Abstract
Background: Positive identification is at the forefront of tasks for forensic practitioners when a set of remains is discovered. Standard means of identification include fingerprints, dental, and DNA analyses; however, additional methods are utilized by forensic practitioners to identify remains when these primary methods of identification are not applicable. Comparative radiography has become a frequently employed approach for positive identification, specifically focused on individualizing characteristics evident in human skeletal variation. Regions that display wide ranges of morphological variation within the human skeleton include the cranium as well as the thorax. With regard to the cranium specifically, paranasal sinuses have been recognized as unique features and are valuable for identification purposes. Objectives: This paper explores the basic information of the anatomy and development, range of variation, and the importance of paranasal sinuses in forensic contexts. Results: This article discusses how practitioners can best use the morphological information contained in the paranasal sinuses and how to compare the antemortem and postmortem datasets involving different imaging modalities for positive identification purposes, in order to provide practical concepts that may assist in cases where paranasal sinuses may be used for forensic human identification. Conclusions: Understanding the development of paranasal sinuses, the imaging techniques applied for their visualization, as well as the principles of identification, is key to conducting proper antemortem vs. postmortem comparisons and effectively utilizing paranasal sinuses in forensic identification contexts.
1. Introduction
When a set of human remains are discovered, forensic practitioners conduct a series of analyses to achieve a positive identification and reconstruct events surrounding the death event. Standard means of identification include fingerprints, dental treatment, and DNA analysis. However, forensic practitioners can rely on other techniques to achieve a positive identification, especially in cases where these standard means cannot be applied.
Skeletal elements, such as bones and teeth, can be used to establish the identity of a set of remains. Most often, this analysis involves antemortem versus postmortem radiograph comparison. In this sense, forensic anthropologists and forensic odontologists are uniquely qualified to process and analyze the remains and compare the postmortem to antemortem records as a means of identification [1]. Dental treatment and healed fractures, especially when they present surgical devices, are often used for forensic human identification due to their individuality. However, when no dental treatment or antemortem fractures are present, an identification can be achieved utilizing skeletal variations and anomalies within bones and teeth.
Human skeletal variation has a significant value for identification purposes due to the wide array of variation that can be present in the skeleton. Cranial, sternal, and rib morphological variations [2,3,4,5] have been studied to better understand their frequency and therefore to establish their significance for identification. Specifically, within the cranium, suture patterns, endocranial meningeal grooves, and paranasal sinuses have been explored for their use in personal identification [1,2,3,4,5,6,7].
The paranasal sinuses consist of four paired, aerated spaces located in the facial region. These paired cavities include the frontal sinus, ethmoidal sinus, maxillary sinus, and the sphenoidal sinus. In 1895, Zuckerandl first observed asymmetric morphology of the frontal sinus, piquing research interests in the paranasal sinuses for identification purposes [6].
Conventional radiography creates an image of the internal structures, which makes it of valuable use for paranasal sinuses comparison. Radiography was first suggested for the use in identifying unknown remains using the frontal sinus variability in 1921 by Schuller [7]. A few years later, in 1927, human identification through frontal sinus analysis was accepted in a court case in the US for the first time [6]. Since then, radiographic comparison of the frontal sinus has been widely employed by forensic practitioners as a means of positive identification [8]. Comparative radiography includes obtaining suitable antemortem radiographs, typically provided by law enforcement, and similarly positioned/oriented postmortem radiographs taken by forensic practitioners. Then, a visual comparison of the area(s) of interest is made by looking for consistencies between the radiographs. Consistencies can be identified from a range of features, including morphology, location, and size of different anatomical structures, and distinct features displayed in the skeleton. These same traits can also be used to identify any inconsistencies that may lead to an exclusion. The paranasal sinuses are highly variable, making them an ideal structure for radiographic comparisons. Today, identification using the morphological appearance of the paranasal sinuses in radiographs has become a common practice. The development and common use of other imaging modalities in the clinical setting, such as computed tomography (CT) and magnetic resonance imaging (MRI), has led to their use in forensic identification contexts. Thus, studies exploring the validity of different imaging techniques of paranasal sinus comparison for identification purposes have increased.
This article aims to cover the basic understanding of the anatomy and variation of the paranasal sinuses and how practitioners can use this information for forensic human identification. Additionally, the utilization of different imaging modalities in context and associated limitations are discussed.
