A Smartphone-Based Algorithm for L Test Subtask Segmentation
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
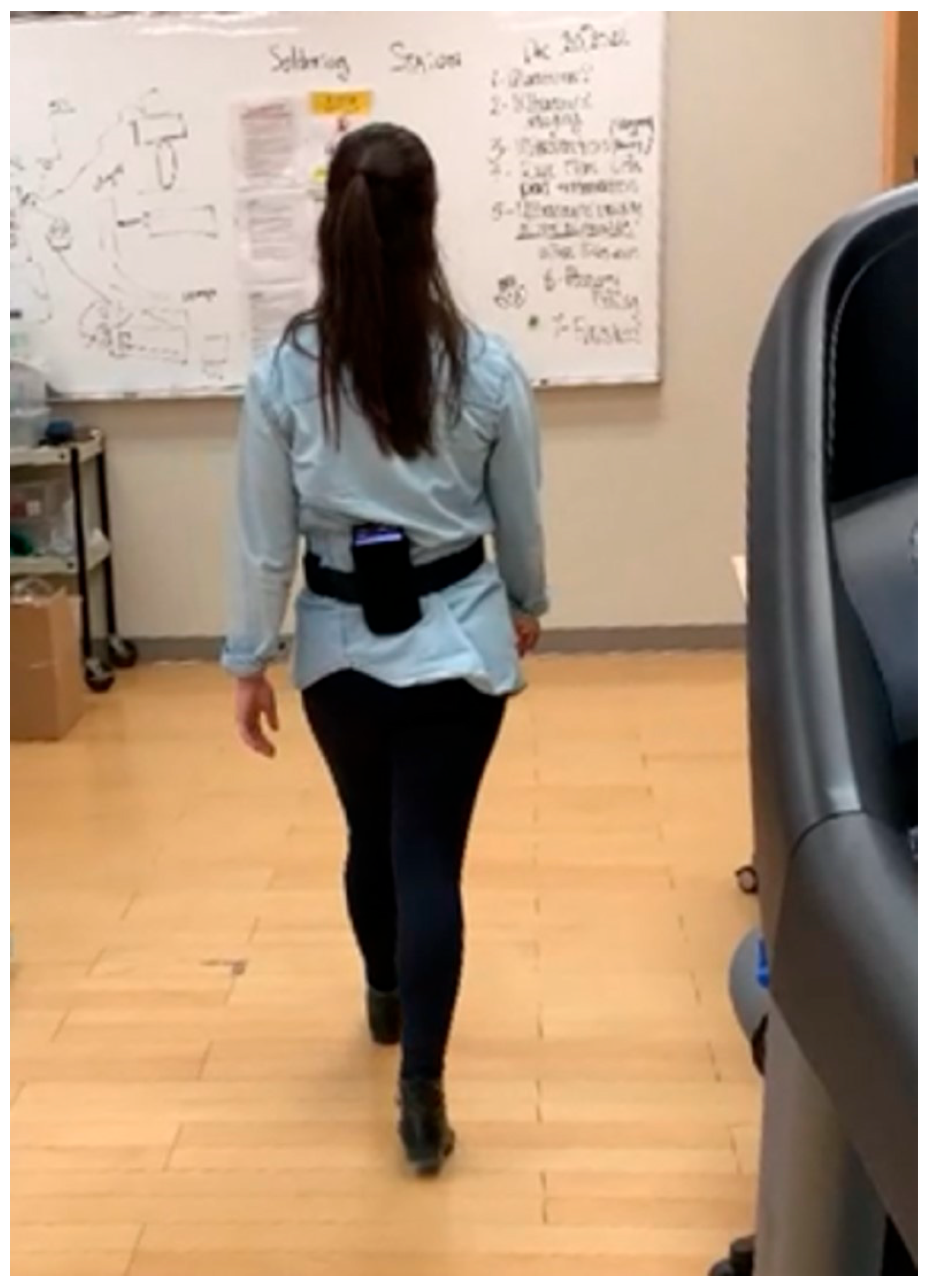
2.2. Data Collection
2.3. Ground Truth
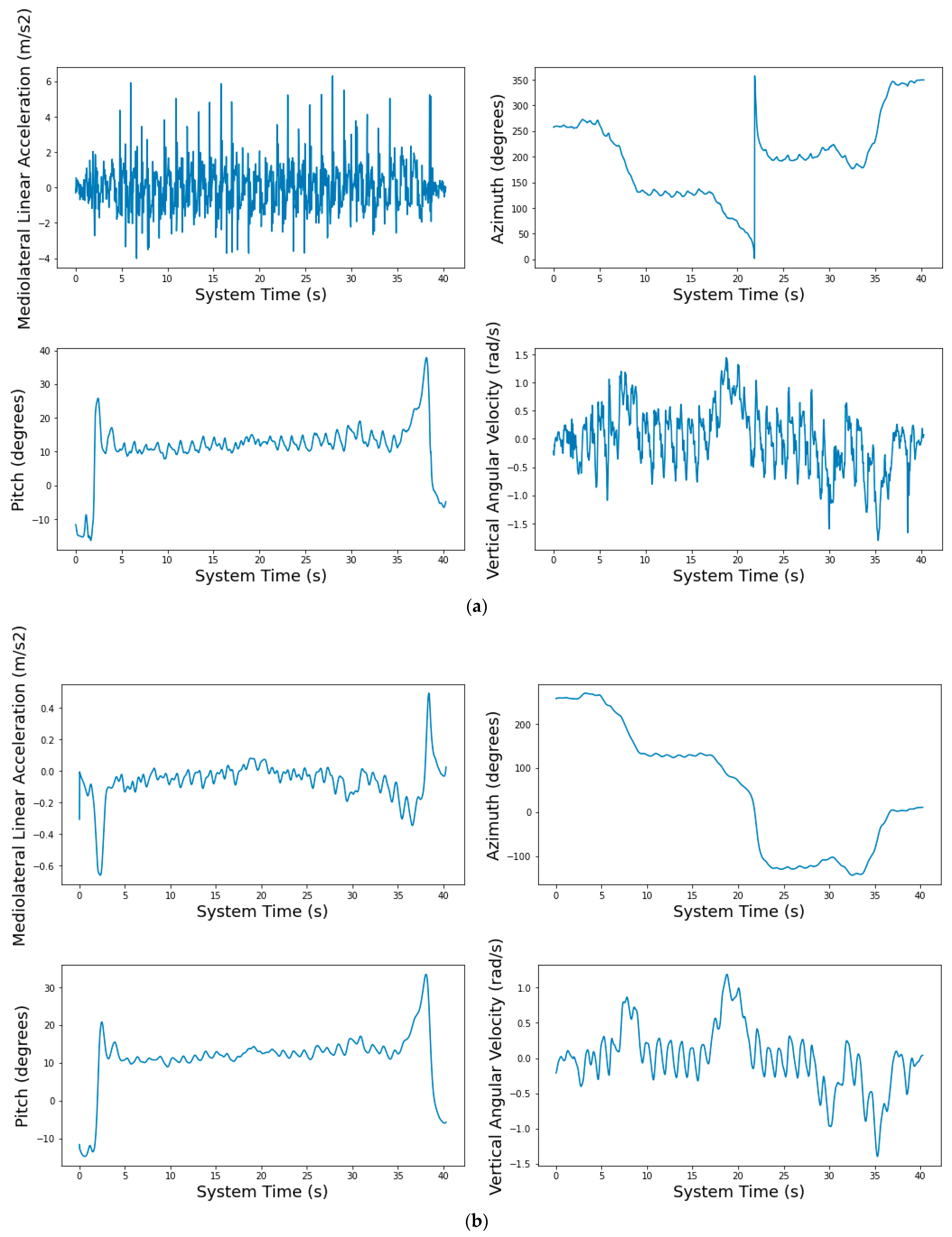
2.4. Preprocessing
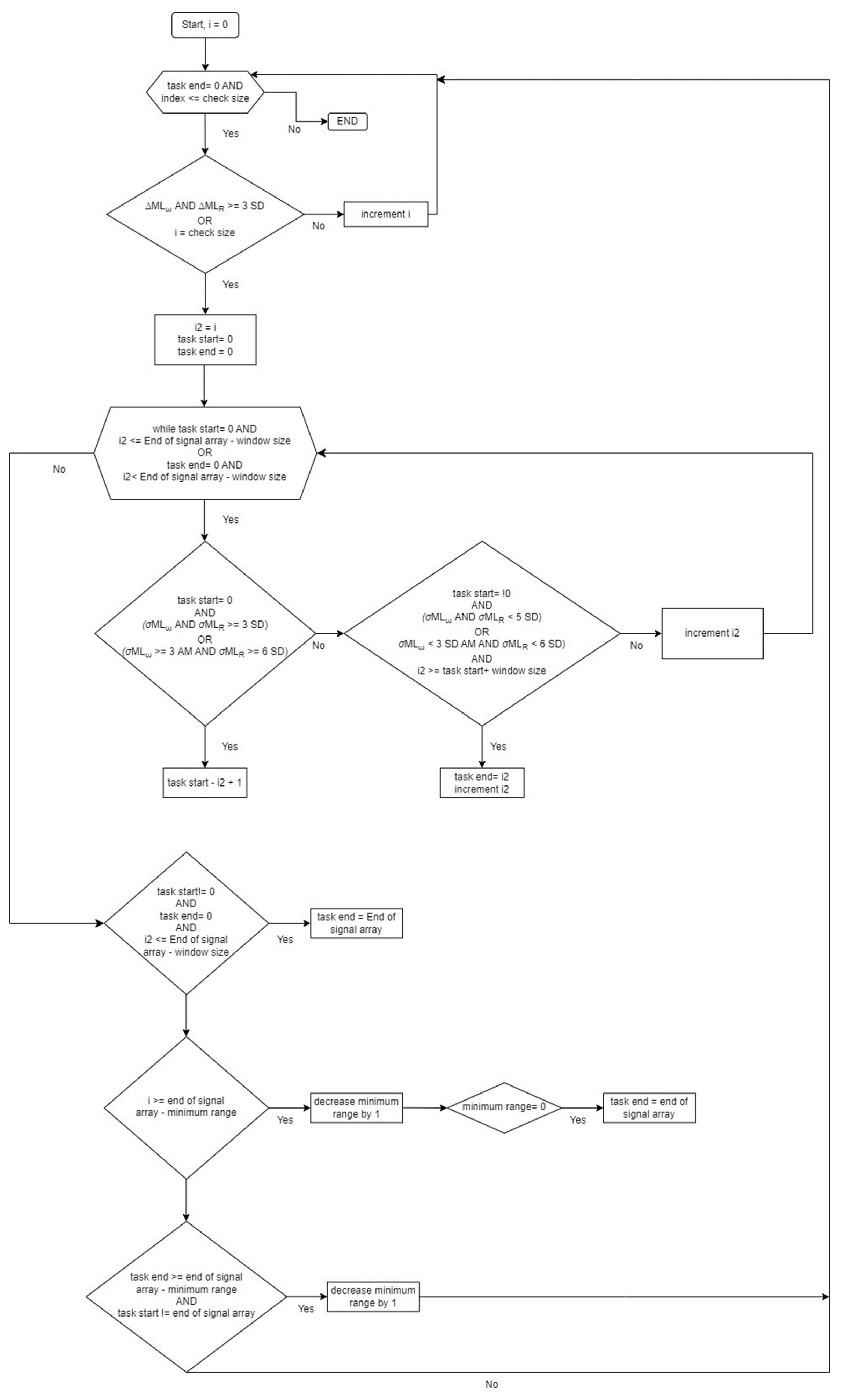
2.5. Algorithm
2.5.1. Algorithm Overview
2.5.2. Threshold Selection
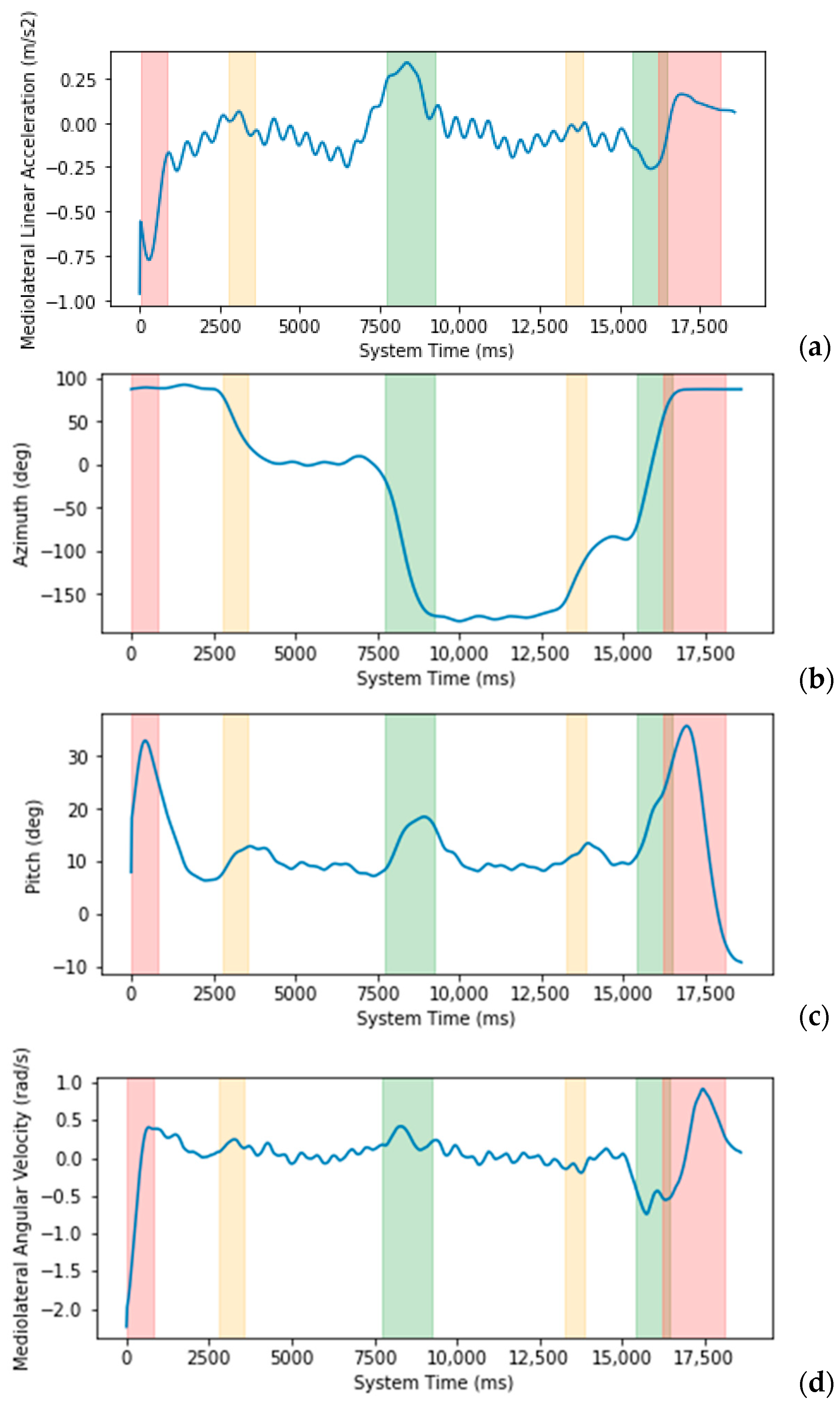
2.5.3. Subtask Identification
3. Results
4. Discussion
Limitations and Future Work
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
References
- Deathe, A.B.; Miller, W.C. The L Test of Functional Mobility: Measurement Properties of a Modified Version of the Timed “Up & Go” Test Designed for People with Lower-Limb Amputations. Phys. Ther. 2005, 85, 626–635. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, H.P.; Ayachi, F.; Lavigne-Pelletier, C.; Blamoutier, M.; Rahimi, F.; Boissy, P.; Jog, M.; Duval, C. Auto detection and segmentation of physical activities during a Timed-Up-and-Go (TUG) task in healthy older adults using multiple inertial sensors. J. Neuroeng. Rehabil. 2015, 12, 36. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, C.-Y.; Huang, H.-Y.; Liu, K.-C.; Chen, K.-H.; Hsu, S.J.; Chan, C.-T. Automatic Subtask Segmentation Approach of the Timed Up and Go Test for Mobility Assessment System Using Wearable Sensors; IEEE: New York, NY, USA, 2019. [Google Scholar] [CrossRef]
- McCreath Frangakis, A.L.; Lemaire, E.D.; Baddour, N. Subtask Segmentation Methods of the Timed Up and Go Test and L Test Using Inertial Measurement Units—A Scoping Review. Information 2023, 14, 127. [Google Scholar] [CrossRef]
- Weiss, A.; Herman, T.; Plotnik, M.; Brozgol, M.; Maidan, I.; Giladi, N.; Gurevich, T.; Hausdorff, J.M. Can an accelerometer enhance the utility of the Timed Up & Go Test when evaluating patients with Parkinson’s disease? Med. Eng. Phys. 2010, 32, 119–125. [Google Scholar] [CrossRef]
