The Role of Artificial Intelligence in Pharmacy Practice and Patient Care: Innovations and Implications
Abstract
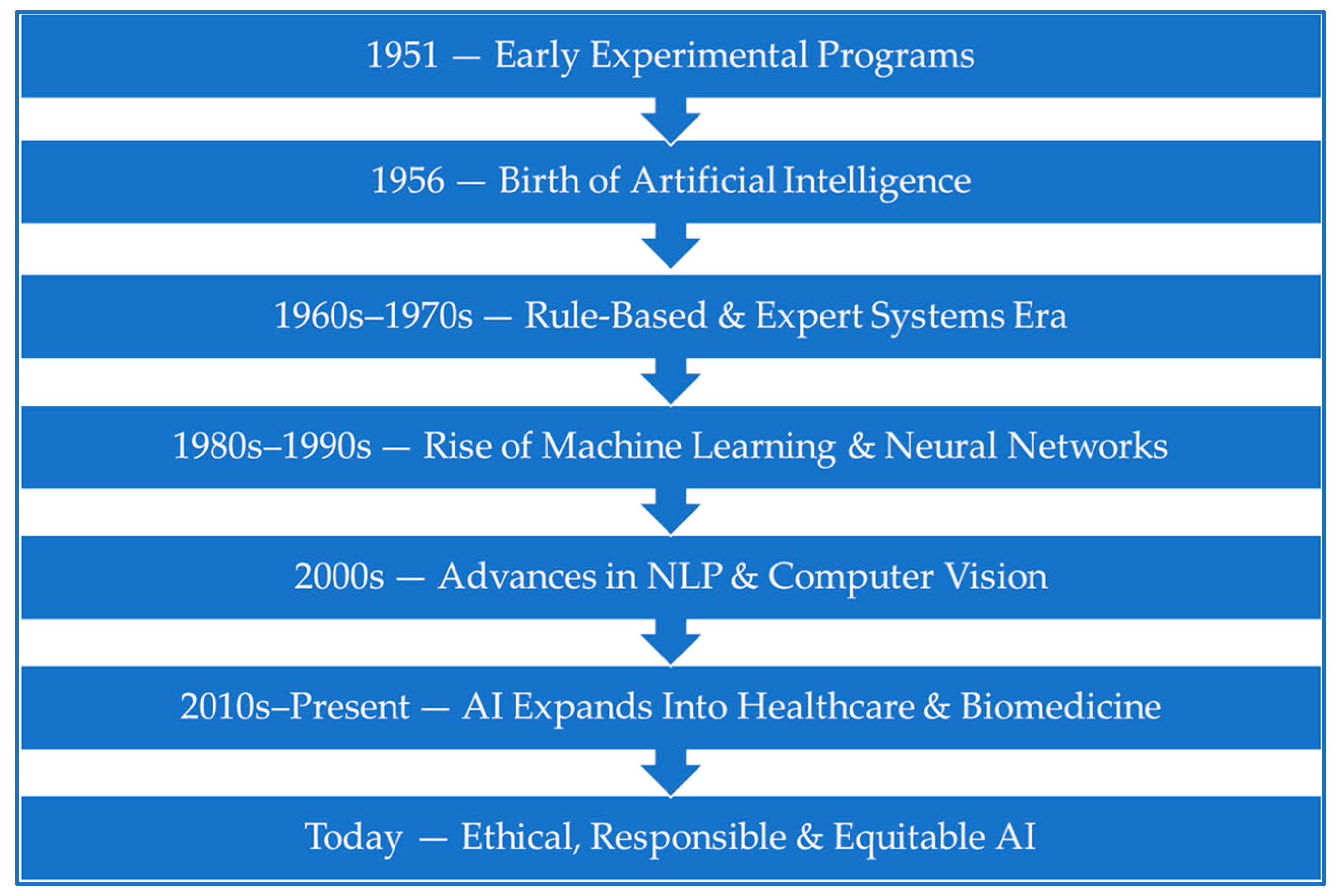
1. Introduction
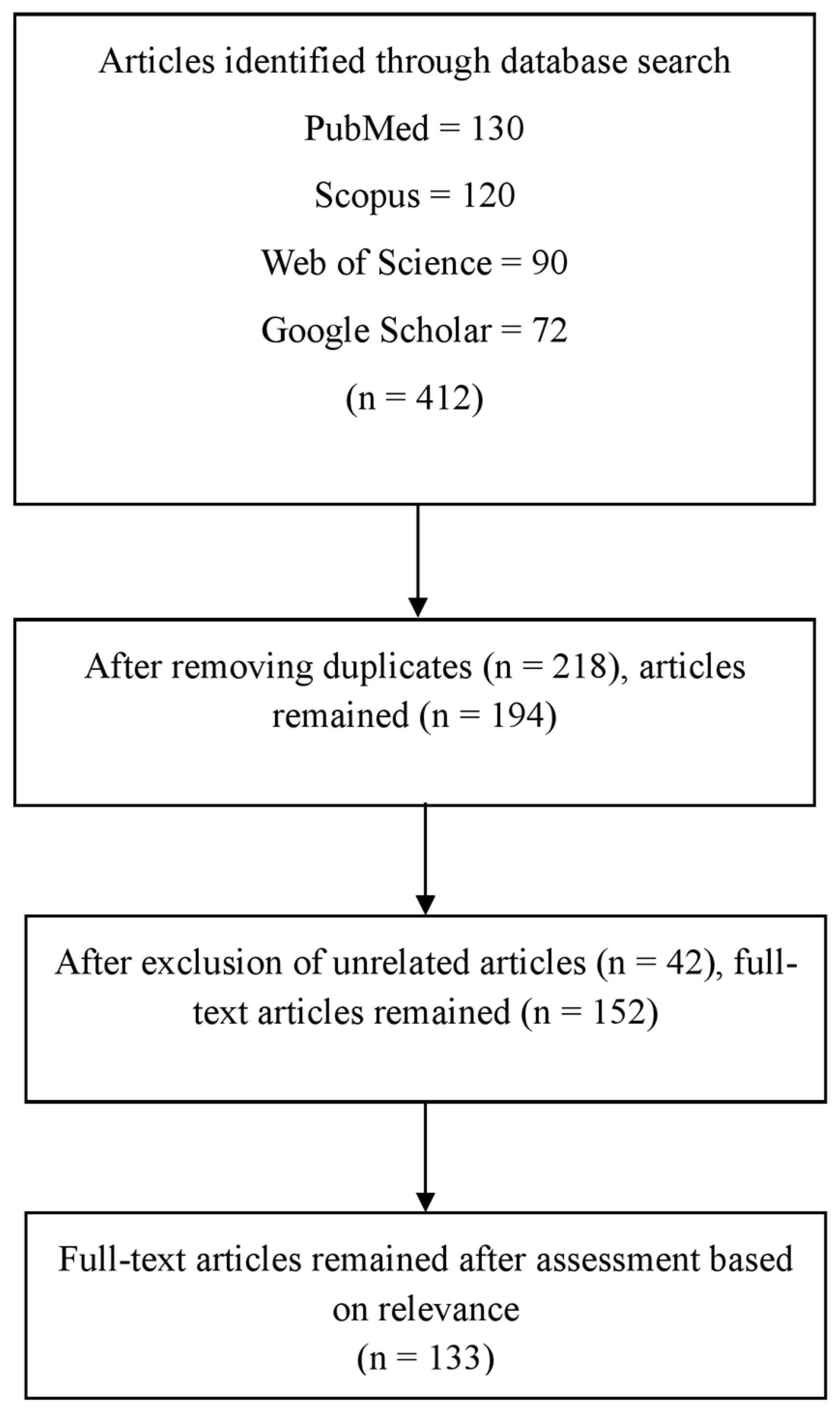
2. Materials and Methods
3. AI in Pharmacy Practice: A Transformative Enabler
4. AI Tools Commonly Used in Pharmacy Practice and Patient Care
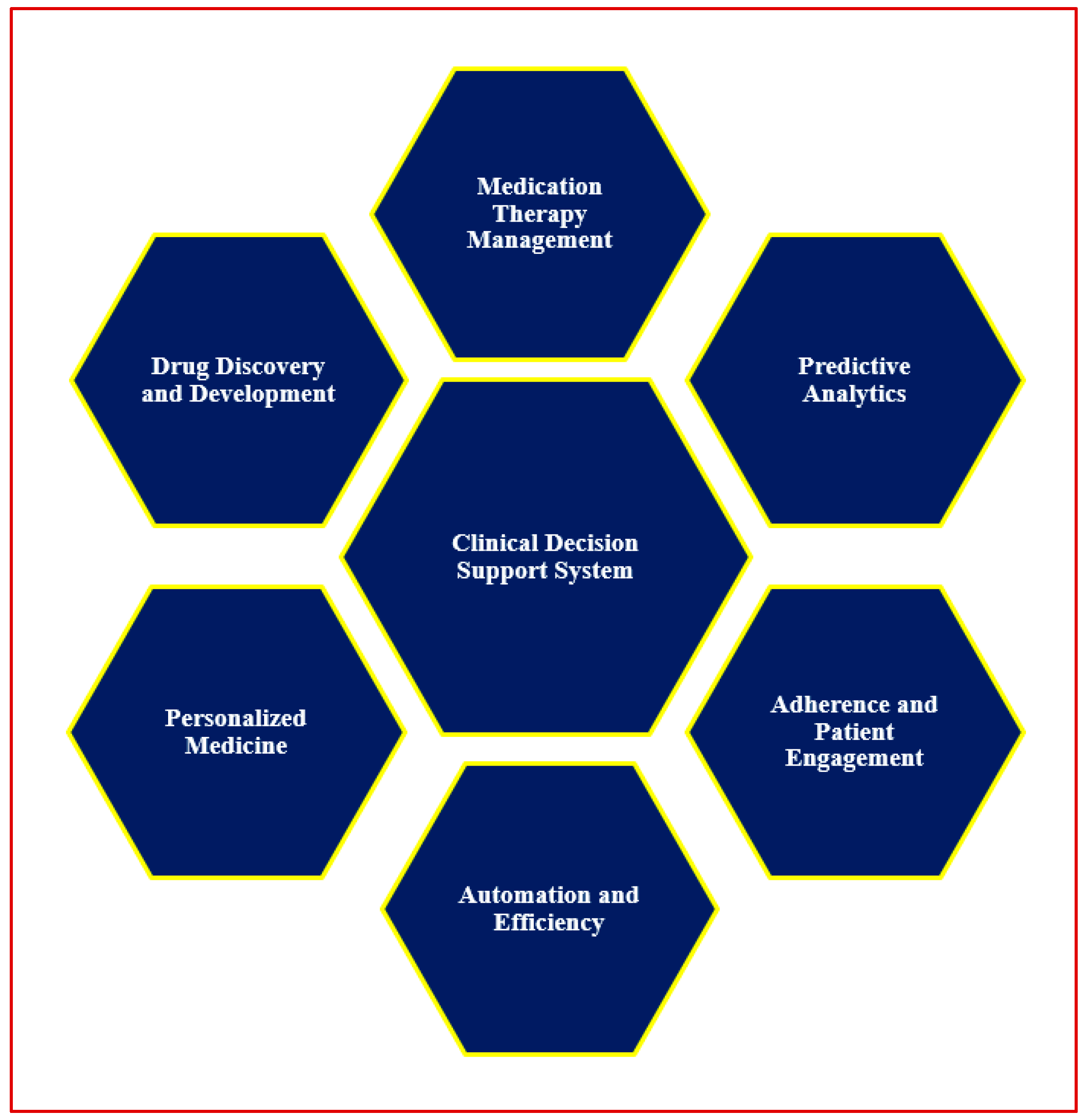
5. AI in Clinical Decision Support Systems
- Medication safety and prescription analysis, including error detection and dose individualization, are supported by CDSS platforms such as MedAware and DoseMeRx.
- Predictive analytics integrated within CDSS can anticipate high-risk scenarios—such as hospital readmissions or ADEs—by identifying subtle patterns in patient data.
- Medication Therapy Management is enhanced when CDSS tools integrate pharmacogenomic and behavioral data to recommend personalized regimens.
