Designing for Special Neurological Conditions: Architecture Design Criteria for Anti-Misophonia and Anti-ADHD Spaces for Enhanced User Experience
Abstract
1. Introduction: Research Problem, Objectives, Scope, and Limitations
1.1. What Is Misophonia
1.2. What Is ADHD
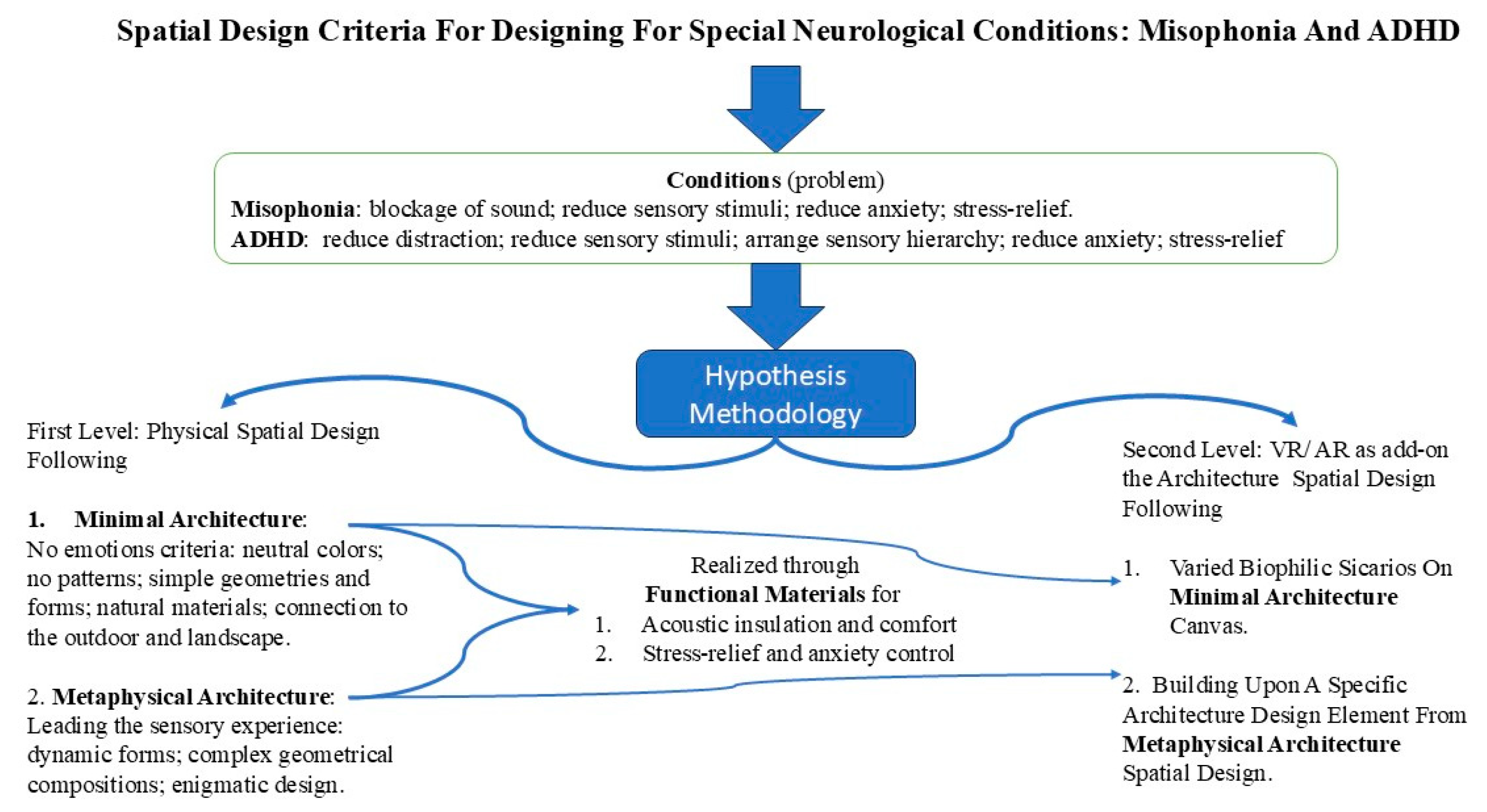
2. Methodology
2.1. Minimal and Metaphysical Architecture in Designing Therapeutic Spaces for Special Neurological Needs (First Level of Intervention)
2.1.1. Minimal Architecture (The “No Emotions” Criteria)
2.1.2. Metaphysical Architecture (Leading the Sensory–Cognitive Experience)
2.2. Advanced Functional Architectural Materials with Therapeutic Value for Special Neurological Needs (Misophonia and ADHD) (First Level of Intervention)
2.2.1. Sound-Blocking Acoustic Materials
2.2.2. Stress-Relief Materials
2.3. VR/AR as an Immersive Therapeutic Approach (An Architectural Add-On) (Second Level of Intervention)
2.3.1. Allowing for the Extension of Spatial Design in Therapeutic VR/AR
2.3.2. Allowing for Building upon the Architectural Scene and Elements to Augment, Connect, and Lead the Sensory Experience
3. Validation and Future Research
4. Conclusions
Supplementary Materials
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- St-Jean, P.; Clark, O.G.; Jemtrud, M. A review of the effects of architectural stimuli on human psychology and physiology. Build. Environ. 2022, 219, 109182. [Google Scholar] [CrossRef]
- Vitoratou, S.; Hayes, C.; Uglik-Marucha, N.; Pearson, O.; Graham, T.; Gregory, J. Misophonia in the UK: Prevalence and norms from the S-Five in a UK representative sample. PLoS ONE 2023, 18, e0282777. [Google Scholar] [CrossRef]
- Misophonia. OHSPIC. 2024. Available online: https://www.oxfordhealth.nhs.uk/ohspic/problems/misophonia/ (accessed on 25 August 2025).
- Neacsiu, A.D.; Szymkiewicz, V.; Galla, J.T.; Li, B.; Kulkarni, Y.; Spector, C.W. The neurobiology of misophonia and implications for novel, neuroscience-driven interventions. Front. Neurosci. 2022, 16, 893903. [Google Scholar] [CrossRef] [PubMed]
