Abstract
Background: Arthrodesis of the first metatarsophalangeal joint (MTP1) is a common intervention for hallux rigidus (HR). The procedure eliminates MTP1 motion but results in significant pain relief and high satisfaction rates, although MTP1 is eliminated. Less evidence is available regarding the effects on gait and the presence of compensatory mechanisms. The aim of this study is to investigate the effects of MTP1 arthrodesis on gait and patient-reported outcome measures (PROMs) compared with preoperative functioning and healthy individuals. Methods: In this prospective study, 10 patients (10 feet) with HR who underwent MTP1 arthrodesis were evaluated before and after surgery and compared with 15 healthy controls (30 feet). Gait analysis was performed with a motion capturing system using the multi-segment Oxford foot model. Spatiotemporal parameters and kinematics were quantitatively analyzed. PROMs were evaluated using validated questionnaires including the American Orthopedic Foot and Ankle Society Hallux Metatarsophalangeal-Interphalangeal (AOFAS-HMI) scale, the Numeric Pain Rating Scale (NPRS), and the Manchester–Oxford Foot Questionnaire (MOXFQ). Results: MTP1 joint motion was reduced in HR and further reduced after MTP1 arthrodesis compared with healthy controls. Furthermore, intersegmental ROM analysis revealed increased forefoot frontal plane motion (pronation and supination) in HR compared with healthy controls. This was also observed after MTP1 arthrodesis, while additionally increased frontal plane motion in the hindfoot (inversion and eversion) was observed compared with HR and healthy controls. PROM evaluation revealed improved AOFAS-HMI (from 55.7 to 79.1 points, p = 0.002) and NPRS (from 5.7 to 1.5 points, p = 0.004) scores after surgery. Additionally, improvements in the MOXFQ score (from 51.0 to 20.0 points, p = 0.002) were observed. Conclusions: Due to the loss of sagittal hallux motion, foot and ankle kinematics are changed in HR patients and after MTP1 arthrodesis compared with healthy controls. Loss of MTP1 motion results in increased frontal plane motion of the forefoot in HR, and increased frontal plane motion of the fore- and hindfoot after MTP1 arthrodesis. Additionally, substantial improvements in PROMs were recorded after surgery.
1. Introduction
Hallux rigidus (HR) is a degenerative condition of the first metatarsophalangeal joint (MTP1). It is the most common foot joint to be affected by osteoarthritis (OA), which progresses during aging [1,2]. Surgical interventions are indicated when conservative treatments fail [2,3]. Arthrodesis is currently the golden standard treatment for moderate to severe HR [1,3,4,5]. It sacrifices motion but results in significant pain relief and high satisfaction rates at short-, mid-, and long-term follow-up [1,3,6,7]. Due to rigid fixation of MTP1, hallux motion is absent, leading to gait alterations and a different pattern of foot loading [3,8,9,10,11].
Pedobarographic studies on subjects with HR have elucidated reduced loading of the hallux and increased loading of the lateral plantar foot zones and lesser metatarsal heads (i.e., fourth and fifth) in patients with HR, who are also described as ‘lateral loaders’ [10,12,13,14]. Evaluation of foot and ankle kinematics exposed reduced dorsiflexion and plantar flexion in the hallux range of motion (ROM), which is compensated via frontal plane motion through increased forefoot pronation and supination [15,16]. This altered gait pattern and weight shift to the lateral side of the foot is considered a compensatory mechanism for the limited ROM and avoidance of engaging the painful MTP1 during gait.
Limited knowledge exists regarding foot compensation after surgical interventions for HR. Some studies, with a certain degree of heterogeneity, have addressed gait changes after MTP1 arthrodesis [3,8,9,10,17]. These studies have reported altered spatiotemporal parameters, such as a decreased step length [9] and step width [8,10], while others have been unable to observe these effects [17,18]. No changes in hip, knee, and especially ankle kinematics have been observed after MTP1 arthrodesis [3,8,9,10]. However, only two cross-sectional studies have analyzed foot and ankle kinematics after MTP1 arthrodesis by using a multi-segment foot model [10,18]; they reported a decreased hindfoot eversion during midstance followed by increased forefoot supination during pre-swing [10,18]. The use of multi-segment foot models is encouraged due to the potential to study motion patterns in multiple foot and ankle joints, which is especially relevant for HR, since it is supposed that kinematic changes imposed by HR are compensated in the foot. A better insight into this compensatory mechanism is relevant in preoperative planning and selecting the optimal intervention for a patient.
The aim of this study is to explore the effects of HR and subsequent treatment with MTP1 arthrodesis on foot and ankle kinematics. Pre- and postoperative kinematics are compared with healthy individuals. It is hypothesized that the forefoot compensates (more pronation and supination) for the loss of hallux motion in subjects with HR and after MTP1 arthrodesis. Additionally, it is expected that patient satisfaction will increase after MTP1 arthrodesis, as well as pain and daily activity limitations declining, compared with the preoperative state, which is studied by using patient-reported outcome measures (PROMs).
2. Methods
2.1. Study Population
This prospective longitudinal study was conducted at the human movement sciences laboratory of our institution. Eligible patients were diagnosed with unilateral symptomatic and radiologically confirmed MTP1 OA, who did not respond to conservative interventions and were willing to undergo MTP1 arthrodesis. Patients with inflammatory joint diseases, bilateral HR, neurological disorders that influence gait, or previously performed surgical interventions to the lower extremities (e.g., hip, knee, or foot) were excluded. Exclusion criteria were identical for healthy controls, although this group was free of lower extremity pathologies. Patients were invited to our laboratory before surgery and at least 9 months after surgery. This study was performed according to the Declaration of Helsinki (2013), and the local medical ethical committee approved this study. All study subjects provided their written informed consent.