- Matey-Sanz, M.; González-Pérez, A.; Casteleyn, S.; Granell, C. Instrumented Timed Up and Go Test Using Inertial Sensors from Consumer Wearable Devices. In Artificial Intelligence in Medicine; Michalowski, M., Abidi, S.S.R., Abidi, S., Eds.; Springer International Publishing: Berlin/Heidelberg, Germany, 2022; pp. 144–154. [Google Scholar] [CrossRef]
- De Luca, V.; Muaremi, A.; Giggins, O.M.; Walsh, L.; Clay, I. Towards fully instrumented and automated assessment of motor function tests. In Proceedings of the 2018 IEEE EMBS International Conference on Biomedical & Health Informatics (BHI), Las Vegas, NV, USA, 4–7 March 2018; pp. 83–87. [Google Scholar] [CrossRef]
- Hellmers, S.; Izadpanah, B.; Dasenbrock, L.; Diekmann, R.; Bauer, J.M.; Hein, A.; Fudickar, S. Towards an Automated Unsupervised Mobility Assessment for Older People Based on Inertial TUG Measurements. Sensors 2018, 18, 3310. [Google Scholar] [CrossRef] [PubMed]
- Vervoort, D.; Vuillerme, N.; Kosse, N.; Hortobágyi, T.; Lamoth, C.J.C. Multivariate Analyses and Classification of Inertial Sensor Data to Identify Aging Effects on the Timed-Up-and-Go Test. PLoS ONE 2016, 11, e0155984. [Google Scholar] [CrossRef]
- Miller Koop, M.; Ozinga, S.J.; Rosenfeldt, A.B.; Alberts, J.L. Quantifying turning behavior and gait in Parkinson’s disease using mobile technology. IBRO Rep. 2018, 5, 10–16. [Google Scholar] [CrossRef] [PubMed]
- Jallon, P.; Dupre, B.; Antonakios, M. A graph based method for timed up & go test qualification using inertial sensors. In Proceedings of the 2011 IEEE International Conference on Acoustics, Speech and Signal Processing (ICASSP), Prague, Czech Republic, 22–27 May 2011; pp. 689–692. [Google Scholar] [CrossRef]
- Hsieh, C.-Y.; Huang, H.-Y.; Liu, K.-C.; Chen, K.-H.; Hsu, S.J.-P.; Chan, C.-T. Subtask Segmentation of Timed Up and Go Test for Mobility Assessment of Perioperative Total Knee Arthroplasty. Sensors 2020, 20, 6302. [Google Scholar] [CrossRef]
- Abdollah, V.; Dief, T.N.; Ralston, J.; Ho, C.; Rouhani, H. Investigating the validity of a single tri-axial accelerometer mounted on the head for monitoring the activities of daily living and the timed-up and go test. Gait Posture 2021, 90, 137–140. [Google Scholar] [CrossRef]