- Adherence monitoring and intervention can also be guided by CDSS through integration with wearable data and patient-reported outcomes, improving chronic disease management.
6. Automation and AI in Pharmacy Inventory and Supply Chain Management
7. AI in Pharmacovigilance
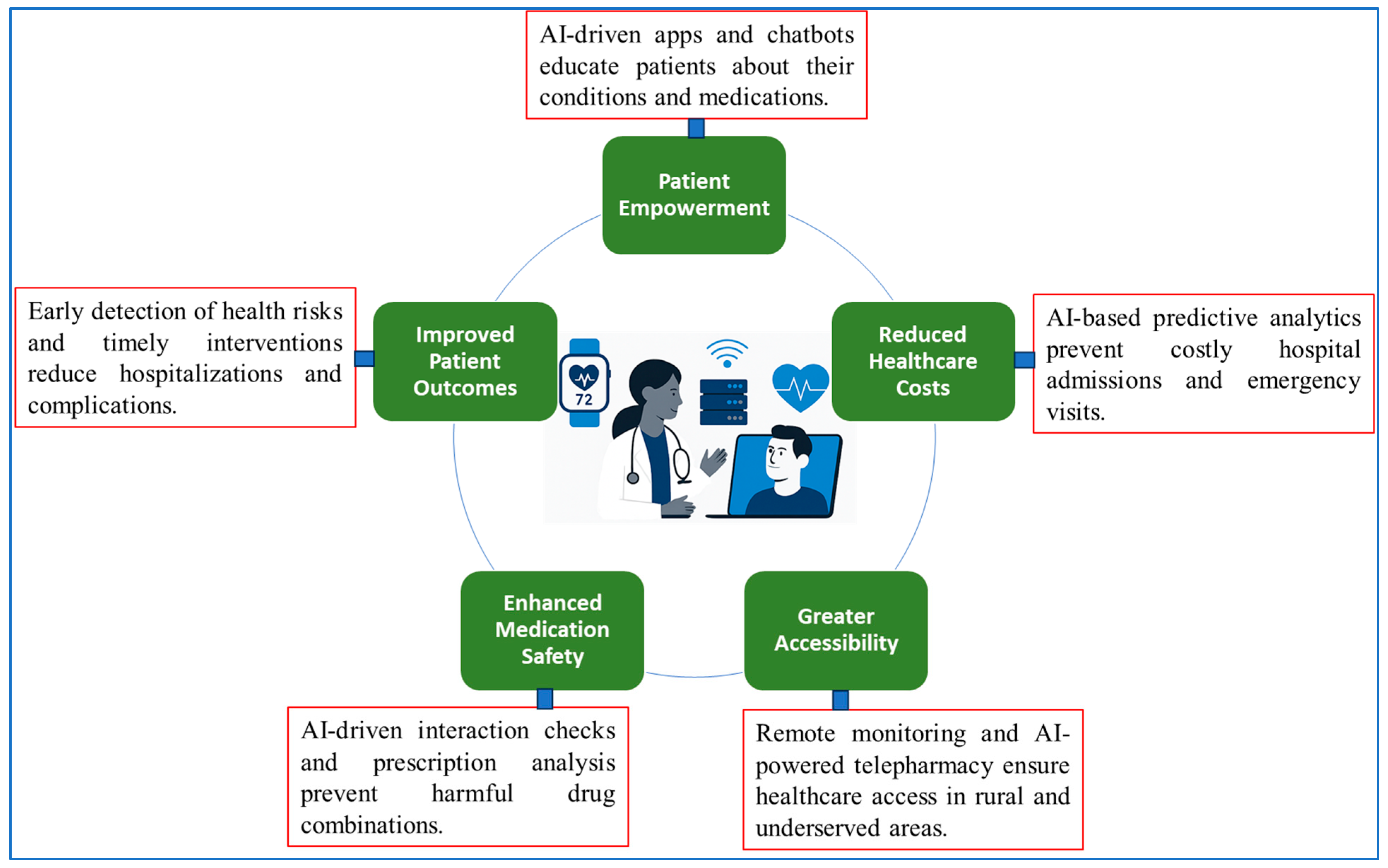
8. AI in Patient Counselling and Education
9. AI in Drug Discovery and Development
10. AI in Personalized Medicine
11. AI and Wearable Technologies in Medication Adherence
12. AI in Remote Patient Monitoring and Telepharmacy
12.1. RPM Applications Enhanced by AI
12.2. Telepharmacy Benefits Powered by AI
- Prescription Verification: AI tools such as NLP analyze digital prescriptions for errors, incorrect dosages, and potential drug interactions [106].