2.2. Operative Technique
All surgical procedures were performed by two experienced surgeons. A Hallu-FIX Integra plate (Integra Life Sciences, Plainsboro, NJ, USA) was used to achieve fixation between the first metatarsal and the proximal phalanx. Patients were restricted from weight-bearing activities on the affected foot for the first month after surgery and wore a stiff-soled shoe postoperatively for two months. One patient underwent revision surgery due to nonunion.
2.3. Motion Analysis
A VICON motion capture setup (Vicon Motion Systems, Oxford, England, UK) consisting of 12 infrared cameras (eight MX3 and four T20 cameras with sampling at 200 Hz) were placed beside a 10 m runway equipped with a force plate (AMTI OR6 Series, Advanced Mechanical Technology Inc., Watertown, NY, USA). According to the Oxford foot model (OFM) guidelines, markers were placed on bony landmarks on both lower extremities [19,20]. Before gait analysis, height, weight, leg length (distance between the anterior iliac spine and medial malleolus), and knee and ankle width (distance between lateral and medial condyles of the knee, and distance between lateral and medial malleoli of the ankle) were measured and used for running the OFM. Thereafter, a static trial in a standing neutral anatomical position was performed. Markers were calibrated and subject-specific joint axes were calculated with this static trial. Subsequently, six markers were removed and dynamic measurements were gained. Subjects were asked to walk barefoot at a self-selected speed. After some practice trials, subjects were asked to walk until at least 15 proper recordings were obtained.
2.4. Data Analysis
VICON Nexus 2.8.1 software was used to trace and label the markers. Subsequently, kinematic data was processed with MATLAB version R2012A (The Mathworks Inc., Natick, MA, USA). Spatiotemporal parameters including gait speed, step width, step length, and stance time were determined. Kinematic waveforms were produced from sagittal plane motions (flexion and extension) of the hallux/forefoot, forefoot/hindfoot, and hindfoot/tibia, as well as frontal plane motions of the forefoot/hindfoot (pronation and supination) and hindfoot/tibia (inversion and eversion). Data was analyzed as one stride (i.e., heel strike to heel strike of the same foot, traced using the force plate forces). For description in this paper of events occurring during the gait cycle, the gait cycle was divided into stance (0–62%) and swing phases (63–100%). Stance was divided into the following phases: loading response (0–12%), midstance (13–31%), terminal stance (32–50%), and pre-swing (51–62%). Swing was divided into initial swing (63–75%), mid-swing (76–87%), and terminal swing (88–100%) [21]. Offset correction was performed for the intersegmental kinematic waveforms by summing the intersegmental angles at each time point (0–100%) and subsequently dividing the sum by 100. ROM during the push-off phase was calculated in each of the planes and was defined as the difference between maximal and minimal intersegmental angles in the 45–65% time interval of the gait cycle.
2.5. Clinical Assessment
PROMs were recorded before and after surgery by using the American Orthopedic Foot and Ankle Society Hallux Metatarsophalangeal-Interphalangeal (AOFAS-HMI) scale, the Manchester–Oxford Foot Questionnaire (MOXFQ) score, and the Numeric Pain Rating Scale (NPRS). The AOFAS-HMI offers scores for pain, function, and alignment. Scores range between 0 and 100 points, with higher scores indicating better outcomes [22]. After arthrodesis, the maximum achievable score is 90, since 10 points are awarded to MTP1 motion, which is eliminated during surgery [23]. The MOXFQ is divided into three subscales: walking and standing problems, foot pain, and issues related to social interactions. Scores range from 0 to 100, where 100 represents the poorest outcome [24,25,26]. The pain experience was assessed with the NPRS, which ranges from 0 to 10, where 10 reflects severest pain [27].
2.6. Radiographic Evaluation
Radiological assessments were performed, and Regnauld’s radiographic classification was used to grade degenerative MTP1 changes preoperatively [28]. The dorsiflexion fusion angle (DFA) was measured with the postoperative radiographs [29].
2.7. Statistical Analysis
Statistical analyses were conducted in GraphPad Prism 8.3 (GraphPad Software, Inc., San Diego, CA, USA). Patient characteristics were compared by using the Mann–Whitney U test. Spatiotemporal parameters and intersegmental ROM in the push-off phase were statistically tested with the Wilcoxon signed rank test (pre- vs. postoperative) and Mann–Whitney U test (HR vs. healthy controls). Pre- and postoperative PROMs were compared with the Wilcoxon signed rank test. Kinematic data was tested using statistical parametric mapping (SPM; version M.0.4.5), which can detect differences at any time point of the gait cycle (0–100%) [30]. An SPM paired t-test was used to compare pre- and postoperative measurements in HR subjects, and an SPM unpaired t-test was used to compare subjects with HR and healthy controls and to compare subjects treated with MTP1 arthrodesis to healthy controls. A p-value ≤ 0.05 was considered statistically significant.
3. Results
3.1. Patient Demographics
In total, 10 patients with HR (10 feet) and 15 healthy controls (30 feet) were available for evaluation. Patients with HR were evaluated prior to surgery and after a mean follow-up duration of 20 months post-MTP1 arthrodesis (range: 10–29 months). Baseline patient demographics demonstrated a significant lower height (p = 0.04) and a higher number of females in the HR group (Table 1). Before surgery, seven patients suffered from HR Grade II and three patients from HR Grade III according to the Regnauld grading system (Table 2). MTP1 arthrodesis resulted in a mean DFA of 25.0°, and MTP1 consolidation was observed in all patients.