- Schröder, A.; van Wingen, G.; Eijsker, N.; San Giorgi, R.; Vulink, N.C.; Turbyne, C.; Denys, D. Misophonia is associated with altered brain activity in the auditory cortex and salience network. Sci. Rep. 2019, 9, 7542. [Google Scholar] [CrossRef] [PubMed]
- Jastreboff, M.; Jastreboff, P. Treatments for Decreased Sound Tolerance (Hyperacusis and Misophonia). Semin. Hear. 2014, 35, 105–120. [Google Scholar] [CrossRef]
- Gregory, J.; Foster, C. Session-by-session change in misophonia: A descriptive case study using intensive CBT. Cogn. Behav. Ther. 2023, 16, e18. [Google Scholar] [CrossRef] [PubMed]
- Jager, I.J.; Vulink, N.C.C.; Bergfeld, I.O.; Loon, A.J.J.M.; Denys, D.A.J.P. Cognitive behavioral therapy for misophonia: A randomized clinical trial. Depress. Anxiety 2020, 38, 708–718. [Google Scholar] [CrossRef]
- Yin, J.; Yuan, J.; Arfaei, N.; Catalano, P.J.; Allen, J.G.; Spengler, J.D. Effects of biophilic indoor environment on stress and anxiety recovery: A between-subjects experiment in virtual reality. Environ. Int. 2020, 136, 105427. [Google Scholar] [CrossRef]
- Gaekwad, J.S.; Sal Moslehian, A.; Roös, P.B.; Walker, A. A Meta-Analysis of Emotional Evidence for the Biophilia Hypothesis and Implications for Biophilic Design. Front. Psychol. 2020, 13, 750245. [Google Scholar] [CrossRef]
- Teixeira, A.; Brito-costa, S.; Gomes, A. Colors in Mind: A Comprehensive Study on the Neurological Impact of Saturation. AHFE Int. 2024, 142. [Google Scholar] [CrossRef]
- Kexiu, L.; Elsadek, M.; Liu, B.; Fujii, E. Foliage colors improve relaxation and emotional status of university students from different countries. Heliyon 2021, 7, e06131. [Google Scholar] [CrossRef] [PubMed]
- SAP. What is Augmented Reality?|SAP Insights. 2024. Available online: https://www.sap.com/products/scm/industry-4-0/what-is-augmented-reality.html (accessed on 5 September 2025).