- Medication Adherence Monitoring: Smart devices and chatbots track medication intake and issue personalized reminders [100].
- Patient Counselling: AI-powered assistants provide 24/7 counselling support and automate frequently asked medication queries, complementing the pharmacist’s role [106].
12.3. Intelligent Dose Adjustment and Risk Mitigation
13. AI in Forecasting Disease Progression and Patient Outcomes
13.1. Predictive Models for Chronic Disease Management
13.2. Role in Personalized and Population Health
13.3. Operational and Economic Implications
14. Challenges and Ethical Considerations in the Integration of AI in Healthcare and Pharmacy
14.1. Data Privacy and Security
14.2. Integration into Clinical Workflows
14.3. Regulatory and Legal Ambiguities
14.4. Algorithmic Bias and Health Equity
14.5. Ethical Use and Professional Oversight
15. Discussion
16. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Elhaddad, M.; Hamam, S. AI-driven clinical decision support systems: An ongoing pursuit of potential. Cureus 2024, 16, e57728. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Allam, H. Prescribing the future: The role of artificial intelligence in pharmacy. Information 2025, 16, 131. [Google Scholar] [CrossRef]
- Verma, M. Artificial intelligence role in modern science: Aims, merits, risks and its applications. Artif. Intell. 2023, 7, 335–342. [Google Scholar]
- Kandhare, P.; Kurlekar, M.; Deshpande, T.; Pawar, A. A review on revolutionizing healthcare technologies with AI and ML applications in pharmaceutical sciences. Drugs Drug Candidates 2025, 4, 9. [Google Scholar] [CrossRef]
- Rahman, A.; Debnath, T.; Kundu, D.; Khan, M.S.I.; Aishi, A.A.; Sazzad, S.; Sayduzzaman, M.; Band, S.S. Machine learning and deep learning-based approach in smart healthcare: Recent advances, applications, challenges and opportunities. AIMS Public Health 2024, 11, 58. [Google Scholar] [CrossRef]
- AlJassas, S.M.; Alzaidi, N.A.; Algharqan, S.M.; Aljawad, S.H.; Alsofyani, B.M.; Hadadi, F.A. Evaluating the Impact of Drug-Drug Interactions in Polypharmacy Strategies for Safe Medication Management. JOHS 2024, 4, 1051–1056. [Google Scholar] [CrossRef]
- Molla, G.; Bitew, M. Revolutionizing personalized medicine: Synergy with multi-omics data generation, main hurdles, and future perspectives. Biomedicines 2024, 12, 2750. [Google Scholar] [CrossRef]
- Arshad, H.; Tayyab, M.; Bilal, M.; Akhtar, S.; Abdullahi, A. Trends and Challenges in harnessing big data intelligence for health care transformation. In Artificial Intelligence for Intelligent Systems; CRC Press: Boca Raton, FL, USA, 2024; pp. 220–240. [Google Scholar]
- Vallano, A.; Pontes, C. Escalating costs of innovative medicines: Perspective and proposals. Front. Public Health 2024, 12, 1449707. [Google Scholar] [CrossRef]
- Aminabee, S. The future of healthcare and patient-centric care: Digital innovations, trends, and predictions. In Emerging Technologies for Health Literacy and Medical Practice; IGI Global Scientific Publishing: Hershey, PA, USA, 2024; pp. 240–262. [Google Scholar]
- Alowais, S.A.; Alghamdi, S.S.; Alsuhebany, N.; Alqahtani, T.; Alshaya, A.I.; Almohareb, S.N.; Aldairem, A.; Alrashed, M.; Bin Saleh, K.; Badreldin, H.A.; et al. Revolutionizing healthcare: The role of artificial intelligence in clinical practice. BMC Med. Educ. 2023, 23, 689. [Google Scholar] [CrossRef]
- Meknassi Salime, G.; Bhirich, N.; Cherif Chefchaouni, A.; El Hamdaoui, O.; El Baraka, S.; Elalaoui, Y. Assessment of Automation Models in Hospital Pharmacy: Systematic Review of Technologies, Practices, and Clinical Impacts. Hosp. Pharm. 2025, 60, 00185787251315622. [Google Scholar] [CrossRef]
- Tantray, J.; Patel, A.; Wani, S.N.; Kosey, S.; Prajapati, B.G. Prescription Precision: A Comprehensive Review of Intelligent Prescription Systems. Curr. Pharm. Des. 2024, 30, 2671–2684. [Google Scholar] [CrossRef]
- Singh, K.; Nashwan, A.J. Artificial Intelligence-driven solutions: Revolutionizing patient care in multimorbidity management. Discov. Health Syst. 2025, 4, 65. [Google Scholar] [CrossRef]
- Chalasani, S.H.; Syed, J.; Ramesh, M.; Patil, V.; Kumar, T.P. Artificial intelligence in the field of pharmacy practice: A literature review. Explor. Res. Clin. Soc. Pharm. 2023, 12, 100346. [Google Scholar] [CrossRef]
- Ogbuagu, O.O.; Mbata, A.O.; Balogun, O.D.; Oladapo, O.; Ojo, O.O.; Muonde, M. Artificial intelligence in clinical pharmacy: Enhancing drug safety, adherence, and patient-centered care. Int. J. Multidiscip. Res. Growth Eval. 2023, 4, 814–822. [Google Scholar] [CrossRef]
- Rammal, D.S.; Alomar, M.; Palaian, S. AI-Driven pharmacy practice: Unleashing the revolutionary potential in medication management, pharmacy workflow, and patient care. Pharm. Pract. 2024, 22, 1–11. [Google Scholar] [CrossRef]
- Rui, A.; Garabedian, P.M.; Marceau, M.; Syrowatka, A.; Volk, L.A.; Edrees, H.H.; Seger, D.L.; Amato, M.G.; Cambre, J.; Dulgarian, S.; et al. Performance of a web-based reference database with natural language searching capabilities: Usability evaluation of DynaMed and Micromedex with Watson. JMIR Hum. Factors 2023, 10, e43960. [Google Scholar] [CrossRef]
- Wolters Kluwer Launches AI-Enhanced UpToDate Enterprise Edition in EMEA. Available online: https://www.wolterskluwer.com/en/news/wolters-kluwer-launches-ai-enhanced-uptodate-enterprise-edition-in-emea (accessed on 4 February 2025).
- Aksoyalp, Z.Ş.; Erdoğan, B.R. Comparative evaluation of Artificial intelligence and drug interaction tools: A perspective with the example of clopidogrel. J. Fac. Pharm. Ank. Univ. 2024, 48, 1011–1020. [Google Scholar] [CrossRef]
- Thapa, R.B.; Karki, S.; Shrestha, S. Exploring potential drug-drug interactions in discharge prescriptions: ChatGPT’s effectiveness in assessing those interactions. Explor. Res. Clin. Soc. Pharm. 2025, 17, 100564. [Google Scholar] [CrossRef]
- Sheikh, M.S.; Barreto, E.F.; Miao, J.; Thongprayoon, C.; Gregoire, J.R.; Dreesman, B.; Erickson, S.B.; Craici, I.M.; Cheungpasitporn, W. Evaluating ChatGPT’s efficacy in assessing the safety of non-prescription medications and supplements in patients with kidney disease. Digit. Health 2024, 10, 20552076241248082. [Google Scholar] [CrossRef] [PubMed]
- Maphosa, V.; Mpofu, B. An Artificial Intelligence-Based Random Forest Model for Reducing Prescription Errors and Improving Patient Safety. 2024. Available online: https://ssrn.com/abstract=4842105 (accessed on 11 August 2025).
