15,504 | 4762 | 924 | 20,266 |
| Non-Heat Days | Heat Wave (Incl. Extreme Heat) Days | Extreme Heat Wave Days | Total | |
|---|---|---|---|---|
| Acute myocardial infarction | ||||
| Events | 55 | 21 | 5 | 76 |
| In which fatal events | 0 (0.0%) | 2 (9.5%) | 2 (40.0%) | 2 (2.6%) |
| Atrial fibrillation | ||||
| Events | 251 | 66 | 17 | 317 |
| In which fatal events | 1 (0.4%) | 0 (0.0%) | 0 (0.0%) | 1 (0.3%) |
| Cardiac arrest | ||||
| Events | 118 | 36 | 4 | 154 |
| In which fatal events | 79 (66.9%) | 26 (72.2%) | 3 (75%) | 105 (68.2%) |
| Other | 2635 (17%) | 930 (20%) * | 183 (20%) * | 3565 (18%) |
| Congestive heart failure | ||||
| Night (00-08) | 3385 (22%) | 1051 (22%) | 192 (21%) | 4436 (22%) |
| Day (09-23) | 12,119 (78%) | 3711 (78%) | 732 (79%) | 15,830 (78%) |
| Total | 15,504 | 4762 | 924 | 20,266 |
| Hypertension | ||||
| Events | 456 | 78 | 13 | 534 |
| In which fatal events | 0 (0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Intermediate coronary syndrome | ||||
| Events | 71 | 16 | 5 | 87 |
| In which fatal events | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Palpitations | ||||
| Events | 172 | 39 | 6 | 211 |
| In which fatal events | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Tachycardia | ||||
| Events | 156 | 40 | 5 | 196 |
| In which fatal events | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Total | ||||
| Events | 1416 | 335 | 63 | 1751 |
| In which fatal events | 81 (5.7%) | 30 (9.0%) | 5 (7.9%) | 111 (6.3) |
| Non-Heat Days | Heat Wave (Incl. Extreme Heat) Days | Extreme Heat Wave Days | Total | |
|---|---|---|---|---|
| All patients | 1.07 * | [1.00; 1.14] | 1.05 | [0.90; 1.23] |
| ≥65 years old | 1.06 | [0.97; 1.16] | 0.95 | [0.77; 1.18] |
| Female | 1.06 | [0.97; 1.16] | 0.99 | [0.80; 1.22] |
| Male | 1.08 | [0.98; 1.189] | 1.12 | [0.87; 1.43] |
| Acute myocardial infarction | 1.53 | [0.52; 4.5] | 1.56 | [0.24; 10.04] |
| Atrial fibrillation | 0.98 | [0.57; 1.69] | 1.42 | [0.4; 5.07] |
| Cardiac arrest | 0.99 | [0.49; 2.01] | 0.47 | [0.09; 2.57] |
| Congestive heart failure | 2.47 * | [1.09; 5.62] | 2.81 | N.A. |
| Hypertension | 0.74 | [0.46; 1.19] | 0.70 | [0.23; 2.14] |
| Intermediate coronary syndrome | 2.08 | [0.59; 7.34] | 6.11 | [0.51; 72.66] |
| Palpitations | 0.73 | [0.37; 1.45] | 1.88 | [0.16; 21.5] |
| Tachycardia | 0.87 | [0.43; 1.74] | 0.29 | [0.03; 2.49] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nawaro, J.; Gianquintieri, L.; Pagliosa, A.; Silvaroli, A.; Sechi, G.M.; Caiani, E.G. Heat Waves and Cardiovascular Events in Milan, Italy: A Geospatial Case-Crossover Approach Using Data from Emergency Medical Services. Med. Sci. Forum 2023, 19, 5. https://doi.org/10.3390/msf2023019005
Nawaro J, Gianquintieri L, Pagliosa A, Silvaroli A, Sechi GM, Caiani EG. Heat Waves and Cardiovascular Events in Milan, Italy: A Geospatial Case-Crossover Approach Using Data from Emergency Medical Services. Medical Sciences Forum. 2023; 19(1):5. https://doi.org/10.3390/msf2023019005
Chicago/Turabian StyleNawaro, Julia, Lorenzo Gianquintieri, Andrea Pagliosa, Alessandra Silvaroli, Giuseppe Maria Sechi, and Enrico G. Caiani. 2023. "Heat Waves and Cardiovascular Events in Milan, Italy: A Geospatial Case-Crossover Approach Using Data from Emergency Medical Services" Medical Sciences Forum 19, no. 1: 5. https://doi.org/10.3390/msf2023019005
APA StyleNawaro, J., Gianquintieri, L., Pagliosa, A., Silvaroli, A., Sechi, G. M., & Caiani, E. G. (2023). Heat Waves and Cardiovascular Events in Milan, Italy: A Geospatial Case-Crossover Approach Using Data from Emergency Medical Services. Medical Sciences Forum, 19(1), 5. https://doi.org/10.3390/msf2023019005