- Iloudi, M.; Lindner, P.; Ali, L.; Wallström, S.; Thunström, A.O.; Ioannou, M.; Anving, N.; Johansson, V.; Hamilton, W.; Falk, Ö.; et al. Physical Versus Virtual Reality-based Calm Rooms for Psychiatric Inpatients: A Quasi-randomized Trial (Preprint). J. Med. Internet Res. 2022, 25, e42365. [Google Scholar] [CrossRef]
- Ceradini, M.; Losanno, E.; Micera, S.; Bandini, A.; Orlandi, S. Immersive VR for upper-extremity rehabilitation in patients with neurological disorders: A scoping review. J. Neuroeng. Rehabil. 2024, 21, 75. [Google Scholar] [CrossRef] [PubMed]
- Sevcenko, K.; Lindgren, I. The effects of virtual reality training in stroke and Parkinson’s disease rehabilitation: A systematic review and a perspective on usability. Eur. Rev. Aging Phys. Act. 2022, 19, 4. [Google Scholar] [CrossRef]
- Nieto-Escamez, F.A.; Cortés-Pérez, I.; Obrero-Gaitán, E.; Fusco, A. Virtual Reality Applications in Neurorehabilitation: Current Panorama and Challenges. Brain Sci. 2023, 13, 819. [Google Scholar] [CrossRef]
- Reilly, C.A.; Greeley, A.B.; Jevsevar, D.S.; Gitajn, I.L. Virtual reality-based physical therapy for patients with lower extremity injuries: Feasibility and acceptability. OTA Int. 2021, 4, e132. [Google Scholar] [CrossRef]
- American Academy of Pediatrics. ADHD: Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Am. Acad. Pediatr. 2011, 128, 1007–1022. [Google Scholar] [CrossRef]
- Peri, S.P.; Parveen, S. Attention deficit and hyperactivity disorder (ADHD): Overview of Gender differences, Genetic, Epigenetic, and Non-genetic aspects. J. Adv. Appl. Sci. Res. 2023, 5. [Google Scholar]
- Gnanavel, S.; Sharma, P.; Kaushal, P.; Hussain, S. Attention deficit hyperactivity disorder and comorbidity: A review of literature. World J. Clin. Cases 2019, 7, 2420–2426. [Google Scholar] [CrossRef]
- Substance Abuse and Mental Health Services Administration. Table 7, DSM-IV to DSM-5 Attention-Deficit/Hyperactivity Disorder Comparison. Nih.gov. 2016. Available online: https://www.ncbi.nlm.nih.gov/books/NBK519712/table/ch3.t3/ (accessed on 1 July 2025).