- Pillay, T.S. Increasing the Impact and Value of Laboratory Medicine Through Effective and AI-Assisted Communication. EJIFCC 2025, 36, 12–25. [Google Scholar]
- Bennani, T. Advancing Healthcare with GenerativeAI: A Multifaceted Approach to Reliable Medical Information and Innovation. Master’s Thesis, Massachusetts Institute of Technology, Cambridge, MA, USA, 2024. [Google Scholar]
- George, A.S.; George, A.H. The rise of robotic children: Implications for family, caregiving, and society. Partn. Univers. Innov. Res. Publ. 2023, 1, 82–101. [Google Scholar]
- Singh, P. Transforming Healthcare Through AI: Enhancing Patient Outcomes and Bridging Accessibility Gaps. 2024. Available online: https://ssrn.com/abstract=5115767 (accessed on 11 August 2025).
- Kumar, K.A.; Rajan, J.F.; Appala, C.; Balurgi, S.; Balaiahgari, P.R. Medibot: Personal medical assistant. In Proceedings of the 2024 2nd International Conference on Networking and Communications (ICNWC), Chennai, India, 2–4 April 2024. [Google Scholar]
- Abbas, M.; Rassam, A.; Karamshahi, F.; Abunora, R.; Abouseada, M. The role of AI in drug discovery. Chembiochem 2024, 25, e202300816. [Google Scholar] [CrossRef]
- Quazi, F.; Mohammed, A.S.; Gorrepati, N. Transforming Treatment and Diagnosis in Healthcare through AI. Int. J. Glob. Innov. Solut. (IJGIS) 2024, 1–15. [Google Scholar] [CrossRef]
- Saini, J.P.S.; Thakur, A.; Yadav, D. AI driven Innovations in Pharmaceuticals: Optimizing Drug Discovery and Industry Operations. RSC Pharm. 2025, 2, 437–454. [Google Scholar] [CrossRef]
- Niazi, S.K. The coming of age of AI/ML in drug discovery, development, clinical testing, and manufacturing: The FDA perspectives. Drug Des. Dev. Ther. 2023, 17, 2691–2725. [Google Scholar] [CrossRef] [PubMed]
- Le, N.N.; Frater, I.; Lip, S.; Padmanabhan, S. Hypertension precision medicine: The promise and pitfalls of pharmacogenomics. Pharmacogenomics 2025, 26, 183–206. [Google Scholar] [CrossRef]
- Patel, J.N.; Morris, S.A.; Torres, R.; Rhead, B.; Vlangos, C.; Mueller, D.J.; Brown, L.C.; Lefkofsky, H.; Ali, M.; De La Vega, F.M.; et al. Pharmacogenomic insights in psychiatric care: Uncovering novel actionability, allele-specific CYP2D6 copy number variation, and phenoconversion in 15,000 patients. Mol. Psychiatry 2024, 29, 3495–3502. [Google Scholar] [CrossRef] [PubMed]
- Li, C. A Review of Identity and Roles of Robotics in the Healthcare Industry. J. Biomed. Sustain. Healthc. Appl. 2024, 4, 22–32. [Google Scholar] [CrossRef]
- Suryavanshi, R.; Yadav, A.; Yadav, A.; Dusankar, Y.; Nalawade, Y.; Yawale, S. AI-Integrated QR Drug Dispenser for Efficient Medication Management. TechRxiv 2024. [Google Scholar] [CrossRef]
- Sutton, R.T.; Chappell, K.D.; Pincock, D.; Sadowski, D.; Baumgart, D.C.; Kroeker, K.I. The Effect of an Electronic Medical Record–Based Clinical Decision Support System on Adherence to Clinical Protocols in Inflammatory Bowel Disease Care: Interrupted Time Series Study. JMIR Med. Inform. 2024, 12, e55314. [Google Scholar] [CrossRef]
- Panicker, R.O.; George, A.E. Adoption of automated clinical decision support system: A recent literature review and a case study. Arch. Med. Health Sci. 2023, 11, 86–95. [Google Scholar] [CrossRef]
- Penchala, R.; Parimala, V.K. Perspective Chapter: Securing the Future of Digital Healthcare with EHR Systems for Modern Cyber Threats. In Electronic Health Records-Issues and Challenges in Healthcare Systems; IntechOpen: London, UK, 2025. [Google Scholar]
- Mohammed, A.S.; Neravetla, A.R.; Nomula, V.K.; Gupta, K.; Dhanasekaran, S. Understanding the impact of AI-driven clinical decision support systems. In Proceedings of the 2024 15th International Conference on Computing Communication and Networking Technologies (ICCCNT), Kamand, India, 24–28 June 2024. [Google Scholar]
- Zitu, M.M.; Owen, D.; Manne, A.; Wei, P.; Li, L. Large language models for adverse drug events: A clinical perspective. J. Clin. Med. 2025, 14, 5490. [Google Scholar] [CrossRef]
- Gosavi, V.R.; Chavan, M.; Joshi, S.M.; Karale, A.V.; Pati, B.K.; Rathore, Y.K. Developing AI-Based Clinical Decision Support Systems for Drug Suggestions: Enhancing Patient Outcomes. Res. J. Pharm. Technol. 2025, 18, 1854–1860. [Google Scholar] [CrossRef]
- Almadani, B.; Kaisar, H.; Thoker, I.R.; Aliyu, F. A systematic survey of distributed decision support systems in healthcare. Systems 2025, 13, 157. [Google Scholar] [CrossRef]
- Kumar, K.S.; Sapanel, Y.; Poon, M.; Sundar, R. Personalized dose selection for the first Waldenström macroglobulinemia patient on the PRECISE CURATE. AI trial. Npj Digit. Med. 2024, 7, 223. [Google Scholar]
- Crooks, K.; Haddud, A. Using Radio Frequency Identification (RFID) Technology in the Pharmaceutical Supply Chain: The Impact on Competitive Advantage. Sustainability 2025, 17, 1378. [Google Scholar] [CrossRef]
- Nweje, U.; Taiwo, M. Leveraging Artificial Intelligence for predictive supply chain management, focus on how AI- driven tools are revolutionizing demand forecasting and inventory optimization. Int. J. Sci. Res. Arch. 2025, 14, 230–250. [Google Scholar] [CrossRef]
- Adeniran, I.A.; Efunniyi, P.C.; Osundare, O.S.; Abhulimen, A.O. Optimizing logistics and supply chain management through advanced analytics: Insights from industries. Eng. Sci. Technol. J. 2024, 5, 52–61. [Google Scholar]
- Dixon, D.; Sattar, H.; Moros, N.; Kesireddy, S.R.; Ahsan, H.; Lakkimsetti, M.; Fatima, M.; Doshi, D.; Sadhu, K.; Junaid Hassan, M. Unveiling the Influence of AI Predictive Analytics on Patient Outcomes: A Comprehensive Narrative Review. Cureus 2024, 16, e59954. [Google Scholar] [CrossRef]
- Akram, W.; Joshi, R.; Haider, T.; Sharma, P.; Jain, V.; Garud, N.; Singh, N. Blockchain technology: A potential tool for the management of pharma supply chain. Res. Soc. Adm. Pharm. 2024, 20, 156–164. [Google Scholar] [CrossRef]
- Sodiya, E.O.; Umoga, U.J.; Amoo, O.O.; Atadoga, A. AI-driven warehouse automation: A comprehensive review of systems. GSC Adv. Res. Rev. 2024, 18, 272–282. [Google Scholar] [CrossRef]
- Sharma, S.; Sharma, H. Drone a technological leap in health care delivery in distant and remote inaccessible areas: A narrative review. Saudi J. Anaesth. 2024, 18, 95–99. [Google Scholar] [CrossRef]
- Phougat, P.; Beniwal, M.; Kapoor, G.; Aggarwal, N.; Kumari, A.; Sharma, R.; Chopra, H.; Sharma, R.; Kamal, M.A. Role and Responsibilities of Various Stakeholders in Pharmacovigilance. Curr. Drug Saf. 2025, 20, 19–32. [Google Scholar] [CrossRef]