2. Anatomy and Development of Paranasal Sinuses
The paranasal sinuses are comprised of four paired, air-filled spaces located within the maxillary, ethmoid, frontal, and sphenoid bones, all of which are covered by a mucous membrane and connected to the nasal cavity [9,10].
These sinuses play several important roles in the human body, encompassing both physiological and mechanical functions. They help to lighten the skull’s weight and enhance voice resonance. Additionally, they provide a cushioning effect against maxillofacial trauma, absorbing shock to protect the facial structures. Sinuses also humidify and warm the air we breathe and contribute to immunological functions [10,11,12] (Figure 1).
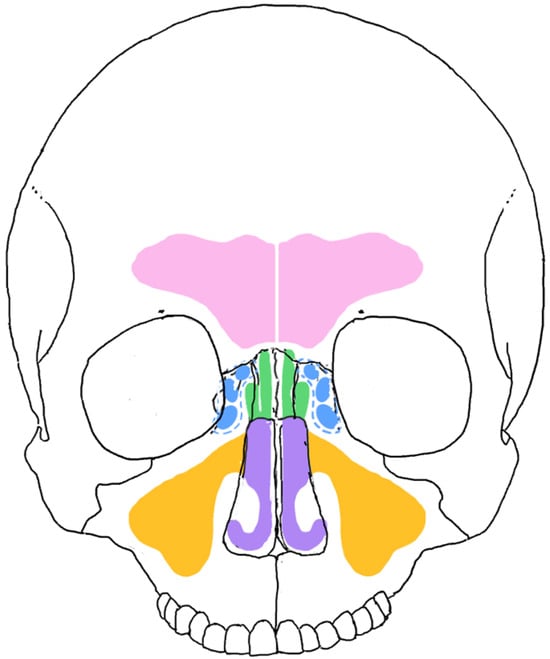
Figure 1.
Location and general morphology of the frontal (pink), sphenoidal (green), ethmoidal (blue) and maxillary (orange), and the nasal cavity (purple).
The development of the paranasal sinuses is an extremely complicated process, and the anatomy of the sinuses is highly variable. Such variability is highly important for their normal function and can assist enormously in personal identification.
An embryo shows its first identifiable head and face between weeks four and five of gestation with a central orifice, the stomodeum, which is surrounded by the mandibular, maxillary, and frontonasal prominences [13]. The facial structures develop between weeks four and ten from five prominences-the frontonasal, paired (left and right) maxillary, and paired (left and right) mandibular prominences [14].
The paranasal sinus development begins during intra-uterine life. Some are present at birth and continue to develop after birth until adult size is reached, enlarging their size by the pneumatization of the surrounding bones.
The ethmoidal sinuses are the first to develop, beginning with the appearance of the infundibulum of the ethmoid bone at about eleven to twelve weeks of intrauterine life. Osseous calcification of the ethmoid bone begins around 25 to 28 weeks of intrauterine life. The anterior ethmoid cells arise from a superior invagination of the middle meatus at around the 20th week. Usually, the ethmoidal sinuses are present at birth [13,14], representing the only pneumatized sinuses at that time.
Ethmoid sinuses are unique compared to the other sinuses because they arise from the cartilaginous nasal capsule, whereas the rest of the paranasal sinuses are the outgrowths of the ethmoid. The maxillary sinus starts as an outpouching of the ethmoid infundibulum and develops inferolaterally towards the maxillary bone. The frontal sinus develops as an extension of the anterior ethmoidal air cells. The sphenoid sinus develops from an invagination of the posterior ethmoid sinus or from the nasal mucosa into the posterior part of the cartilaginous nasal capsule [14,15]. Developmentally, the ethmoid sinus plays a key role in the formation of the rest of the paranasal sinuses, which develop through a complex process of pneumatization of the bones surrounding the nasal cavity, with the ethmoid sinus being the central structure, but not the sole origin of the other sinuses [15].
The maxillary sinus starts its development in the third gestational month. As mentioned earlier in this article, the development of the primordial ethmoidal infundibulum starts to appear around eleven to twelve weeks, and a channel develops infero-laterally towards the precursor of the maxillary bone to form the primordial maxillary sinus. At birth, the maxillary sinus is present as a small sac in the lateral nasal wall [16,17]. The maxillary sinus develops considerably between birth and three years and again between seven and twelve years. The floor of the maxillary sinus reaches its most inferior position at 20 years of age [16,17].
