Periodontal Regeneration
Definition
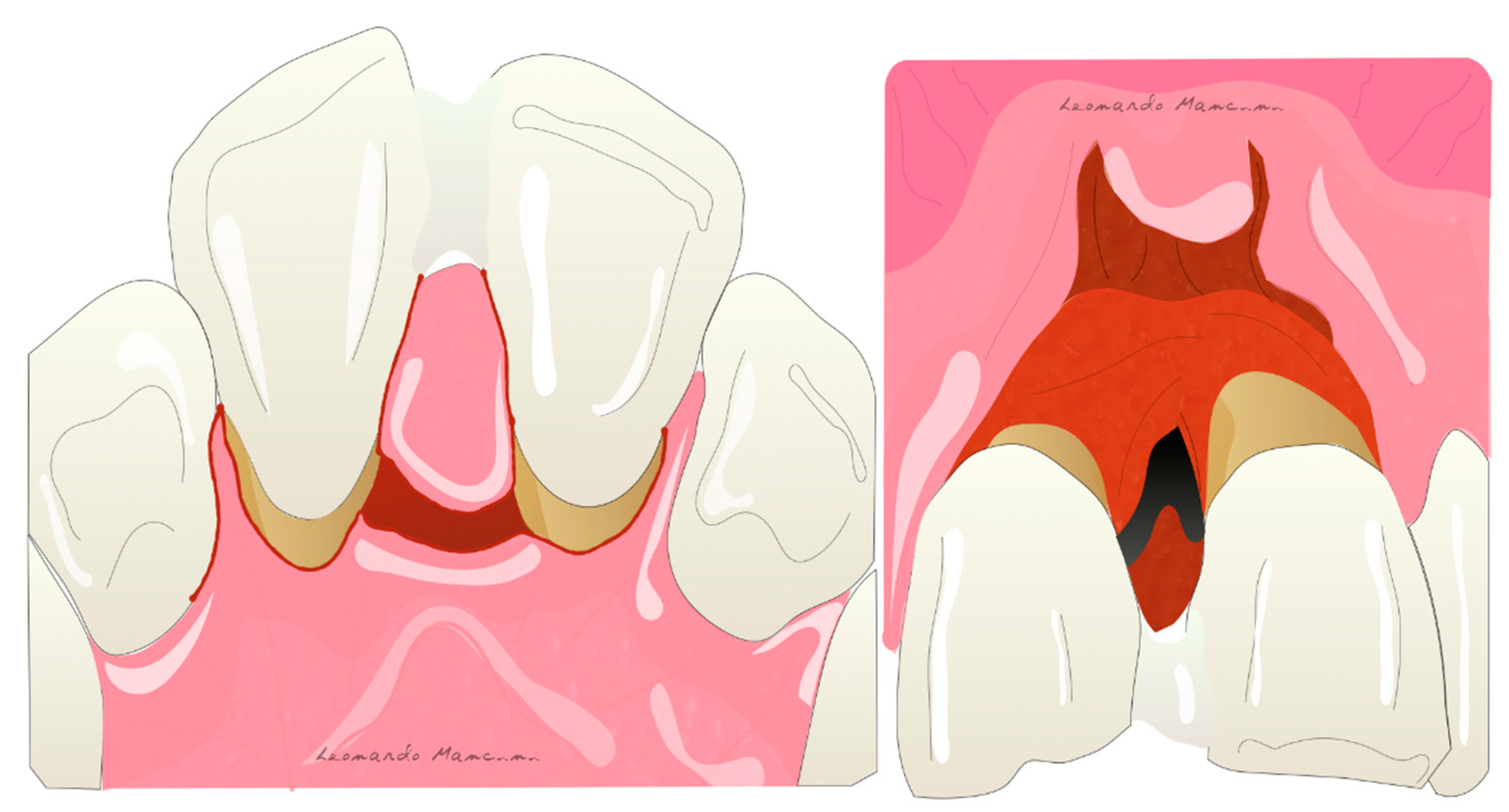
:1. Introduction and History
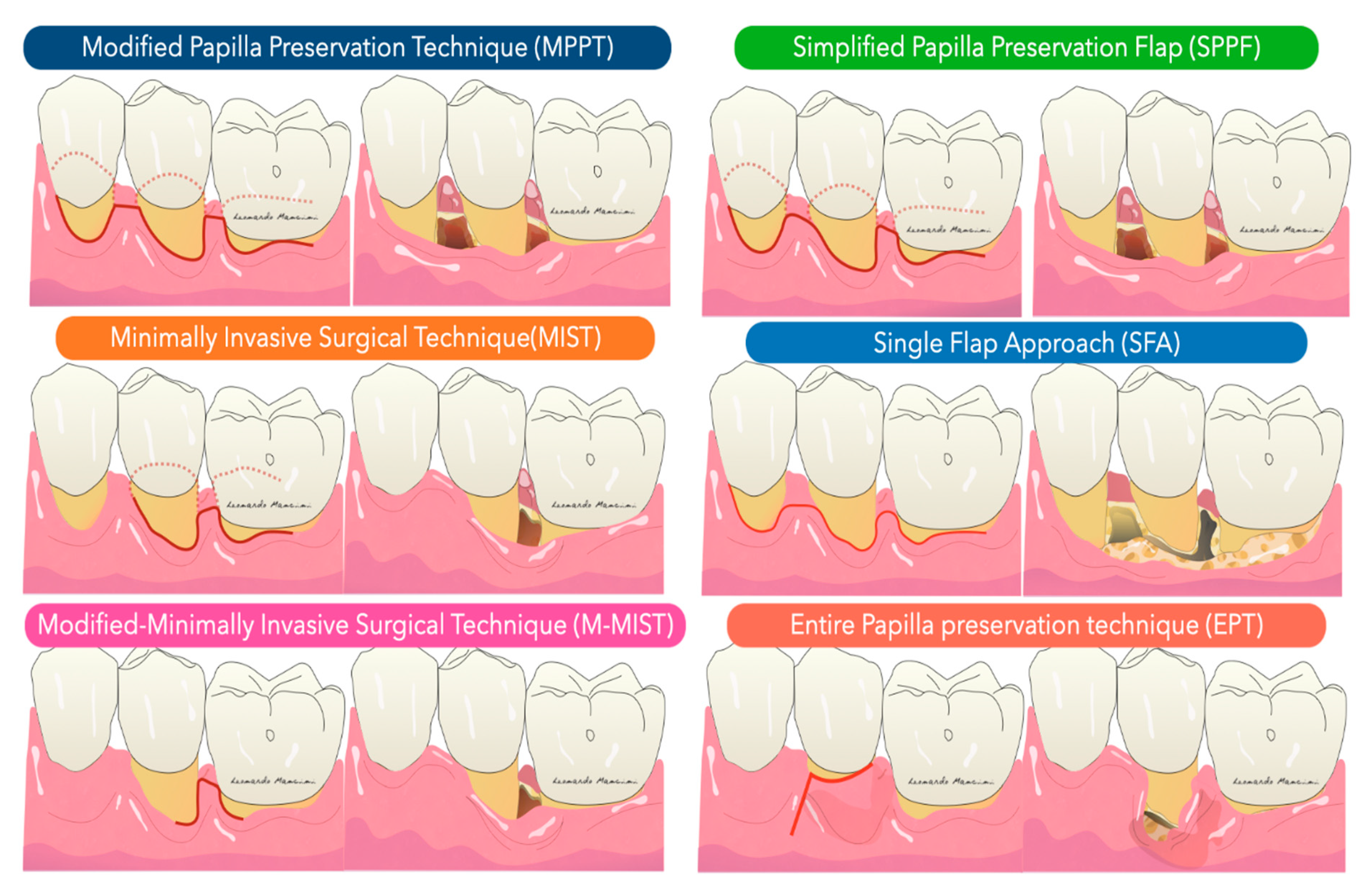
2. Techniques
3. Materials
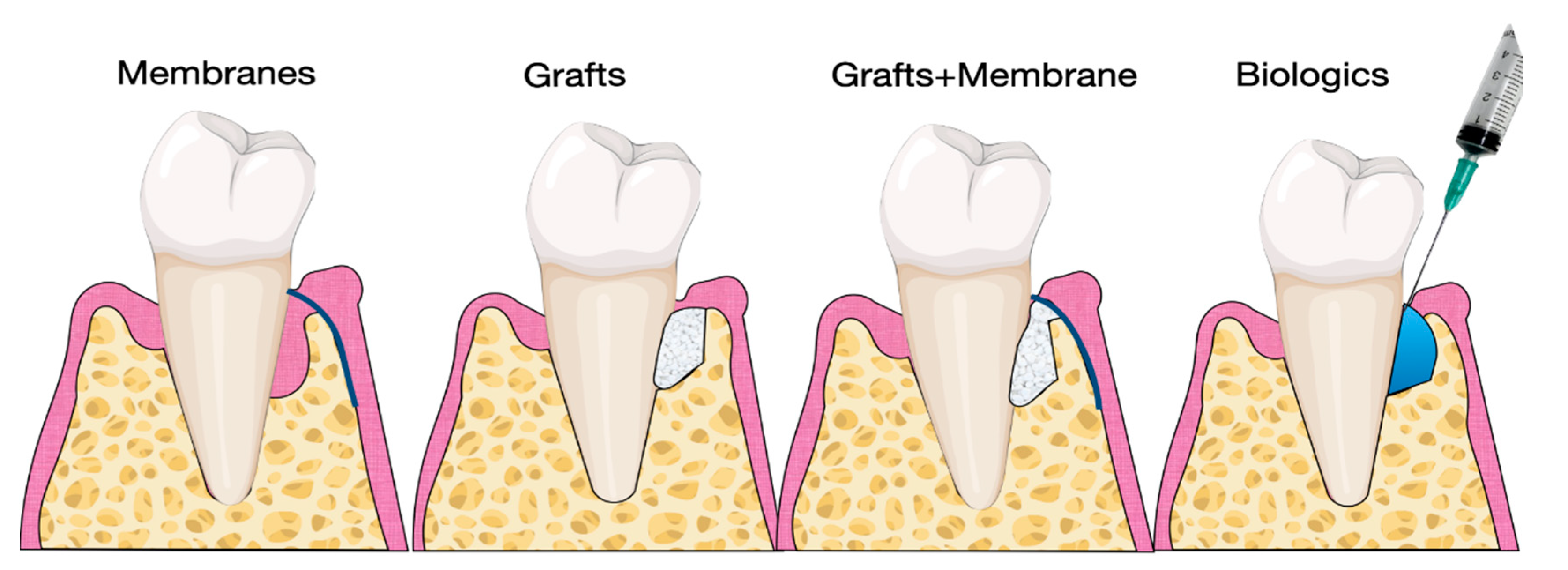
3.1. Grafts and Fillers
3.2. Membranes
- Biocompatibility: the membrane should not activate an immune response or an acute inflammation, which may worsen the regenerative phase.
