Abstract
During the coronavirus (COVID-19) pandemic, we saw significant decreases in the incidence of bloodstream infections (BSIs), antibiotic-resistant infections, and the burden of resistant infections. The reasons for this are complex and multifactorial, but likely, at least in part, due to changes in healthcare delivery and healthcare seeking behavior. As healthcare systems return to pre-pandemic ways of working, now is a pivotal moment to ensure focus remains on what is often referred to as the ‘silent pandemic’: antimicrobial resistance (AMR). The ninth English Surveillance Programme for Antimicrobial Utilization and Resistance (ESPAUR) report provides an overview of the national data on antibiotic prescribing and resistance, antimicrobial stewardship implementation, and awareness activities. The active contribution from and collaboration with the ESPAUR oversight group and the engagement of stakeholder organizations, including the devolved administrations, are also reported. Findings from the ESPAUR report were presented at a webinar on 23 November 2022.
1. Introduction
Findings from the English Surveillance Programme for Antimicrobial Utilization and Resistance (ESPAUR) report were presented at the ESPAUR 2021/22 webinar. UKHSA hosted the ESPAUR 2021–22 report interactive webinar on Wednesday 23 November 2022. The recording is available.
ESPAUR was established by the UK Health Security Agency (UKHSA) in 2013 to support the delivery of the UK National Action Plan (NAP) for antimicrobial resistance (AMR) [1]. The ESPAUR programme and oversight group works across the healthcare system, and with external stakeholders to bring together the elements of antimicrobial utilization and resistance surveillance to inform on trends and the impact of external forces on antimicrobial prescribing, and progress towards the 5-year NAP.
The aims of ESPAUR are to (1) develop and maintain robust surveillance systems for monitoring and reporting trends in antimicrobial use and resistance, in order to measure the impact of surveillance, antimicrobial stewardship, and other interventions on antimicrobial resistance that affect human health, and (2) develop systems and processes to optimize antimicrobial prescribing across healthcare settings [2].
Chapter 1 of the ESPAUR report provides an overview of the key messages from each chapter [3] (Figure 1). Data and data sources, data processing and statistical analyses are detailed in the ESPAUR Report Annexe [4].
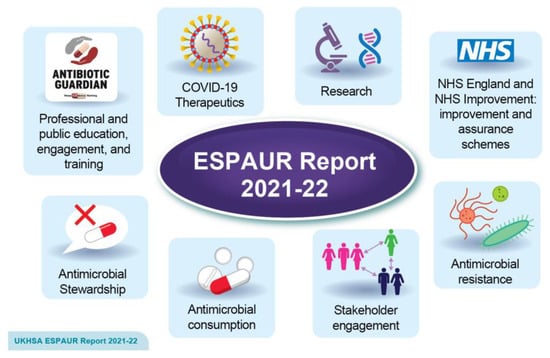
Figure 1.
Chapters in the ESPAUR report 2021–2022. Reprinted with permission from Ref. [4]. Copyright 2022 UK Health Security Agency.
2. Highlights from the Chapters
2.1. Chapter 2—Antimicrobial Resistance (AMR)
The UK NAP ambition for AMR is to reduce the (estimated) total number of antibiotic-resistant infections in the UK by 10% from the 2018 baseline by 2025 [5]. Progress has been made towards this target, with a 9.1% reduction being achieved between 2018 and 2021 in England, although much of this reduction occurred during the pandemic and is likely to be in part due to the interventions in place at that time [6]. After an initial increase seen between 2018 and 2019, there was a 15.7% decline in the estimated number of severe antibiotic-resistant infections between 2019 and 2020, followed by a slight increase in 2021 (2.2%) [6].
For the first time in the ESPAUR report, data have been disaggregated to describe varying rates of AMR burden related to ethnicity and deprivation. The rate of carbapenems-producing Gram-negative bacteria notifications varied by indices of multiple deprivation (IMD), with a higher rate of notifications seen in the more deprived deciles (2021: 6.8 per 100,000 population in the most deprived decile compared with 2.8 per 100,000 population in the least deprived) [6]. In 2021, 81% (50,329) of BSI episodes (as per AMR burden combinations) were recorded in persons within a white ethnic group, of which 20.9% were resistant to at least one key antimicrobial [6]. The highest percentage resistance was noted in the Asian or Asian British ethnic group, with 32.8% of key organisms BSI-resistant to at least one key antimicrobial [6]. Further work to develop a deeper understanding of the impact of ethnicity, deprivation, regional divergence, along with potential confounders, remains a crucial avenue of enquiry and essential to the identification of appropriate target interventions. UKHSA has developed an AMR health inequalities workstream to better understand how the burden of AMR differentially impacts certain groups, and to embed a systematic approach to reducing health inequalities in AMR.
