The Effectiveness and Cost-Effectiveness of the ‘Walk with Me’ Peer-Led Walking Intervention to Increase Physical Activity in Inactive Older Adults: Study Protocol for a Randomised Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
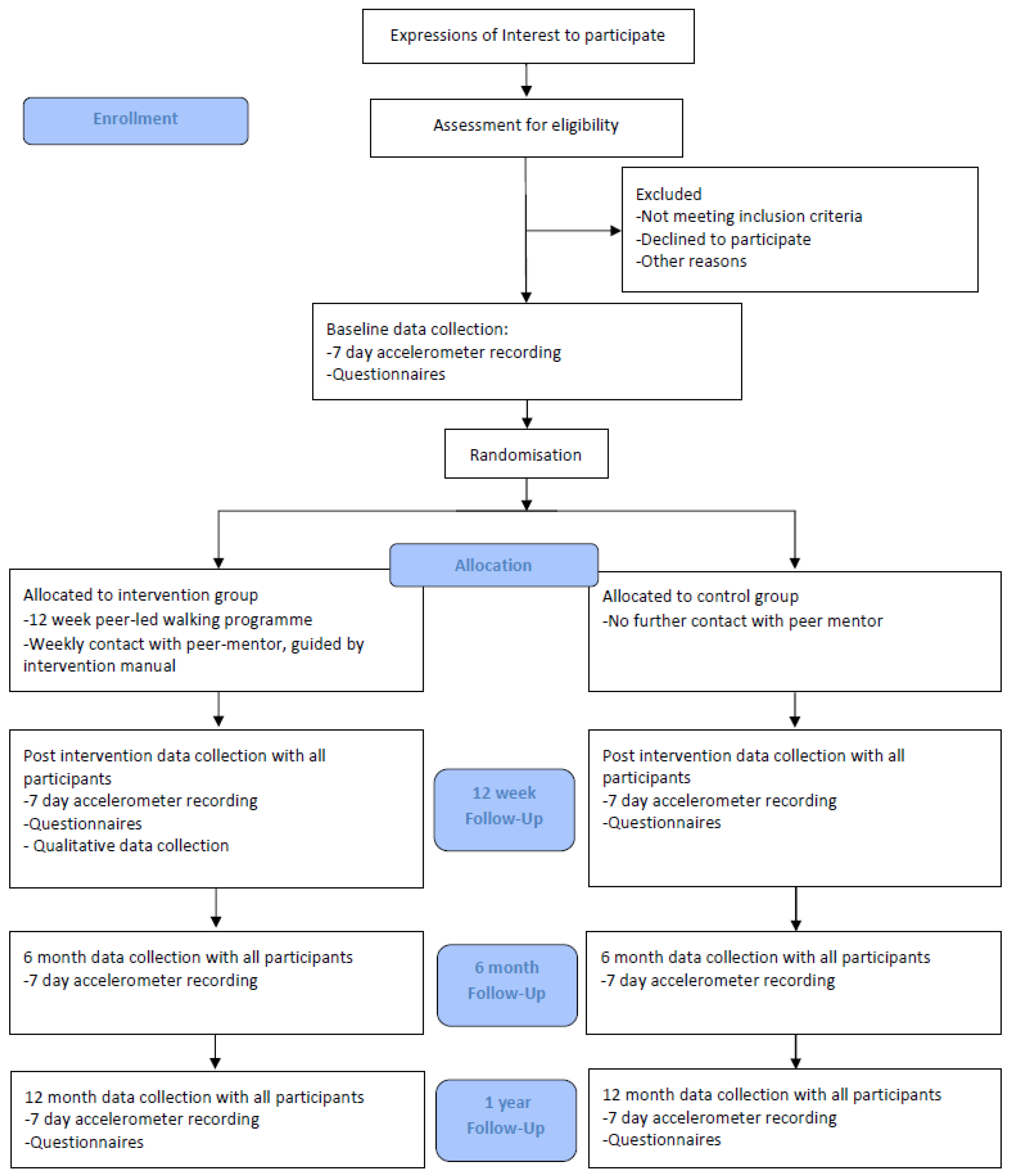
2.1. Study Design
2.2. Study Setting and Recruitment
2.3. Eligibility Criteria
- Males or females aged 60 years or over.
- Living in a socio-economically disadvantaged community, defined as the most disadvantaged quartile of electoral wards in Northern Ireland according to the NIMDM.