Table 1.
Patient demographics a.

Table 2.
Spatiotemporal parameters a.
3.2. Spatiotemporal Parameters
No statistically significant differences were observed in spatiotemporal parameters before and after surgery (Table 2). HR step length was significantly shorter preoperatively compared with healthy controls (0.56 m vs. 0.64 m, respectively; p < 0.002), while HR step width was significantly smaller postoperatively compared with healthy controls (0.10 m vs. 0.13 m, respectively; p = 0.05) (Table 2).
3.3. Foot and Ankle Kinematics
Reduced dorsiflexion in the hallux/forefoot segment was observed in subjects with HR during pre-swing before (p = 0.039) and after surgery (p = 0.049) compared with healthy controls (Figure 1A). Sagittal ROM (dorsiflexion and plantar flexion) during push-off in the hallux/forefoot segment was significantly lower prior to surgery (15.9° vs. 22.8°, respectively; p = 0.02) and after MTP1 arthrodesis (14.4° vs. 22.8°, respectively; p = 0.02) compared with healthy controls (Figure 2A). No difference was detected in sagittal ROM during push-off in the hallux/forefoot segment before and after MTP1 arthrodesis (p = 0.91, Figure 2A).
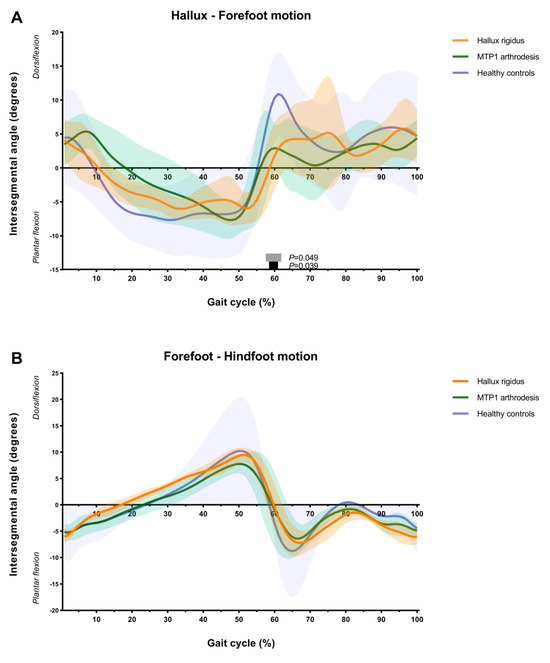
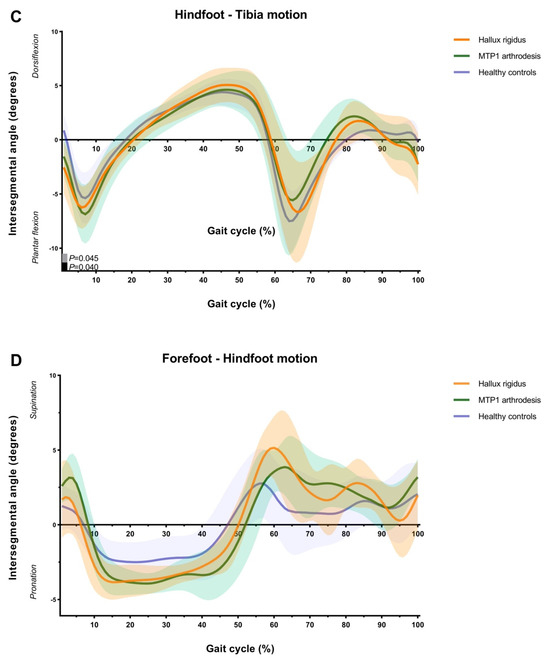
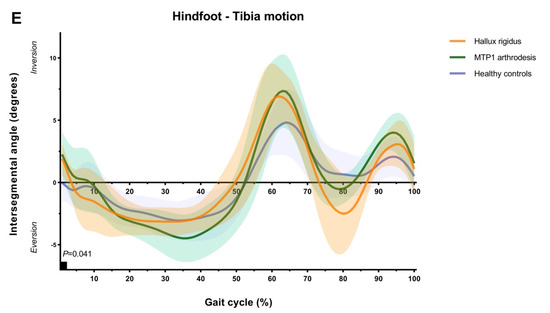
Figure 1.
This collection of figures presents average absolute joint angles of one stride during gait in the HR group, the MTP1 arthrodesis group, and healthy controls. Motion in the sagittal plane for the hallux/forefoot, forefoot/hindfoot, and hindfoot/tibia ((A), (B), (C), respectively) and in the frontal plane for the forefoot/hindfoot and hindfoot/tibia ((D), (E), respectively). Mean values (dark lines) are accompanied by their standard deviations (transparent areas). Results of the SPM analyses are displayed on the x-axis. Statistically significant differences (p ≤ 0.05) are indicated in black (HR vs. healthy controls) or gray (MTP1 arthrodesis vs. healthy controls). No statistically significant differences were detected between the HR and MTP1 arthrodesis groups.