- Cell-exclusion: it should act as a barrier and exclude specific types of cells.
- Tissue integration: it should prevent the down-growth of epithelial cells and the encapsulation of the material.
- Space-making: it should create and maintain space adjacent to the root surface, allowing the ingrowth of tissue from the periodontal ligament.
- Clinical handling: it should be easy to handle.
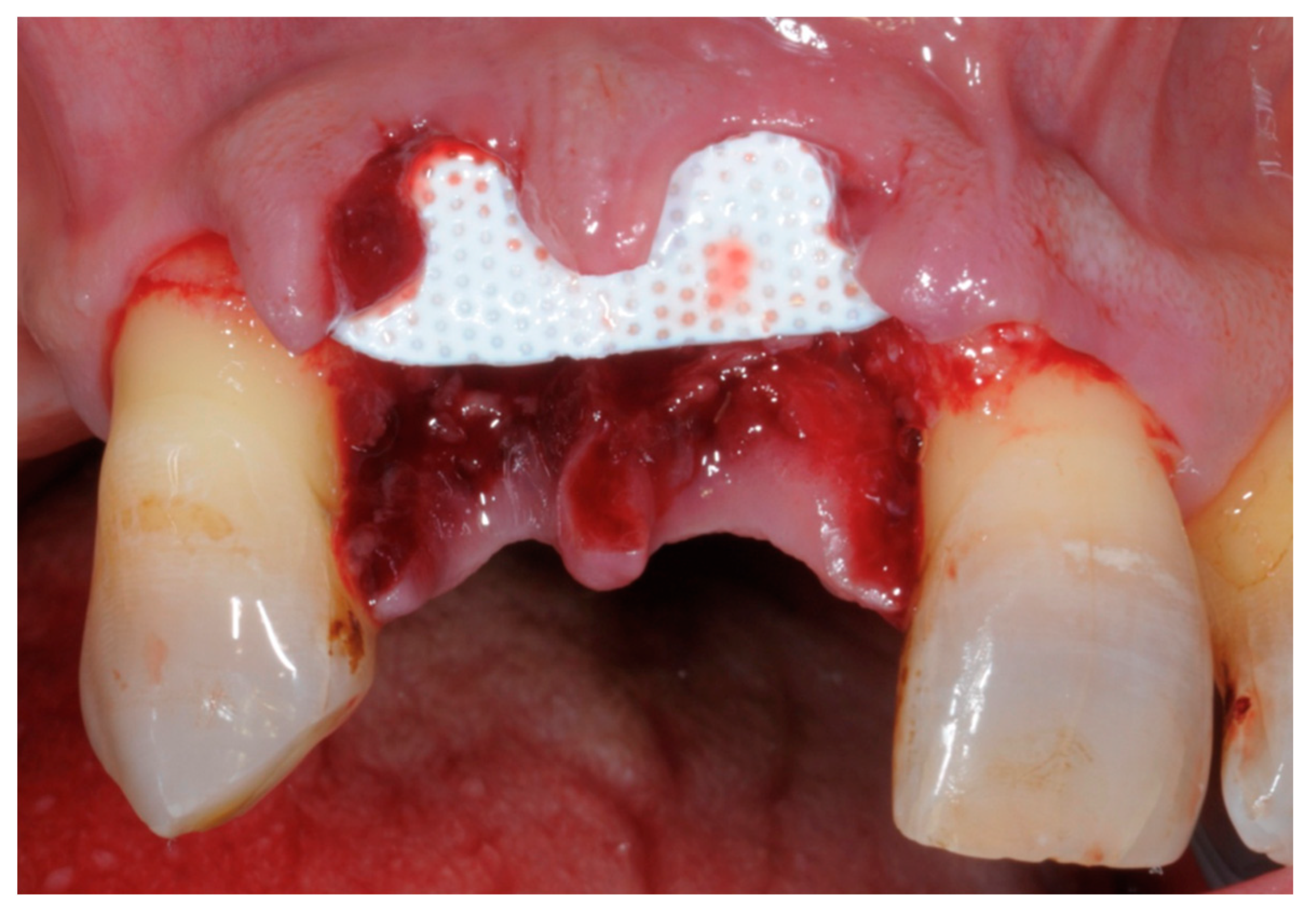
- Non-resorbable membranes are generally indicated in guided bone regeneration (GBR) or in situations of bone deficiency. They are no longer used in periodontal regeneration mainly because the introduction of minimal flaps does not allow the insertion of these unwieldy barriers. Titanium reinforced membranes and polytetrafluorethylene are the most common (Figure 5 and Figure 6). Nowadays, new technologies and the introduction of tissue engineering mean that the regenerative process is oriented towards the use of resorbable materials, avoiding the need for a second surgical phase [51,52].