- Catalá-López, F.; Hutton, B. El tratamiento del trastorno por déficit de atención e hiperactividad en niños y adolescentes: Epidemiología, multimorbilidad y servicios de salud integrados. An. Pediatría 2018, 88, 181–182. [Google Scholar] [CrossRef] [PubMed]
- Rosack, J. Brain Scans Reveal Physiology of ADHD. Psychiatr. News 2004, 39, 26–27. [Google Scholar] [CrossRef]
- Wilens, T.E.; Spencer, T.J. Understanding Attention-Deficit/Hyperactivity Disorder from Childhood to Adulthood. Postgrad. Med. 2010, 122, 97–109. [Google Scholar] [CrossRef] [PubMed]
- Matte, B.; Rohde, L.A.; Turner, J.B.; Fisher, P.W.; Shen, S.; Bau, C.H.D.; Nigg, J.T.; Grevet, E.H. Reliability and Validity of Proposed DSM-5 ADHD Symptoms in a Clinical Sample of Adults. J. Neuropsychiatry Clin. Neurosci. 2015, 27, 228–236. [Google Scholar] [CrossRef] [PubMed]
- Wolraich, M.L.; Hagan, J.F.; Allan, C.; Chan, E.; Davison, D.; Earls, M.; Evans, S.W.; Flinn, S.K.; Froehlich, T.; Frost, J.; et al. Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics 2020, 144, e20192528. [Google Scholar] [CrossRef]
- Cabral, M.D.I.; Liu, S.; Soares, N. Attention-deficit/hyperactivity disorder: Diagnostic criteria, epidemiology, risk factors and evaluation in youth. Transl. Pediatr. 2020, 9, S104–S113. [Google Scholar] [CrossRef]
- Ra, C.K.; Cho, J.; Stone, M.D.; De La Cerda, J.; Goldenson, N.I.; Moroney, E.; Tung, I.; Lee, S.S.; Leventhal, A.M. Association of Digital Media Use with Subsequent Symptoms of Attention-Deficit/Hyperactivity Disorder Among Adolescents. JAMA 2018, 320, 255. [Google Scholar] [CrossRef]
- Montag, C.; Lachmann, B.; Herrlich, M.; Zweig, K. Addictive Features of Social media/messenger Platforms and Freemium Games against the Background of Psychological and Economic Theories. Int. J. Environ. Res. Public Health 2019, 16, 2612. [Google Scholar] [CrossRef] [PubMed]
- Lemola, S.; Perkinson-Gloor, N.; Brand, S.; Dewald-Kaufmann, J.F.; Grob, A. Adolescents’ Electronic Media Use at Night, Sleep Disturbance, and Depressive Symptoms in the Smartphone Age. J. Youth Adolesc. 2015, 44, 405–418. [Google Scholar] [CrossRef]
- El Archi, S.; Barrault, S.; Brunault, P.; Ribadier, A.; Varescon, I. Co-occurrence of Adult ADHD Symptoms and Problematic Internet Use and Its Links with Impulsivity, Emotion Regulation, Anxiety, and Depression. Front. Psychiatry 2022, 13, 792206. [Google Scholar] [CrossRef]
- Bashiri, A.; Ghazisaeedi, M.; Shahmoradi, L. The opportunities of virtual reality in the rehabilitation of children with attention deficit hyperactivity disorder: A literature review. Korean J. Pediatr. 2017, 60, 337. [Google Scholar] [CrossRef]
- Romero-Ayuso, D.; Toledano-González, A.; del Rodríguez-Martínez, M.C.; Arroyo-Castillo, P.; Triviño-Juárez, J.M.; González, P.; Ariza-Vega, P.; Del González, A.P.; Segura-Fragoso, A. Effectiveness of Virtual Reality-Based Interventions for Children and Adolescents with ADHD: A Systematic Review and Meta-Analysis. Children 2021, 8, 70. [Google Scholar] [CrossRef]
- Wong, K.P.; Zhang, B.; Yuen, C.; Xie, Y.J.; Li, Y.; Li, C.; Qin, J. Empowering Social Growth Through Virtual Reality–Based Intervention for Children with Attention-Deficit/Hyperactivity Disorder: 3-Arm Randomized Controlled Trial. JMIR Serious Games 2024, 12, e58963. [Google Scholar] [CrossRef]