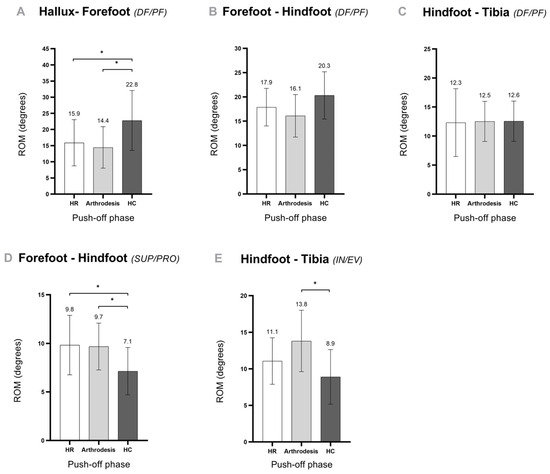
Figure 2.
These five figures present intersegmental ROM during push-off in the sagittal plane (A–C) and frontal plane (D,E) in the different foot segments. Results are before surgery (HR), after MTP1 arthrodesis (arthrodesis), and healthy controls (HC). Data are presented as means with standard deviations. * A p-value ≤ 0.05 is considered a statistically significant difference. Abbreviations: PF—plantar flexion; SUP—supination; PRO—pronation; IN—inversion; EV—eversion.
Sagittal forefoot and hindfoot motion (dorsiflexion and plantar flexion) were comparable in the three studied groups (Figure 1B,C). Only increased plantar flexion was observed in subjects with HR and MTP1 compared with healthy controls (p = 0.045 and p = 0.04, respectively; Figure 1C) during loading response in the hindfoot/tibia segment. Furthermore, no differences in sagittal ROM (dorsiflexion and plantar flexion) during push-off in the forefoot and hindfoot were seen between the studied groups (Figure 2B,C).
In the frontal plane, increased forefoot motion (pronation and supination) was seen during push-off in the HR group compared with healthy controls (9.8° vs. 7.1°, respectively; p = 0.04, Figure 2D) and in the MTP1 arthrodesis group compared with healthy controls (9.7° vs. 7.1°, respectively; p = 0.02, Figure 2D). These differences in frontal plane forefoot motion were not seen after analyzing the kinematic data with SPM (Figure 1D).
Furthermore, increased frontal plane hindfoot motion (inversion and eversion) was seen during push-off after MTP1 arthrodesis compared with healthy controls (13.8° vs. 8.9°, respectively; p = 0.009, Figure 2E). This finding was not seen after analyzing the data with SPM (Figure 1E), although increased inversion of the hindfoot was seen after MTP1 arthrodesis compared with healthy controls in loading response (p = 0.041, Figure 1E).
3.4. PROMs
AOFAS-HMI scores increased significantly from 55.7 points prior to surgery to 79.1 points after surgery (p = 0.002). Additionally, NPRS scores significantly decreased from 5.7 points prior to surgery to 1.5 points after surgery (p = 0.004). MOXFQ index scores improved from 51.0 points before surgery to 20.0 points after surgery (p = 0.002). Furthermore, significant improvements in all subdomains of the MOXFQ were observed (Table 3).

Table 3.
Clinical outcome measures and PROMs prior to surgery (HR) and after surgery (MTP1 arthrodesis) a.
4. Discussion
The aim of this prospective study is to determine the effects of MTP1 arthrodesis on foot and ankle kinematics, as well as on PROMs, compared with patients’ preoperative state and healthy controls. As hypothesized, after MTP1 arthrodesis, dorsiflexion in the hallux/forefoot segment was reduced during pre-swing; accordingly, intersegmental ROM analysis confirmed the decreased ROM during push-off in the hallux/forefoot segment compared with healthy controls. Loss of MTP1 motion after MTP1 arthrodesis is compensated in the forefoot and hindfoot via increased frontal plane motion during push-off compared with healthy controls. Increased frontal plane motion (pronation and supination) in the forefoot during push-off was also seen in subjects with HR, although hindfoot motion (inversion and eversion) was not affected. Subjects reported significant pain reduction and fewer limitations in standing and walking after MTP1 arthrodesis. Additionally, improvements in participating in daily and social activities were seen.
This prospective comparative study is one of the first studies evaluating effects of MTP1 arthrodesis on foot and ankle kinematics and PROMs before and after surgery. The number of quantitative kinematic studies in which studies evaluate gait after MTP1 arthrodesis is limited [3,8,9,10,17]. Previous studies used a foot model where the foot was analyzed as single rigid body, wherein sagittal ankle kinematics was analyzed [3,8,9]. In the present study, no significant changes in ankle ROM during gait before and after MTP1 arthrodesis were observed, which was in accordance with the literature [3,8,9]. Two cross-sectional studies have used multi-segment foot models and have observed similar foot compensation after MTP1 arthrodesis [10,18]. In the present study, reduced dorsiflexion in the hallux/forefoot segment during stance (0–62% of the gait cycle) and increased frontal plane motions (pronation and supination) in the forefoot after MTP1 arthrodesis compared with healthy controls was observed. This has also been observed in the previous studies [10,18]. Increased hindfoot inversion and eversion during stance has not been observed by previous studies [10,18]. However, the present study determined that this compensation occurred during push-off. This part of the gait cycle has not been analyzed by previous studies [10,18]. Additionally, some significant differences during loading response were observed in the sagittal plane of the hindfoot/tibia and in the frontal plane of the hindfoot/tibia. However, since these differences were small, it was concluded that they were not clinically relevant.