2.2. Chapter 3—Antimicrobial Consumption
Total antibiotic consumption has been decreasing with a sharp decline seen coinciding with the COVID-19 pandemic. There was an overall 10.9% decrease in antibiotic consumption between 2019 and 2020 alone, followed by a further decline of 0.5% from 2020 to 2021 [7]. Antibiotic prescribing continued to be the highest in the general practice setting in 2021 (72.1%) and it is also here that the largest reductions in antibiotic prescribing have consistently occurred [7]. In 2021, antibiotic prescribing has also decreased in dental practices, following a spike between 2019 and 2020, but has increased in hospital inpatient, outpatient, and other community settings between 2020 and 2021 [7].
Total consumption of systemic antifungals prescribed in the community and NHS hospitals in England decreased by 22.9% between 2017 and 2021. However, between 2020 and 2021, antifungal consumption has increased by 7.1% [7].
The reasons for the fall in antimicrobial consumption are likely multifactorial, but driven by a reduction in respiratory infections, supported by reports of reduced respiratory antibiotic prescribing in the young [8], and reduced general practice consultations [9]. Other factors likely include improved infection prevention and control measures, social restrictions, the use of facemasks, and changes in-service delivery, such as less face-to-face consultations in primary care.
2.3. Chapter 4—Antimicrobial Stewardship
Whilst improvements and reductions in antibiotic prescribing have been made, continued stewardship and surveillance are needed to sustain progress towards the NAP. The factors contributing to improvements in antimicrobial stewardship are likely multifactorial, but UKHSA continues to lead some of the key national primary and secondary care antimicrobial stewardship (AMS) interventions, including the TARGET (Treat Antibiotics Responsibly, Guidance, Education and Tools) toolkit hosted on the Royal College of General Practitioners (RCGP) website [10], and Start Smart then Focus (AMS toolkit for secondary care).
The TARGET Antibiotic Checklist [11], an antimicrobial stewardship tool, was included as a component of the 2021 to 2022 Pharmacy Quality Scheme (PQS), and 74% of pharmacies in England submitted data from over 200,000 individuals collecting an antibiotic prescription. High engagement from pharmacy staff suggests that the AMS principles introduced with the TARGET Antibiotic Checklist may be embedded [12].
In line with the NAP ambition to “enhance the role of pharmacists in primary care”, UKHSA, in collaboration with partners, has developed evidence-based, system-wide intervention (‘How to...’ guides) to support primary care teams to review the dose and duration of long-term and repeat antimicrobial prescriptions. The intervention focuses on toolkits and resource guides, specifically for acne and chronic obstructive pulmonary disease exacerbations (COPD). Acne and COPD were prioritized as Primary Care Network (PCN) data, revealing that these are the most common clinical conditions associated with the highest use of long-term or repeat antibiotics [12].
Within secondary care, AMS interventions included the development of a UK-wide antimicrobial intravenous-to-oral switch (IVOS) criteria and sample tools for hospitalised adult patients. This was developed from local policies, literature, and expert opinion with consensus for switch criteria obtained via a 4-stage Delphi process involving 279 multidisciplinary colleagues from all four UK nations [12].
2.4. Chapter 5—NHS England: Improvement and Assurance Schemes
Within primary care, the NHS System Oversight Framework 2021/22, which aims to ensure alignment of priorities across the NHS, retained two primary care antibiotic prescribing metrics: total items prescribed and broad-spectrum proportion [13]. By the end of 2021 to 2022, 50% of 42 Integrated Care Systems (ICSs: local partnerships of NHS providers, local authorities, and others who have collective responsibility for planning services, improving health and reducing inequalities for their population of 500,000 to 3 million) met the NAP reduction target for total antibiotic prescribing and 83% met the reduction target for the proportion of broad-spectrum antibiotics [9].
For NHS trusts providing acute care, a requirement to reduce antibiotic consumption by 2% from each trust’s 2018 calendar year baseline was reinstated in the NHS Standard Contract for 2021 to 2022, following suspension during the COVID-19 pandemic [14]. By the end of 2021 to 2022, 50% of acute trusts met this ambition to reduce a total consumption of antimicrobials by 2% [9].
