Abstract
Networks form the backbone of any healthcare system. Various databases were searched with relevant keywords, data were abstracted, and numerous papers were appraised for this synthesis. This compiled systematic review gives a comprehensive overview of various networks that are found in healthcare, with a special reference to the treatment, referral, and best-practice care of patients. Special support networks, such as Clinical decision support systems, Physician collaboration networks, Telemedicine networks, and Shared healthcare record access, are also described, as these support networks play a pivotal role in improving the quality of healthcare for patients.
1. Introduction
Networks in healthcare play a critical role in coordinating care and improving the quality of healthcare for patients. Networks are essential tools in the healthcare industry, as they enable communication and information sharing among individuals working in different roles and locations. Networks provide an efficient way to share patient data, treatment protocols, research results, resources, and staff information with various participants in the health care system. Additionally, networks facilitate electronic communication between different healthcare providers, including physicians of various specialties, who can exchange patient records quickly and accurately. Furthermore, networks offer users a secure method of data transfer that is more reliable than traditional paper-based methods. By optimizing interconnectivity among a wide array of stakeholders within the healthcare system, networks empower medical practitioners to provide better quality care for patients [1].
Healthcare networks come in a variety of forms, including managed care organizations, accountable care organizations, and provider-sponsored groups. Networks that are owned and run by healthcare providers, including hospitals or physician groups, are known as provider-sponsored organizations. Accountable care organizations are groups of healthcare professionals who collaborate to coordinate and enhance the standard of treatment for a group of patients while also reducing the associated expenses [1,2].
2. Materials and Methods
2.1. The Study Design
A systematic review of observational studies was conducted to provide an overview of the prevalent networks in healthcare systems. The Cochrane Collaboration methodology [2] was followed, and we adhered to PRISMA guidelines [3].
2.2. Search Strategy
Observational healthcare studies which focused on networks were searched, analyzed, and included in this review. Institutional Elsevier’s Clinical Key, PubMed, and Google Scholar were searched for the relevant literature pertaining to Networks in healthcare systems. Keywords included “networks in healthcare”, “net-work analysis”, “data sets”, and “graph theory” [2].
2.3. Inclusion and Exclusion Criteria
Two authors analyzed and selected N = 25 relevant papers for analysis, abstraction, and inclusion in this review as per the PRISMA flowchart shown in Figure 1. Papers that had no information about network terminology and healthcare were excluded from this review.
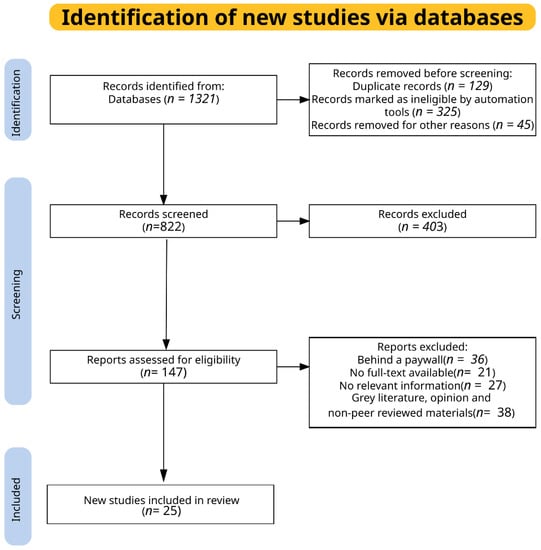
Figure 1.
Methodology of our systematic review as per PRISMS guidelines for reporting of Systematic reviews [3].
Duplicate hits were excluded from this study. Those papers behind a large paywall or without full text were also excluded. Outdated papers were excluded, but no relevant material was omitted from the synthesis. This generated a total 147 papers. Studies about the theoretical framework of networks, computer networks, or IOT networks were excluded. Non-English language studies, grey literature, non-peer reviewed, and unavailable full text were excluded from the review [2].
2.4. Data Abstraction and Quality Checks
Data extracted from the included papers included the authors, affiliation, author’s observations, inferences, conclusions, date of publication, and the impact factor of the journal. The quality of evidence was determined by mutual agreement between the authors [2,3].
3. Results of Systematic Review on Networks in Healthcare
This section may be divided by subheadings. It should provide a concise and precise description of the experimental results, their interpretation, as well as the experimental conclusions that can be drawn.
3.1. Informatics, Networks, Systems, and Databases Defined [2,3]
Informatics is the science of acquisition, processing, and inferring from data. Informatics data can be generated from several diverse sources, such as laboratory experiments, abstractly from mathematical computations, automated analyzers, sensors, clinical research, etc. Bioinformatics is the most popular branch of informatics that deals with biological information and is concerned with proteins, DNA, RNA, and their complex interactions [3,4].
3.1.1. Networks
Networks are interconnected systems, services, devices, and applications in informatics that allow for communication and information sharing. Networks, such as computer networks, social networks, and biological networks, are essential in many areas of informatics.
The communication infrastructure that enables computers to share resources, exchange data, and communicate with one another, is referred to as a computer network. This infrastructure consists of hardware, such as routers, switches, and firewalls, as well as software that implements TCP/IP, HTTP, and DNS protocols.