- Able to communicate in English and live independently in the community (i.e., at home), including those residing in independent living facilities. We will also only include individuals planning to stay in their current accommodation during the next year, to try and ensure they will be available for follow-up assessment.
- Individuals not in employment at the outset will be included provided they are not planning on returning to work over the following 12 months. This is to mitigate against the potential interaction between returning to work and changes in physical activity.
- Competent to give informed consent, assessed as a score of 24 and higher on the Mini-Mental State Exam [19]
- Non-frail, assessed as a score of <3 using the PRISMA-7 questionnaire [20]
- Individuals who report no recent medical history in the last six months that would limit the ability to participate in a walking programme are assessed using the Physical Activity Readiness Questionnaire [21]
2.4. Allocation and Randomisation
2.5. Walk with Me Intervention
2.6. Peer Mentors
2.7. Control Group
2.8. Outcome Measures
2.9. Health Economic Evaluation
2.10. Statistical Analysis
2.11. Sample Size
2.12. Process Evaluation
2.13. Implementation
2.14. Mechanisms of Impact
2.15. Contextual Factors
2.16. Assessment of Harms
3. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- United Nations. World Population Ageing 2017 Highlights; United Nations: New York, NY, USA, 2019. [Google Scholar]
- Chief Medical Officer’s Annual Report 2023: Health in an Ageing Society. Available online: https://www.gov.uk/government/publications/chief-medical-officers-annual-report-2023-health-in-an-ageing-society (accessed on 10 December 2023).
- Cunningham, C.; O’ Sullivan, R.; Caserotti, P.; Tully, M.A. Consequences of physical inactivity in older adults: A systematic review of reviews and meta-analyses. Scand. J. Med. Sci. Sports 2020, 30, 816–827. [Google Scholar] [CrossRef]
- Sari, N. Exercise, physical activity and healthcare utilization: A review of literature for older adults. Maturitas 2011, 70, 285–289. [Google Scholar] [CrossRef] [PubMed]
- Gomes, M.; Figueiredo, D.; Teixeira, L.; Poveda, V.; Paúl, C.; Santos-Silva, A.; Costa, E. Physical inactivity among older adults across Europe based on the SHARE database. Age Ageing 2017, 46, 71–77. [Google Scholar] [CrossRef]
- Shankar, A.; McMunn, A.; Banks, J.; Steptoe, A. Loneliness, social isolation, and behavioral and biological health indicators in older adults. Health Psychol. 2011, 30, 377–385. [Google Scholar] [CrossRef] [PubMed]
- McPhee, J.S.; French, D.P.; Jackson, D.; Nazroo, J.; Pendleton, N.; Degens, H. Physical activity in older age: Perspectives for healthy ageing and frailty. Biogerontology 2016, 17, 567–580. [Google Scholar] [CrossRef] [PubMed]
- Craike, M.; Wiesner, G.; Hilland, T.A.; Bengoechea, E.G. Interventions to improve physical activity among socioeconomically disadvantaged groups: An umbrella review. Int. J. Behav. Nutr. Phys. Act 2018, 15, 43. [Google Scholar] [CrossRef] [PubMed]
- Harris, T.; Kerry, S.M.; Limb, E.S.; Furness, C.; Wahlich, C.; Victor, C.R.; Iliffe, S.; Whincup, P.H.; Ussher, M.; Ekelund, U.; et al. Physical activity levels in adults and older adults 3-4 years after pedometer-based walking interventions: Long-term follow-up of participants from two randomised controlled trials in UK primary care. PLoS Med. 2018, 15, e1002526. [Google Scholar] [CrossRef] [PubMed]
- Ekkekakis, P.; Zenko, Z.; Ladwig, M.A.; Hartman, M.E. Affect as a potential determinant of physical activity and exercise: Critical appraisal of an emerging research field. In Affective Determinants of Health Behaviour; Williams, D.M., Rhodes, R.E., Conner, M.T., Eds.; Oxford University Press: New York, NY, USA, 2018. [Google Scholar]
