Low Malaria Transmission in Rosso, an Irrigated Rice-Growing Area in Mauritania
Abstract
:1. Introduction
2. Results
2.1. Demographic Characteristics of Patients
2.2. Clinical Presentation and Malaria Diagnosis
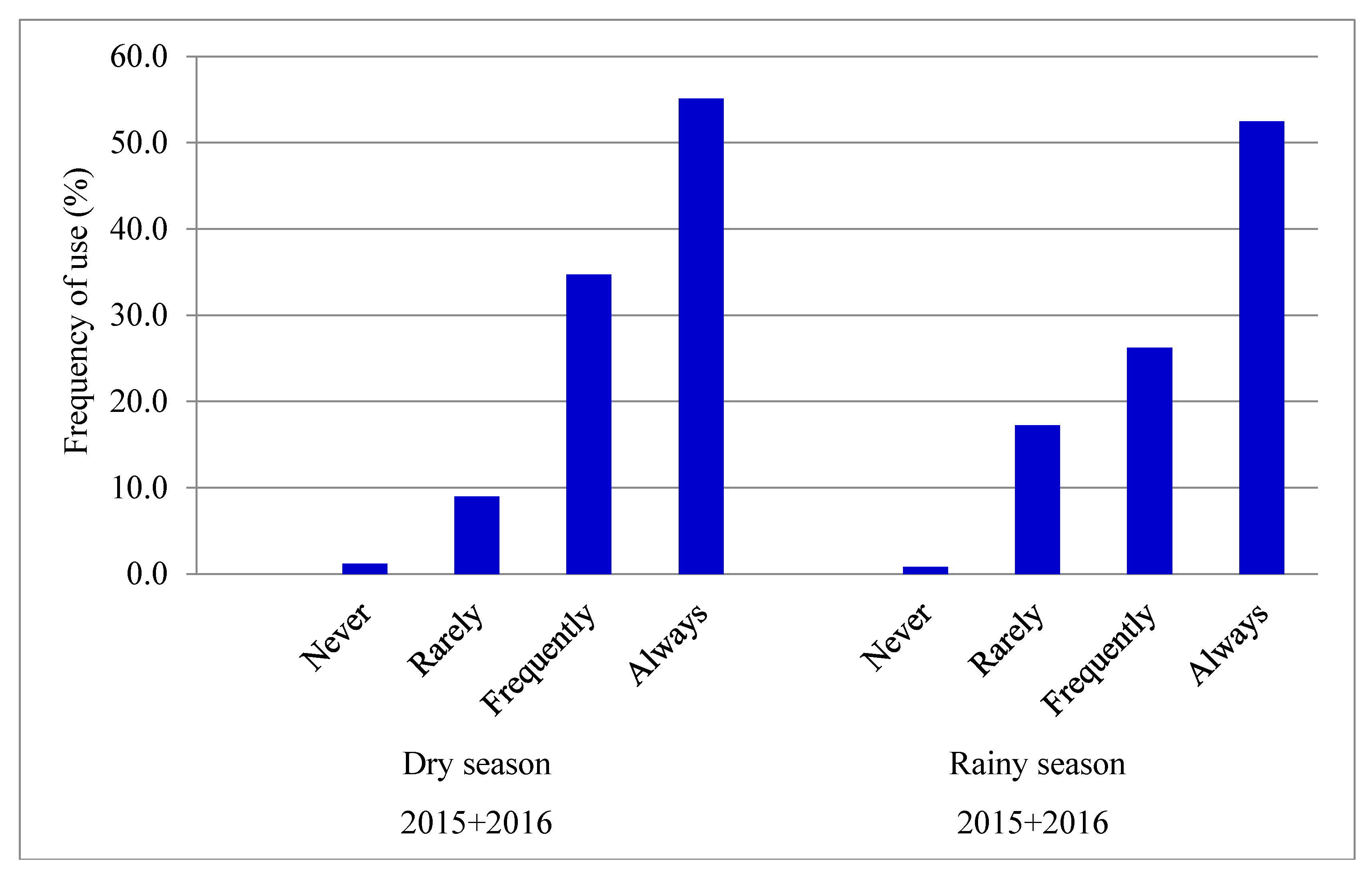
2.3. Ownership and Use of ITNs
3. Discussion
4. Materials and Methods
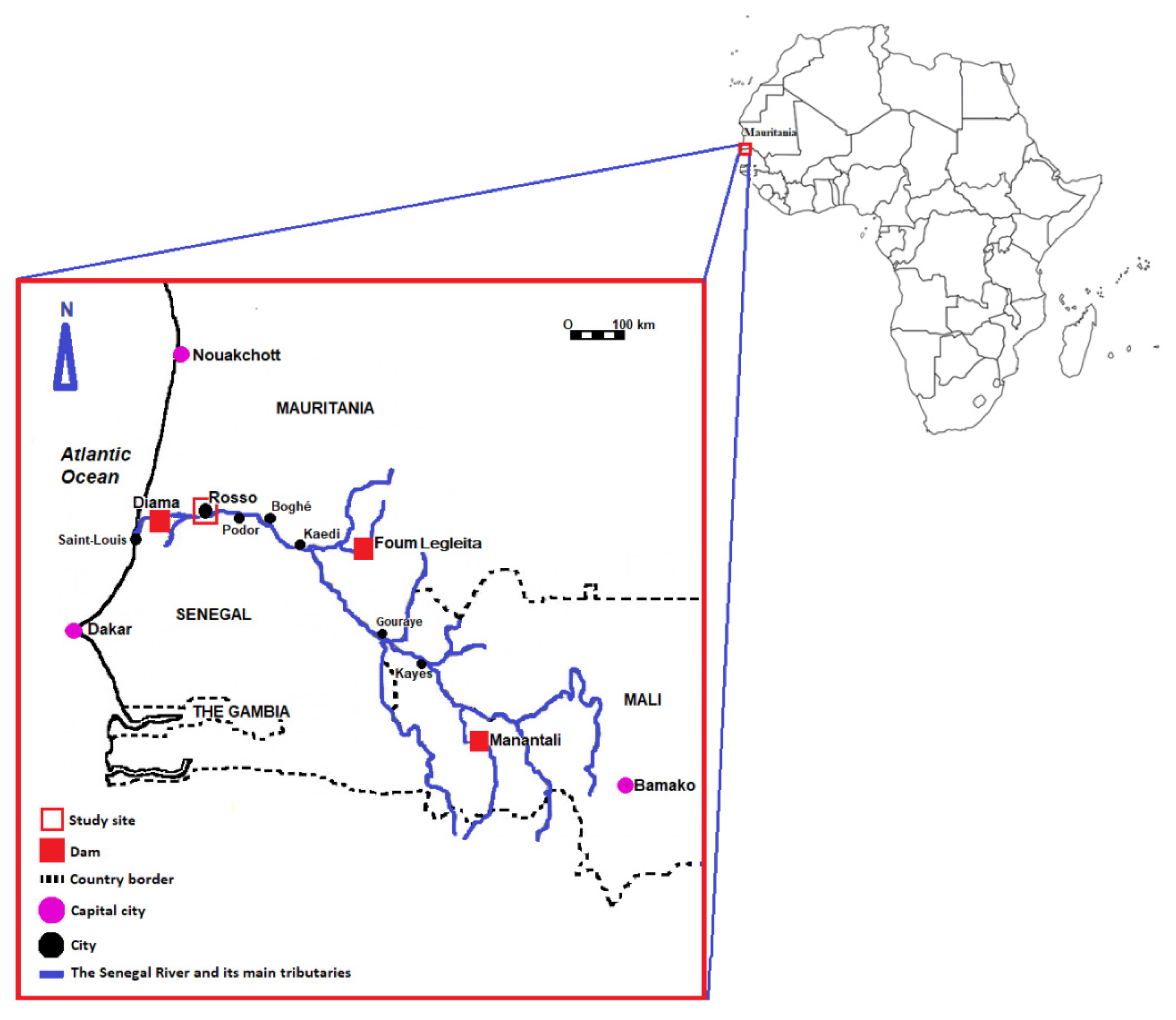
4.1. Study Area
4.2. Study Population, Inclusion Criteria, and Data Collection
4.3. Malaria Diagnosis
4.4. Data Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- World Health Organization. World Malaria Report 2020; WHO: Geneva, Switzerland, 2020; Available online: https://apps.who.int/iris/handle/10665/337660 (accessed on 5 December 2021).