Social networks are online spaces, such as Facebook, Twitter, and LinkedIn, that let users connect and communicate with one another. These platforms make it possible for people and communities to exchange knowledge, concepts, and resources.
The term “biological networks” describes the intricate webs of interactions between various biological components, including genes, proteins, and metabolites. To understand biological processes, such as gene expression, protein–protein interactions, and metabolic pathways, these networks can be examined using a variety of computational and mathematical tools. Generally, networks are important in informatics because they enable information sharing and exchange, encourage teamwork and communication, and serve as the foundation for a variety of applications and systems [3].
3.1.2. System
A system in informatics can be defined as a group of elements, processes, and procedures created to carry out a single function or collection of related functions. These elements could be people who work with the system to accomplish a certain objective, as well as technology, software, data, and other elements.
In informatics, there are many kinds of systems, including:
- Information systems: Systems created to gather, process, store, and disseminate information are known as information systems. Databases, data warehouses, and decision support systems are a few examples of information systems [3].
Operating systems are programs that control hardware resources and give other programs a place to run. The operating systems Windows, macOS, and Linux are a few examples.
- Network systems: These are the systems that allow for inter-device communication. Network systems examples include routers, switches, etc.
- Software systems: Systems that offer software applications for carrying out activities are known as software systems. Word processing programs, spreadsheets, and video editing software are a few examples of software systems.
Systems for managing and controlling industrial activities, such as manufacturing and electricity production, are known as control systems [2,3].
3.1.3. Database
A database is a grouping of well-organized data in informatics that can be quickly accessed, maintained, and updated. Databases are used in many different contexts and fields, such as industry, government, scientific research, and healthcare.
Based on their organization and structure, databases can be divided into various categories, including:
- Relational databases: These databases employ tables to store data, and primary and foreign keys are used to identify the relationships between the tables.
- Non-Relational databases (NoSQL databases): These databases store data in a non-relational manner and are frequently used for real-time and big data applications.
- Object-oriented databases: This category of database uses objects to store data, similar to what object-oriented programming does.
- Graph databases: Databases that use graph topologies to store data and the relationships between entities are known as “graph databases.”
- Database management systems (DBMS), which are software programs that let users create, edit, and query databases, can be used to access and manipulate databases. Oracle, MySQL, Microsoft SQL Server, and MongoDB are all well-known DBMS.
Large amounts of structured and unstructured data, such as patient health information, financial data, scientific data, and government data, are stored and managed in informatics using databases. Since they offer a structured and organized means to store, handle, and access data, which is necessary for successful and efficient data processing and analysis, databases are crucial in informatics [2].
3.2. Role of Networks in Healthcare
By enabling the exchange of resources and information and promoting collaboration and coordination between many stakeholders, networks in healthcare play a crucial role in enhancing the efficacy and efficiency of the healthcare system [5]. Networks in healthcare come in a wide variety of shapes and sizes. Here are a few illustrations:
3.2.1. Research Networks
A research network is a type of professional communication platform that provides researchers with the tools to interact and collaborate within their respective fields. It enables the sharing of ideas and knowledge among experts on a variety of topics, making it an invaluable tool for research productivity. Researchers also benefit from being able to track research activities, manage collaboration projects, access up-to-date literature reviews, discuss scholarly matters, and receive real-time feedback from colleagues around the world. Examples of research networks include ResearchGate, Semantic Scholar, and Academia.edu.
Additionally, many research networks are designed with security in mind and provide encryption technologies to ensure that sensitive data are transmitted securely. Research data are shared and made available for others to review or reuse on data-sharing networks, such as Figshare. With these features, a well-executed network can provide great value for both experienced and novice researchers alike. These networks bring together scholars from various universities to work together on projects and studies pertaining to healthcare [6].
3.2.2. Patient Group Networks or Patient Groups
Patient group networks are organized groups of individuals that come together to share and exchange healthcare information, experiences, and resources, as depicted in Figure 2. These networks link patients and the people who care for them to resources, support groups, and knowledge about certain illnesses or treatments. Through the network, individuals can access shared resources, such as medical knowledge, treatment options, research studies, support programs, and more. They also provide a platform for patients to connect to others with similar illnesses and challenges, allowing them to exchange ideas, success stories, and practical advice. Examples of patient group networks include PatientView, and NHS-Patient Participation Groups (PPGs).
Figure 2.
Healthcare system is a living organism comprising of many networks of professions and departments. This image composite is under CC0 in public domain license.
Patient group networks are beneficial to both patients and healthcare providers, as they enable the dissemination of up-to-date, timely information, which can inform best practices and enable personalized treatments tailored to individual needs. This collective sharing of health information strengthens patient engagement in their own care while giving healthcare providers access to valuable data and insight into larger trends in health outcomes or disease management programs [7].
3.2.3. Health Insurance Networks or Payer Networks
Health insurance networks, or payer networks, are a critical component of providing healthcare coverage. These networks are managed by insurers and provide subscribers with access to a range of providers, facilities, and services. The network contains key contracts that both the insurer and provider accept regarding the cost of service provided to members. Examples of types of health insurance networks in the US include Preferred Provider Organizations (PPOs) and Health Maintenance Organizations (HMOs).