2.5. Chapter 6—Professional and Public Education, Engagement and Training
UKHSA continues to lead the education and engagement of healthcare professionals and the public through World Antimicrobial Awareness Week (WAAW), European Antibiotic Awareness Day (EAAD), and the National Healthcare Students’ AMR Conference for medical and pharmacy students.
WAAW 2021 offered an opportunity to engage professionals and the public in AMR by consolidating digital campaigning introduced in 2020. A new WAAW and EAAD toolkit for healthcare professionals in England was developed to provide guidance to support the NHS, local authorities and others to lead activities and encourage the responsible use of antibiotics. There was also continued engagement with Antibiotic Guardian Schools Ambassadors providing antibiotic use, and infection prevention and control education to children and young people through schools and community groups [15].
A redesign and national rollout of the e-Bug resources is helping meet objectives to support schools and communities to reinvigorate key infection prevention and control (IPC), and AMR messages [16]. Groundwork for the national implementation of TARGET and e-Bug professional training and resources has commenced, aiming for consistent education of healthcare professionals (HCP) and the public in the future [15].
2.6. Chapter 7—COVID-19 Therapeutics
UKHSA’s COVID-19 therapeutics programme has supported the deployment of COVID-19 therapies by undertaking genomic, virological, and epidemiological surveillance of COVID-19 therapeutics. Between 1 October 2021 and 31 March 2022, there were over 51,000 treatment requests for neutralizing monoclonal antibodies and antivirals against COVID-19 for patients in England [17]. This programme identified eleven mutations which exhibited a significant change between samples obtained from patients before and after treatment, and which may help the virus evade antimicrobials. This has been an important evidence base for changes to clinical commissioning policies for COVID-19 therapeutics [18].
2.7. Chapter 8—Research
The UKHSA continues to undertake a wide range of new and ongoing research projects in the field of healthcare-associated infections (HCAIs) and AMR, which cover many of the major themes of the NAP for AMR. Key research is presented from the two National Institute for Health Research (NIHR) Health Protection Research Units (HPRUs), led by the Imperial College London and Oxford University in partnership with UKHSA. The research outputs are described in further detail in Chapter 8 of the ESPAUR Report [19].
3. Stakeholder Engagement
UKHSA could not deliver its range of activities, progress towards its objectives or produce the ESPAUR report without active contribution from and collaboration with the ESPAUR oversight group and the engagement of stakeholder organizations (Figure 2). More than 20 national stakeholders, ranging from government organizations to independent healthcare providers to patient representatives, are current and active members of the ESPAUR Oversight Group and contribute to reducing AMR in the United Kingdom:
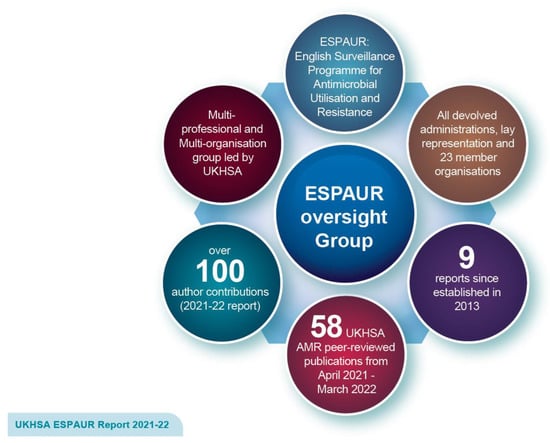
Figure 2.
Key outputs of the ESPAUR oversight group. Reprinted with permission from Ref. [4]. Copyright 2022 UK Health Security Agency.
- Department of Health and Social Care (DHSC), including Dental Public Health, Office for Health Improvement and Disparities (OHID)
- DHSC Expert Advisory Committee on Antimicrobial Prescribing, Resistance and Healthcare-Associated Infection (APRHAI)
- British National Formulary (BNF)
- British Society for Antimicrobial Chemotherapy (BSAC)
- Care Quality Commission (CQC)
- College of General Dentistry
- IQVIA
- National Institute of Health and Care Excellence (NICE)
- NHS England (NHSE)
- Patient representation
- Primary Care Pharmacy Association (PCPA)
- Royal College of Nursing (RCN)
- Royal College of Physicians (RCP)
- Royal College of General Practitioners (RCGP)
- Royal Pharmaceutical Society (RPS)
- Rx-Info Ltd.