- Ortega-Bastidas, P.; Aqueveque, P.; Gómez, B.; Saavedra, F.; Cano-de-la-Cuerda, R. Use of a Single Wireless IMU for the Segmentation and Automatic Analysis of Activities Performed in the 3-m Timed Up & Go Test. Sensors 2019, 19, 1647. [Google Scholar] [CrossRef]
- Zakaria, N.A.; Kuwae, Y.; Tamura, T.; Minato, K.; Kanaya, S. Quantitative analysis of fall risk using TUG test. Comput. Methods Biomech. Biomed. Eng. 2013, 18, 426–437. [Google Scholar] [CrossRef] [PubMed]
- Silva, J.; Sousa, I. Instrumented timed up and go: Fall risk assessment based on inertial wearable sensors. In Proceedings of the 2016 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Benevento, Italy, 15–18 May 2016; pp. 1–6. [Google Scholar] [CrossRef]
- Greene Barry, R.; O’Donovan, A.; Romero-Ortuno, R.; Cogan, L.; Scanaill, C.N.; Kenny, R.A. Quantitative Falls Risk Assessment Using the Timed Up and Go Test. IEEE Trans. Biomed. Eng. 2010, 57, 2918–2926. [Google Scholar] [CrossRef] [PubMed]
- Milosevic, M.; Jovanov, E.; Milenković, A. Quantifying Timed-Up-and-Go test: A smartphone implementation. In Proceedings of the 2013 IEEE International Conference on Body Sensor Networks, Cambridge, MA, USA, 6–9 May 2013. [Google Scholar] [CrossRef]
- Negrini, S.; Serpelloni, M.; Amici, C.; Gobbo, M.; Silvestro, C.; Buraschi, R.; Borboni, A.; Crovato, D.; Lopomo, N.F. Use of Wearable Inertial Sensor in the Assessment of Timed-Up-and-Go Test: Influence of Device Placement on Temporal Variable Estimation. In Wireless Mobile Communication and Healthcare; Perego, P., Andreoni, G., Rizzo, G., Eds.; Springer International Publishing: Berlin/Heidelberg, Germany, 2017; pp. 310–317. [Google Scholar] [CrossRef]
- Beyea, J.; McGibbon, C.A.; Sexton, A.; Noble, J.; O’Connell, C. Convergent Validity of a Wearable Sensor System for Measuring Sub-Task Performance during the Timed Up-and-Go Test. Sensors 2017, 17, 934. [Google Scholar] [CrossRef] [PubMed]