- Lindsay Smith, G.; Banting, L.; Eime, R.; O’Sullivan, G.; van Uffelen, J.G.Z. The association between social support and physical activity in older adults: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 56. [Google Scholar] [CrossRef]
- Kwasnicka, D.; Dombrowski, S.U.; White, M.; Sniehotta, F. Theoretical explanations for maintenance of behaviour change: A systematic review of behaviour theories. Health Psychol. Rev. 2016, 10, 277–296. [Google Scholar] [CrossRef]
- Burton, E.; Farrier, K.; Hill, K.D.; Codde, J.; Airey, P.; Hill, A.M. Effectiveness of peers in delivering programs or motivating older people to increase their participation in physical activity: Systematic review and meta-analysis. J. Sports Sci. 2018, 36, 666–678. [Google Scholar] [CrossRef]
- Tully, M.A.; Cunningham, C.; Wright, A.; McMullan, I.; Doherty, J.; Collins, D.; Tudor-Locke, C.; Morgan, J.; Phair, G.; Laventure, B.; et al. Peer-Led Walking Programme to Increase Physical Activity in Inactive 60- to 70-Year-Olds: Walk with Me Pilot RCT; NIHR Journals Library: Southampton, UK, 2019. [Google Scholar]
- Avery, K.N.; Williamson, P.R.; Gamble, C.; O’Connell Francischetto, E.; Metcalfe, C.; Davidson, P.; Williams, H.; Blazeby, J.M.; Members of the Internal Pilot Trials Workshop supported by the Hubs for Trials Methodology Research. Informing efficient randomised controlled trials: Exploration of challenges in developing progression criteria for internal pilot studies. BMJ Open 2017, 7, e013537. [Google Scholar] [CrossRef] [PubMed]
- Northern Ireland Multiple Deprivation Measure 2017 (NIMDM2017). Available online: https://www.nisra.gov.uk/statistics/deprivation/northern-ireland-multiple-deprivation-measure-2017-nimdm2017 (accessed on 10 December 2023).
- Department of Health and Social Care. UK Chief Medical Officers’ Physical Activity Guidelines; Department of Health and Social Care: London, UK, 2019.
- Ahmad, S.; Harris, T.; Limb, E.; Kerry, S.; Victor, C.; Ekelund, U.; Iliffe, S.; Whincup, P.; Beighton, C.; Ussher, M.; et al. Evaluation of reliability and validity of the General Practice Physical Activity Questionnaire (GPPAQ) in 60-74 year old primary care patients. BMC Fam. Pract. 2015, 16, 113. [Google Scholar] [CrossRef] [PubMed]
- Roccaforte, W.H.; Burke, W.J.; Bayer, B.L.; Wengel, S.P. Validation of a telephone version of the mini-mental state examination. J. Am. Geriatr. Soc. 1992, 40, 697–702. [Google Scholar] [CrossRef]
- Raîche, M.; Hébert, R.; Dubois, M.F. PRISMA-7: A case-finding tool to identify older adults with moderate to severe disabilities. Arch. Gerontol. Geriatr. 2008, 47, 9–18. [Google Scholar] [CrossRef]
- Adams, R. Revised Physical Activity Readiness Questionnaire. Can. Fam. Physician 1999, 45, 992–995. [Google Scholar] [PubMed]
- Bandura, A. Social Foundations of Thought and Action: A Social Cognitive Theory; Prentice-Hall: Englewood Cliffs, NJ, USA, 1986. [Google Scholar]
- Michie, S.; van Stralen, M.M.; West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement Sci. 2011, 6, 42. [Google Scholar] [CrossRef]
- Michie, S.; Wood, C.E.; Johnston, M.; Abraham, C.; Francis, J.J.; Hardeman, W. Behaviour change techniques: The development and evaluation of a taxonomic method for reporting and describing behaviour change interventions (a suite of five studies involving consensus methods, randomised controlled trials and analysis of qualitative data). Health Technol. Assess. 2015, 19, 1–188. [Google Scholar] [CrossRef]
- Kerr, J.; Rosenberg, D.E.; Nathan, A.; Millstein, R.A.; Carlson, J.A.; Crist, K.; Wasilenko, K.; Bolling, K.; Castro, C.M.; Buchner, D.M.; et al. Applying the ecological model of behavior change to a physical activity trial in retirement communities: Description of the study protocol. Contemp. Clin. Trials 2012, 33, 1180–1188. [Google Scholar] [CrossRef]