- UK Clinical Pharmacy Association: Pharmacy Infection Network (UKCPA PIN)
- Veterinary Medicines Directorate (DEFRA)
- Antimicrobial Resistance and Healthcare-Associated Infection (ARHAI) Scotland, NHS National Services Scotland
- Public Health Scotland
- Public Health Wales
- Public Health Agency Northern Ireland (Health and Social Care Northern Ireland-HSCNI)
- UKHSA (represented by individuals with appropriate expertise from the HCAI, antimicrobial utilization (AMU), AMR, Fungal and Sepsis Division, Behavioral Insights, Regions, Field Service, Microbiology services, and Communications teams)
Stakeholder Activities
A wide range of stakeholder activities have been undertaken over the previous year. The following activity is an example of the range of stakeholder undertakings with the aim of reducing AMR: resources, such as the TARGET Antibiotics toolkit [3], have been promoted across the UK via the use of campaigns and other methods. One such campaign, run in 2021, aimed to introduce the ‘Antibiotic Checklist’, including a resource pack with self-care leaflets and posters, to all community pharmacies in Wales.
Furthermore, there has been significant commitment over the previous year to develop educational resources, publish evidence-based resources, and promote AMS programmes. For example, to facilitate the use of the Antibiotic Checklist, an E-Learning module was developed in collaboration with stakeholders involved in health education and improvement. This module was based on the E-Learning module previously developed by PHE (now UKHSA) and Health Education England. Pharmacy stakeholders have also developed a range of pharmacy resources, including podcasts, blogs, and webinars, and an education programme on infection prevention and control and antimicrobial stewardship, using competencies developed with the University of Cardiff, has continued to be delivered.
In addition to these activities, the ESPAUR Oversight Group has provided support to national and international networks by contributing to the European Antibiotic Awareness Day and World Health Organization’s Antimicrobial Awareness Week. For example, public health colleagues ran a campaign during WAAW 2021 to highlight the importance of AMR to both professionals and the public. Finally, the surveillance of AMR infections has been improved following the launch of the NHS AMR dashboard. This allows key data on emergency admissions due to bacterial infection and/or sepsis to be viewed at the Integrated Care System, Clinical Commissioning Group, NHS Trust, and regional and national levels, broken down by individual criteria.
Author Contributions
Conceptualization, D.A.-O. and S.H.; methodology, N.C., E.C. and C.T.-H.; validation, C.S.B. and R.H.; resources, D.A.-O., C.S.B., R.H. and S.H.; writing—original draft preparation, N.C., E.C. and C.T.-H.; visualization, E.C. and C.T.-H.; project administration, E.C. and C.T.-H. All authors have read and agreed to the published version of the manuscript.
Funding
This editorial received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Publicly available datasets were analyzed in this study. This data can be found here: English surveillance programme for antimicrobial utilization and resistance (ESPAUR) report—GOV.UK (www.gov.uk, accessed on 25 November 2022).
Acknowledgments
The authors would like to acknowledge the ESPAUR Oversight Group members and individual chapter authors for their dedication and contribution. Contributors to the stakeholder chapter are also acknowledged: Gil Damant, Tamsin Dewe, Jeff Featherstone, Kitty Healey, Martin Astbury, Natasha Bell-Asher, Nicholas Brown, Mary Collier, Judith Ewing, Naomi Fleming, Rose Gallagher, Ellie Gillham, Kieran Hand, Martin Llewelyn, William Malcolm, Sannah Malik, Arianne Matlin, Nicholas Reid, Tracy Rogers, Wendy Thompson, Jonathan Underhill, Fiona Watson, Lydia Harman, and Simon Hartnett-Welch.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Tackling Antimicrobial Resistance 2019 to 2024: The UK’s 5-Year National Action Plan; Department of Health and Social Care: London, UK, 2019.
- Hopkins, S.; Johnson, A. Chapter 1 Introduction. In The English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR) Report 2018; Public Health England: London, UK, 2018. [Google Scholar]
- Cunningham, N.; Hopkins, S. Chapter 1 Introduction. In The English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR) Report 2021 to 2022; UK Health Security Agency: London, UK, 2022. [Google Scholar]
- UK Health Security Agency. English surveillance programme for antimicrobial utilisation and resistance (ESPAUR) Report 2021 to 2022. Available online: https://www.gov.uk/government/publications/english-surveillance-programme-antimicrobial-utilisation-and-resistance-espaur-report (accessed on 25 November 2022).