- Ouldabdallahi, M.; Ouldbezeid, M.; Dieye, M.; Yacine, B.; Faye, O. Study of the incidence of malaria in febrile patients and among schoolchildren in the region of Trarza, Islamic Republic of Mauritania. Bull. Soc. Pathol. Exot. 2011, 104, 288–290. [Google Scholar] [CrossRef] [PubMed]
- Ouldabdallahi Moukah, M.O.; Ba, O.; Ba, H.; Ould Khairy, M.L.; Faye, O.; Bogreau, H.; Simard, F.; Basco, L.K. Malaria in three epidemiological strata in Mauritania. Malar. J. 2016, 15, 204. [Google Scholar] [CrossRef] [Green Version]
- Ould Ahmedou Salem, M.S.; Mint Lekweiry, K.; Bouchiba, H.; Pascual, A.; Pradines, B.; Ould Mohamed Salem Boukhary, A.; Briolant, S.; Basco, L.K.; Bogreau, H. Characterization of Plasmodium falciparum genes associated with drug resistance in Hodh Elgharbi, a malaria hotspot near Malian-Mauritanian border. Malar. J. 2017, 16, 140. [Google Scholar] [CrossRef] [PubMed]
- Deida, J.; Tahar, R.; Khalef, Y.O.; Lekweiry, K.M.; Hmeyade, A.; Khairy, M.L.O.; Simard, F.; Bogreau, H.; Basco, L.; Boukhary, A.O.M.S. Oasis malaria, northern Mauritania. Emerg. Infect. Dis. 2019, 25, 273–280. [Google Scholar] [CrossRef]
- Diallo, S.M.; Bogreau, H.; Papa Mze, N.; Ould Ahmedou Salem, M.S.; Ould Khairy, M.L.; Parola, P.; Basco, L.; Ould Mohamed Salem Boukhary, A. Malaria epidemiology in Kobeni department, southeastern Mauritania from 2015 to 2017. Infect. Dis. Poverty 2020, 9, 21. [Google Scholar] [CrossRef] [Green Version]
- Dia, I.; Konate, L.; Samb, B.; Sarr, J.B.; Diop, A.; Rogerie, F.; Faye, M.; Riveau, G.; Remoue, F.; Diallo, M.; et al. Bionomics of malaria vectors and relationship with malaria transmission and epidemiology in three physiographic zones in the Senegal River basin. Acta Trop. 2008, 105, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Lekweiry, K.M.; Salem, M.S.; Cotteaux-Lautard, C.; Jarjaval, F.; Marin-Jauffre, A.; Bogreau, H.; Basco, L.; Briolant, S.; Boukhary, A.O.; Brahim, K.O.; et al. Circumsporozoite protein rates, blood-feeding pattern and frequency of knockdown resistance mutations in Anopheles spp. in two ecological zones of Mauritania. Parasites Vectors 2016, 9, 268. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mint Mohamed Lemine, A.; Ould Lemrabott, M.A.; Hasni Ebou, M.; Mint Lekweiry, K.; Ould Ahmedou Salem, M.S.; Ould Brahim, K.; Ouldabdallahi Moukah, M.; Ould Bouraya, I.N.; Brengues, C.; Trape, J.F.; et al. Mosquitoes (Diptera: Culicidae) in Mauritania: A review of their biodiversity, distribution and medical importance. Parasites Vectors 2017, 10, 35. [Google Scholar] [CrossRef] [Green Version]
- Steinhardt, L.C.; Jean, Y.S.; Impoinvil, D.; Mace, K.E.; Wiegand, R.; Huber, C.S.; Alexandre, J.S.F.; Frederick, J.; Nkurunziza, E.; Jean, S.; et al. Effectiveness of insecticide-treated bednets in malaria prevention in Haiti: A case-control study. Lancet Glob. Health 2017, 5, e96–e103. [Google Scholar] [CrossRef] [Green Version]
- Ijumba, J.N.; Lindsay, S.W. Impact of irrigation on malaria in Africa: Paddies paradox. Med. Vet. Entomol. 2001, 15, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Jobin, W.R.; Negrón-Aponte, H.; Michelson, E.H. Schistosomiasis in the Gorgol valley of Mauritania. Am. J. Trop. Med. Hyg. 1976, 25, 587–594. [Google Scholar] [CrossRef]
- Chaine, J.P.; Malek, E.A. Urinary schistosomiasis in the Sahelian region of the Senegal River Basin. Trop. Geogr. Med. 1983, 35, 249–256. [Google Scholar] [PubMed]
- Poussin, J.C.; Diallo, Y.; Legoupil, J.C.; Sow, A. Increase in rice productivity in the Senegal River valley due to improved collective management of irrigation schemes. Agron. Sustain. Dev. 2005, 25, 225–236. [Google Scholar] [CrossRef]