- Adame, M.R.; Al-Jawad, A.; Romanovas, M.; Hobert, M.A.; Maetzler, W.; Möller, K.; Manoli, Y. TUG Test Instrumentation for Parkinson’s disease patients using Inertial Sensors and Dynamic Time Warping. Biomed. Eng./Biomed. Tech. 2012, 57, 1071–1074. [Google Scholar] [CrossRef]
- Witchel, H.J.; Oberndorfer, C.; Needham, R.; Healy, A.; Westling, C.E.I.; Guppy, J.H.; Bush, J.; Barth, J.; Herberz, C.; Roggen, D.; et al. Thigh-Derived Inertial Sensor Metrics to Assess the Sit-to-Stand and Stand-to-Sit Transitions in the Timed Up and Go (TUG) Task for Quantifying Mobility Impairment in Multiple Sclerosis. Front. Neurol. 2018, 9, 689–695. [Google Scholar] [CrossRef] [PubMed]
- Salarian, A.; Horak, F.B.; Zampieri, C.; Carlson-Kuhta, P.; Nutt, J.G.; Aminian, K. iTUG, a sensitive and reliable measure of mobility. IEEE Trans. Neural Syst. Rehabil. Eng. 2010, 18, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Higashi, Y.; Yamakoshi, K.; Fujimoto, T.; Sekine, M.; Tamura, T. Quantitative evaluation of movement using the timed up-and-go test. IEEE Eng. Med. Biol. Mag. 2008, 27, 38–46. [Google Scholar] [CrossRef]
- Yahalom, G.; Yekutieli, Z.; Israeli-Korn, S.; Elincx-Benizri, S.; Livneh, V.; Fay-Karmon, T.; Rubel, Y.; Tchelet, K.; Zauberman, J.; Hassin-Baer, S. AppTUG-A Smartphone Application of Instrumented ‘Timed Up and Go’ for Neurological Disorders. EC Neurol. 2018, 10, 689–695. [Google Scholar]
- Pew, C.; Klute, G.K. Turn Intent Detection for Control of a Lower Limb Prosthesis. IEEE Trans. Biomed. Eng. 2018, 65, 789–796. [Google Scholar] [CrossRef]
- Nguyen, H.; Lebel, K.; Boissy, P.; Bogard, S.; Goubault, E.; Duval, C. Auto detection and segmentation of daily living activities during a Timed Up and Go task in people with Parkinson’s disease using multiple inertial sensors. J. Neuroeng. Rehabil. 2017, 14, 26. [Google Scholar] [CrossRef]
- Mellone, S.; Tacconi, C.; Chiari, L. Validity of a Smartphone-based instrumented Timed Up and Go. Gait Posture 2012, 36, 163–165. [Google Scholar] [CrossRef] [PubMed]