The sphenoidal sinus develops as an invagination of the nasal mucosa into the posterior part of the cartilaginous nasal capsules around the third month of gestation. The sphenoidal sinus is not present at birth, since its pneumatization will start between one and three years of life. Between ages six and seven, the sphenoid sinus extends inferiorly to the pterygoid canal and then posteriorly to the hypophyseal fossa by age eight. The sphenoid sinuses reach maturity around twelve to fourteen years of age and are housed centrally and posteriorly in the body of the sphenoid bone.
The frontal sinus is not visible at birth and will begin to develop around the second year of life, from an outgrowth of the anterior ethmoid cells extending into the frontal bone. At one to two years of age, pneumatization starts at the horizontal plate of the frontal bone, which advances superiorly by age three, reaching the orbital roof at four to seven years of age [10,13]. It becomes radiographically evident around five or six years of age, and the final size and morphology is achieved around the 20–25 years of age [6,17].
Development of the paranasal sinuses is an extremely complicated process, and the anatomy of the sinuses is highly variable, which represents a clear advantage for their use in personal identification.
Understanding the growth and development of the paranasal sinuses is important for accurate interpretation in juvenile remains and in cases where antemortem and postmortem records correspond to different stages of development. Prior to their full development, the paranasal sinuses do not show distinctive structural traits. Moreover, there is a lack of research regarding their applicability in forensic identifications before their complete development [18]. According to that, the ethmoidal and sphenoidal sinuses won’t be used for identification in individuals younger than 12 years of age, and the frontal and maxillary sinuses won’t be used in individuals younger than 20 years of age for identification purposes (Table 1).

Table 1.
Approximate age of initial radiographic appearance; approximate age of developmental completeness of the paranasal sinuses; and radiographic projections where the sinus can be visualized.
3. Imaging Techniques to Explore Paranasal Sinuses
As previously mentioned in this article, the identification using paranasal sinuses consists of a morphological comparison between the antemortem and postmortem images of these structures. The antemortem images are those taken in a clinical context while the individual was alive, whereas the postmortem images are those obtained from remains being analyzed.
Medical imaging of the cranial region includes a series of imaging techniques, dependent on the purpose of the analysis, which are commonly used in cases of diseases and trauma. Maxillofacial projections, dental radiographs, computed tomography (CT) scans, and magnetic resonance imaging (MRI) are commonly conducted on living individuals in clinical settings. These images may be of high value in forensic contexts (representing antemortem records), since they can be compared to the imaging obtained in the postmortem analysis of the remains (postmortem records) in order to achieve a positive identification or an exclusion.
3.1. Conventional Radiographs
Conventional radiographs consist of high-energy electromagnetic wave packets (referred to as photons) that have the ability to penetrate human tissues, generating an image according to the number of photons that are absorbed, scattered, and transmitted through the matter [19,20]. So that the darker greys correspond to lower-density tissues (such as fat or muscle) and whiter areas correspond to high-density materials (such as bone and metal).
Paranasal sinuses are visible in different skull projections that are frequently taken in the clinical context for diagnosis, treatment, and follow-up monitoring. The antero-posterior skull radiograph shows the frontal sinus morphology and structure very accurately; it can be observed as well in the occipitomental (or Waters) projection; this view also represents a good visualization of the overall maxillary sinus. The occipitofrontal (or Caldwell) projection shows mainly the maxillary sinus, although the frontal and anterior ethmoidal sinuses are also represented in this projection, the lateral projection of the skull may assist in the visualization of the sphenoidal sinus, and the frontal and maxillary sinuses can be observed in this projection, but their view it’s not very informative for identification purposes. The submentovertex (or Hirtz) projection allows the visualization of the sphenoidal sinus. Additionally, some dental radiographs allow for visualization of the maxillary sinuses. The panoramic radiographs, extensively used in the dental clinical context, show the inferior portion of the maxillary sinuses; periapical radiographs may also include the inferior portion of the maxillary sinus when taken in the upper premolar and molar areas [19,20]. Cranial radiographs are ideal for paranasal sinus analysis, specifically the frontal sinus (Table 1). The unique sinus morphology allows practitioners to compare antemortem and postmortem radiographs to identify areas of concordance to establish a positive identification or an exclusion. A key aspect in the comparison is to take the postmortem radiographs mimicking the projection of the antemortem radiograph as closely as possible, since differences in the angulation can lead to significant differences in the radiographic image. Moreover, radiation overexposure concerns that apply to clinical settings are not an issue when postmortem radiographs are taken.