- Diuk-Wasser, M.A.; Touré, M.B.; Dolo, G.; Bagayoko, M.; Sogoba, N.; Sissoko, I.; Traoré, S.F.; Taylor, C.E. Effect of rice cultivation patterns on malaria vector abundance in rice-growing villages in Mali. Am. J. Trop. Med. Hyg. 2007, 76, 869–874. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sow, S.; de Vlas, S.J.; Engels, D.; Gryseels, B. Water-related disease patterns before and after the construction of the Diama dam in northern Senegal. Ann. Trop. Med. Parasitol. 2002, 96, 575–586. [Google Scholar] [CrossRef]
- Faye, O.; Fontenille, D.; Hervé, J.P.; Diack, P.A.; Diallo, S.; Mouchet, J. Malaria in the Saharan region of Senegal. 1. Entomological transmission findings. Ann. Soc. Belg. Med. Trop. 1993, 73, 21–30. [Google Scholar] [PubMed]
- Faye, O.; Gaye, O.; Hervé, J.P.; Diack, P.A.; Diallo, S. Malaria in the Saharan region of Senegal. 2. Parasitological indices. Ann. Soc. Belg. Med. Trop. 1993, 73, 31–36. [Google Scholar]
- Faye, O.; Fontenille, D.; Gaye, O.; Sy, N.; Molez, J.F.; Konate, L.; Hebrard, G.; Herve, J.P.; Trouillet, J.; Diallo, S.; et al. Malaria and rice growing in the Senegal River delta (Senegal). Ann. Soc. Belg. Med. Trop. 1995, 75, 179–189. [Google Scholar] [PubMed]
- Faye, O.; Gaye, O.; Konaté, L.; Molez, J.F.; Feller-Dansokho, E.; Hervé, J.P. Prediction and prevention of malaria epidemics in the valley of the Senegal River. Santé 1998, 8, 347–352. [Google Scholar]
- Carrara, G.C.; Petrarca, V.; Niang, M.; Coluzzi, M. Anopheles pharoensis and transmission of Plasmodium falciparum in the Senegal River delta, West Africa. Med. Vet. Entomol. 1990, 4, 421–424. [Google Scholar] [CrossRef]
- Ndiath, M.O.; Sarr, J.B.; Gaayeb, L.; Mazenot, C.; Sougoufara, S.; Konate, L.; Remoue, F.; Hermann, E.; Trape, J.F.; Riveau, G.; et al. Low and seasonal malaria transmission in the middle Senegal River basin: Identification and characteristics of Anopheles vectors. Parasites Vectors 2012, 5, 21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ould Lemrabott, M.A.; Ould Ahmedou Salem, M.S.; Ould Brahim, K.; Brengues, C.; Rossignol, M.; Bogreau, H. Seasonal abundance, blood meal sources and insecticide susceptibility in major anopheline malaria vectors from southern Mauritania. Parasites Vectors 2018, 11, 232. [Google Scholar] [CrossRef] [PubMed]
- Dolo, G.; Briët, O.J.T.; Dao, A.; Traoré, S.F.; Bouaré, M.; Sogoba, N.; Niaré, O.; Bagayogo, M.; Sangaré, D.; Teuscher, T.; et al. Malaria transmission in relation to rice cultivation in the irrigated Sahel of Mali. Acta Trop. 2004, 89, 147–159. [Google Scholar] [CrossRef] [PubMed]
- Ba, O.; Sow, A.; Ba, H.; Dahdi, S.; Lo, B. Seasonal transmission of malaria in the Senegal River Valley: Case study of the city of Kaedi-Mauritanie. Pan Afr. Med. J. 2019, 34, 185. [Google Scholar] [CrossRef] [PubMed]
- Touray, S.; Bâ, H.; Bâ, O.; Koïta, M.; Ould Ahmed Salem, C.B.; Keïta, M.; Traoré, D.; Sy, I.; Winkler, M.S.; Utzinger, J.; et al. Absence of dry season Plasmodium parasitaemia, but high rates of reported acute respiratory infection and diarrhoea in preschool-aged children in Kaédi, southern Mauritania. Parasites Vectors 2012, 5, 193. [Google Scholar] [CrossRef] [Green Version]
- Hofmann, N.E.; Gruenberg, M.; Nate, E.; Ura, A.; Rodriguez-Rodriguez, D.; Salib, M.; Mueller, I.; Smith, T.A.; Laman, M.; Robinson, L.J.; et al. Assessment of ultra-sensitive malaria diagnosis versus standard molecular diagnostics for malaria elimination: An in-depth molecular community cross-sectional study. Lancet Infect. Dis. 2018, 18, 1108–1116. [Google Scholar] [CrossRef]
- Mohon, A.N.; Getie, S.; Jahan, N.; Alam, M.S.; Pillai, D.R. Ultrasensitive loop mediated isothermal amplification (US-LAMP) to detect malaria for elimination. Malar. J. 2019, 18, 350. [Google Scholar] [CrossRef]