- Resorbable membranes are made from collagen, a natural substance that can be resorbed (Figure 7). Several types are available, and these differ in resorption time. As reported in Table 1, the fabrication of these membranes may or may not involve cross-linking [53]. The cross-linking process aims to reinforce the chemical bonds among the collagen fibers, and this results in a long resorption time. Collagen membranes have a low risk of exposure in the oral cavity, but due to their low mechanical stability, the use of bone substitutes or fillers is also required [42]. The use of membranes raises the potential for complications such as exposure, which could reduce the regenerative potential and allow the infiltration of bacteria and possible infection of the site [42].
3.3. Biologics
3.4. Futures Biologics
3.5. Future Therapies
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
Entry Link on the Encyclopedia Platform
References
- Tonetti, M.S.; Eickholz, P.; Loos, B.G.; Papapanou, P.; van der Velden, U.; Armitage, G.; Bouchard, P.; Deinzer, R.; Dietrich, T.; Hughes, F.; et al. Principles in prevention of periodontal diseases: Consensus report of group 1 of the 11th European Workshop on Periodontology on effective prevention of periodontal and peri-implant diseases. J. Clin. Periodontol. 2015, 42, S5–S11. [Google Scholar] [CrossRef] [PubMed]
- Kassebaum, N.J.; Bernabé, E.; Dahiya, M.; Bhandari, B.; Murray, C.J.; Marcenes, W. Global burden of severe periodontitis in 1990–2010: A systematic review and meta-regression. J. Dent. Res. 2014, 93, 1045–1053. [Google Scholar] [CrossRef] [PubMed]
- Baehni, P.; Tonetti, M.S.; Group 1 of the European Workshop on Periodontology. Conclusions and consensus statements on periodontal health, policy and education in Europe: A call for action--consensus view 1. Consensus report of the 1st European Workshop on Periodontal Education. Eur. J. Dent. Educ. Off. J. Assoc. Dent. Educ. Eur. 2010, 14, 2–3. [Google Scholar] [CrossRef] [PubMed]
- Kinane, D.; Bouchard, P.; On Behalf of Group E of the European Workshop on Periodontology. Periodontal diseases and health: Consensus Report of the Sixth European Workshop on Periodontology. J. Clin. Periodontol. 2008, 35, 333–337. [Google Scholar] [CrossRef]
- Romandini, M.; Baima, G.; Antonoglou, G.; Bueno, J.; Figuero, E.; Sanz, M. Periodontitis, Edentulism, and Risk of Mortality: A Systematic Review with Meta-analyses. J. Dent. Res. 2021, 100, 37–49. [Google Scholar] [CrossRef]
- Hujoel, P.P. Endpoints in periodontal trials: The need for an evidence-based research approach. Periodontol. 2000 2004, 36, 196–204. [Google Scholar] [CrossRef]
- Claffey, N.; Egelberg, J. Clinical indicators of probing attachment loss following initial periodontal treatment in advanced periodontitis patients. J. Clin. Periodontol. 1995, 22, 690–696. [Google Scholar] [CrossRef]
- Matuliene, G.; Pjetursson, B.E.; Salvi, G.E.; Schmidlin, K.; Brägger, U.; Zwahlen, M.; Lang, N.P. Influence of residual pockets on progression of periodontitis and tooth loss: Results after 11 years of maintenance. J. Clin. Periodontol. 2008, 35, 685–695. [Google Scholar] [CrossRef]
- Lang, N.P.; Adler, R.; Joss, A.; Nyman, S. Absence of bleeding on probing. An indicator of periodontal stability. J. Clin. Periodontol. 1990, 17, 714–721. [Google Scholar] [CrossRef]
- Schätzle, M.; Löe, H.; Lang, N.P.; Bürgin, W.; Anerud, A.; Boysen, H. The clinical course of chronic periodontitis. J. Clin. Periodontol. 2004, 31, 1122–1127. [Google Scholar]
- Papapanou, P.N.; Wennström, J. The angular bony defect as indicator of further alveolar bone loss. J. Clin. Periodontol. 1991, 18, 317–322. [Google Scholar] [CrossRef] [PubMed]
- Rams, T.E.; Listgarten, M.A.; Slots, J. Radiographic alveolar bone morphology and progressive periodontitis. J. Clin. Periodontol. 2018, 89, 424–430. [Google Scholar] [CrossRef] [PubMed]
- Melcher, A.H. On the repair potential of periodontal tissues. J. Periodontol. 1976, 47, 256–260. [Google Scholar] [CrossRef] [PubMed]
- Nyman, S.; Lindhe, J.; Karring, T.; Rylander, H. New attachment following surgical treatment of human periodontal disease. J. Clin. Periodontol. 1982, 9, 290–296. [Google Scholar] [CrossRef]
- Gottlow, J.; Nyman, S.; Lindhe, J.; Karring, T.; Wennström, J. New attachment formation in the human periodontium by guided tissue regeneration. Case reports. J. Clin. Periodontol. 1986, 13, 604–616. [Google Scholar] [CrossRef] [PubMed]
- Susin, C.; Fiorini, T.; Lee, J.; De Stefano, J.A.; Dickinson, D.P.; Wikesjö, U.M. Wound healing following surgical and regenerative periodontal therapy. Periodontology 2000 2015, 68, 83–98. [Google Scholar] [CrossRef] [PubMed]