3.2. Computed Tomography (CT)
Computed Tomography (CT) uses x-rays and computer processing to generate detailed cross-sectional images of the body. By rotating an x-ray source and detectors around the patient, CT scans capture multiple projections that are reconstructed into 2D or 3D images, allowing for high-resolution visualization of internal structures [21]. In the later years, Cone Beam Computed Tomography (CBCT) has been widely used in clinical settings, which employs a cone-shaped x-ray beam and a flat-panel detector, rotating around the patient to produce volumetric images. Unlike conventional CT, which uses a fan-shaped beam and multiple detector rows, CBCT is optimized for high-resolution imaging of hard tissues with a lower radiation dose, making it particularly useful in dentistry, maxillofacial surgery, and orthopedic imaging [21]. Since CT uses x-rays to obtain the image, the scale of grays observed in the tomographic imaging follows the same criteria as the conventional radiographs. The gray scale is analogous with how dense the structures being scanned are [22]. Cranial CT scans can be utilized in forensic contexts for frontal sinus comparisons, since paranasal sinuses are well visualized in CT scans as air cavities. Additionally, CT scans contain volumetric data that can be used to create three-dimensional (3D) models, which can be useful for research and in certain cases for identification.
3.3. Magnetic Resonance Imaging (MRI)
Magnetic Resonance Imaging (MRI) is another imaging technique that is comparable to CT imaging. However, MRI uses radio waves to create a detailed picture of the internal anatomical structures. Thus, the scale of grays in MRI represents variations in signal intensity, which depend on the relaxation times of hydrogen nuclei (protons) in different tissues [23]. So, MRI provides superior soft-tissue contrast compared to x-rays, making it ideal for examining soft tissues. While x-rays are less sensitive to soft-tissue variations and very effective in visualizing bones and other dense structures [23]. In the clinical context, MRIs of the paranasal sinuses are normally taken in patients with sinusitis, polyps, or any mass within the paranasal and maxillofacial area.
As CT scans and MRIs have become a more commonly used tool in the medical field in the last decades, they have become more available and a valuable source of antemortem records that can be used for comparison analyses in forensic contexts. Even through the advancements in imaging technology, radiography is still the most commonly available antemortem imaging technique and the most commonly used in the postmortem analyses, since forensic practitioners typically have radiography equipment readily accessible versus a CT or MRI scanner. However, as new digital imaging techniques develop and become more widely employed, it is important for forensic practitioners to understand the limitations and benefits of the imaging techniques and how to use them for postmortem vs. antemortem comparisons.
4. Postmortem Versus Antemortem Imaging Comparison
Forensic experts take the postmortem images and compare them with the antemortem records provided. Depending on the nature of antemortem records and the imaging technique available in the postmortem analysis, oftentimes forensic practitioners must combine different imaging techniques at the time of comparison. While the antemortem images can include a wide range of imaging techniques, the postmortem imaging techniques applied in the postmortem analysis will depend on the equipment available for the different forensic institutions. As mentioned, in most cases, conventional radiographs are the only imaging technique available in forensic settings.
Due to low-cost, non-invasive/non-destructive, fast imaging acquisition, and good quality of resolution and contrast, radiographs play a key role in clinical and forensic settings [24]. However, the image quality may present significant differences when comparing traditional or screen-film radiography (SFR) and digital radiography (DR). While SFR doesn’t allow post-processing adjustments, once the image is chemically fixed, over or underexposure irreversibly degrades the image quality [25] and the only attempts to improve it are through image adjustments in Photoshop, PowerPoint, or similar computer programs. Due to the post-processing adjustments applied to DR and the possibility to enhance low-contrast findings, this is the preferred technique nowadays [26]. DR was introduced in 1983, increasing its implementation in the 90s and early 2000s and presenting full dominance of the clinical setting from 2010 until the present day [26,27,28]. Thus, it is not unusual to be provided with antemortem SFR and compare them with postmortem DR, even though the sinuses margins and differentiation will present better quality in the digital images, the comparison between these two modalities of radiographs generally doesn’t present difficulties for forensic professionals.
The comparison between antemortem panoramic radiographs and postmortem periapical radiographs is commonly performed in cases utilizing the maxillary sinus. In these cases, only the lower part of the maxillary sinuses can be compared (Figure 2).