- Danwang, C.; Kirakoya-Samadoulougou, F.; Samadoulougou, S. Assessing field performance of ultrasensitive rapid diagnostic tests for malaria: A systematic review and meta-analysis. Malar. J. 2021, 20, 245. [Google Scholar] [CrossRef]
- Zainabadi, K. Ultrasensitive diagnostics for low-density asymptomatic Plasmodium falciparum infections in low-transmission settings. J. Clin. Microbiol. 2021, 59, e01508-20. [Google Scholar] [CrossRef] [PubMed]
- Marrama, L.; Jambou, R.; Rakotoarivony, I.; Leong Pock Tsi, J.M.; Duchemin, J.B.; Laventure, S.; Mouchet, J.; Roux, J. Malaria transmission in southern Madagascar: Influence of the environment and hydro-agricultural works in sub-arid and humid regions. Part 1. Entomological investigations. Acta Trop. 2004, 89, 193–203. [Google Scholar] [CrossRef] [PubMed]
- Khaemba, B.M.; Mutani, A.; Bett, M.K. Studies of anopheline mosquitoes transmitting malaria in a newly developed highland urban area: A case study of Moi University and its environs. East Afr. Med. J. 1994, 71, 159–164. [Google Scholar] [PubMed]
- Jaleta, K.T.; Hill, S.R.; Seyoum, E.; Balkew, M.; Gebre-Michael, T.; Ignell, R.; Tekie, H. Agro-ecosystems impact malaria prevalence: Large-scale irrigation drives vector population in western Ethiopia. Malar. J. 2013, 12, 350. [Google Scholar] [CrossRef] [Green Version]
- Diakité, N.R.; Guindo-Coulibaly, N.; Adja, A.M.; Ouattara, M.; Coulibaly, J.T.; Utzinger, J.; N’Goran, E.K. Spatial and temporal variation of malaria entomological parameters at the onset of a hydro-agricultural development in central Côte d’Ivoire. Malar. J. 2015, 14, 340. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pryce, J.; Richardson, M.; Lengeler, C. Insecticide-treated nets for preventing malaria. Cochrane Database Syst. Rev. 2018, 11, CD000363. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.S.; Fullman, N.; Stokes, A.; Ravishankar, N.; Masiye, F.; Murray, C.J.; Gakidou, E. Net benefits: Associations between insecticide-treated mosquito nets and malaria morbidity and childhood mortality in sub-Saharan Africa. PLoS Med. 2011, 8, e1001091. [Google Scholar] [CrossRef] [Green Version]
- Bayoh, M.N.; Mathias, D.K.; Odiere, M.R.; Mutuku, F.M.; Kamau, L.; Gimnig, J.E.; Vulule, J.M.; Hawley, W.A.; Hamel, M.J.; Walker, E.D. Anopheles gambiae: Historical population decline associated with regional distribution of insecticide-treated bed nets in western Nyanza province, Kenya. Malar. J. 2010, 9, 62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Takken, W.; Verhulst, N.O. Host preferences of blood-feeding mosquitoes. Annu. Rev. Entomol. 2013, 58, 433–453. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Diuk-Wasser, M.A.; Toure, M.B.; Dolo, G.; Bagayoko, M.; Sogoba, N.; Traore, S.F.; Manoukis, N.; Taylor, C.E. Vector abundance and malaria transmission in rice-growing villages in Mali. Am. J. Trop. Med. Hyg. 2005, 72, 725–731. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sanchez-Ribas, J.; Parra-Henao, G.; Guimarães, A.E. Impact of dams and irrigation schemes in anopheline (Diptera: Culicidae) bionomics and malaria epidemiology. Rev. Inst. Med. Trop. Sao Paulo 2012, 54, 179–191. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ouldabdallahi, M.; Alew, I.; Ould Ahmedou Salem, M.S.; Ba, M.D.D.; Ould Mohamed Salem Boukhary, A.; Ould Khairy, M.L.; Aziz, M.B.; Ringwald, P.; Basco, L.K.; Niang, S.D.; et al. Efficacy of artesunate-amodiaquine for the treatment of acute uncomplicated falciparum malaria in southern Mauritania. Malar. J. 2014, 13, 496. [Google Scholar] [CrossRef]
- World Bank. Senegal River Basin Multi-Purpose Water Resources Development Project. 2013. Available online: http://documents1.worldbank.org/curated/en/714611468009330144/pdf/ICR26530ICR0Se00PUBLIC00Box379845B0.pdf (accessed on 18 October 2021).