This system helps define providers who have agreed to accept reimbursement rates for medical services in return for being part of the network. An important factor in the selection of health plans is size and the type of network since providers may choose not to join networks associated with specific carriers, which limits choices for patients with that carrier’s product/s. As such, it is essential for insurers and employers to create open systems with diverse options so that subscribers can attain optimal healthcare coverage [8].
3.2.4. Clinical Decision Support Systems (CDSS)
Clinical decision support systems (CDSS) are a form of technology that aims to assist the clinician in making decisions regarding the care of patients. Many of these tools are integrated into Hospital Information Management Systems (HIMS) such as Suvarna (India). Artificial intelligence is slowly making great progress in CDSS tools. These tools make better decisions about patient care by using knowledge bases and algorithms [8].
3.2.5. Telemedicine Networks
Telemedicine networks are an increasingly important part of healthcare delivery. They enable healthcare providers to transmit medical data and images electronically, thereby connecting distant specialist physicians with primary care providers or hospitals in remote locations. Examples of types of Telemedicine networks include the SmarTigr system by the Charleston Area Medical Centre. Access to timely medical advice from leading specialists across the globe has created an unprecedented level of convenience for patients, with improved prevention and diagnosis of illnesses, quicker treatments, and better health outcomes. In addition to facilitating the flow of vital medical information through virtual visits between clinicians and their patients, regardless of geographical distance, telemedicine networks also allow healthcare organizations to analyze data more efficiently and provide a higher quality of patient care. As a result, telemedicine is becoming a cost-effective solution for many organizations within the healthcare industry. These networks allow medical professionals to use video conferencing or other technologies to provide distant medical services, such as consultations and follow-up visits [9].
3.2.6. Supply Chain Networks
Hospital supply chain networks are complex yet vitally important systems that connect healthcare providers with product manufacturers and distributors. These networks aid in controlling the movement of medical equipment and supplies both within and between different healthcare institutions. Examples of types of hospital supply chain networks include Trinity Heath in the US and Intermountain Healthcare in Utah, US. These networks must provide reliable, high-quality services to ensure that hospitals have the necessary supplies when they are needed. Every hospital’s needs are unique and may include a range of products from medical equipment to pharmaceuticals to medical facility maintenance supplies. In addition, there is often a great deal of fluctuation in demand for various items, requiring a sophisticated and agile planning process at all levels of the supply chain network. Strategic relationships between suppliers and hospitals can ensure the delivery of optimal quality products, reduce costs over time, protect against sudden changes in market conditions, and guarantee smooth operations for both partners. Furthermore, efficient hospital supply chain networks depend on stringent processes for contract negotiation, inventory management, cost tracking, and performance evaluations to maximize results [10].
3.2.7. Public Health Networks
These networks help public health organizations, research institutes, and other groups seeking to enhance the health of communities share information and resources. Examples of types of public health networks include National Health Trust (NHS) and HelpAge, India. These networks unite organizations, including governmental bodies, non-profits, and academic institutions, that are dedicated to enhancing public health [10].
3.2.8. Social Networks for Health
These networks bring together patients, carers, and medical professionals to exchange knowledge, resources, and emotional support for certain medical issues. Social media use in the healthcare industry is on the rise because it provides the public, patients, and healthcare professionals with a forum to discuss health issues with the potential to improve health outcomes. Their functions range from the promotion of health initiatives and patient education to professional networking up until the usage of hospitals, pharmaceutical firms, etc., to reach out to the public and patients, increase visibility, and promote goods and services [11].
3.2.9. Provider Networks
These are networks of healthcare providers, such as doctors, hospitals, and clinics, that have agreed to work together and provide care to patients [12].
3.2.10. Clinical Trial Networks
These are networks of researchers and healthcare providers that conduct clinical trials to test the safety and effectiveness of new treatments and therapies [7].
3.2.11. Shared Healthcare Record Access
Shared healthcare record access has become increasingly important in recent years as providers strive to create a comprehensive, patient-centric approach to care. It enables clinicians to fully understand a patient’s history and records, physician orders, labs, imaging results, medications administered, and past procedures. Through the electronic sharing of data, clinicians can obtain reliable information quickly and securely, allowing for the provision of safe and appropriate care recommendations. Additionally, shared healthcare records can be used to hold patients accountable by automatically reminding them about appointments and interventions, which could help improve their quality of life. Thus, increased access for medical professionals enables more efficient collaboration with higher quality outcomes for patients. Multiple healthcare professionals having concurrent access to a patient’s medical record is referred to as shared record access. This can be especially helpful when several doctors are collaborating to coordinate care for a patient because it enables all providers to stay informed about the patient’s health state and treatment strategy [13].
3.3. Special Network Interaction Terminologies
“Inter-provider communication” is the term used to describe information sharing between healthcare professionals, usually with the goal of coordinating patient care. There are numerous ways to do this, such as through phone conversations, faxes, and electronic health records (EHRs) [1].