- Kooiman, T.J.; Dontje, M.L.; Sprenger, S.R.; Krijnen, W.P.; van der Schans, C.P.; de Groot, M. Reliability and validity of ten consumer activity trackers. BMC Sports Sci. Med. Rehabil. 2015, 7, 24. [Google Scholar] [CrossRef]
- McDonough, S.M.; Tully, M.A.; O’Connor, S.R.; Boyd, A.; Kerr, D.P.; O’Neill, S.M.; Delitto, A.; Bradbury, I.; Tudor-Locke, C.; Baxter, D.G.; et al. The back 2 activity trial: Education and advice versus education and advice plus a structured walking programme for chronic low back pain. BMC Musculoskelet. Disord. 2010, 11, 163. [Google Scholar] [CrossRef]
- Harris, T.; Kerry, S.M.; Limb, E.S.; Victor, C.R.; Iliffe, S.; Ussher, M.; Whincup, P.H.; Ekelund, U.; Fox-Rushby, J.; Furness, C.; et al. Effect of a Primary Care Walking Intervention with and without Nurse Support on Physical Activity Levels in 45- to 75-Year-Olds: The Pedometer And Consultation Evaluation (PACE-UP) Cluster Randomised Clinical Trial. PLoS Med. 2017, 14, e1002210. [Google Scholar] [CrossRef]
- Kerr, J.; Rosenberg, D.; Millstein, R.A.; Bolling, K.; Crist, K.; Takemoto, M.; Godbole, S.; Moran, K.; Natarajan, L.; Castro-Sweet, C.; et al. Cluster randomized controlled trial of a multilevel physical activity intervention for older adults. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 32. [Google Scholar] [CrossRef] [PubMed]
- Müller-Riemenschneider, F.; Reinhold, T.; Nocon, M.; Willich, S.N. Long-term effectiveness of interventions promoting physical activity: A systematic review. Prev. Med. 2008, 47, 354–368. [Google Scholar] [CrossRef]
- Goyder, E.; Hind, D.; Breckon, J.; Dimairo, M.; Minton, J.; Everson-Hock, E.; Read, S.; Copeland, R.; Crank, H.; Horspool, K.; et al. A randomised controlled trial and cost-effectiveness evaluation of ‘booster’ interventions to sustain increases in physical activity in middle-aged adults in deprived urban neighbourhoods. Health Technol. Assess. 2014, 18, 1–210. [Google Scholar] [CrossRef]
- Jancey, J.; Lee, A.; Howat, P.; Clarke, A.; Wang, K.; Shilton, T. Reducing attrition in physical activity programs for older adults. J. Aging Phys. Act. 2007, 15, 152–165. [Google Scholar] [CrossRef]
- Boulton, E.; Hawley-Hague, H.; French, D.P.; Mellone, S.; Zacchi, A.; Clemson, L.; Vereijken, B.; Todd, C. Implementing behaviour change theory and techniques to increase physical activity and prevent functional decline among adults aged 61-70: The PreventIT project. Prog. Cardiovasc. Dis. 2019, 62, 147–156. [Google Scholar] [CrossRef]
- Best, K.L.; Miller, W.C.; Eng, J.J.; Routhier, F. Systematic Review and Meta-Analysis of Peer-Led Self-Management Programs for Increasing Physical Activity. Int. J. Behav. Med. 2016, 23, 527–538. [Google Scholar] [CrossRef] [PubMed]
- Migueles, J.H.; Cadenas-Sanchez, C.; Ekelund, U.; Delisle Nyström, C.; Mora-Gonzalez, J.; Löf, M.; Labayen, I.; Ruiz, J.R.; Ortega, F.B. Accelerometer Data Collection and Processing Criteria to Assess Physical Activity and Other Outcomes: A Systematic Review and Practical Considerations. Sports Med. 2017, 47, 1821–1845. [Google Scholar] [CrossRef] [PubMed]
- Trost, S.G.; McIver, K.L.; Pate, R.R. Conducting accelerometer-based activity assessments in field-based research. Med. Sci. Sports Exerc. 2005, 37 (Suppl. S11), S531–S543. [Google Scholar] [CrossRef]
- Freedson, P.S.; Melanson, E.; Sirard, J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med. Sci. Sports Exerc. 1998, 30, 777–781. [Google Scholar] [CrossRef]
- Tennant, R.; Hiller, L.; Fishwick, R.; Platt, S.; Joseph, S.; Weich, S.; Parkinson, J.; Secker, J.; Stewart-Brown, S. The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): Development and UK validation. Health Qual. Life Outcomes 2007, 5, 63. [Google Scholar] [CrossRef]
- Lloyd, K.; Devine, P. Psychometric properties of the Warwick-Edinburgh Mental Well-being Scale (WEMWBS) in Northern Ireland. J. Ment. Health 2012, 21, 257–263. [Google Scholar] [CrossRef]