- Peng, W.K.; Kong, T.F.; Ng, C.S.; Chen, L.; Huang, Y.; Bhagat, A.A.; Nguyen, N.T.; Preiser, P.R.; Han, J. Micromagnetic resonance relaxometry for rapid label-free malaria diagnosis. Nat. Med. 2014, 20, 1069–1073. [Google Scholar] [CrossRef] [PubMed]
- Di Gregorio, E.; Ferrauto, G.; Schwarzer, E.; Gianolio, E.; Valente, E.; Ulliers, D.; Aime, S.; Skorokhod, O. Relaxometric studies of erythrocyte suspensions infected by Plasmodium falciparum: A tool for staging infection and testing anti-malarial drugs. Magn. Reson. Med. 2020, 84, 3366–3378. [Google Scholar] [CrossRef]
- Peng, W.K.; Ng, T.T.; Loh, T.P. Machine learning assistive rapid, label-free molecular phenotyping of blood with two-dimensional NMR correlational spectroscopy. Commun. Biol. 2020, 3, 535. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, T.; Hashimoto, M.; Nagatomi, K.; Nogami, T.; Sofue, Y.; Hayashi, T.; Ido, Y.; Yatsushiro, S.; Abe, K.; Kajimoto, K.; et al. Development of a quantitative, portable, and automated fluorescent blue-ray device-based malaria diagnostic equipment with an on-disc SiO2 nanofiber filter. Sci. Rep. 2020, 10, 6585. [Google Scholar] [CrossRef] [PubMed]
- Arndt, L.; Koleala, T.; Orbán, Á.; Ibam, C.; Lufele, E.; Timinao, L.; Lorry, L.; Butykai, Á.; Kaman, P.; Molnár, A.P.; et al. Magneto-optical diagnosis of symptomatic malaria in Papua New Guinea. Nat. Commun. 2021, 12, 969. [Google Scholar] [CrossRef] [PubMed]
- Office National de la Statistique. Recensement Général de la Population et de L’habitat 2013. Monographie de la Vill e de Rosso. Available online: http://www.ons.mr/index.php/publications/operations-statistiques/16-rgph-2013 (accessed on 18 October 2021).
- Ministry of Rural Development, Mauritania. Plan National de Développement Agricole (PNDA) 2015–2025. Available online: http://extwprlegs1.fao.org/docs/pdf/Mau175842.pdf (accessed on 5 December 2021).