- McCreath Frangakis, A.L.; Lemaire, E.D.; Baddour, N. Subtask Segmentation of the L Test Using Smartphone Inertial Measurement Units. In Proceedings of the 2023 5th International Conference on Bio-engineering for Smart Technologies (BioSMART), Paris, France, 7–9 June 2023; pp. 1–4. [Google Scholar] [CrossRef]
- Capela, N.A.; Lemaire, E.D.; Baddour, N. Novel algorithm for a smartphone-based 6-minute walk test application: Algorithm, application development, and evaluation. J. Neuroeng. Rehabil. 2015, 12, 19. [Google Scholar] [CrossRef] [PubMed]
- Android Apps on Google Play. Available online: https://play.google.com/store/games?hl=en&gl=US (accessed on 26 March 2024).
- Kinovea. Available online: https://www.kinovea.org/ (accessed on 14 September 2023).
- Tudor-Locke, C.; Aguiar, E.J.; Han, H.; Ducharme, S.W.; Schuna, J.M.; Barreira, T.V.; Moore, C.C.; Busa, M.A.; Lim, J.; Sirard, J.R.; et al. Walking cadence (steps/min) and intensity in 21–40 year olds: CADENCE-adults. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 8. [Google Scholar] [CrossRef] [PubMed]
- Capela, N.; Lemaire, E.; Baddour, N.; Rudolf, M.; Goljar, N.; Burger, H. Evaluation of a smartphone human activity recognition application with able-bodied and stroke participants. J. Neuroeng. Rehabil. 2016, 13, 5. [Google Scholar] [CrossRef]
- Juneau, P.; Baddour, N.; Burger, H.; Bavec, A.; Lemaire, E.D. Amputee Fall Risk Classification Using Machine Learning and Smartphone Sensor Data from 2-Minute and 6-Minute Walk Tests. Sensors 2022, 22, 1479. [Google Scholar] [CrossRef]


| Age Group | Sex | Number of Participants |
|---|---|---|
| 18–29 | Male | 3 |
| Female | 9 | |
| 30–39 | Male | 0 |
| Female | 1 | |
| 40–49 | Male | 0 |
| Female | 0 | |
| 50–59 | Male | 2 |
| Female | 4 | |
| 60–69 | Male | 1 |
| Female | 1 |
| Subtask | Signal | Beginning of Search | End of Search | Direction of Search | Magnitude Change Threshold | Standard Deviation Threshold |
|---|---|---|---|---|---|---|