- Algarvio, R.C.; Conceição, J.; Rodrigues, P.P.; Ribeiro, I.; Ferreira-da-Silva, R. Artificial intelligence in pharmacovigilance: A narrative review and practical experience with an expert-defined Bayesian network tool. Int. J. Clin. Pharm. 2025, 47, 932–944. [Google Scholar] [CrossRef]
- Nagar, A.; Gobburu, J.; Chakravarty, A. Artificial intelligence in pharmacovigilance: Advancing drug safety monitoring and regulatory integration. Ther. Adv. Drug Saf. 2025, 16, 20420986251361435. [Google Scholar] [CrossRef]
- Alsaedi, S.; Ogasawara, M.; Alarawi, M.; Gao, X.; Gojobori, T. AI-powered precision medicine: Utilizing genetic risk factor optimization to revolutionize healthcare. NAR Genom. Bioinform. 2025, 7, lqaf038. [Google Scholar] [CrossRef] [PubMed]
- De Micco, F.; Di Palma, G.; Ferorelli, D.; De Benedictis, A.; Tomassini, L.; Tambone, V.; Cingolani, M.; Scendoni, R. Artificial intelligence in healthcare: Transforming patient safety with intelligent systems-A systematic review. Front. Med. 2024, 11, 1522554. [Google Scholar] [CrossRef]
- Correia, J.C.; Waqas, A.; Assal, J.P.; Davies, M.J.; Somers, F.; Golay, A.; Pataky, Z. Effectiveness of therapeutic patient education interventions for chronic diseases: A systematic review and meta-analyses of randomized controlled trials. Front. Med. 2022, 9, 996528. [Google Scholar] [CrossRef] [PubMed]
- Clark, M.; Bailey, S. Chatbots in Health Care: Connecting Patients to Information: Emerging Health Technologies; Canadian Agency for Drugs and Technologies in Health: Ottawa, ON, Canada, 2024. [Google Scholar]
- Thakkar, A.; Gupta, A.; De Sousa, A. Artificial intelligence in positive mental health: A narrative review. Front. Digit. Health 2024, 6, 1280235. [Google Scholar] [CrossRef] [PubMed]
- Khalifa, M.; Albadawy, M. Artificial intelligence for diabetes: Enhancing prevention, diagnosis, and effective management. Comput. Methods Programs Biomed. Update 2024, 5, 100141. [Google Scholar] [CrossRef]
- Maleki Varnosfaderani, S.; Forouzanfar, M. The Role of AI in Hospitals and Clinics: Transforming Healthcare in the 21st Century. Bioengineering 2024, 11, 337. [Google Scholar] [CrossRef]
- Zhang, H.; Wang, X.; Luo, H.; Zeng, W.; Hong, X.; Feng, J.; Lu, G.; Su, Y.; Tong, W.; Xiao, Y. Comparison of preoperative education by artificial intelligence versus traditional physicians in perioperative management of urolithiasis surgery: A prospective single-blind randomized controlled trial conducted in China. Front. Med. 2025, 12, 1543630. [Google Scholar] [CrossRef]
- Kukade, A.; Kawade, S.; Lokare, S.; Kharage, A. Artificial Intelligence in Medication Adherence and Personalized Treatment Plans. Int. J. Sci. Res. Technol. 2025, 2, IJSRT/250304208. [Google Scholar]
- Olawade, D.B.; Wada, O.Z.; Odetayo, A.; David-Olawade, A.C.; Asaolu, F.; Eberhardt, J. Enhancing Mental Health with Artificial Intelligence: Current Trends and Future Prospects. J. Med. Surg. Public Health 2024, 3, 100099. [Google Scholar] [CrossRef]
- Haque, M.D.R.; Rubya, S. An Overview of Chatbot-Based Mobile Mental Health Apps: Insights From App Description and User Reviews. JMIR Mhealth Uhealth 2023, 11, e44838. [Google Scholar] [CrossRef] [PubMed]
- van der Schyff, E.L.; Ridout, B.; Amon, K.L.; Forsyth, R.; Campbell, A.J. Providing Self-Led Mental Health Support Through an Artificial Intelligence-Powered Chat Bot (Leora) to Meet the Demand of Mental Health Care. J. Med. Internet Res. 2023, 25, e46448. [Google Scholar] [CrossRef]
- Sertkaya, A.; Beleche, T.; Jessup, A.; Sommers, B.D. Costs of Drug Development and Research and Development Intensity in the US, 2000–2018. JAMA Netw. Open 2024, 7, e2415445. [Google Scholar] [CrossRef]
- Serrano, D.R.; Luciano, F.C.; Anaya, B.J.; Ongoren, B.; Kara, A.; Molina, G.; Ramirez, B.I.; Sánchez-Guirales, S.A.; Simon, J.A.; Tomietto, G.; et al. Artificial Intelligence (AI) Applications in Drug Discovery and Drug Delivery: Revolutionizing Personalized Medicine. Pharmaceutics 2024, 16, 1328. [Google Scholar] [CrossRef]
- Blanco-González, A.; Cabezón, A.; Seco-González, A.; Conde-Torres, D.; Antelo-Riveiro, P.; Piñeiro, Á.; Garcia-Fandino, R. The Role of AI in Drug Discovery: Challenges, Opportunities, and Strategies. Pharmaceuticals 2023, 16, 891. [Google Scholar] [CrossRef]
- Alghamdi, M.A. From Molecules to Medicines: The Role of AI-Driven Drug Discovery Against Alzheimer’s Disease and Other Neurological Disorders. Pharmaceuticals 2025, 18, 1041. [Google Scholar] [CrossRef]
- Han, R.; Yoon, H.; Kim, G.; Lee, H.; Lee, Y. Revolutionizing Medicinal Chemistry: The Application of Artificial Intelligence (AI) in Early Drug Discovery. Pharmaceuticals 2023, 16, 1259. [Google Scholar] [CrossRef]
- Bhat, A.R.; Ahmed, S. Artificial Intelligence (AI) in drug design and discovery: A comprehensive review. Silico Res. Biomed. 2025, 1, 10049. [Google Scholar] [CrossRef]
- Ocana, A.; Pandiella, A.; Privat, C.; Bravo, I.; Luengo-Oroz, M.; Amir, E.; Gyorffy, B. Integrating artificial intelligence in drug discovery and early drug development: A transformative approach. Biomark. Res. 2025, 13, 45. [Google Scholar] [CrossRef]
- Fu, C.; Chen, Q. The future of pharmaceuticals: Artificial intelligence in drug discovery and development. J. Pharm. Anal. 2025, 15, 101248. [Google Scholar] [CrossRef] [PubMed]
- Askin, S.; Burkhalter, D.; Calado, G.; El Dakrouni, S. Artificial Intelligence Applied to clinical trials: Opportunities and challenges. Health Technol. 2023, 13, 203–213. [Google Scholar] [CrossRef]
- Ismail, A.; Al-Zoubi, T.; El Naqa, I.; Saeed, H. The role of artificial intelligence in hastening time to recruitment in clinical trials. BJR Open 2023, 5, 20220023. [Google Scholar] [CrossRef]
- Singh, R.; Paxton, M.; Auclair, J. Regulating the AI-enabled ecosystem for human therapeutics. Commun. Med. 2025, 5, 181. [Google Scholar] [CrossRef] [PubMed]
- Visan, A.I.; Negut, I. Integrating Artificial Intelligence for Drug Discovery in the Context of Revolutionizing Drug Delivery. Life 2024, 14, 233. [Google Scholar] [CrossRef]
- Singh, A. Artificial intelligence for drug repurposing against infectious diseases. Artif. Intell. Chem. 2024, 2, 10071. [Google Scholar] [CrossRef]
- Insilico Medicine’s AI-Driven Drug Rentosertib Receives Official Generic Name; InSilico Medicine: Cambridge, MA, USA, 2025; Available online: https://www.news-medical.net/news/20250307/Insilico-Medicines-AI-driven-drug-Rentosertib-receives-official-generic-name.aspx (accessed on 11 August 2025).