- Zhang, W.; Li, H.; Sheng, Y. A Study of the Effects of Virtual Reality-Based Sports Games on Improving Executive and Cognitive Functions in Minors with ADHD—A Meta-Analysis of Randomized Controlled Trials. Behav. Sci. 2024, 14, 1141. [Google Scholar] [CrossRef] [PubMed]
- Shema-Shiratzky, S.; Brozgol, M.; Cornejo-Thumm, P.; Geva-Dayan, K.; Rotstein, M.; Leitner, Y.; Hausdorff, J.M.; Mirelman, A. Virtual reality training to enhance behavior and cognitive function among children with attention-deficit/hyperactivity disorder: Brief report. Dev. Neurorehabilit. 2018, 22, 431–436. [Google Scholar] [CrossRef] [PubMed]
- Gajanova, L.; Nadanyiova, M.; Moravcikova, D. The Use of Demographic and Psychographic Segmentation to Creating Marketing Strategy of Brand Loyalty. Sci. Ann. Econ. Bus. 2019, 66, 65–84. [Google Scholar] [CrossRef]
- Al Sayyed, H.; Al-Azhari, W. Investigating the role of biophilic design to enhance comfort in residential spaces: Human physiological response in immersive virtual environment. Front. Virtual Real. 2025, 6, 1411425. [Google Scholar] [CrossRef]
- Vasilski, D. Minimalism in architecture: Abstract conceptualization of architecture. Arhit. I Urban. 2015, 16–23. [Google Scholar] [CrossRef]
- Kamal, M.; Nasir, O. Minimalism in architecture: A basis for resource conservation and sustainable development. Facta Univ.-Ser. Archit. Civ. Eng. 2022, 20, 277–300. [Google Scholar] [CrossRef]
- Robinson, S. Designing Movement, Modulating Mood. Dimensions 2021, 1, 97–112. [Google Scholar] [CrossRef]
- Neuendorfhouse.com. Neuendorf House|Home. 2025. Available online: https://neuendorfhouse.com/ (accessed on 27 May 2025).
- Higuera-Trujillo, J.L.; Llinares, C.; Macagno, E. The Cognitive-Emotional Design and Study of Architectural Space: A Scoping Review of Neuroarchitecture and Its Precursor Approaches. Sensors 2021, 21, 2193. [Google Scholar] [CrossRef]
- Djebbara, Z.; King, J.; Ebadi, A.; Nakamura, Y.; Bermudez, J. Contemplative neuroaesthetics and architecture: A sensorimotor exploration. Front. Archit. Res. 2023, 13, 97–111. [Google Scholar] [CrossRef]
- Spence, C. Senses of Place: Architectural Design for the Multisensory Mind. Cogn. Res. Princ. Implic. 2020, 5, 46. [Google Scholar] [CrossRef] [PubMed]
- Thampanichwat, C.; Meksrisawat, P.; Jinjantarawong, N.; Sinnugool, S.; Phaibulputhipong, P.; Chunhajinda, P.; Bhutdhakomut, B. A Systematic Review of Architecture Stimulating Attention through the Six Senses of Humans. Sustainability 2024, 16, 6371. [Google Scholar] [CrossRef]
- esplugues.cat. Espacio Corberó|Esplugues.Cat. 2022. Available online: https://www.esplugues.cat/es/espai-corbero/ (accessed on 4 August 2025).
- Santini, F. Giorgio De Chirico can Influence Your Photography-2-Francesco Santini. Francesco Santini. 2020. Available online: https://www.santiniphotography.com/blog/giorgio-de-chirico-can-influence-your-photography-2/ (accessed on 4 August 2025).
- Tao, Y.; Ren, M.; Zhang, H.; Peijs, T. Recent progress in acoustic materials and noise control strategies—A review. Appl. Mater. Today 2021, 24, 101141. [Google Scholar] [CrossRef]
- Arjunan, A.; Baroutaji, A.; Robinson, J.; Vance, A.; Arafat, A. Acoustic metamaterials for sound absorption and insulation in buildings. Build. Environ. 2024, 251, 111250. [Google Scholar] [CrossRef]
- Zewe, A. This Sound-Suppressing Silk Can CREATE Quiet Spaces; MIT News|Massachusetts Institute of Technology: Cambridge, MA, USA, 2024; Available online: https://news.mit.edu/2024/sound-suppressing-silk-can-create-quiet-spaces-0507 (accessed on 4 August 2025).