Previous gait studies have reported differences in spatiotemporal parameters after MTP1 arthrodesis. One study has reported decreased step length [9], and two studies have reported a decreased step width [8,10]; others have not observed these effects [17,18]. In the presented study, a decreased step width was also observed after MTP1 arthrodesis, which is in accordance with previous published studies [8,10]. Brodsky et al. suggested that a decrease in step width indicates a narrower base of support during gait, which is interpreted as increased stability during this activity [8]. Stevens et al. suggested that the decrease in step width was an effect of the inclusion of more women in their MTP1 arthrodesis group, since it is known that step width is smaller in women [10]. We agree with both suggestions; also, in our study, more women were included in our intervention group. Based on the present results, it is additionally suggested that step width narrows after MTP1 arthrodesis due to the observed compensation mechanism of increased frontal plane motion in the forefoot (pronation and supination) and hindfoot (inversion and eversion). It is suggested that these foot motions could be easier to perform and require less effort when feet are positioned in a narrower base. Furthermore, step length was significantly shorter in HR compared with healthy controls. This was also observed in one previous study, while it was not further discussed [9]. It is suggested that this will be an effect of the lower gait speed, since step length is directly related to gait speed [31,32]. This trend was also observed in the present study; step length will be greater when gait speed increases (Table 2). Finally, in the present study, healthy controls were taller than patients of the intervention groups, which could also lead to an increased step length [31].
This study demonstrates that foot motion is changed in HR and after MTP1 arthrodesis compared with healthy controls. Intersegmental foot motion is partly comparable in HR and after subsequent MTP1 arthrodesis. In HR, frontal plane motion (pronation and supination) in the forefoot increases due to reduced MTP1 motion. After MTP1 arthrodesis, increased frontal plane motion in the forefoot is also observed, while increased hindfoot motion in the frontal plane (inversion and eversion) is detected, which is not seen in HR. It is suggested that frontal plane motion in the forefoot increases due to the severely affected MTP1 joint in subjects with HR, causing pain and mechanical impingement, which limits MTP1 joint motion. These factors lead to the avoidance of loading and toeing-off over the MTP1 joint during push-off, which is compensated by an increased frontal plane motion of the forefoot [33]. After surgery, MTP1 joint motion is further lost due to fusion of the MTP1 joint. Therefore, toeing-off over the MTP1 joint is further reduced and other joints need to compensate for the loss of hallux motion. Due to further loss of MTP1 joint motion after MTP1 arthrodesis, the hindfoot is also compensating in frontal plane motions besides the forefoot. Therefore, frontal plane motions in the forefoot and hindfoot seem to be essential to compensate for the loss of motion of the MTP1 joint.
The long-term effects of this compensatory mechanism, as well as the development of additional foot and ankle complaints or pathologies in other foot joints, remain unclear and need further investigation through future long-term follow-up studies. Nevertheless, a significant impact on the emergence of new foot and ankle complaints is not expected, as existing long-term clinical follow-up data after MTP1 arthrodesis demonstrate minimal pain (VAS 0.66) and high levels of patient satisfaction (AOFAS 91 points, MOXFQ 19.6 points) after 22 years of follow-up [7]. These findings suggest that the compensatory mechanism is unlikely to contribute to the development of new foot and ankle issues. However, based on the current study results and the available evidence, no definitive recommendations can yet be made regarding revalidation and rehabilitation protocols following MTP1 arthrodesis. Further studies are needed to confirm these findings and to specifically assess the long-term effects and potential emergence of new foot and ankle complaints resulting from this compensatory mechanism.
Surgery results in a significant reduction in patient-reported complaints and improvements in patient-reported satisfaction. The use of several PROMs (AOFAS-HMI, NPRS, and MOXFQ) indicate that, after MTP1 arthrodesis, pain is significantly reduced and patients report fewer limitations in standing and walking; additionally, participation is improved in daily and social activities. The observed clinical improvements align with findings from previously published studies, which evaluated PROMs postoperatively or at midterm follow-up after MTP1 arthrodesis [7,34,35,36,37,38]. Furthermore, the following clinically relevant improvements based on the MOXFQ are observed after surgery: scores in the MOXFQ domains are comparable to or greater than the minimal clinically important differences of 12, 16, and 24 in the MOXFQ domains of pain, walking or standing, and social interaction, respectively [25]. Comparing the AOFAS-HMI scores with healthy individuals’ values, which range between 87.4 and 84 points for people between 50 and 79 years of age, allows to conclude that a mean AOFAS-HMI score of 79.1 after surgery in the present study is approaching the normal reference values of individuals without any foot pathology [39].
Moreover, the present study demonstrates that following MTP1 arthrodesis, patients experience a substantial reduction in complaints and an increase in satisfaction, while the foot compensates for the loss of MTP1 joint motion after surgery. Therefore, improvements in PROMs do not necessarily indicate normalized foot function to the level observed in healthy individuals without foot pathology. In addition to the altered foot biomechanics following MTP1 arthrodesis, the observed improvements in clinical outcomes and reduction in pain may, from the patient’s perspective, be the most meaningful and valuable results.
This is the first prospective study evaluating the effects of MTP1 arthrodesis on foot and ankle kinematics and on PROMs in patients with HR before and after surgery compared with healthy individuals. Most prior studies have been limited to describing one of these outcomes or have used a cross-sectional study design [3,8,10,33].