- Gite, S.; Zanak, U.; Bharate, S.; Rathod, P.; Mawal, V.; Dalve, P.; Nagrik, S. Artificial intelligence in predictive modeling of drug-drug interactions: Advances, applications, and future directions. Int. J. Sci. Res. Technol. 2025, 2, 172–201. [Google Scholar] [CrossRef]
- Srivastava, N.; Verma, S.; Singh, A.; Shukla, P.; Singh, Y.; Oza, A.D.; Kaur, T.; Chowdhury, S.; Kapoor, M.; Yadav, A.N. Advances in artificial intelligence-based technologies for increasing the quality of medical products. Daru 2024, 33, 1. [Google Scholar] [CrossRef]
- Jaiswal, R. The Role of Artificial Intelligence in Advancing Pharmacovigilance Systems in Pharmafocus Asia. 2025. Available online: https://www.pharmafocusasia.com/articles/the-role-of-artificial-intelligence-in-advancing-pharmacovigilance-systems (accessed on 11 August 2025).
- Parekh, A.E.; Shaikh, O.A.; Simran; Manan, S.; Hasibuzzaman, M.A. Artificial intelligence (AI) in personalized medicine: AI-generated personalized therapy regimens based on genetic and medical history: Short communication. Ann. Med. Surg. 2023, 85, 5831–5833. [Google Scholar] [CrossRef]
- Parvin, N.; Joo, S.W.; Jung, J.H.; Mandal, T.K. Multimodal AI in Biomedicine: Pioneering the Future of Biomaterials, Diagnostics, and Personalized Healthcare. Nanomaterials 2025, 15, 895. [Google Scholar] [CrossRef]
- Satheeskumar, R. AI-driven diagnostics and personalized treatment planning in oral oncology: Innovations and future directions. Oral. Oncol. Rep. 2025, 13, 100704. [Google Scholar] [CrossRef]
- Vilhekar, R.S.; Rawekar, A. Artificial Intelligence in Genetics. Cureus 2024, 16, e52035. [Google Scholar] [CrossRef] [PubMed]
- Soldà, G.; Asselta, R. Applying artificial intelligence to uncover the genetic landscape of coagulation factors. J. Thromb. Haemost. 2025, 23, 1133–1145. [Google Scholar] [CrossRef]
- Taherdoost, H.; Ghofrani, A. AI’s role in revolutionizing personalized medicine by reshaping pharmacogenomics and drug therapy. Intell. Pharm. 2024, 2, 643–650. [Google Scholar] [CrossRef]
- Moges, T.A.; Dagnew, S.B.; Wondm, S.A.; Ferede, Y.A.; Yiblet, T.G.; Almaw, A.; Shumet Yimer, Y.; Tesfaw Addis, G.; Zewdu, W.S.; Dagnew, F.N. Determinants of medication non-adherence among patients with chronic diseases at community pharmacy settings in South Gondar Zone, Northwest Ethiopia: A multicenter cross-sectional study. Front. Public Health 2024, 12, 1409153. [Google Scholar] [CrossRef] [PubMed]
- Religioni, U.; Barrios-Rodríguez, R.; Requena, P.; Borowska, M.; Ostrowski, J. Enhancing therapy adherence: Impact on clinical outcomes, healthcare costs, and patient quality of life. Medicina 2025, 61, 153. [Google Scholar] [CrossRef]
- Chantzaras, A.; Yfantopoulos, J. Determinants of medication adherence in patients with diabetes, hypertension, and hyperlipidemia. Hormones 2025, 24, 443–459. [Google Scholar] [CrossRef] [PubMed]
- Mahajan, A.; Heydari, K.; Powell, D. Wearable AI to enhance patient safety and clinical decision-making. Npj Digit. Med. 2025, 8, 176. [Google Scholar] [CrossRef]
- Huang, G.; Chen, X.; Liao, C. AI-Driven Wearable Bioelectronics in Digital Healthcare. Biosensors 2025, 15, 410. [Google Scholar] [CrossRef] [PubMed]
- Iino, H.; Kizaki, H.; Imai, S.; Hori, S. Medication management initiatives using wearable devices: Scoping review. JMIR Hum. Factors 2024, 11, e57652. [Google Scholar] [CrossRef]
- Birla, M.; Rajan, R.; Roy, P.G.; Gupta, I.; Malik, P.S. Integrating artificial intelligence-driven wearable technology in oncology decision-making: A narrative review. Oncology 2025, 103, 69–81. [Google Scholar] [CrossRef]
- Gaoudam, N.; Sakhamudi, S.K.; Kamal, B.; Addla, N.; Reddy, E.P.; Ambala, M.; Lavanya, K.; Palaparthi, E.C.; Bhattam, A.; Periasamy, P.; et al. Wearable Devices and AI-Driven Remote Monitoring in Cardiovascular Medicine: A Narrative Review. Cureus 2025, 17, e90208. [Google Scholar] [CrossRef]
- Ghadi, Y.Y.; Shah, S.F.A.; Waheed, W.; Mazhar, T.; Ahmad, W.; Saeed, M.M.; Hamam, H. Integration of wearable technology and artificial intelligence in digital health for remote patient care. J. Cloud Comput. 2025, 14, 39. [Google Scholar] [CrossRef]
- Chaturvedi, U.; Chauhan, S.B.; Singh, I. The impact of artificial intelligence on remote healthcare: Enhancing patient engagement, connectivity, and overcoming challenges. Intell. Pharm. 2025, 3, 323–329. [Google Scholar] [CrossRef]
- Reis, Z.S.N.; Pereira, G.M.V.; Dias, C.d.S.; Lage, E.M.; de Oliveira, I.J.R.; Pagano, A.S. Artificial intelligence-based tools for patient support to enhance medication adherence: A focused review. Front. Digit. Health 2025, 7, 1523070. [Google Scholar] [CrossRef] [PubMed]
- Hoshino, J.; Hyry, J.; Kobayashi, T.; Anzai, D. Development of a Wearable System for the Detection of Ingestible Medication Based on Electromagnetic Waves. Electronics 2024, 13, 543. [Google Scholar] [CrossRef]
- Almeman, A. The digital transformation in pharmacy: Embracing online platforms and the cosmeceutical paradigm shift. J. Health Popul. Nutr. 2024, 43, 60. [Google Scholar] [CrossRef]
- Shajari, S.; Kuruvinashetti, K.; Komeili, A.; Sundararaj, U. The emergence of AI-based wearable sensors for digital health technology: A review. Sensors 2023, 23, 9498. [Google Scholar] [CrossRef]
- Snyder, L.D.; DePietro, M.; Reich, M.; Neely, M.L.; Lugogo, N.; Pleasants, R.; Li, T.; Granovsky, L.; Brown, R.; Safioti, G. Predictive machine learning algorithm for COPD exacerbations using a digital inhaler with integrated sensors. BMJ Open Respir. Res. 2025, 12, e002577. [Google Scholar] [CrossRef]
- Medanki, S.; Dommati, N.; Bodapati, H.H.; Katru, V.N.S.K.; Moses, G.; Komaraju, A.; Donepudi, N.S.; Yalamanchili, D.; Sateesh, J.; Turimerla, P. Artificial intelligence powered glucose monitoring and controlling system: Pumping module. World J. Exp. Med. 2024, 14, 87916. [Google Scholar] [CrossRef] [PubMed]
- Sarasmita, M.A.; Sudarma, I.W.; Jaya, M.K.A.; Irham, L.M.; Susanty, S. Telepharmacy implementation to support pharmaceutical care services during the COVID-19 pandemic: A scoping review. Can. J. Hosp. Pharm. 2024, 77, e3430. [Google Scholar] [CrossRef] [PubMed]
- Ko, H.Y.K.; Tripathi, N.K.; Mozumder, C.; Muengtaweepongsa, S.; Pal, I. Real-Time Remote Patient Monitoring and Alarming System for Noncommunicable Lifestyle Diseases. Int. J. Telemed. Appl. 2023, 2023, 9965226. [Google Scholar] [CrossRef]
- Liu, Y.; Wang, B. Advanced applications in chronic disease monitoring using IoT mobile sensing device data, machine learning algorithms and frame theory: A systematic review. Front. Public Health 2025, 13, 1510456. [Google Scholar] [CrossRef] [PubMed]