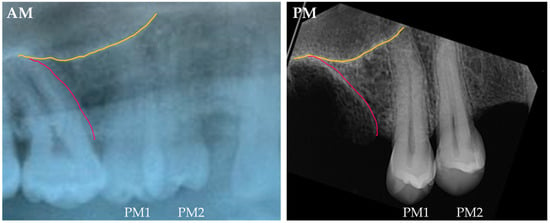
Figure 2.
Comparison between an antemortem panoramic radiograph fragment (AM) and postmortem periapical radiograph (PM) of the right maxillary premolar and molar area. The inferior border (or the floor) of the maxillary sinus is highlighted in yellow, and the 1st and 2nd premolars are labeled as PM1 and PM2, and the mesial alveolar portion of the molar is highlighted in pink. This comparison depicts consistent morphologies between the AM and PM radiographs, where the relationship of the inferior part of the maxillary sinus with the dental roots is key for the comparison. Source: Department of Applied Forensic Sciences at Mercyhurst University casework.
Since the first clinical use of computed tomography in 1971, its clinical application increased rapidly through the 1980s until the 2000s, when CT techniques became a key component of modern radiology [29,30,31,32]. Due to the extended use of the CT-scans in the clinical context, cranial CTs are frequently provided as antemortem medical records, which can be compared to postmortem imaging, which in most cases consists of radiography. Although CT scans contain volumetric data, and despite the current extensive research in three-dimensional comparison and overlay of the paranasal sinuses, 3D renderings of the sinuses aren’t generally of great use in forensic identification daily casework, since most of the comparisons are conducted between an antemortem CT scan and a postmortem radiograph, given the accessibility to this technique in the forensic institutions. According to that, forensic practitioners often use reformatting tools rather than using 3D reconstructions, which do not offer information on the internal structure of the sinuses (Figure 3).
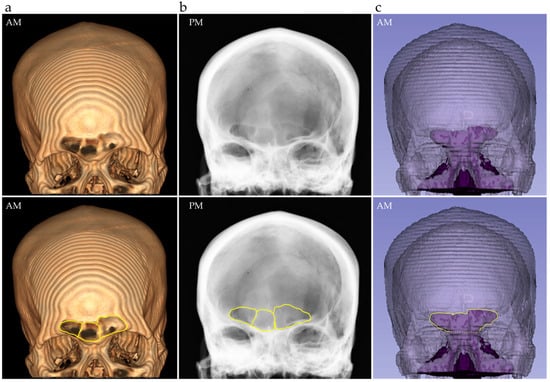
Figure 3.
Antemortem (AM) 3D rendering reconstruction from a CBCT scan (a); postmortem (PM) anterior posterior cranial radiograph (b); volumetric reconstruction of frontal sinus in AM CBCT scan (c). The frontal sinus outline and septa are highlighted in yellow in the lower images. The cut in the CBCT in (a) was conducted at a level that allows the visualization of the overall sinus, thus can be compared with the postmortem radiograph (b), while the volumetric reconstruction (c) lacks the ultrastructure information visible in the postmortem radiograph. Source: Department of Applied Forensic Sciences at Mercyhurst University casework.
5. Value and Use of Paranasal Sinuses in Human Identification
The individualizing potential of paranasal sinuses due to their morphological variability and uniqueness makes these structures highly reliable for postmortem versus antemortem imaging comparisons [2].
The frontal sinus has been extensively researched as an individualizing structure, presenting unique architecture that differs even in monozygotic twins [33,34,35,36]. Its morphological variation ranges from minimal expression (or even aplasia) to complex labyrinthic formations, presenting variation in the presence or absence and asymmetry of right and left lobes, sinus outline morphology, and number and location of septa [37,38]. In the first author’s experience, the location and morphology of the crista galli of the ethmoid and the frontal sinus lobes, are informative structures that can add to the comparisons (Figure 4), but in order to use the crista galli in the comparison, the PM image should mimic in high detail the AM in terms of projection and positioning of the cranium. Moreover, the anatomical variations of the frontal sinus aren’t significantly influenced by sex or population affinity [38], and the highly individualistic morphology generally supersedes more subtle differences related to imaging orientation or image quality concerns [37], giving this structure great value for personal identification in forensic casework (Figure 5).