Another strength of this study is the use of the OFM, a widely adopted multi-segment model for assessing foot and ankle kinematics that enables motion detection in the first ray [19,20,40,41]. However, it is important to note that the OFM measures relative motion between foot segments rather than at isolated joints in the traditional anatomical sense. Consequently, motion detected in the hallux/forefoot segment following MTP1 arthrodesis still represents movement of the forefoot and the interphalangeal joint of the first ray. The identification of joint motion using dynamic imaging techniques and markers remains challenging. Research and development of multi-segment foot models is ongoing to improve the reliability of detecting foot and ankle motion during gait [41,42]. Despite the described findings, the present study has some limitations. The relatively small sample size could be a potential weakness, as it could result in underpowering. Therefore, absolute data is reported to present the magnitude of the observed differences and to facilitate the decision regarding whether a clinically relevant effect has been found [43,44]. Secondly, ROM during the push-off phase is calculated based on percentages of the gait cycle, although determination based on ground reaction force (GRF) data is considered the most accurate approach. This method is recommended in future gait studies. Finally, one surgical revision is performed due to nonunion. The literature reports of nonunion or delayed union rates are approximately 6.6% [6]. Despite the complication in this study, no specific gait deviations are noted compared with the other patients with arthrodesis.
Long-term studies are recommended to investigate functional foot and ankle problems after long-term follow-up due to the altered gait pattern in patients with MTP1 arthrodesis compared with healthy subjects. Moreover, comparison with different surgical interventions could be innovative, as an increase in hallux motion during walking is expected after total joint replacement. Therefore, the foot is likely to compensate less and present gait patterns comparable to healthy individuals. Perhaps this is a more suitable option for patients with less compensatory reserve (i.e., less frontal forefoot and hindfoot motion). Upcoming studies must also elucidate which patient would have, for example, an advantage from a restoration of hallux motion (i.e., a total joint prosthesis) instead of an MTP1 fixation with arthrodesis. If known, kinematic analysis could contribute to surgical planning, resulting in an optimal selection of a patient’s intervention.
5. Conclusions
The present study demonstrates that the loss of hallux motion after MTP1 arthrodesis is compensated by increased frontal plane motion in the forefoot and hindfoot. Prior to surgery, in which patients suffer from painful HR, a comparable motion pattern in the forefoot by increased frontal plane motion is observed, while hindfoot motion in the frontal plane does not change. Therefore, it is proved that the foot has the intrinsic capacity to compensate for the loss of MTP1 motion in HR and after MTP1 arthrodesis. Proper functioning of the forefoot and hindfoot is a considerable component of preoperative planning to select subjects suitable for MTP1 arthrodesis. Furthermore, improvements in PROMs, which reflect a significant reduction in pain and increased satisfaction in functioning in daily and social activities, are seen after surgery.
Author Contributions
Conceptualization, R.T.A.L.d.B., J.S., H.M.S., K.M. and A.M.W.; methodology, R.T.A.L.d.B., J.S., H.M.S., K.M. and A.M.W.; software, R.T.A.L.d.B. and J.S.; validation R.T.A.L.d.B., J.S., H.M.S., K.M. and A.M.W.; formal analysis, R.T.A.L.d.B. and J.S.; investigation, R.T.A.L.d.B. and J.S.; resources, R.T.A.L.d.B., J.S., H.M.S., K.M. and A.M.W.; data curation, R.T.A.L.d.B. and J.S.; writing—original draft preparation, R.T.A.L.d.B.; writing—review and editing, R.T.A.L.d.B., J.S., H.M.S., K.M. and A.M.W.; visualization, R.T.A.L.d.B.; supervision, H.M.S., K.M. and A.M.W.; project administration, R.T.A.L.d.B.; funding acquisition, not applicable. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of azM/UM 14-4-080, date of approval 15 January 2015.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| AOFAS-HMI | American Orthopedic Foot and Ankle Society (AOFAS) rating system for the Hallux Metatarsophalangeal-Interphalangeal (HMI) scale |
| DF | dorsiflexion |
| EV | eversion |
| HC | healthy controls |
| HR | hallux rigidus |
| IN | inversion |
| MOXFQ | Manchester–Oxford Foot Questionnaire |
| MTP1 | first metatarsophalangeal joint |
| NPRS | Numeric Pain Rating Scale |
| OFM | Oxford foot model |
| PF | plantar flexion |
| PRO | pronation |
| ROM | range of motion |
| SUP | supination |
| T1 | first toe |
| T2-T5 | second to fifth toe |