- Cortellini, P.; Tonetti, M.S. Clinical and radiographic outcomes of the modified minimally invasive surgical technique with and without regenerative materials: A randomized-controlled trial in intra-bony defects. J. Clin. Periodontol. 2011, 38, 365–373. [Google Scholar] [CrossRef]
- Pagliaro, U.; Cortellini, P.; Nieri, M.; Rotundo, R.; Cairo, F.; Pini-Prato, G.; Carnevale, G.; Esposito, M. Author’s Response: Re: Finkelman RD. Letter to the Editor: Re: “Clinical Guidelines of the Italian Society of Periodontology for the Reconstructive Surgical Treatment of Angular Bony Defects in Periodontal Patients”. J. Clin. Periodontol. 2009, 80, 722. [Google Scholar] [CrossRef]
- Tu, Y.K.; Woolston, A.; Faggion, C.M. Do bone grafts or barrier membranes provide additional treatment effects for infrabony lesions treated with enamel matrix derivatives? A network meta-analysis of randomized-controlled trials. J. Clin. Periodontol. 2010, 37, 59–79. [Google Scholar] [CrossRef]
- Bowers, G.M.; Chadroff, B.; Carnevale, R.; Mellonig, J.; Corio, R.; Emerson, J.; Stevens, M.; Romberg, E. Histologic evaluation of new attachment apparatus formation in humans. Part I. J. Periodontol. 1989, 60, 664–674. [Google Scholar] [CrossRef]
- Cortellini, P.; Pini Prato, G.; Tonetti, M.S. Periodontal regeneration of human infrabony defects. II. Re-entry procedures and bone measures. J. Periodontol. 1993, 64, 261–268. [Google Scholar] [CrossRef]
- Sculean, A.; Donos, N.; Blaes, A.; Lauermann, M.; Reich, E.; Brecx, M. Comparison of enamel matrix proteins and bioabsorbable membranes in the treatment of intrabony periodontal defects. A split-mouth study. J. Periodontol. 1999, 70, 255–262. [Google Scholar] [CrossRef] [PubMed]
- Sanz, M.; Tonetti, M.S.; Zabalegui, I.; Sicilia, A.; Blanco, J.; Rebelo, H.; Rasperini, G.; Merli, M.; Cortellini, P.; Suvan, J.E. Treatment of intrabony defects with enamel matrix proteins or barrier membranes: Results from a multicenter practice-based clinical trial. J. Periodontol. 2004, 75, 726–733. [Google Scholar] [CrossRef] [PubMed]
- Needleman, I.G.; Worthington, H.V.; Giedrys-Leeper, E.; Tucker, R.J. Guided tissue regeneration for periodontal infra-bony defects. Cochrane Database Syst. Rev. 2006, CD001724. [Google Scholar] [CrossRef]
- Kao, R.T.; Nares, S.; Reynolds, M.A. Periodontal regeneration—Intrabony defects: A systematic review from the AAP Regeneration Workshop. J. Periodontol. 2015, 86, S77–S104. [Google Scholar] [CrossRef]
- Selvig, K.A.; Kersten, B.G.; Wikesjö, U.M. Surgical treatment of intrabony periodontal defects using expanded polytetrafluoroethylene barrier membranes: Influence of defect configuration on healing response. J. Periodontol. 1993, 64, 730–733. [Google Scholar] [CrossRef] [PubMed]
- De Sanctis, M.; Zucchelli, G.; Clauser, C. Bacterial colonization of bioabsorbable barrier material and periodontal regeneration. J. Periodontol. 1996, 67, 1193–1200. [Google Scholar] [CrossRef]
- Cortellini, P.; Prato, G.P.; Tonetti, M.S. The modified papilla preservation technique. A new surgical approach for interproximal regenerative procedures. J. Periodontol. 1995, 66, 261–266. [Google Scholar] [CrossRef]
- Takei, H.H.; Han, T.J.; Carranza, F.A., Jr.; Kenney, E.B.; Lekovic, V. Flap technique for periodontal bone implants. Papilla preservation technique. J. Periodontol. 1985, 56, 204–210. [Google Scholar] [CrossRef]
- Cortellini, P.; Pini Prato, G.; Tonetti, M.S. Periodontal regeneration of human intrabony defects with titanium reinforced membranes. A controlled clinical trial. J. Periodontol. 1995, 66, 797–803. [Google Scholar] [CrossRef]
- Cortellini, P.; Prato, G.P.; Tonetti, M.S. The simplified papilla preservation flap. A novel surgical approach for the management of soft tissues in regenerative procedures. Int. J. Periodontics Restor. Dent. 1999, 19, 589–599. [Google Scholar]
- Cortellini, P.; Tonetti, M.S. A minimally invasive surgical technique with an enamel matrix derivative in the regenerative treatment of intra-bony defects: A novel approach to limit morbidity. J. Clin. Periodontol. 2007, 34, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Cortellini, P.; Tonetti, M.S. Microsurgical approach to periodontal regeneration. Initial evaluation in a case cohort. J. Periodontol. 2001, 72, 559–569. [Google Scholar] [CrossRef] [PubMed]
- Trombelli, L.; Farina, R.; Franceschetti, G. Use of the single flap approach in periodontal reconstructive surgery. Dent. Cadmos. 2007, 8, 15–25. [Google Scholar]