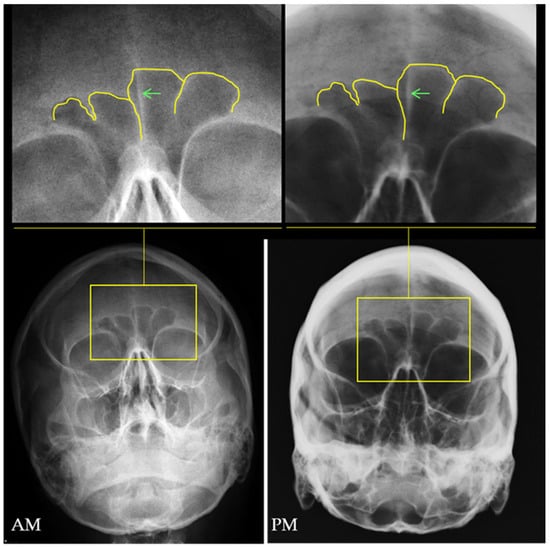
Figure 4.
Frontal sinus comparison between an antemortem (AM) Waters projection and a postmortem (PM) radiograph of the cranium in similar orientation. The frontal sinus outline and septa are highlighted in yellow and the crista galli is indicated by the green arrow in the superior images. Source: Department of Applied Forensic Sciences at Mercyhurst University casework.
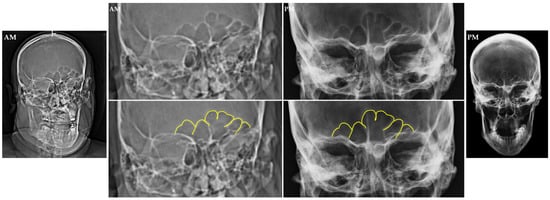
Figure 5.
Frontal sinus comparison between antemortem (AM) and postmortem (PM) radiographs. The frontal sinus outline and septa are highlighted in yellow in the lower images. Even though slightly different projections are observed between the AM and PM radiographs, the sinus morphology can be assessed and shows consistency between the AM and PM images, mainly in terms of number and morphology of lobes and septa. Source: Department of Applied Forensic Sciences at Mercyhurst University casework.
The sphenoidal sinus has shown morphological uniqueness; however, three-dimensional (3D) techniques are preferred for comparison; most of the recent research focuses on 3D–3D superimposition [5,39], which would be applicable in cases where antemortem and postmortem three-dimensional images are available. In radiographs, the sphenoidal sinus can be properly visualized in cranial lateral projections. In cases using these types of images, it is the authors’ advice to use other anatomical structures in combination with the sphenoidal sinus, such as the clinoid processes, cranial sutures, or the meningeal grooves morphology, since this projection doesn’t provide much detail of its architecture (Figure 6).
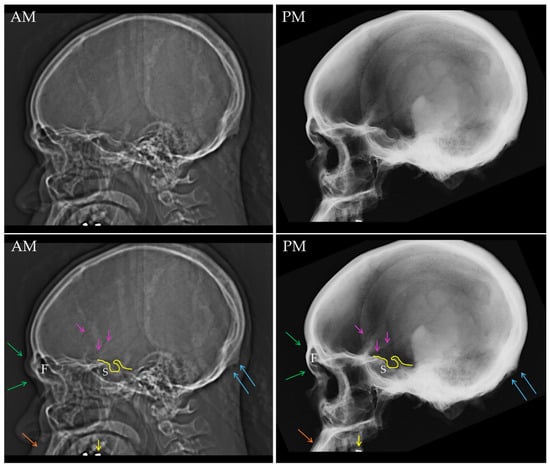
Figure 6.
Comparison between a lateral view of the cranium of the antemortem CBCT scan (AM) and the lateral radiograph of the remain’s cranium (PM). Since this view doesn’t offer a detailed image of the frontal (F) and sphenoidal (S) sinuses, other skeletal features were included in the comparison such as the morphology of the clinoid processes and the overall sella turcica (outlined in yellow), glabella (green arrows), meningeal grooves (purple arrows), the inion and an entheses located inferiorly to it (blue arrows), maxillary prognatism (orange arrow), and the presence of a dental restoration in the upper left 2nd molar (yellow arrow). Source: Department of Applied Forensic Sciences at Mercyhurst University casework.
Although some studies have reported the ethmoidal sinus uniqueness and use for human identification cases [40,41], it is the least explored of the paranasal sinuses for forensic identification purposes. This may be due to the difficulty of visualizing the ethmoidal sinus in most common radiographical projections. Rather than the ethmoidal sinus, the crista galli of the ethmoid, visualized in projections capturing the frontal sinus, has shown to be of high value in the comparison.