- Bonga, K.B.; Bertolacci, L.; Contardi, M.; Paul, U.C.; Zafar, M.S.; Mancini, G.; Marini, L.; Ceseracciu, L.; Fragouli, D.; Athanassiou, A. Mycelium Agrowaste-Bound Biocomposites as Thermal and Acoustic Insulation Materials in Building Construction. Macromol. Mater. Eng. 2024, 309, 2300449. [Google Scholar] [CrossRef]
- Walter, N.; Gürsoy, B. A Study on the Sound Absorption Properties of Mycelium-Based Composites Cultivated on Waste Paper-Based Substrates. Biomimetics 2022, 7, 100. [Google Scholar] [CrossRef] [PubMed]
- Shah, R.; Greenberger, P.A. Chapter 29: Unproved and controversial methods and theories in allergy-immunology. Allergy Asthma Proc. 2012, 33, 100–102. [Google Scholar] [CrossRef][Green Version]
- Coppus, J. Harnessing Halotherapy and Himalayan Salt: A Natural Approach to Neurological Wellness; Delta Neuro Health: Westerville, OH, USA, 2024; Available online: https://www.deltaneurohealth.com/post/harnessing-halotherapy-and-himalayan-salt-a-natural-approach-to-neurological-wellness?utm_source=chatgpt.com (accessed on 7 July 2025).[Green Version]
- Hariri, H.H.; Schlenoff, J.B. Saloplastic Macroporous Polyelectrolyte Complexes: Cartilage Mimics. Macromolecules 2010, 43, 8656–8663. [Google Scholar] [CrossRef]
- Li, J.; Li, L.; Brink, H.A.; Allegri, G.; Lindhoud, S. Polyelectrolyte complex-based materials for separations: Progress, challenges and opportunities. Mater. Horiz. 2025, 12, 4998–5030. [Google Scholar] [CrossRef]
- Porcel, C.H.; Schlenoff, J.B. Compact Polyelectrolyte Complexes: ‘Saloplastic’ Candidates for Biomaterials. Biomacromolecules 2009, 10, 2968–2975. [Google Scholar] [CrossRef] [PubMed]
- Munir, I. Promoting Brain Health with Salt Therapy and the Power of Salt Bricks. Pink Salt Wall. 2023. Available online: https://www.pinksaltwall.com/blogs/salt-therapy/promoting-brain-health-with-salt-therapy-and-the-power-of-salt-bricks?utm_source=chatgpt.com (accessed on 7 July 2025).
- Corrigan, N.; Păsărelu, C.-R.; Voinescu, A. Immersive virtual reality for improving cognitive deficits in children with ADHD: A systematic review and meta-analysis. Virtual Real. 2023, 27, 3545–3564. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Ai, X.; Zhang, X.; Ma, F.; Zhuang, Y.; Wang, S. Evaluating virtual reality technology in psychotherapy: Impacts on anxiety, depression, and ADHD. Front. Psychiatry 2024, 15, 1480788. [Google Scholar] [CrossRef]
- Cho, G.H.; Hwangbo, G.; Shin, H.S. The Effects of Virtual Reality-based Balance Training on Balance of the Elderly. J. Phys. Ther. Sci. 2014, 26, 615–617. [Google Scholar] [CrossRef]
- Zheng, P.; Yuan, K.; Liu, S.; Xue, Z.; Ma, P.; Teo, E.W.; Chang, J. Effects of virtual reality technology on attention deficit in children with ADHD: A systematic review and Meta-analysis. J. Affect. Disord. 2025, 384, 127–134. [Google Scholar] [CrossRef]
- Sun, J.-L.; Chaw, X.-J.; Fresnoza, S.; Kuo, H.-I. Effects of virtual reality-based exercise intervention in young people with attention-deficit/hyperactivity disorder: A systematic review. J. Neuroeng. Rehabil. 2025, 22, 139. [Google Scholar] [CrossRef]
- Schröder, D.; Wrona, K.J.; Müller, F.; Heinemann, S.; Fischer, F.; Dockweiler, C. Impact of virtual reality applications in the treatment of anxiety disorders: A systematic review and meta-analysis of randomized-controlled trials. J. Behav. Ther. Exp. Psychiatry 2023, 81, 101893. [Google Scholar] [CrossRef]