- Cortellini, P.; Tonetti, M.S. Improved wound stability with a modified minimally invasive surgical technique in the regenerative treatment of isolated interdental intrabony defects. J. Clin. Periodontol. 2009, 36, 157–163. [Google Scholar] [CrossRef]
- Aslan, S.; Buduneli, N.; Cortellini, P. Entire Papilla Preservation Technique: A Novel Surgical Approach for Regenerative Treatment of Deep and Wide Intrabony Defects. Int. J. Periodontics Restor. Dent. 2017, 37, 227–233. [Google Scholar] [CrossRef]
- Aslan, S.; Buduneli, N.; Cortellini, P. Entire papilla preservation technique in the regenerative treatment of deep intrabony defects: 1-Year results. J. Clin. Periodontol. 2017, 44, 926–932. [Google Scholar] [CrossRef]
- Bottino, M.C.; Thomas, V.; Schmidt, G.; Vohra, Y.K.; Chu, T.M.; Kowolik, M.J.; Janowski, G.M. Recent advances in the development of GTR/GBR membranes for periodontal regeneration--a materials perspective. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2012, 28, 703–721. [Google Scholar] [CrossRef]
- Sculean, A.; Stavropoulos, A.; Windisch, P.; Keglevich, T.; Karring, T.; Gera, I. Healing of human intrabony defects following regenerative periodontal therapy with a bovine-derived xenograft and guided tissue regeneration. Clin. Oral Investig. 2004, 8, 70–74. [Google Scholar] [CrossRef]
- Sculean, A.; Nikolidakis, D.; Nikou, G.; Ivanovic, A.; Chapple, I.L.; Stavropoulos, A. Biomaterials for promoting periodontal regeneration in human intrabony defects: A systematic review. Periodontology 2015, 68, 182–216. [Google Scholar] [CrossRef]
- Bosshardt, D.D.; Hjørting-Hansen, E.; Buser, D. The fate of the autogenous bone graft. Forum Implantol. 2009, 5, 4–11. [Google Scholar]
- Bosshardt, D.D.; Sculean, A. Does periodontal tissue regeneration really work? Periodontol. 2000 2009, 51, 208–219. [Google Scholar] [CrossRef] [PubMed]
- Windisch, P.; Szendroi-Kiss, D.; Horváth, A.; Suba, Z.; Gera, I.; Sculean, A. Reconstructive periodontal therapy with simultaneous ridge augmentation. A clinical and histological case series report. Clin. Oral Investig. 2008, 12, 257–264. [Google Scholar] [CrossRef] [PubMed]
- Sculean, A.; Windisch, P.; Keglevich, T.; Gera, I. Clinical and histologic evaluation of an enamel matrix protein derivative combined with a bioactive glass for the treatment of intrabony periodontal defects in humans. Int. J. Periodontics Restor. Dent. 2005, 25, 139–147. [Google Scholar]
- Wang, H.L.; Greenwell, H.; Fiorellini, J.; Giannobile, W.; Offenbacher, S.; Salkin, L.; Townsend, C.; Sheridan, P.; Genco, R.J.; Research, Science and Therapy Committee. Periodontal regeneration. J. Periodontol. 2005, 76, 1601–1622. [Google Scholar] [PubMed]
- Committee on Research, Science and Therapy of the American Academy of Periodontology. Tissue banking of bone allografts used in periodontal regeneration. J. Periodontol. 2001, 72, 834–838. [Google Scholar] [CrossRef] [PubMed]
- Dragoo, M.R.; Kaldahl, W.B. Clinical and histological evaluation of alloplasts and allografts in regenerative periodontal surgery in humans. Int. J. Periodontics Restor. Dent. 1983, 3, 8–29. [Google Scholar]
- Karring, T.; Nyman, S.; Gottlow, J.; Laurell, L. Development of the biological concept of guided tissue regeneration--animal and human studies. Periodontology 2000, 1, 26–35. [Google Scholar] [CrossRef]
- Urban, I.A.; Monje, A. Guided Bone Regeneration in Alveolar Bone Reconstruction. Oral Maxillofac. Surg. Clin. N. Am. 2019, 31, 331–338. [Google Scholar] [CrossRef]
- Bosshardt, D.D.; Stadlinger, B.; Terheyden, H. Cell-to-cell communication--periodontal regeneration. Clin. Oral Implant. Res. 2015, 26, 229–239. [Google Scholar] [CrossRef]
- Tavelli, L.; McGuire, M.K.; Zucchelli, G.; Rasperini, G.; Feinberg, S.E.; Wang, H.L.; Giannobile, W.V. Extracellular matrix-based scaffolding technologies for periodontal and peri-implant soft tissue regeneration. J. Periodontol. 2020, 91, 17–25. [Google Scholar] [CrossRef]
- Eickholz, P.; Kim, T.S.; Holle, R.; Hausmann, E. Long-term results of guided tissue regeneration therapy with non-resorbable and bioabsorbable barriers. I. Class II furcations. J. Periodontol. 2001, 72, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Behring, J.; Junker, R.; Walboomers, X.F.; Chessnut, B.; Jansen, J.A. Toward guided tissue and bone regeneration: Morphology, attachment, proliferation, and migration of cells cultured on collagen barrier membranes. A systematic review. Odontology 2008, 96, 1–11. [Google Scholar] [CrossRef]
- US FDA. What Are “Biologics” Questions and Answers. Available online: www.fda.gov/about-fda/center-biologics-evaluation-and-research-cber/what-are-biologics-questions-and-answers (accessed on 31 December 2020).