The term “interpersonal contacts” describes face-to-face encounters between patients and healthcare professionals. Consultations, rounds, and appointments are a few examples [1,5].
The transfer of a patient’s care from one carer to another is referred to as a “patient handoff”. When a patient is transferred from one hospital unit to another, when they are released from the hospital and go home, or when they are referred to a specialist, this can happen. As they guarantee that patients receive the proper quality of care at each step of their treatment, handoffs are a crucial component of the care process [1,2].
3.4. Networks in Healthcare
To communicate and exchange patient health information, a health network links the healthcare providers, payers, and other relevant stakeholders. By making it simpler for healthcare practitioners to access and share pertinent patient information, a health network seeks to increase the quality and effectiveness of healthcare. Thereby, it may be conceivable to reduce unnecessary testing and treatment, increase patient confidentiality, and deliver better-coordinated care. Electronic health records (EHRs), health information exchanges (HIEs), and other forms of systems and networks are among the technologies that health networks may deploy. Organizations, including government agencies, hospitals, insurance companies, and other stakeholders, may run health networks [5].
3.4.1. Routinely Collected Healthcare Data (RCHD)
Data that is routinely gathered for the purpose of delivering healthcare services is referred to as routinely collected healthcare data (RCHD). This may comprise information on the patient’s background, medical conditions, prescribed treatments, and test outcomes. RCHD is frequently used to monitor the effectiveness and efficacy of healthcare services as well as to spot trends and patterns in the patients’ use of healthcare services. It is a useful tool for enhancing the provision of healthcare and its results and can be used to guide research and policy choices [9].
3.4.2. Hospital Management System (HMS)
A hospital’s administrative and clinical activities are managed by a hospital management system (HMS), which is a computerized or web-based system. An HMS’s objective is to enhance a hospital’s operational effectiveness and efficiency by streamlining and automating numerous activities. Electronic health records (EHRs), appointment scheduling, billing and financial administration, inventory and supply chain management, reporting, and analytics are just a few of the many features and functionalities that an HMS may offer. Different hospital stakeholders, such as administrators, doctors, nurses, and other staff members, may use an HMS [14].
3.4.3. Health Information Network (HIN)
To communicate and exchange patient health information, healthcare providers, payers, and other relevant parties are linked by a system called a health information network (HIN). By making it simpler for healthcare practitioners to access and share pertinent patient information, an HIN aims to increase the quality and efficiency of healthcare. By doing so, it may be possible to decrease unnecessary testing and treatment, increase patient security, and deliver better-coordinated care. Electronic health records (EHRs), health information exchanges (HIEs), and other types of systems and networks are just a few examples of the technology that can be used by an HIN [15].
3.4.4. Electronic Health Records (EHRs)
A network of electronic health records (EHRs) connects healthcare providers and enables the electronic sharing and exchange of patient health data. By facilitating the access and exchange of pertinent patient data, EHR networks can be utilized to raise the standard and effectiveness of healthcare. By doing so, it may be possible to decrease unnecessary testing and treatment, increase patient security, and deliver better-coordinated care. Electronic health records (EHRs), health information exchanges (HIEs), and other types of systems and networks may all be used in EHR networks [16].
3.4.5. Health Information Exchanges (HIEs)
Health Information Exchanges (HIEs) are systems that allow businesses in each area or community to electronically share health-related data. By simplifying the process for healthcare providers to access and share pertinent patient records, an HIE aims to increase the quality, safety, and efficiency of healthcare. Thereby, it may be possible to decrease unnecessary testing and treatment, increase patient security, and deliver better-coordinated care. Electronic health records (EHRs) and clinical data repositories are only a couple of the technologies and standards that HIEs may employ to streamline information transmission. Governmental bodies, healthcare providers, payers, and other stakeholders are just a few of the groups that may support and run HIEs [17].
3.4.6. Institutional Exchange Networks (IES)
Systems or platforms that enable the exchange of products, services, or other resources between organizations or institutions are referred to as institutional exchange networks. These networks may be in the shape of exchanges, clearinghouses, or other intermediaries. They could run through actual sites, the internet, or a mix of both. Stock exchanges, which make it easier to buy and sell stocks and other assets, as well as procurement networks, which aid businesses in locating suppliers for their needs, are a few typical illustrations of institutional exchange networks. Institutional exchange networks can let companies access a greater range of resources and possibilities, which can be crucial in enabling trade and commerce [18].
3.4.7. Patient-Transfer Network (PTN)
A system that aids in the transfer of patients across various healthcare facilities is known as a patient-transfer network. The transportation of patients between hospitals, nursing homes, long-term care facilities, and other types of healthcare facilities can be arranged with the help of these networks. Patient-transfer networks can help ease the burden on individual healthcare facilities by enabling them to transfer patients to other facilities when necessary. They can also help ensure that patients receive the right level of care and treatment based on their needs. These networks may use a variety of modes of transportation, such as ambulances, helicopters, or other vehicles, and may be run by public entities, private businesses, or a combination of both [19].