- Coman, L.-I.; Ianculescu, M.; Paraschiv, E.-A.; Alexandru, A.; Bădărău, I.-A. Smart solutions for diet-related disease management: Connected care, remote health monitoring systems, and integrated insights for advanced evaluation. Appl. Sci. 2024, 14, 2351. [Google Scholar] [CrossRef]
- Mayya, V.; Kandala, R.N.; Gurupur, V.; King, C.; Vu, G.T.; Wan, T.T. Need for an artificial intelligence-based diabetes care management system in India and the United States. Health Serv. Res. Manag. Epidemiol. 2024, 11, 23333928241275292. [Google Scholar] [CrossRef]
- Faisal, S.; Ivo, J.; Abu Fadaleh, S.; Patel, T. Exploring the value of real-time medication adherence monitoring: A qualitative study. Pharmacy 2023, 11, 18. [Google Scholar] [CrossRef]
- Soeno, S.; Liu, K.; Watanabe, S.; Sonoo, T.; Goto, T. Development of novel optical character recognition system to reduce recording time for vital signs and prescriptions: A simulation-based study. PLoS ONE 2024, 19, e0296319. [Google Scholar] [CrossRef]
- Pais, C.; Liu, J.; Voigt, R.; Gupta, V.; Wade, E.; Bayati, M. Large language models for preventing medication direction errors in online pharmacies. Nat. Med. 2024, 30, 1574–1582. [Google Scholar] [CrossRef] [PubMed]
- Dsouza, V.S.; Leyens, L.; Kurian, J.R.; Brand, A.; Brand, H. Artificial Intelligence in Pharmacovigilance: A Systematic Review on Predicting Adverse Drug Reactions in Hospitalized Patients. Res. Soc. Adm. Pharm. 2025, 21, 453–462. [Google Scholar] [CrossRef]
- Awala, E.V.; Olutimehin, D. Revolutionizing remote patient care: The role of machine learning and AI in Enhancing Tele-pharmacy Services. World J. Adv. Res. Rev. 2024, 24, 1133–1149. [Google Scholar] [CrossRef]
- Khalifa, M.; Albadawy, M. Artificial intelligence for clinical prediction: Exploring key domains and essential functions. Comput. Methods Programs Biomed. Update 2024, 5, 100148. [Google Scholar] [CrossRef]
- Olawade, D.B.; Aderinto, N.; David-Olawade, A.C.; Egbon, E.; Adereni, T.; Popoola, M.R.; Tiwari, R. Integrating AI-driven wearable devices and biometric data into stroke risk assessment: A review of opportunities and challenges. Clin. Neurol. Neurosurg. 2025, 249, 108689. [Google Scholar] [CrossRef] [PubMed]
- Armoundas, A.A.; Narayan, S.M.; Arnett, D.K.; Spector-Bagdady, K.; Bennett, D.A.; Celi, L.A.; Friedman, P.A.; Gollob, M.H.; Hall, J.L.; Kwitek, A.E.; et al. Use of artificial intelligence in improving outcomes in heart disease: A scientific statement from the American Heart Association. Circulation 2024, 149, e1028–e1050. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Liang, N.; Zhang, H.; Li, H.; Yang, Y.; Zong, X.; Chen, Y.; Wang, Y.; Shi, N. Harnessing the power of clinical decision support systems: Challenges and opportunities. Open Heart 2023, 10, e002432. [Google Scholar] [CrossRef]
- Baig, M.M.; Hobson, C.; GholamHosseini, H.; Ullah, E.; Afifi, S. Generative AI in improving personalized patient care plans: Opportunities and barriers towards its wider adoption. Appl. Sci. 2024, 14, 10899. [Google Scholar] [CrossRef]
- Rehman, A.U.; Li, M.; Wu, B.; Ali, Y.; Rasheed, S.; Shaheen, S.; Liu, X.; Luo, R.; Zhang, J. Role of artificial intelligence in revolutionizing drug discovery. Fundam. Res. 2025, 5, 1273–1287. [Google Scholar] [CrossRef]
- González-Rivas, J.P.; Seyedi, S.A.; Mechanick, J.I. Artificial intelligence enabled lifestyle medicine in diabetes care: A narrative review. Am. J. Lifestyle Med. 2025, 15598276251359185. [Google Scholar] [CrossRef]
- Epelde, F. Revolutionizing patient safety: The economic and clinical impact of artificial intelligence in hospitals. Hospitals 2024, 1, 185–194. [Google Scholar] [CrossRef]
- Shah, R.; Bozic, K.J.; Jayakumar, P. Artificial Intelligence in Value-Based Health Care. HSS J.® 2025, 21, 15563316251340074. [Google Scholar]
- Ye, J.; Woods, D.; Jordan, N.; Starren, J. The role of artificial intelligence for the application of integrating electronic health records and patient-generated data in clinical decision support. AMIA Summits Transl. Sci. Proc. 2024, 2024, 459. [Google Scholar]
- Hasan, H.E.; Jaber, D.; Khabour, O.F.; Alzoubi, K.H. Ethical considerations and concerns in the implementation of AI in pharmacy practice: A cross-sectional study. BMC Med. Ethics 2024, 25, 55. [Google Scholar] [CrossRef] [PubMed]
- Elendu, C.; Amaechi, D.C.; Elendu, T.C.; Jingwa, K.A.; Okoye, O.K.; Okah, M.J.; Ladele, J.A.; Farah, A.H.; Alimi, H.A. Ethical implications of AI and robotics in healthcare: A review. Medicine 2023, 102, e36671. [Google Scholar] [CrossRef]
- Kumar, R.; Singh, A.; Kassar, A.S.A.; Humaida, M.I.; Joshi, S.; Sharma, M. Adoption challenges to artificial intelligence literacy in public healthcare: An evidence based study in Saudi Arabia. Front. Public Health 2025, 13, 1558772. [Google Scholar] [CrossRef] [PubMed]
- Weiner, E.B.; Dankwa-Mullan, I.; Nelson, W.A.; Hassanpour, S. Ethical challenges and evolving strategies in the integration of artificial intelligence into clinical practice. PLoS Digit. Health 2025, 4, e0000810. [Google Scholar] [CrossRef] [PubMed]
- Pham, T. Ethical and legal considerations in healthcare AI: Innovation and policy for safe and fair use. R. Soc. Open Sci. 2025, 12, 241873. [Google Scholar] [CrossRef]
- Mennella, C.; Maniscalco, U.; De Pietro, G.; Esposito, M. Ethical and regulatory challenges of AI technologies in healthcare: A narrative review. Heliyon 2024, 10, e26297. [Google Scholar] [CrossRef]
- Hanna, M.G.; Pantanowitz, L.; Jackson, B.; Palmer, O.; Visweswaran, S.; Pantanowitz, J.; Deebajah, M.; Rashidi, H.H. Ethical and bias considerations in artificial intelligence/machine learning. Mod. Pathol. 2025, 38, 100686. [Google Scholar] [CrossRef]
- Ueda, D.; Kakinuma, T.; Fujita, S.; Kamagata, K.; Fushimi, Y.; Ito, R.; Matsui, Y.; Nozaki, T.; Nakaura, T.; Fujima, N.; et al. Fairness of artificial intelligence in healthcare: Review and recommendations. Jpn. J. Radiol. 2024, 42, 3–15. [Google Scholar] [CrossRef]

| Subfield | Definition | Role in Healthcare |
|---|---|---|
| Machine Learning | Learns patterns from data | Predicting adverse drug reactions (ADRs), therapy optimization |
| Deep Learning | Neural networks for complex tasks | Imaging, genomic analysis |
| Natural Language Processing | Understands human language | Drug information extraction, chatbot queries |