- Snounou, G.; Viriyakosol, S.; Zhu, X.P.; Jarra, W.; Pinheiro, L.; do Rosario, V.E.; Thaithong, S.; Brown, K.N. High sensitivity of detection of human malaria parasites by the use of nested polymerase chain reaction. Mol. Biochem. Parasitol. 1993, 61, 315–320. [Google Scholar] [CrossRef]
| Characteristics | 2015 | 2016 | 2015–2016 |
|---|---|---|---|
| Number (%) | 246 (77.4) | 72 (22.6) | 318 (100) |
| Sex (n, %) | |||
| Male | 119 (48.4) | 34 (47.2) | 153 (48.1) |
| Female | 127 (51.6) | 38 (52.8) | 165 (51.9) |
| Age group (year; n, %) | |||
| <5 | 23 (9.3) | 7 (9.7) | 30 (9.4) |
| 5–9 | 35 (14.2) | 15 (20.8) | 50 (15.7) |
| 10–19 | 42 (17.1) | 14 (19.4) | 56 (17.6) |
| 20–39 | 95 (38.6) | 20 (27.7) | 115 (36.2) |
| 40–59 | 38 (15.4) | 9 (12.5) | 47 (14.8) |
| ≥60 | 13 (5.3) | 7 (9.7) | 20 (6.3) |
| Mean axillary temperature (°C) (range) | 37.9 (35.3–40.5) | 38.0 (36.0–40.0) | 38.0 (35.3–40.5) |
| Mean haemoglobin (g/dL) (range) | 10.1 (6.0–13.0) | 11.0 (8.4–12.0) | 10.5 (6.0–13.0) |
| Ethnicity | |||
| Moors | 179 (72.8) | 48 (66.7) | 227 (71.4) |
| Black Africans | 67 (27.2) | 24 (33.3) | 91 (28.6) |
| Travel history | |||
| Yes | 106 (43.0) | 14 (19.5) | 120 (37.7) |
| No | 140 (57.0) | 58 (80.5) | 198 (62.3) |
| Malaria test positivity | |||
| Rapid diagnostic test | 4 (2 Pf + 2 Pan) | 3 (Pf) | 7 (2.2) |
| Microscopy | 1 (Pf) | 1 (Pf) | 2 (0.6) |
| Polymerase chain reaction | 1 (Pv) | 1 (Pv) | 2 (0.6) |
| Characteristics | 2015 | 2016 | 2015–2016 |
|---|---|---|---|
| Household ownership of ITNs (n, %) 1 | |||
| Yes | 223 (91.1) | 62 (93.9) | 285 (91.6) |
| No | 22 (8.9) | 4 (6.1) | 26 (8.4) |
| Number of ITNs per household (n, %) | |||
| 1 | 42 (18.8) | 8 (12.9) | 50 (17.5) |
| 2–4 | 130 (58.3) | 41 (66.1) | 171 (60.0) |
| >4 | 51 (22.8) | 13 (20.9) | 64 (22.4) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ould Lemrabott, M.A.; Mint Lekweiry, K.; Deida, J.; Djigo, O.K.M.; Ould Ahmedou Salem, M.S.; Ould Khalef, Y.; Bogreau, H.; Simard, F.; Basco, L.; Ould Mohamed Salem Boukhary, A. Low Malaria Transmission in Rosso, an Irrigated Rice-Growing Area in Mauritania. Parasitologia 2021, 1, 257-268. https://doi.org/10.3390/parasitologia1040027
Ould Lemrabott MA, Mint Lekweiry K, Deida J, Djigo OKM, Ould Ahmedou Salem MS, Ould Khalef Y, Bogreau H, Simard F, Basco L, Ould Mohamed Salem Boukhary A. Low Malaria Transmission in Rosso, an Irrigated Rice-Growing Area in Mauritania. Parasitologia. 2021; 1(4):257-268. https://doi.org/10.3390/parasitologia1040027
Chicago/Turabian StyleOuld Lemrabott, Mohamed Aly, Khadijetou Mint Lekweiry, Jemila Deida, Oum Kelthoum Mamadou Djigo, Mohamed Salem Ould Ahmedou Salem, Yacoub Ould Khalef, Hervé Bogreau, Frédéric Simard, Leonardo Basco, and Ali Ould Mohamed Salem Boukhary. 2021. "Low Malaria Transmission in Rosso, an Irrigated Rice-Growing Area in Mauritania" Parasitologia 1, no. 4: 257-268. https://doi.org/10.3390/parasitologia1040027
APA StyleOuld Lemrabott, M. A., Mint Lekweiry, K., Deida, J., Djigo, O. K. M., Ould Ahmedou Salem, M. S., Ould Khalef, Y., Bogreau, H., Simard, F., Basco, L., & Ould Mohamed Salem Boukhary, A. (2021). Low Malaria Transmission in Rosso, an Irrigated Rice-Growing Area in Mauritania. Parasitologia, 1(4), 257-268. https://doi.org/10.3390/parasitologia1040027