- Herdman, M.; Gudex, C.; Lloyd, A.; Janssen, M.; Kind, P.; Parkin, D.; Bonsel, G.; Badia, X. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual. Life Res. 2011, 20, 1727–1736. [Google Scholar] [CrossRef]
- Russell, D.W. UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. J. Pers. Assess. 1996, 66, 20–40. [Google Scholar] [CrossRef]
- Lubben, J.E. Assessing social networks among elderly populations. Fam. Commy. Health 1998, 11, 42–52. [Google Scholar] [CrossRef]
- Guralnik, J.M.; Ferrucci, L.; Simonsick, E.M.; Salive, M.E.; Wallace, R.B. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N. Engl. J. Med. 1995, 332, 556–561. [Google Scholar] [CrossRef] [PubMed]
- Resnick, B.; Palmer, M.H.; Jenkins, L.S.; Spellbring, A.M. Path analysis of efficacy expectations and exercise behaviour in older adults. J. Adv. Nurs. 2000, 31, 1309–1315. [Google Scholar] [CrossRef] [PubMed]
- Steinhardt, M.A.; Dishman, R.K. Reliability and validity of expected outcomes and barriers for habitual physical activity. J. Occup. Med. 1989, 31, 536–546. [Google Scholar] [CrossRef] [PubMed]
- Umstattd, M.R.; Motl, R.; Wilcox, S.; Saunders, R.; Watford, M. Measuring physical activity self-regulation strategies in older adults. J. Phys. Act. Health 2009, 6 (Suppl. S1), S105–S112. [Google Scholar] [CrossRef]
- National Institute for Health and Care Research. Our Principles: The Principles that Guide the Development of NICE Guidance and Standards. Available online: https://www.nice.org.uk/about/who-we-are/our-principles (accessed on 26 February 2024).
- NICE Health Technology Evaluations: The Manual. Available online: https://www.nice.org.uk/process/pmg36/chapter/introduction-to-health-technology-evaluation (accessed on 10 December 2023).
- Husereau, D.; Drummond, M.; Augustovski, F.; de Bekker-Grob, E.; Briggs, A.H.; Carswell, C.; Caulley, L.; Chaiyakunapruk, N.; Greenberg, D.; Loder, E.; et al. Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) Statement: Updated Reporting Guidance for Health Economic Evaluations. Value Health 2022, 25, 3–9. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Excellence. Position Statement on Use of the EQ-5D-5L Value Set for England (Updated October 2019); National Institute for Health and Care Excellence: London, UK, 2019. [Google Scholar]
- Billingham, L.J.; Abrams, K.R.; Jones, D.R. Methods for the analysis of quality-of-life and survival data in health technology assessment. Health Technol. Assess. 1999, 3, 1–152. [Google Scholar] [CrossRef] [PubMed]
- Gc, V.S.; Suhrcke, M.; Atkin, A.J.; van Sluijs, E.; Turner, D. Cost-effectiveness of physical activity interventions in adolescents: Model development and illustration using two exemplar interventions. BMJ Open 2019, 9, e027566. [Google Scholar] [CrossRef] [PubMed]
- Frew, E.J.; Bhatti, M.; Win, K.; Sitch, A.; Lyon, A.; Pallan, M.; Adab, P. Cost-effectiveness of a community-based physical activity programme for adults (Be Active) in the UK: An economic analysis within a natural experiment. Br. J. Sports Med. 2014, 48, 207–212. [Google Scholar] [CrossRef] [PubMed]
- Roux, L.; Pratt, M.; Tengs, T.O.; Yore, M.M.; Yanagawa, T.L.; Van Den Bos, J.; Rutt, C.; Brownson, R.C.; Powell, K.E.; Heath, G.; et al. Cost effectiveness of community-based physical activity interventions. Am. J. Prev. Med. 2008, 35, 578–588. [Google Scholar] [CrossRef] [PubMed]
- Deidda, M.; Coll-Planas, L.; Giné-Garriga, M.; Guerra-Balic, M.; Roqué I Figuls, M.; Tully, M.A.; Caserotti, P.; Rothenbacher, D.; Salvà Casanovas, A.; Kee, F.; et al. Cost-effectiveness of exercise referral schemes enhanced by self-management strategies to battle sedentary behaviour in older adults: Protocol for an economic evaluation alongside the SITLESS three-armed pragmatic randomised controlled trial. BMJ Open 2018, 8, e022266. [Google Scholar] [CrossRef] [PubMed]