| Computer Vision | Enables machines to interpret visual data | Pill identification, prescription label verification, automated inspection in compounding pharmacies |
| Reinforcement Learning | Learns via feedback | Dosing strategies, inventory control |
| AI Application | Purpose | Examples | References |
|---|---|---|---|
| AI-Powered Drug Interaction Checkers | Identify adverse effects from polypharmacy | DynaMedex (Micromedex with Watson), UpToDate® Enterprise EditionAI Chatbots (e.g., ChatGPT, Copilot, Gemini) | [18,19,20,21,22] |
| AI-Based Prescription Analysis & Medication Safety | Detect prescription errors, ensure dose accuracy, and guideline compliance | MedAware, DoseMeRx | [23,24] |
| AI Chatbots for Patient Counselling & Adherence | Improve patient understanding, adherence, and self-management | Pillo Health, Ada Health, MediBot | [25,26,27,28] |
| AI-Driven Drug Discovery & Pharmacovigilance | Accelerate drug development and detect adverse events post-marketing | IBM Watson for Drug Discovery, DeepMind Health, FDA Sentinel System | [29,30,31,32] |
| AI for Personalized Medicine & Pharmacogenomics | Tailor drug therapy using genetic and clinical data | PharmGKB, Tempus | [33,34] |
| AI in Automated Dispensing & Robotics | Enhance accuracy and efficiency in medication handling | BD Rowa™ Vmax, Omnicell, PillPack | [17,35,36] |
| AI in Clinical Decision Support Systems (CDSS) | Assist in evidence-based prescribing and drug safety | Epic Systems, IBM Watson Health, Cerner Millennium | [37,38,39] |
| Stage | AI Application | Techniques/Tools | Example | References |
|---|---|---|---|---|
| Target Identification | Pinpoint disease-associated genes, proteins, pathways | ML, DL, NLP, Multi-omics Integration | BenevolentAI | [78,79] |
| Drug Design & Optimization | Design drug molecules with optimal properties | Generative AI, Molecular Docking, Quantum-AI Modeling | Insilico Medicine (IPF candidate in 18 months) | [79,80] |
| Interaction & Toxicity Prediction | Predict pharmacokinetics and adverse effects | DL, In Silico Pharmacology, Toxicology AI Models | IBM Watson for Drug Discovery | [72,81] |
| Clinical Trial Optimization | Enhance recruitment, reduce costs, and improve trial design | EHR Mining, Synthetic Control Arms, Adaptive Trial Designs | Deep 6 AI | [76] |
| Regulatory & Post-Market Surveillance | Streamline submissions and monitor real-world safety | NLP for Documentation, RWE Analytics, Automated Compliance | Bayer’s Regulatory AI Platform | [82,83] |
| Technology/Tool | Functionality | Examples/Features | References |
|---|---|---|---|
| Smart Pill Bottles/Dispensers | Track medication access and send reminders | Alarms, real-time alerts, EHR synchronization, automated dispensing | [95] |
| Smartwatches/Fitness Bands | Monitor adherence and physiological responses | Vibration alerts, biomarker tracking (e.g., BP, glucose), motion detection of intake | [94,96,97] |
| AI-Enabled Smart Patches | Ensure drug release and monitor compliance | Bluetooth data transmission, adherence logging, alternative to oral/injectable meds | [94,97] |
| Ingestible Sensors (Smart Pills) | Confirm ingestion and track medication absorption | Ingestion data transmission to app/wearables, used in psychiatry and cardiology | [101] |
| AI Virtual Assistants/Chatbots | Provide reminders, education, and real-time support | Voice/text alerts, Alexa/Google integration, habit-based scheduling | [99] |
| AI Communication Tools | Engage patients and provide follow-ups | Two-way SMS, app alerts, telehealth prompts, missed dose follow-ups | [64] |
| AI Monitoring Systems | Analyze behavior and confirm medication intake | Facial recognition, behavioral cues, provider alerts for non-compliance | [94] |
| Area | AI Application | Function/Example | References |
|---|---|---|---|
| Remote Patient Monitoring | Real-Time Health Data Analysis | Detects anomalies from wearables (e.g., arrhythmias, BP changes) | [107] |
| Predictive Analytics | Forecasts disease exacerbations (e.g., COPD, glucose spikes) | [108] | |
| Automated Alerts & Interventions | Notifies providers/patients; suggests lifestyle changes or treatment adjustments | [109] | |
| Personalized Treatment Plans | AI-adjusted insulin/medication dosing based on real-time data | [110] | |
| Telepharmacy | Drug Interaction Detection | Evaluates DDIs via AI tools (e.g., UpToDate®, Chatbots) | [20,21] |
| Medication Adherence Monitoring | Tracks intake via smart devices | [111] | |
| Prescription Verification | Identifies errors using OCR/NLP in digital prescriptions | [112,113] | |
| Pharmacovigilance & ADR Monitoring | Analyzes EHRs and patient data for real-time ADR detection | [15,114] | |
| Personalized Dose Adjustment | Calculates dosages based on patient-specific factors | [115,116] |
| Challenge Area | Key Issues | Suggested Mitigations |
|---|---|---|
| Data Privacy & Security | Breaches, consent, regulatory compliance | Encryption, access control, data governance frameworks |
| Workflow Integration | Compatibility, resistance, training gaps | Infrastructure upgrades, AI literacy programs |
| Regulatory & Legal Gaps | Approval ambiguity, liability questions | Adaptive frameworks, post-market model surveillance |
| Algorithmic Bias | Unequal outcomes, underrepresentation | Inclusive datasets, pharmacist oversight, transparency |
| Ethical Oversight | Over-reliance, patient autonomy concerns | Clinical validation, disclosure, human-in-the-loop design |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alam, A.; Shah, S.S.; Rabbani, S.A.; El-Tanani, M. The Role of Artificial Intelligence in Pharmacy Practice and Patient Care: Innovations and Implications. BioMedInformatics 2025, 5, 65. https://doi.org/10.3390/biomedinformatics5040065
Alam A, Shah SS, Rabbani SA, El-Tanani M. The Role of Artificial Intelligence in Pharmacy Practice and Patient Care: Innovations and Implications. BioMedInformatics. 2025; 5(4):65. https://doi.org/10.3390/biomedinformatics5040065
Chicago/Turabian StyleAlam, Aftab, Syed Sikandar Shah, Syed Arman Rabbani, and Mohamed El-Tanani. 2025. "The Role of Artificial Intelligence in Pharmacy Practice and Patient Care: Innovations and Implications" BioMedInformatics 5, no. 4: 65. https://doi.org/10.3390/biomedinformatics5040065
APA StyleAlam, A., Shah, S. S., Rabbani, S. A., & El-Tanani, M. (2025). The Role of Artificial Intelligence in Pharmacy Practice and Patient Care: Innovations and Implications. BioMedInformatics, 5(4), 65. https://doi.org/10.3390/biomedinformatics5040065