| Stand-Up | MLR 1 MLω 2 [2,3,6,7,8,9,11,12,13,14,15,16,17,18,19,20,21,22,23,27] | Start of data array | End of data array | Start to end of array | 3 SD above mean 3 | 5 SD above mean 3 or 6 SD above mean (MLR) and 3 SD above mean (MLω) |
| First 90° Turn | Azimuth [30] | One second after end of stand-up | End of data array | Start to end of array | 35° | 5° |
| First 180° Turn | Azimuth | One second after end of first 90° turn | End of data array | Start to end of array | 35° | 5° |
| Second 90° Turn | Azimuth | One second after end of first 180° turn | End of data array | Start to end of array | 35° | 5° |
| Second 180° Turn | Azimuth | One second after end of second 90° turn | End of data array | Start to end of array | 35° | 5° |
| Sit-Down | MLR 1 MLω 2 | One second after end of second 90° turn | End of data array | End to beginning of array | 3 SD above mean 3 | 5 SD above mean 3 or 6 SD above mean (MLR) and 3 SD above mean (MLω) |
| Participant ID | Stand-Up | GT Stand-Up | Sit-Down | GT Sit-Down | First 90° Turn | GT First 90° Turn | First 180° Turn | GT First 180° Turn | Second 90° Turn | GT Second 90° Turn | Second 180° Turn | GT Second 180° Turn |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LT_001 | 1.08 ± 0.12 | 0.85 ± 0.08 | 0.61 ± 0.11 | 1.23 ± 0.44 | 0.74 ± 0.25 | 0.97 ± 0.08 | 1.04 ± 0.14 | 1.21 ± 0.14 | 0.57 ± 0.08 | 0.75 ± 0.07 | 0.71 ± 0.08 | 0.75 ± 0.11 |
| LT_002 | 1.47 ± 0.32 | 0.79 ± 0.44 | 1.54 ± 0.33 | 1.05 ± 0.52 | 0.71 ± 0.42 | 0.63 ± 0.34 | 0.89 ± 0.45 | 1.01 ± 0.51 | 0.53 ± 0.07 | 0.61 ± 0.30 | 0.78 ± 0.18 | 0.49 ± 0.35 |
| LT_003 | 1.15 ± 0.12 | 0.69 ± 0.11 | 1.6 ± 0.09 | 1.18 ± 0.19 | 0.57 ± 0.10 | 0.69 ± 0.29 | 0.79 ± 0.07 | 1.02 ± 0.16 | 0.52 ± 0.02 | 0.66 ± 0.17 | 0.68 ± 0.08 | 0.72 ± 0.13 |
| LT_004 | 1.03 ± 0.07 | 1.07 ± 0.15 | 1.25 ± 0.08 | 1.20 ± 0.09 | 0.60 ± 0.11 | 0.73 ± 0.08 | 0.94 ± 0.09 | 1.10 ± 0.07 | 0.53 ± 0.03 | 0.66 ± 0.11 | 0.82 0.04 | 1.01 ± 0.06 |
| LT_005 | 1.35 ± 0.48 | 0.85 ± 0.32 | 0.85 ± 0.28 | 0.74 ± 0.34 | 0.55 ± 0.02 | 0.73 ± 0.12 | 0.88 ± 0.03 | 1.08 ± 0.08 | 0.62 ± 0.13 | 0.87 ± 0.07 | 0.91 ± 0.13 | 0.69 ± 0.06 |