3.4.8. Patient Information-Sharing Healthcare Networks
Patient information-sharing healthcare networks are platforms that let healthcare professionals from various institutions exchange data and materials pertaining to patient care. These networks can facilitate better patient care coordination and efficiency while giving providers access to a greater range of knowledge and resources. Medical records, diagnostic pictures, and other types of healthcare data can be shared more easily with the help of patient-sharing networks, which can also be used to plan patient transfers between facilities. A wide range of healthcare providers, such as hospitals, primary care clinics, specialized care centers, and others, may be part of these networks, which may be run by government agencies, private businesses, or a combination of both [20].
3.4.9. Network Epidemiology
The study of disease transmission among populations using network analysis techniques is known as network epidemiology. To comprehend the connections and linkages among the people in a population, network analysis uses statistical and mathematical methods. These methods are utilized in network epidemiology to comprehend how diseases spread throughout a community from person to person as well as how various risk factors and interventions may influence the spread of diseases. Network epidemiology can be used to pinpoint disease transmission patterns and create plans to stop the spread of contagious illnesses. It can also be used to comprehend how social and behavioral elements, such as interpersonal relationships and social networks, may affect the spread of disease [21].
The study of how communicable diseases spread across networks of people, such as social networks or contact networks within a community, is known as network epidemiology. In network epidemiology, the network’s nodes stand in for specific individuals, and the edges between them signify some sort of interaction or spread of the disease between those individuals. Researchers can better understand the spread of infectious diseases and develop measures to stop their transmission by looking at the structure and dynamics of these networks. The study of non-communicable diseases, such as chronic ailments that could be influenced by social and behavioral factors, also benefits from the use of network epidemiology [22].
3.4.10. Workplace Interaction Networks
Workplace interaction networks are the channels via which people communicate and interact with one another at work. These networks may consist of both formal lines of communication, such as conferences and emails, as well as informal channels, including exchanges on social media and around the water cooler. Depending on the size and structure of the business, these networks might be of varying sizes and complexities. The interaction network may be more coherent and strongly connected in smaller firms, where people contact more regularly and on a more personal basis. The interaction network may be more dispersed and hierarchical in larger firms, with people interacting more formally and through less personal relationships. The effectiveness and efficiency of workplace interaction networks can be significantly impacted by their dynamics [23].
The organization’s overall efficacy and productivity can be significantly impacted by the dynamics of workplace interaction networks. For instance, a well-functioning interaction network may stimulate collaboration and teamwork, facilitate problem-solving, and facilitate the sharing of ideas and knowledge. A dysfunctional interaction network, on the other hand, might result in misunderstandings, disputes, and a lack of productivity. Therefore, it is crucial that businesses actively manage and promote productive workplace interaction networks [24].
3.4.11. Physician Collaboration Networks (PCNs)
The networks of physicians who collaborate with one another to provide patients with care are known as physician collaboration networks. Networks of healthcare professionals from various specializations or institutions may be included, as well as both formal and informal avenues of communication. By ensuring that patients receive the most appropriate and well-coordinated treatment possible, physician collaboration networks seek to improve patient outcomes and satisfaction. These networks can assist with the spreading of medical knowledge and skills, which helps cut down on pointless treatments and tests. Professional networks are a type of PNC, such as the American Medical Association or the American Nurses Association, as they unite healthcare experts in a specific field or expertise [25].
Physician Collaboration networks can be set up in a variety of ways, including through trade associations or electronic medical record systems. When patients have chronic or complex medical illnesses that call for the advice of various doctors, these networks can be especially helpful. To deliver high-quality healthcare, effective physician collaboration networks are necessary. These networks can also help to lower costs, improve patient outcomes, and to provide their patients with the best treatment possible; healthcare companies must establish and maintain these partnership networks [26,27].
3.4.12. Comorbidity Networks
The links between various clinical situations, such as diseases or disorders in a population, are depicted in clinical co-occurrence networks, which are graphs. These networks are utilized to comprehend comorbidity patterns or the coexistence of several chronic illnesses in a single person. Researchers can find common comorbidity patterns and probable risk factors for the emergence of certain illnesses by examining clinical co-occurrence networks. By using this knowledge, comorbid illnesses can be better managed and treated, and preventative measures can be created. Using information from electronic health records claims data, or other clinical data sources, clinical co-occurrence networks can be built. The intricacy of comorbidities and their possible effects on health outcomes can be understood via these networks. They can also be used to spot common comorbidity trends and prospective treatments for better managing several chronic illnesses [28].
3.4.13. Limitations and Challenges Associated with Different Healthcare Networks
Healthcare networks also have several limitations and weaknesses associated with them as enlisted in Figure 3. Healthcare organizations, technology providers, and regulatory organizations must work together to address these issues. They are elucidated as the following list:
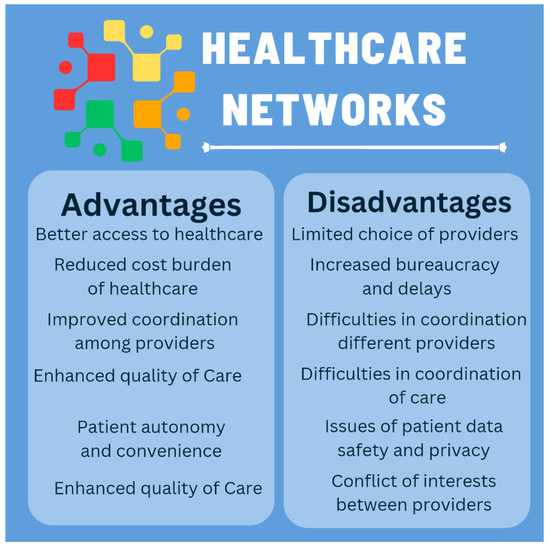
Figure 3.