- Adalsteinsson, E.; Toumi, M. Benefits of probabilistic sensitivity analysis—A review of NICE decisions. J. Mark Access Health Policy 2013, 1, 21240. [Google Scholar] [CrossRef]
- Schulz, K.F.; Altman, D.G.; Moher, D.; CONSORT Group. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. BMJ 2010, 340, c332. [Google Scholar] [CrossRef]
- Larsen, R.T.; Christensen, J.; Juhl, C.B.; Andersen, H.B.; Langberg, H. Physical activity monitors to enhance amount of physical activity in older adults—A systematic review and meta-analysis. Eur. Rev. Aging Phys. Act. 2019, 16, 7. [Google Scholar] [CrossRef]
- S Oliveira, J.; Sherrington, C.; R Y Zheng, E.; Franco, M.R.; Tiedemann, A. Effect of interventions using physical activity trackers on physical activity in people aged 60 years and over: A systematic review and meta-analysis. Br. J. Sports Med. 2020, 54, 1188–1194. [Google Scholar] [CrossRef]
- Moore, G.F.; Audrey, S.; Barker, M.; Bond, L.; Bonell, C.; Hardeman, W.; Moore, L.; O’Cathain, A.; Tinati, T.; Wight, D.; et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015, 350, h1258. [Google Scholar] [CrossRef]
- Wiltsey Stirman, S.; Baumann, A.A.; Miller, C.J. The FRAME: An expanded framework for reporting adaptations and modifications to evidence-based interventions. Implement. Sci. 2019, 14, 58. [Google Scholar] [CrossRef] [PubMed]
- Barnett, D.W.; Barnett, A.; Nathan, A.; Van Cauwenberg, J.; Cerin, E.; Council on Environment and Physical Activity (CEPA)—Older Adults working group. Built environmental correlates of older adults’ total physical activity and walking: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 103. [Google Scholar] [CrossRef] [PubMed]
- Goodrich, D.E.; Larkin, A.R.; Lowery, J.C.; Holleman, R.G.; Richardson, C.R. Adverse events among high-risk participants in a home-based walking study: A descriptive study. Int. J. Behav. Nutr. Phys. Act. 2007, 4, 20. [Google Scholar] [CrossRef] [PubMed][Green Version]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cunningham, C.; O’Doherty, M.; Neill, R.D.; Adams, M.; Kee, F.; Cupples, M.E.; Hardeman, W.; Simpson, E.E.A.; Murphy, M.H.; Callaghan, C.; et al. The Effectiveness and Cost-Effectiveness of the ‘Walk with Me’ Peer-Led Walking Intervention to Increase Physical Activity in Inactive Older Adults: Study Protocol for a Randomised Controlled Trial. J. Ageing Longev. 2024, 4, 28-40. https://doi.org/10.3390/jal4010003
Cunningham C, O’Doherty M, Neill RD, Adams M, Kee F, Cupples ME, Hardeman W, Simpson EEA, Murphy MH, Callaghan C, et al. The Effectiveness and Cost-Effectiveness of the ‘Walk with Me’ Peer-Led Walking Intervention to Increase Physical Activity in Inactive Older Adults: Study Protocol for a Randomised Controlled Trial. Journal of Ageing and Longevity. 2024; 4(1):28-40. https://doi.org/10.3390/jal4010003
Chicago/Turabian StyleCunningham, Conor, Maeve O’Doherty, Ruth D. Neill, Michael Adams, Frank Kee, Margaret E. Cupples, Wendy Hardeman, Ellen Elizabeth Anne Simpson, Marie H. Murphy, Chris Callaghan, and et al. 2024. "The Effectiveness and Cost-Effectiveness of the ‘Walk with Me’ Peer-Led Walking Intervention to Increase Physical Activity in Inactive Older Adults: Study Protocol for a Randomised Controlled Trial" Journal of Ageing and Longevity 4, no. 1: 28-40. https://doi.org/10.3390/jal4010003
APA StyleCunningham, C., O’Doherty, M., Neill, R. D., Adams, M., Kee, F., Cupples, M. E., Hardeman, W., Simpson, E. E. A., Murphy, M. H., Callaghan, C., O’Sullivan, R., Brolly, C., Agus, A., McDowell, C., Laventure, B., Casey, S., McDonough, S. M., & Tully, M. A. (2024). The Effectiveness and Cost-Effectiveness of the ‘Walk with Me’ Peer-Led Walking Intervention to Increase Physical Activity in Inactive Older Adults: Study Protocol for a Randomised Controlled Trial. Journal of Ageing and Longevity, 4(1), 28-40. https://doi.org/10.3390/jal4010003