- Tackling Antimicrobial Resistance 2019 to 2024: Addendum to the UK’s 5-Year National Action Plan; Department of Health and Social Care: London, UK, 2022.
- Guy, R.; Higgins, H.; Rudman, J.; Fountain, H.; Henderson, K.; Bennet, K.; Hopkins, K.; Demirjian, A.; Gerver, S.; Mirfenderesky, M. Chapter 2 Antimicrobial Resistance. In The English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR) Report 2021-22; UK Health Security Agency: London, UK, 2022. [Google Scholar]
- Bou-Antoun, S.; Falola, A.; Fountain, H.; Squire, H.; Brown, C.; Hopkins, S.; Gerver, S.; Demirjian, A. Chapter 3 Antimicrobial consumption. In The English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR) Report 2021 to 2022; UK Health Security Agency: London, UK, 2022. [Google Scholar]
- Andrews, A.; Bou-Antoun, S.; Guy, R.; Brown, C.S.; Hopkins, S.; Gerver, S. Respiratory antibacterial prescribing in primary care and the COVID-19 pandemic in England, winter season 2020–21. J. Antimicrob. Chemother. 2022, 77, 799–802. [Google Scholar] [CrossRef] [PubMed]
- Hand, K.; Beech, E.; McLeod, M.; Bou-Antoun, S.; Squire, H.; Budd, E.; Featherstone, J.; Parekh, S.; Lecky, D.; Hayes, C.; et al. Chapter 5 NHS England: Improvement and assurance schemes. In The English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR) Report 2021 to 2022; UK Health Security Agency: London, UK, 2022. [Google Scholar]
- Royal College of General Practitioners. TARGET Antibiotics Toolkit Hub. 2022. Available online: https://elearning.rcgp.org.uk/course/view.php?id=553 (accessed on 25 November 2022).
- Royal College of General Practitioners. TARGET Antibiotics Toolkit Hub—TARGET Antibiotic Checklist. 2022. Available online: https://elearning.rcgp.org.uk/mod/book/view.php?id=13511&chapterid=784 (accessed on 25 November 2022).
- Casale, E.; Hayes, C.; Lecky, D.; O’Neil, L.; Sides, E.; Cooper, E.; Pursey, F.; Parekh, S.; Fisher, L.; MacKenna, B.; et al. Chapter 4 Antimicrobial stewardship. In The English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR) Report 2021 to 2022; UK Health Security Agency: London, UK, 2022. [Google Scholar]
- NHS England. NHS System Oversight Framework 2021/22. 2021. Available online: https://www.england.nhs.uk/publication/system-oversight-framework-2021-22/ (accessed on 25 November 2022).
- NHS England. 2021/22 NHS Standard Contract. 2021. Available online: https://www.england.nhs.uk/nhs-standard-contract/previous-nhs-standard-contracts/21-22/ (accessed on 25 November 2022).
- Hayes, C.; Charlesworth, J.; Ashiru-Oredope, D.; Sides, E.; Jackson, A.; Cooper, E.; Read, B.; Seaton, D.; Flintham, L.; Sidhu, H.; et al. Chapter 6 Professional education and training and public engagement. In The English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR) Report 2021 to 2022; UK Health Security Agency: London, UK, 2022. [Google Scholar]
- e-Bug. 2022. Available online: https://e-Bug.eu (accessed on 25 November 2022).
- Squire, H.; Lochen, A.; Ashiru-Oredope, D.; Hand, K.; Hartman, H.; Triggs-Hodge, C.; Fountain, H.; Bou-Antoun, S.; Gerver, S.; Demirjian, A. Chapter 7. COVID-19 therapeutics. In The English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR) Report 2021 to 2022; UK Health Security Agency: London, UK, 2022. [Google Scholar]
- UK Health Security Agency. COVID-19 Therapeutic Agents: Technical Briefings. 2022. Available online: https://www.gov.uk/government/publications/covid-19-therapeutic-agents-technical-briefings (accessed on 25 November 2022).
- Agnew, E.; Charlesworth, J.; Bacon, J.; Charani, E.; Turton, J.; Guy, R.; Lipworth, S.; Borek, A.; Collin, S.; Ashiru-Oredope, D.; et al. Chapter 8 Research. In The English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR) Report 2021 to 2022; UK Health Security Agency: London, UK, 2022. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).