- Holopainen, R.; Tiihonen, J.; Lähteenvuo, M. Efficacy of immersive extended reality (XR) interventions on different symptom domains of schizophrenia spectrum disorders. A systematic review. Front. Psychiatry 2023, 14, 1208287. [Google Scholar] [CrossRef]
- Tarrant, J.; Viczko, J.; Cope, H. Virtual Reality for Anxiety Reduction Demonstrated by Quantitative EEG: A Pilot Study. Front. Psychol. 2018, 9, 1280. [Google Scholar] [CrossRef]
- Hughes, C.L.; Fidopiastis, C.; Stanney, K.M.; Bailey, P.S.; Ruiz, E. The Psychometrics of Cybersickness in Augmented Reality. Front. Virtual Real. 2020, 1, 602954. [Google Scholar] [CrossRef]
- Zhang, J.; Che, X.; Chang, E.; Qu, C.; Di, X.; Liu, H.; Su, J. How different text display patterns affect cybersickness in augmented reality. Sci. Rep. 2024, 14, 11693. [Google Scholar] [CrossRef]
- Clemente-Suárez, V.J.; Beltrán-Velasco, A.I.; Herrero-Roldán, S.; Rodriguez-Besteiro, S.; Martínez-Guardado, I.; Martín-Rodríguez, A.; Tornero-Aguilera, J.F. Digital Device Usage and Childhood Cognitive Development: Exploring Effects on Cognitive Abilities. Children 2024, 11, 1299. [Google Scholar] [CrossRef]
- Frolli, A.; Savarese, G.; Di Carmine, F.; Bosco, A.; Saviano, E.; Rega, A.; Carotenuto, M.; Ricci, M.C. Children on the Autism Spectrum and the Use of Virtual Reality for Supporting Social Skills. Children 2022, 9, 181. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.-Q.; Zhang, X.-X.; Wang, C.-H.; Yang, J. Effect of cognitive training based on virtual reality on the children with autism spectrum disorder. Curr. Res. Behav. Sci. 2021, 2, 100013. [Google Scholar] [CrossRef]
- Adeyemi, V. The Impact of Digital Technology on Child’s Cognitive and Social Development: Implications for Education. Prem. J. Psychol. 2025, 2, 100006. [Google Scholar] [CrossRef]
- Lundin, R.M.; Yeap, Y.; Menkes, D.B. Adverse Effects of Virtual and Augmented Reality Interventions in Psychiatry: Systematic Review. JMIR Ment. Health 2023, 10, e43240. [Google Scholar] [CrossRef]
- Kanschik, D.; Bruno, R.R.; Wolff, G.; Kelm, M.; Jung, C. Virtual and augmented reality in intensive care medicine: A systematic review. Ann. Intensive Care 2023, 13, 81. [Google Scholar] [CrossRef]







Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abdallah, Y.K. Designing for Special Neurological Conditions: Architecture Design Criteria for Anti-Misophonia and Anti-ADHD Spaces for Enhanced User Experience. Architecture 2025, 5, 85. https://doi.org/10.3390/architecture5040085
Abdallah YK. Designing for Special Neurological Conditions: Architecture Design Criteria for Anti-Misophonia and Anti-ADHD Spaces for Enhanced User Experience. Architecture. 2025; 5(4):85. https://doi.org/10.3390/architecture5040085
Chicago/Turabian StyleAbdallah, Yomna K. 2025. "Designing for Special Neurological Conditions: Architecture Design Criteria for Anti-Misophonia and Anti-ADHD Spaces for Enhanced User Experience" Architecture 5, no. 4: 85. https://doi.org/10.3390/architecture5040085
APA StyleAbdallah, Y. K. (2025). Designing for Special Neurological Conditions: Architecture Design Criteria for Anti-Misophonia and Anti-ADHD Spaces for Enhanced User Experience. Architecture, 5(4), 85. https://doi.org/10.3390/architecture5040085