- Cambini, A.F.T.; Ordesi, P.; Arcara, C.; Caccianiga, G. Rigenerazione tissutale guidata in difetti infraosseimediante innesto di amelogenine. Dent. Clin. N. Am. 2012, 3, 19–26. [Google Scholar]
- Giannobile, W.V.; Somerman, M.J. Growth and amelogenin-like factors in periodontal wound healing. A systematic review. Ann. Periodontol. 2003, 8, 193–204. [Google Scholar] [CrossRef] [PubMed]
- Heijl, L.; Heden, G.; Svärdström, G.; Ostgren, A. Enamel matrix derivative (EMDOGAIN) in the treatment of intrabony periodontal defects. J. Clin. Periodontol. 1997, 24, 705–714. [Google Scholar] [CrossRef]
- Pontoriero, R.; Wennström, J.; Lindhe, J. The use of barrier membranes and enamel matrix proteins in the treatment of angular bone defects. A prospective controlled clinical study. J. Clin. Periodontol. 1999, 26, 833–840. [Google Scholar] [PubMed]
- Cortellini, P.; Nieri, M.; Prato, G.P.; Tonetti, M.S. Single minimally invasive surgical technique with an enamel matrix derivative to treat multiple adjacent intra-bony defects: Clinical outcomes and patient morbidity. J. Clin. Periodontol. 2008, 35, 605–613. [Google Scholar] [CrossRef]
- Miron, R.J.; Sculean, A.; Cochran, D.L.; Froum, S.; Zucchelli, G.; Nemcovsky, C.; Donos, N.; Lyngstadaas, S.P.; Deschner, J.; Dard, M.; et al. Twenty years of enamel matrix derivative: The past, the present and the future. J. Clin. Periodontol. 2016, 43, 668–683. [Google Scholar] [CrossRef]
- Kaigler, D.; Avila, G.; Wisner-Lynch, L.; Nevins, M.L.; Nevins, M.; Rasperini, G.; Lynch, S.E.; Giannobile, W.V. Platelet-derived growth factor applications in periodontal and peri-implant bone regeneration. Expert Opin. Biol. Ther. 2011, 11, 375–385. [Google Scholar] [CrossRef]
- Nevins, M.; Giannobile, W.V.; McGuire, M.K.; Kao, R.T.; Mellonig, J.T.; Hinrichs, J.E.; McAllister, B.S.; Murphy, K.S.; McClain, P.K.; Nevins, M.L.; et al. Platelet-derived growth factor stimulates bone fill and rate of attachment level gain: Results of a large multicenter randomized controlled trial. J. Periodontol. 2005, 76, 2205–2215. [Google Scholar] [CrossRef] [PubMed]
- Giannobile, W.V.; Ryan, S.; Shih, M.S.; Su, D.L.; Kaplan, P.L.; Chan, T.C. Recombinant human osteogenic protein-1 (OP-1) stimulates periodontal wound healing in class III furcation defects. J. Periodontol. 1998, 69, 129–137. [Google Scholar] [CrossRef] [PubMed]
- Wikesjö, U.M.; Guglielmoni, P.; Promsudthi, A.; Cho, K.S.; Trombelli, L.; Selvig, K.A.; Jin, L.; Wozney, J.M. Periodontal repair in dogs: Effect of rhBMP-2 concentration on regeneration of alveolar bone and periodontal attachment. J. Clin. Periodontol. 1999, 26, 392–400. [Google Scholar]
- Tarallo, F.; Mancini, L.; Pitzurra, L.; Bizzarro, S.; Tepedino, M.; Marchetti, E. Use of platelet-rich fibrin in the treatment of grade 2 furcation defects: Systematic review and meta-analysis. J. Clin. Med. 2020, 9, 2104. [Google Scholar] [CrossRef] [PubMed]
- Marchetti, E.; Mancini, L.; Bernardi, S.; Bianchi, S.; Cristiano, L.; Torge, D.; Marzo, G.; Macchiarelli, G. Evaluation of different autologous platelet concentrate biomaterials: Morphological and biological comparisons and considerations. Materials 2020, 13, 2282. [Google Scholar] [CrossRef]
- Yukna, R.; Salinas, T.J.; Carr, R.F. Periodontal regeneration following use of ABM/P-1 5: A case report. Int. J. Periodontics Restor. Dent. 2002, 22, 146–155. [Google Scholar]
- Camelo, M.; Nevins, M.L.; Schenk, R.K.; Lynch, S.E.; Nevins, M. Periodontal regeneration in human Class II furcations using purified recombinant human platelet-derived growth factor-BB (rhPDGF-BB) with bone allograft. Int. J. Periodontics Restor. Dent. 2003, 23, 213–225. [Google Scholar]
- Thoma, D.S.; Payer, M.; Jakse, N.; Bienz, S.P.; Hüsler, J.; Schmidlin, P.R.; Jung, U.W.; Hämmerle, C.; Jung, R.E. Randomized, controlled clinical two-centre study using xenogeneic block grafts loaded with recombinant human bone morphogenetic protein-2 or autogenous bone blocks for lateral ridge augmentation. J. Clin. Periodontol. 2018, 45, 265–276. [Google Scholar] [CrossRef] [PubMed]
- Chiu, H.C.; Chiang, C.Y.; Tu, H.P.; Wikesjö, U.M.; Susin, C.; Fu, E. Effects of bone morphogenetic protein-6 on periodontal wound healing/regeneration in supraalveolar periodontal defects in dogs. J. Clin. Periodontol. 2013, 40, 624–630. [Google Scholar] [CrossRef]