Insights into the advantage and disadvantages of healthcare networks.
- Security: Healthcare networks are required to protect patient information in order to abide by laws such as HIPAA. Healthcare networks are a popular target for fraudsters, making it challenging to guarantee the network’s security.
- Interoperability: Electronic health records (EHRs), medical equipment, and administrative systems are only a few of the many systems that make up healthcare networks. Since these systems frequently employ several data formats and protocols, sharing data between them can be difficult.
- Cost: Healthcare networks need a large investment in hardware, software, and infrastructure. Smaller healthcare companies may find it difficult to pay to maintain a modern network due to the cost of upgrades and maintenance.
- Scalability: As medical technology evolves, healthcare networks must be able to handle the growing data volumes. Scalability is essential to ensuring that medical professionals have timely access to patient data when they need it.
- Accessibility: Patients must have access to their test findings and medical records, but healthcare networks must make sure that only those with the proper authorization can access this data. It might be difficult to provide patients with access to their data while upholding security and privacy.
- Compliance: Healthcare networks are required to adhere to legal regulations, such as HIPAA and be able to prove that they are doing so. This might be difficult, especially for smaller healthcare groups with limited resources.
- Data analytics: Healthcare networks produce enormous volumes of data, yet it can be difficult to glean insights from this data. Organizations in the healthcare industry must be equipped with the right knowledge and skills to examine this data successfully [29].
4. Case Studies on Healthcare Networks
The following are some case studies in actual healthcare networks that operate, scale, and deliver services to millions of people worldwide.
4.1. Case Studies on Indian Healthcare Networks
4.1.1. Apollo Hospitals in India
One of the biggest private healthcare networks in India is Apollo Hospitals. Dr. Prathap C. Reddy created it in 1983, and since then, it has grown to include more than 70 hospitals and clinics in India and other nations. With a strong emphasis on technical innovation, Apollo Hospitals has adopted a variety of cutting-edge medical techniques and technology in order to offer patients top-notch care.
4.1.2. Manipal Hospitals in India
Established in 1953, Manipal Hospitals is a chain of medical facilities. With more than 20 hospitals and clinics spread out across the nation, it has subsequently expanded to become one of India’s largest healthcare networks. In addition to having a strong focus on research and innovation, Manipal Hospitals is renowned for its competence in fields including cardiology, oncology, and orthopedics [30].
4.1.3. National Rural Health Mission (NRHM) in India
The National Rural Health Mission (NRHM) is a flagship initiative of the Indian government with the goal of enhancing the provision of healthcare in rural areas. It was introduced in 2005 and has since been adopted by all of India’s states and union territories. The program’s main objectives are to improve the healthcare system’s infrastructure, deliver high-quality treatment, and encourage community involvement in healthcare. In several states, NRHM has been successful in lowering maternal and infant mortality rates [30].
4.1.4. Ayushman Bharat Scheme in India
The Indian government introduced the Ayushman Bharat healthcare program in 2018. The program intends to give 500 million individuals, primarily from the poor parts of society, access to free healthcare services. Ayushman Bharat offers financial protection against hospitalization costs and has a component for preventive healthcare. The program has been effective in enhancing disadvantaged people’s access to healthcare services.
4.1.5. Rashtriya Swasthya Bima Yojana (RSBY) in India [30]
The Indian government introduced the RSBY health insurance program in 2008. Families who are below the poverty level can take advantage of the program’s health insurance coverage. RSBY seeks to increase accessibility to high-quality healthcare services while offering financial security against catastrophic medical costs. The program has been effective in lowering out-of-pocket medical expenses for low-income families [30,31].
4.1.6. National Health Stack (NHS)
The National Health Stack (NHS) is a digital infrastructure project that the Indian government launched to increase the efficiency of healthcare delivery [31]. It attempts to develop a common architecture for health information that will allow communication between various healthcare systems. By eliminating duplication and improving data exchange, the NHS is intended to increase the effectiveness of healthcare delivery and save healthcare costs [32].
4.2. Case Studies on North American Healthcare Networks
4.2.1. Healthcare Network in the US
Rochester, a Minnesota-based Mayo Clinic, is a non-profit hospital and medical research organization. Arizona, Florida, Minnesota, and Wisconsin all have hospitals, clinics, and research facilities that are a part of the Mayo Clinic network. More than 1.3 million people receive care from the organization’s medical practice each year, and its research division carries out ground-breaking research in areas including cardiology, neurology, and cancer [33,34].