References
- Ho, B.; Baumhauer, J. Hallux rigidus. EFORT Open Rev. 2017, 2, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Keiserman, L.S.; Sammarco, V.J.; Sammarco, G.J. Surgical treatment of the hallux rigidus. Foot Ankle Clin. 2005, 10, 75–96. [Google Scholar] [CrossRef] [PubMed]
- Galois, L.; Girard, D.; Martinet, N.; Delagoutte, J.P.; Mainard, D. Optoelectronic gait analysis after metatarsophalangeal arthrodesis of the hallux: Fifteen cases. Rev. Chir. Orthop. Reparatrice Appar. Mot. 2006, 92, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Roddy, E.; Menz, H.B. Foot osteoarthritis: Latest evidence and developments. Ther. Adv. Musculoskelet. Dis. 2018, 10, 91–103. [Google Scholar] [CrossRef]
- Kumar, S.; Pradhan, R.; Rosenfeld, P.F. First metatarsophalangeal arthrodesis using a dorsal plate and a compression screw. Foot Ankle Int. 2010, 31, 797–801. [Google Scholar] [CrossRef]
- Stevens, J.; de Bot, R.; Hermus, J.P.S.; van Rhijn, L.W.; Witlox, A.M. Clinical outcome following total joint replacement and arthrodesis for hallux rigidus: A systematic review. JBJS Rev. 2017, 5, e2. [Google Scholar] [CrossRef]
- Stevens, J.; de Bot, R.; Witlox, A.M.; Borghans, R.; Smeets, T.; Beertema, W.; Hendrickx, R.P.; Schotanus, M.G.M. Long-term effects of cheilectomy, Keller’s arthroplasty, and arthrodesis for symptomatic hallux rigidus on patient-reported and radiologic outcome. Foot Ankle Int. 2020, 41, 775–783. [Google Scholar] [CrossRef]
- Brodsky, J.W.; Baum, B.S.; Pollo, F.E.; Mehta, H. Prospective gait analysis in patients with first metatarsophalangeal joint arthrodesis for hallux rigidus. Foot Ankle Int. 2007, 28, 162–165. [Google Scholar] [CrossRef]
- DeFrino, P.F.; Brodsky, J.W.; Pollo, F.E.; Crenshaw, S.J.; Beischer, A.D. First metatarsophalangeal arthrodesis: A clinical, pedobarographic and gait analysis study. Foot Ankle Int. 2002, 23, 496–502. [Google Scholar] [CrossRef]
- Stevens, J.; Meijer, K.; Bijnens, W.; Fuchs, M.C.; van Rhijn, L.W.; Hermus, J.P.; van Hoeve, S.; Poeze, M.; Witlox, A.M. Gait Analysis of foot compensation after arthrodesis of the first metatarsophalangeal joint. Foot Ankle Int. 2017, 38, 181–191. [Google Scholar] [CrossRef]
- Rajan, R.; Mishra, A. A systematic review of total arthroplasty and arthrodesis for end-stage hallux rigidus: A biomechanical perspective. Foot 2021, 49, 101838. [Google Scholar] [CrossRef] [PubMed]
- Van Gheluwe, B.; Dananberg, H.J.; Hagman, F.; Vanstaen, K. Effects of hallux limitus on plantar foot pressure and foot kinematics during walking. J. Am. Podiatr. Med. Assoc. 2006, 96, 428–436. [Google Scholar] [CrossRef] [PubMed]
- Shereff, M.J.; Baumhauer, J.F. Hallux rigidus and osteoarthrosis of the first metatarsophalangeal joint. J. Bone Jt. Surg. Am. 1998, 80, 898–908. [Google Scholar] [CrossRef] [PubMed]
- Miana, A.; Paola, M.; Duarte, M.; Nery, C.; Freitas, M. Gait and Balance Biomechanical Characteristics of Patients With Grades III and IV Hallux Rigidus. J. Foot Ankle Surg. 2022, 61, 452–455. [Google Scholar] [CrossRef]
- Kuni, B.; Wolf, S.I.; Zeifang, F.; Thomsen, M. Foot kinematics in walking on a level surface and on stairs in patients with hallux rigidus before and after cheilectomy. J. Foot Ankle Res. 2014, 7, 13. [Google Scholar] [CrossRef]
- Stevens, J.; de Bot, R.; Hermus, J.P.S.; Schotanus, M.G.M.; Meijer, K.; Witlox, A.M. Gait analysis of foot compensation in symptomatic Hallux Rigidus patients. Foot Ankle Surg. 2022, 28, 1272–1278. [Google Scholar] [CrossRef]
- Picouleau, A.; Orsoni, N.; Hardy, J.; Mabit, C.; Charissoux, J.L.; Marcheix, P.S. Analysis of the effects of arthrodesis of the hallux metatarsophalangeal joint on gait cycle: Results of a GAITRite((R)) treadmill test. Int. Orthop. 2020, 44, 2167–2176. [Google Scholar] [CrossRef]
- Rajan, R.A.; Kerr, M.; Hafesji-Wade, A.; Osler, C.J.; Outram, T. A prospective clinical and biomechanical analysis of feet following first metatarsophalangeal joint arthrodesis for end stage hallux rigidus. Gait Posture 2024, 109, 208–212. [Google Scholar] [CrossRef]
- Wright, C.J.; Arnold, B.L.; Coffey, T.G.; Pidcoe, P.E. Repeatability of the modified Oxford foot model during gait in healthy adults. Gait Posture 2011, 33, 108–112. [Google Scholar] [CrossRef]
- Carson, M.C.; Harrington, M.E.; Thompson, N.; O’Connor, J.J.; Theologis, T.N. Kinematic analysis of a multi-segment foot model for research and clinical applications: A repeatability analysis. J. Biomech. 2001, 34, 1299–1307. [Google Scholar] [CrossRef]
- Perry, J.; Burnfield, J. Gait Analysis: Normal and Pathological Function; Slack Incorporated: West Deptford, NJ, USA, 2010. [Google Scholar]
- Ibrahim, T.; Beiri, A.; Azzabi, M.; Best, A.J.; Taylor, G.J.; Menon, D.K. Reliability and validity of the subjective component of the American Orthopaedic Foot and Ankle Society clinical rating scales. J. Foot Ankle Surg. 2007, 46, 65–74. [Google Scholar] [CrossRef] [PubMed]