- de Santana, R.B.; de Santana, C.M. Human intrabony defect regeneration with rhFGF-2 and hyaluronic acid—A randomized controlled clinical trial. J. Clin. Periodontol. 2015, 42, 658–665. [Google Scholar] [CrossRef]
- Yao, Y.; Kauffmann, F.; Maekawa, S.; Sarment, L.V.; Sugai, J.V.; Schmiedeler, C.A.; Doherty, E.J.; Holdsworth, G.; Kostenuik, P.J.; Giannobile, W.V. Sclerostin antibody stimulates periodontal regeneration in large alveolar bone defects. Sci. Rep. 2020, 10, 16217. [Google Scholar] [CrossRef]
- McGuire, M.K.; Tavelli, L.; Feinberg, S.E.; Rasperini, G.; Zucchelli, G.; Wang, H.L.; Giannobile, W.V. Living cell-based regenerative medicine technologies for periodontal soft tissue augmentation. J. Periodontol. 2020, 91, 155–164. [Google Scholar] [CrossRef] [PubMed]
- Trovato, L.; Naro, F.; D’Aiuto, F.; Moreno, F. Promoting tissue repair by micrograft stem cells delivery. Stem Cells Int. 2020, 2195318. [Google Scholar] [CrossRef] [PubMed]
- Mummolo, S.; Mancini, L.; Quinzi, V.; D’Aquino, R.; Marzo, G.; Marchetti, E. Rigenera® autologous micrografts in oral regeneration: Clinical, histological, and radiographical evaluations. Appl. Sci. 2020, 10, 5084. [Google Scholar] [CrossRef]
- Rasperini, G.; Pilipchuk, S.P.; Flanagan, C.L.; Park, C.H.; Pagni, G.; Hollister, S.J.; Giannobile, W.V. 3D-printed bioresorbable scaffold for periodontal repair. J. Dent. Res. 2015, 94, 153S–157S. [Google Scholar] [CrossRef] [PubMed]
- Zucchelli, G.; Mounssif, I.; Marzadori, M.; Mazzotti, C.; Felice, P.; Stefanini, M. Connective Tissue Graft Wall Technique and Enamel Matrix Derivative for the Treatment of Infrabony Defects: Case Reports. Int. J. Periodontics Restor. Dent. 2017, 37, 673–681. [Google Scholar] [CrossRef] [PubMed]




| Class | Material | Description | Commercial Name |
|---|---|---|---|
| Non Resorbable | Titanium | Mesh with biological hole or completely covered | Regenplate; Ridge—Form Mesh®; Frios® bone shields |
| Non Resorbable | Polytetrafluorethylene (PTFE) | Dense PTFE. Expanded PTFE. Dual textured PTFE. Titanium reinforced PTFE. | Cytoplast® TXT-200 Gore-tex® NeoGen® Gore-Tex® Ti; NeoGen® Ti. Reinforced and Cytoplast Ti-250® |
| Resorbable (animal origin) | Cross Linked | Cross linked type I collagen Cross-linked type I and type III | OsseoGuard® BioMend®; OSSIX®PLUS MatrixDerm™; Osseo Guard Flex®; EZCure™ |
| Resorbable (animal origin) | Non-Cross Linked | Type I collagen Type I and III collagen Collagen with intermingled elastin Type I, III, IV, VI and other proteins | CollaTape®; Tutodent® BioGide®; botiss Jason® Creos xenoprotect DynaMatrix® |
| Growth Factors | Biologic Function | Phase of Investigation | Evidence for Periodontal Regeneration? |
|---|---|---|---|
| P-15 | Improving cells adhesion | FDA approved | Yes [67] |
| RhPDGF-BB | Chemiotaxis of progenitor’s cells and angiogenesis stimulation | FDA approved | Yes [68] |
| BMP-2 | Osteogenic differentiation | FDA approved | Yes [69] |
| BMP-6 | Osteogenesis enhancer | Preclinical | On dog [70] |
| BMP-12 | Active on ligaments and tendons | Preclinical | On dog [64] |
| rhFGF2 | Fibroblast and endothelial proliferation | FDA approved | Yes [71] |
| OP-1 | Increase mitogenesis and differentiation of osteoblast | Preclinical | On dog [63] |
| SOST antibodies | Antiresorption effect on bone | FDA approved | Yes [72] |
| PTH | Anabolic effect on bone | Clinical | N/A |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mancini, L.; Fratini, A.; Marchetti, E. Periodontal Regeneration. Encyclopedia 2021, 1, 87-98. https://doi.org/10.3390/encyclopedia1010011
Mancini L, Fratini A, Marchetti E. Periodontal Regeneration. Encyclopedia. 2021; 1(1):87-98. https://doi.org/10.3390/encyclopedia1010011
Chicago/Turabian StyleMancini, Leonardo, Adriano Fratini, and Enrico Marchetti. 2021. "Periodontal Regeneration" Encyclopedia 1, no. 1: 87-98. https://doi.org/10.3390/encyclopedia1010011
APA StyleMancini, L., Fratini, A., & Marchetti, E. (2021). Periodontal Regeneration. Encyclopedia, 1(1), 87-98. https://doi.org/10.3390/encyclopedia1010011