| LT_006 | 1.16 ± 0.10 | 1.03 ± 0.08 | 0.57 ± 0.15 | 1.19 ± 0.10 | 0.66 ± 0.09 | 0.95 ± 0.07 | 1.19 ± 0.11 | 1.42 ± 0.18 | 0.59 ± 0.08 | 0.81 ± 0.14 | 1.04 ± 0.12 | 1.02 ± 0.06 |
| LT_007 | 1.04 ± 0.05 | 0.89 ± 0.18 | 1.25 ± 0.29 | 1.32 ± 0.19 | 0.60 ± 0.08 | 0.78 ± 0.16 | 0.87 ± 0.10 | 0.98 ± 0.21 | 0.59 ± 0.08 | 0.59 ± 0.11 | 0.77 ± 0.12 | 0.85 ± 0.12 |
| LT_008 | 1.02 ± 0.03 | 1.06 ± 0.12 | 0.72 ± 0.14 | 1.43 ± 0.19 | 0.53 ± 0.04 | 0.94 ± 0.16 | 1.28 ± 0.24 | 1.41 ± 0.13 | 0.71 ± 0.13 | 0.88 ± 0.21 | 0.84 ± 0.17 | 1.07 ± 0.09 |
| LT_009 | 1.26 ± 0.15 | 1.01 ± 0.25 | 1.5 ± 0.14 | 1.19 ± 0.14 | 0.52 ± 0.05 | 0.70 ± 0.08 | 0.82 ± 0.10 | 1.07 ± 0.05 | 0.5 ± 0.00 | 0.78 ± 0.16 | 0.81 ± 0.04 | 0.96 ± 0.05 |
| LT_010 | 1.03 ± 0.06 | 0.82 ± 0.11 | 1.16 ± 0.43 | 1.16 ± 0.18 | 0.66 ± 0.7 | 0.84 ± 0.09 | 0.86 ± 0.07 | 1.15 ± 0.07 | 0.64 ± 0.07 | 0.87 ± 0.09 | 0.83 ± 0.04 | 1.09 ± 0.09 |
| LT_011 | 1.00 ± 0.00 | 0.91 ± 0.07 | 0.85 ± 0.15 | 1.14 ± 0.19 | 0.75 ± 0.12 | 1.06 ± 0.08 | 0.94 ± 0.14 | 1.51 ± 0.20 | 0.63 ± 0.07 | 0.89 ± 0.10 | 0.97 ± 0.12 | 1.23 ± 0.09 |
| LT_012 | 1.08 ± 0.09 | 0.87 ± 0.09 | 0.96 ± 0.41 | 1.31 ± 0.20 | 0.59 ± 0.07 | 0.62 ± 0.05 | 0.93 ± 0.10 | 1.05 ± 0.09 | 0.78 ± 0.16 | 0.81 ± 0.10 | 0.78 ± 0.12 | 1.01 ± 0.13 |
| LT_013 | 1.26 ± 0.23 | 0.96 ± 0.14 | 1.55 ± 0.38 | 1.42 ± 0.12 | 0.61 ± 0.08 | 0.74 ± 0.12 | 1.05 ± 0.11 | 1.11 ± 0.10 | 0.73 ± 0.11 | 0.93 ± 0.18 | 0.78 ± 0.11 | 0.90 ± 0.08 |
| LT_014 | 1.25 ± 0.06 | 0.78 ± 0.06 | 1.54 ± 0.18 | 1.14 ± 0.09 | 0.6 ± 0.12 | 0.71 ± 0.12 | 0.99 ± 0.11 | 1.11 ± 0.05 | 0.62 ± 0.10 | 0.82 ± 0.10 | 0.95 ± 0.15 | 1.08 ± 0.09 |
| LT_015 | 1.24 ± 0.14 | 0.98 ± 0.04 | 1.53 ± 0.13 | 1.43 ± 0.24 | 0.70 ± 0.04 | 0.86 ± 0.17 | 1.05 ± 0.18 | 1.44 ± 0.04 | 0.72 ± 0.03 | 1.12 ± 0.04 | 0.99 ± 0.03 | 1.30 ± 0.03 |
| LT_016 | 1.65 ± 0.42 | 1.55 ± 0.36 | 1.48 ± 0.36 | 1.76 ± 0.24 | 0.84 ± 0.15 | 0.93 ± 0.10 | 1.15 ± 0.21 | 1.39 ± 0.26 | 0.90 ± 0.19 | 0.99 ± 0.12 | 1.16 ± 0.21 | 1.47 ± 0.27 |
| LT_017 | 1.31 ± 0.16 | 0.91 ± 0.12 | 1.71 ± 0.08 | 1.43 ± 0.08 | 0.74 ± 0.06 | 0.87 ± 0.12 | 1.03 ± 0.10 | 1.26 ± 0.04 | 0.74 ± 0.06 | 0.80 ± 0.17 | 1.03 ± 0.10 | 1.17 ± 0.13 |