- Kitaoka, H.B.; Alexander, I.J.; Adelaar, R.S.; Nunley, J.A.; Myerson, M.S.; Sanders, M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994, 15, 349–353. [Google Scholar] [CrossRef] [PubMed]
- Morley, D.; Jenkinson, C.; Doll, H.; Lavis, G.; Sharp, R.; Cooke, P.; Dawson, J. The Manchester-Oxford Foot Questionnaire (MOXFQ): Development and validation of a summary index score. Bone Jt. Res. 2013, 2, 66–69. [Google Scholar] [CrossRef] [PubMed]
- Dawson, J.; Coffey, J.; Doll, H.; Lavis, G.; Cooke, P.; Herron, M.; Jenkinson, C. A patient-based questionnaire to assess outcomes of foot surgery: Validation in the context of surgery for hallux valgus. Qual. Life Res. 2006, 15, 1211–1222. [Google Scholar] [CrossRef]
- Budiman-Mak, E.; Conrad, K.J.; Roach, K.E. The Foot Function Index: A measure of foot pain and disability. J. Clin. Epidemiol. 1991, 44, 561–570. [Google Scholar] [CrossRef]
- Downie, W.W.; Leatham, P.A.; Rhind, V.M.; Wright, V.; Branco, J.A.; Anderson, J.A. Studies with pain rating scales. Ann. Rheum. Dis. 1978, 37, 378–381. [Google Scholar] [CrossRef]
- Regnauld, B. Disorders of the Great Toe; Springer: Berlin/Heidelberg, Germany, 1986; pp. 345–359. [Google Scholar]
- Coughlin, M.J. Rheumatoid forefoot reconstruction—A long-term follow-up study. J. Bone Jt. Surg.-Am. Vol. 2000, 82a, 322–341. [Google Scholar] [CrossRef]
- Pataky, T.C. Generalized n-dimensional biomechanical field analysis using statistical parametric mapping. J. Biomech. 2010, 43, 1976–1982. [Google Scholar] [CrossRef]
- Murray, M.P.; Kory, R.C.; Clarkson, B.H.; Sepic, S.B. Comparison of free and fast speed walking patterns of normal men. Am. J. Phys. Med. 1966, 45, 8–23. [Google Scholar] [CrossRef]
- Fukuchi, C.A.; Fukuchi, R.K.; Duarte, M. Effects of walking speed on gait biomechanics in healthy participants: A systematic review and meta-analysis. Syst. Rev. 2019, 8, 153. [Google Scholar] [CrossRef]
- Canseco, K.; Long, J.; Marks, R.; Khazzam, M.; Harris, G. Quantitative characterization of gait kinematics in patients with hallux rigidus using the Milwaukee foot model. J. Orthop. Res. 2008, 26, 419–427. [Google Scholar] [CrossRef] [PubMed]
- Beertema, W.; Draijer, W.F.; van Os, J.J.; Pilot, P. A retrospective analysis of surgical treatment in patients with symptomatic hallux rigidus: Long-term follow-up. J. Foot Ankle Surg. 2006, 45, 244–251. [Google Scholar] [CrossRef] [PubMed]
- Voskuijl, T.; Onstenk, R. Operative Treatment for Osteoarthritis of the First Metatarsophalangeal Joint: Arthrodesis Versus Hemiarthroplasty. J. Foot Ankle Surg. 2015, 54, 1085–1088. [Google Scholar] [CrossRef] [PubMed]
- Erdil, M.; Elmadag, N.M.; Polat, G.; Tuncer, N.; Bilsel, K.; Ucan, V.; Erkocak, O.F.; Sen, C. Comparison of arthrodesis, resurfacing hemiarthroplasty, and total joint replacement in the treatment of advanced hallux rigidus. J. Foot Ankle Surg. 2013, 52, 588–593. [Google Scholar] [CrossRef]
- Chraim, M.; Bock, P.; Alrabai, H.M.; Trnka, H.J. Long-term outcome of first metatarsophalangeal joint fusion in the treatment of severe hallux rigidus. Int. Orthop. 2016, 40, 2401–2408. [Google Scholar] [CrossRef]
- de Bot, R.; Veldman, H.D.; Eurlings, R.; Stevens, J.; Hermus, J.P.S.; Witlox, A.M. Metallic hemiarthroplasty or arthrodesis of the first metatarsophalangeal joint as treatment for hallux rigidus: A systematic review and meta-analysis. Foot Ankle Surg. 2022, 28, 139–152. [Google Scholar] [CrossRef]
- Schneider, W.; Jurenitsch, S. Normative data for the American Orthopedic Foot and Ankle Society ankle-hindfoot, midfoot, hallux and lesser toes clinical rating system. Int. Orthop. 2016, 40, 301–306. [Google Scholar] [CrossRef]
- van Hoeve, S.; Vos, J.; Weijers, P.; Verbruggen, J.; Willems, P.; Poeze, M.; Meijer, K. Repeatability of the Oxford Foot Model for Kinematic Gait Analysis of the Foot and Ankle. Clin. Res. Foot Ankle 2015, 3, 1–8. [Google Scholar]
- Schallig, W.; van den Noort, J.C.; McCahill, J.; Stebbins, J.; Leardini, A.; Maas, M.; Harlaar, J.; van der Krogt, M.M. Comparing the kinematic output of the Oxford and Rizzoli Foot Models during normal gait and voluntary pathological gait in healthy adults. Gait Posture 2020, 82, 126–132. [Google Scholar] [CrossRef]
- Schallig, W.; van den Noort, J.C.; Piening, M.; Streekstra, G.J.; Maas, M.; van der Krogt, M.M.; Harlaar, J. The Amsterdam Foot Model: A clinically informed multi-segment foot model developed to minimize measurement errors in foot kinematics. J. Foot Ankle Res. 2022, 15, 46. [Google Scholar] [CrossRef]
- Aarts, S.; van den Akker, M.; Winkens, B. The importance of effect sizes. Eur. J. Gen. Pract. 2014, 20, 61–64. [Google Scholar] [CrossRef]
- Sullivan, G.M.; Feinn, R. Using Effect Size-or Why the P Value Is Not Enough. J. Grad. Med. Educ. 2012, 4, 279–282. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).