4.2.2. Cleveland Clinic Healthcare Network in the US
Cleveland Clinic is an Ohio-based, non-profit academic medical center. Ohio, Florida, Nevada, Canada, and the United Arab Emirates are among the locations where the Cleveland Clinic network has hospitals, clinics, and research facilities [32]. More than 5 million people receive care from the organization’s medical practice each year, and its research division carries out ground-breaking studies in specialties such as immunology, neurology, and cardiology [35,36].
5. Conclusions
The implementation of a responsive and sustainable healthcare network is essential for the success of any healthcare service. These healthcare networks serve as an example of how crucial it is to give common people access to high-quality care. They are all committed to enhancing the health of their communities and have all adopted cutting-edge methods of providing healthcare services.
Healthcare networks come in a variety of forms, each with its own advantages and disadvantages. For instance, a hospital network consists of several hospitals that cooperate to offer patients in various regions specialized care. On the other hand, a physician network entails a team of medical professionals who pool their resources, knowledge, and patients to improve the standard of care. Health information exchanges make it easier for healthcare providers to share patient data, and accountable care organizations, which prioritize improving patient outcomes while cutting costs, are two other forms of healthcare networks. Healthcare networks can strengthen technology and infrastructure, increase access to treatment, reduce costs, enhance patient care, improve employee retention and recruitment, as well as boost negotiating power.
The ultimate objective of these networks is to advance improved patient care by developing a healthcare system that is more effective, collaborative, and patient friendly. By coordinating care and eliminating service duplication, healthcare networks can also aid in lowering healthcare expenditures.
Healthcare networks, however, may potentially have certain disadvantages. These might restrict the range of physicians that patients can choose to see, which is one possible drawback. Patients might be forced to only see specialists in the network. Additionally, because patients may see several clinicians within the network who are unfamiliar with their unique health history and needs, healthcare networks might not always be able to offer the same level of individualized treatment as individual providers.
Healthcare networks promote the implementation and standardization of best practices guidelines in patient care, increasing the interaction between patients and physicians, physicians and support staff including pharmacists, physiotherapists, and nurses, and provide ample opportunities for the improvement of patient care, enhancing vaccination drive in communities, the implementation of clinical trials, support research, sharing of resources, enhanced supply cum logistics, and the surveillance and prevention of diseases. In addition, collaboration via networks has a positive impact on the overall economics of healthcare systems.
Author Contributions
Conceptualization, S.K.R.; methodology, S.K.R. and R.S.I.; software, S.K.R.; validation, S.K.R. and R.S.I.; formal analysis, S.K.R. and R.S.I.; investigation, S.K.R. and R.S.I.; resources, S.K.R. and R.S.I.; data curation, S.K.R. and R.S.I.; writing—original draft preparation, S.K.R. and R.S.I.; writing—review and editing, S.K.R. and R.S.I.; visualization, S.K.R. and R.S.I.; supervision, S.K.R. and R.S.I.; project administration, S.K.R. and R.S.I.; funding acquisition, S.K.R. and R.S.I. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
Available at corresponding authors Figshare.com repository.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Anderson-Wallace, M. Networks in Healthcare-Managing Complex Relationships; Emerald Group Publishing Limit: Bingley, UK, 2016. [Google Scholar]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Hoboken, NJ, USA, 2019. [Google Scholar]
- McKenzie, M.J.; Bossuyt, J.E.; Boutron, P.M.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; Chou, R.; Glanville, J.; et al. The PRISMA 2020 statement: An Updated Guideline for Reporting Systematic Reviews. Br. Med. J. 2021, 372, n71. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred Reporting Items for Systematic Review and meta-analysis Protocols (PRISMA-P) 2015 Statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [PubMed]
- Weil, T.P. Health Networks: Can They Be the Solution? University of Michigan Press: Ann Arbor, MI, USA, 2001. [Google Scholar]
- Irasiak, A.; Sroka, E.; Górka, W.; Socha, M.; Piasecki, A. Deaf-friendly research—Conducting research using an electronic questionnaire. E-Mentor 2021, 92, 4–15. [Google Scholar] [CrossRef]
- An, C.; O’Malley, A.J.; Rockmore, D.N.; Stock, C.D. Analysis of the U.S. patient referral network. Stat. Med. 2017, 37, 847–866. [Google Scholar] [CrossRef]