| LT_018 | 1.12 ± 0.10 | 0.74 ± 0.36 | 1.44 ± 0.29 | 1.07 ± 0.53 | 0.63 ± 0.10 | 0.77 ± 0.38 | 0.71 ± 0.36 | 0.97 ± 0.48 | 0.68 ± 0.04 | 0.88 ± 0.43 | 0.72 ± 0.35 | 1.06 ± 0.52 |
| LT_019 | 1.13 ± 0.05 | 0.96 ± 0.07 | 1.48 ± 0.33 | 1.45 ± 0.05 | 0.60 ± 0.06 | 0.80 ± 0.07 | 1.40 ± 0.10 | 1.50 ± 0.13 | 0.71 ± 0.09 | 0.97 ± 0.11 | 0.98 ± 0.06 | 1.29 ± 0.10 |
| LT_020 | 1.04 ± 0.06 | 0.88 ± 0.05 | 1.50 ± 0.20 | 1.25 ± 0.16 | 0.50 ± 0.00 | 0.66 ± 0.12 | 1.14 ± 0.39 | 1.47 ± 0.23 | 0.56 ± 0.08 | 0.67 ± 0.05 | 0.65 ± 0.03 | 0.80 ± 0.07 |
| LT_021 | 1.05 ± 0.05 | 0.82 ± 0.08 | 0.83 ± 0.23 | 1.08 ± 0.07 | 0.64 ± 0.12 | 0.95 ± 0.09 | 0.95 ± 0.11 | 1.31 ± 0.12 | 0.66 ± 0.13 | 0.88 ± 0.15 | 0.85 ± 0.03 | 0.98 ± 0.07 |
| Metric | Stand-Up | Sit-Down | First 90° Turn | First 180° Turn | Second 90° Turn | Second 180° Turn |
|---|---|---|---|---|---|---|
| Accuracy (%) | 98.5 | 97.1 | 98.7 | 98.7 | 98.9 | 98.8 |
| Specificity (%) | 98.6 | 98.6 | 99.8 | 99.9 | 99.9 | 99.8 |
| Sensitivity (%) | 97.4 | 78.3 | 74.3 | 81.7 | 77.1 | 82.1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
McCreath Frangakis, A.L.; Lemaire, E.D.; Baddour, N. A Smartphone-Based Algorithm for L Test Subtask Segmentation. BioMedInformatics 2024, 4, 1262-1274. https://doi.org/10.3390/biomedinformatics4020069
McCreath Frangakis AL, Lemaire ED, Baddour N. A Smartphone-Based Algorithm for L Test Subtask Segmentation. BioMedInformatics. 2024; 4(2):1262-1274. https://doi.org/10.3390/biomedinformatics4020069
Chicago/Turabian StyleMcCreath Frangakis, Alexis L., Edward D. Lemaire, and Natalie Baddour. 2024. "A Smartphone-Based Algorithm for L Test Subtask Segmentation" BioMedInformatics 4, no. 2: 1262-1274. https://doi.org/10.3390/biomedinformatics4020069
APA StyleMcCreath Frangakis, A. L., Lemaire, E. D., & Baddour, N. (2024). A Smartphone-Based Algorithm for L Test Subtask Segmentation. BioMedInformatics, 4(2), 1262-1274. https://doi.org/10.3390/biomedinformatics4020069