- Chae, S. Benefits of Network Health Insurance with Primary Care. SSRN Electron. J. 2018, 5, 21–23. [Google Scholar] [CrossRef]
- Brunson, J.C.; Laubenbacher, R.C. Applications of network analysis to routinely collected health care data: A systematic review. J. Am. Med. Inform. Assoc. 2017, 25, 210–221. [Google Scholar] [CrossRef]
- Rajamani, S.K.; Naik, S. New Technology Trends in the Teaching of the Art of Otolaryngological Surgery. In Technology Trends in Higher Education; A2Z EduLearningHub LLP: Calicut, India, 2020; Volume 1, pp. 30–34. [Google Scholar]
- Valente, T.W. Social Networks and Health; Oxford University Press: Oxford, UK, 2010. [Google Scholar]
- Miller, D.W.; McWilliams, T.R.; Ansel, T.C. Employed Physician Networks: A Guide to Building Strategic Advantage, Value, and Financial Sustainability; Health Administration Press: Chicago, IL, USA, 2019. [Google Scholar]
- Wickramasinghe, N.; Bali, R.K.; Tatnall, A. Using actor network theory to understand network centric healthcare operations. Int. J. Electron. Healthc. 2007, 3, 317. [Google Scholar] [CrossRef]
- Yan, J.; Zhong, X.; Yan, W. Analysis on Two Basic Issues of Modern Hospital Management System. Mod. Manag. Forum 2018, 2. [Google Scholar] [CrossRef]
- Rabiei, R.; Aasdi, F.; Moghaddasi, H.; Shojaei Baghini, M. A Model for the National Mental Health Information Network. Appl. Health Inf. Technol. 2021. [Google Scholar] [CrossRef]
- Victores, A.J.; Coggins, K.; Takashima, M. Electronic health records and resident workflow: A time-motion study of otolaryngology residents. Laryngoscope 2014, 125, 594–598. [Google Scholar] [CrossRef]
- Mohammadpour, A. Iran’s National Health Information Network: Developing an Architectural Model. Appl. Health Inf. Technol. 2021, 1, 52–55. [Google Scholar] [CrossRef]
- Wang, Y. A Network-Exchange Approach to Corruption: Brokers and Institution Spanning in a Chinese Corruption Network. Deviant Behav. 2019, 4, 1636–1649. [Google Scholar] [CrossRef]
- Cruz-Cunha, M.M.; Miranda, I.M.; Goncalves, P. Handbook of Research on ICTs and Management Systems for Improving Efficiency in Healthcare and Social Care; Medical Information Science Reference: Hershey, PA, USA, 2013. [Google Scholar]
- O’Sullivan, D.; Fraccaro, P.; Carson, E.; Weller, P. Decision time for clinical decision support systems. Clin. Med. 2014, 14, 338–341. [Google Scholar] [CrossRef]
- Rajamani, S.K.; Iyer, R.S. Development of an Android Mobile Phone Application for Finding Closed-Loop, Analytical Solutions to Dense Linear, Algebraic Equations for The Purpose of Mathematical Modelling in Healthcare and Neuroscience Research. NeuroQuantology 2022, 20, 4959–4973. [Google Scholar]
- Morris, M. Network Epidemiology; OUP Oxford: Oxford, UK, 2004. [Google Scholar]
- Shepherd, H. Organizational practices and workplace relationships in precarious work: New survey evidence. Soc. Netw. 2021, in press. [Google Scholar] [CrossRef]
- Farrell, L. Workplace education and corporate control in global networks of interaction. J. Educ. Work 2004, 17, 479–493. [Google Scholar] [CrossRef]
- Uddin, S.; Hossain, L.; Kelaher, M. Effect of physician collaboration network on hospitalization cost and readmission rate. Eur. J. Public Health 2011, 22, 629–633. [Google Scholar] [CrossRef]
- Hardwick, P.J. Families and the professional network: An attempted classification of professional network actions which can hinder change. J. Fam. Ther. 1991, 13, 187–205. [Google Scholar] [CrossRef]
- Kapoor, B.; Kleinbart, M. Building an Integrated Patient Information System for a Healthcare Network. J. Cases Inf. Technol. 2012, 14, 27–41. [Google Scholar] [CrossRef]
- Brunson, J.C.; Agresta, T.P.; Laubenbacher, R.C. Sensitivity of comorbidity network analysis. JAMIA Open 2019, 3, 94–103. [Google Scholar] [CrossRef]
- Zhang, Y.; Yu, L.; Wang, L. High Access Performance Strategy for next Generation Healthcare Networks. J. Netw. 2014, 9, 1477–1484. [Google Scholar] [CrossRef]
- Kumar, P. Impact of COVID-19 Pandemic Era 2020 on Rashtriya Bal Swasthya Karyakram (RBSK)—National Child Health Program in India—A Cross-Sectional Comparative Research Study. Public Health Open Access 2022, 6, 1–18. [Google Scholar] [CrossRef]
- Astakhov, V. Biomedical Informatics; Humana Press: New York, NY, USA, 2009; ISBN 9781934115633. [Google Scholar]
- Pevzner, P.A. Educating Biologists in the 21st Century: Bioinformatics Scientists versus Bioinformatics Technicians. Bioinformatics 2004, 20, 2159–2161. [Google Scholar] [CrossRef] [PubMed]
- Divya, R. Transgender Healthcare in Medical Curriculum. Madr. J. Case Rep. Stud. 2021, 5, 180–181. [Google Scholar] [CrossRef]
- Domingo, M.C. Managing Healthcare through Social Networks. Computer 2010, 43, 20–25. [Google Scholar] [CrossRef]
- An, W.; Doan, L. Health Surveillance through Social Networks. Soc. Netw. 2015, 42, 8–17. [Google Scholar] [CrossRef]
- Supplemental Material for Social Networks and Neural Receptivity to Persuasive Health Messages. Health Psychol. 2021, 3, 2–5. [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).