The maxillary sinus has been widely researched and used for human identification purposes due to its morphological variation and the clear visualization in several radiographical modalities such as panoramic, AP/PA cranial projections, Waters and lateral projections, as well as periapical radiographs. Although some research has suggested the influence of sex in the maxillary sinus volume, statistical analyses did not show significant differences between males’ and females’ data [39]. Maxillary body contour and septal pattern provide useful data for the postmortem vs. antemortem comparisons. Maxillary sinus morphological changes may occur after posterior tooth loss and as a result of sinus lift procedures prior to dental implant surgery, so that extractions and sinus bone graft surgery should be considered as a potential source of inconsistencies due to the sinus pneumatization [42,43,44]. In comparisons using the maxillary sinus, it is of high importance to rely not only on the sinus morphology but also on the relationship of the sinus floor with other anatomical structures such as the dental roots or the alveolar bone (Figure 7).
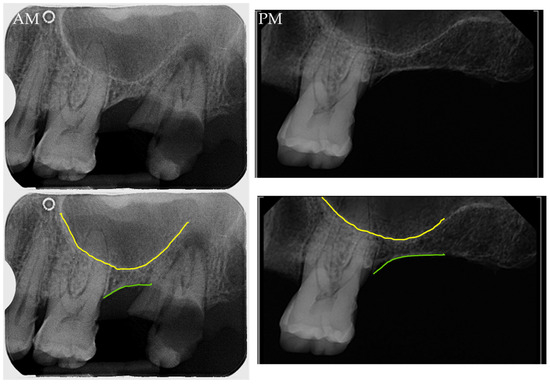
Figure 7.
Comparison of the antemortem (AM) and the postmortem (PM) periapical radiographs, where the floor of the maxillary sinus is highlighted in yellow and the lower limit of the maxillary bone in the alveolar region is highlighted in green. Although the third molar is present in the AM and missing in the PM image, the sinus morphology and relationship with the first molar and the distal maxillary bone is consistent in both images. Additionally, the relationship between the sinus floor and the first molar’s root is maintained in the AM and the PM images. Source: Department of Applied Forensic Sciences at Mercyhurst University casework.
6. Limitations of the Use of Paranasal Sinuses for Identification
Despite the usefulness of paranasal sinuses for forensic identification purposes, some limitations must be taken into account at the time of applying the antemortem versus postmortem morphological comparison of the paranasal sinuses.
The quality of the images to be compared can impact the process. Antemortem images are taken in the clinical context of diagnostic, treatment plan, or follow-up of diseases and trauma; they are not optimized for forensic purposes, which can result in resolution or contrast issues, as well as the presence of artifacts. Although these limitations are more significant in non-digital radiographs (SFR), since no post-processing is possible, other imaging techniques, such as CT scan, can present quality limitations in the resolution, noise, and slice thickness [28,29,45,46]. Moreover, when the antemortem image only shows a part of the sinus (due to the clinical question), only partial comparisons can be conducted, but they still offer a valuable assessment. Although nowadays radiography dominates the forensic imaging realm, other techniques such as CT scans are becoming more accessible for forensic practitioners.
Another limitation is the use of different imaging techniques in the antemortem and postmortem data. Comparing two-dimensional with three-dimensional images introduces challenges for correlating the different anatomical structures and their morphological traits. Radiographical superimposition of structures, geometric distortions, and contrast can limit the differentiation of certain traits that can be easily distinguished in three-dimensional imaging techniques [37]. The understanding of anatomy, image acquisition, interpretation, and the post-processing management when available can assist in lowering the impact of different imaging techniques comparison [47].
Cases of hypoplasia and aplasia of the sinus can impact the assessment of this structure since the lack of distinctive traits impairs the identification. However, these are rare developmental anomalies, and their frequency in the population has been explored mainly for anatomical and clinical purposes. Total aplasia paranasal sinus is an extremely rare condition; few cases have been reported in the scientific literature [48,49,50]. Bilateral frontal sinus aplasia is found in 1–5% of the population, while unilateral aplasia frequency corresponds to 4–15% of the population, and hypoplasia is present in 14–15% of the population [51,52,53]. Maxillary sinus hypoplasia is a rare anomaly found in 1.73 to 10.5% of the population, not only related to developmental causes but also to trauma and acquired diseases [54]. Sphenoidal aplasia has been reported in 1% or less of the population, and it has been related to skeletal diseases [55]. The cases of hypoplasia are classified according to the location of the rudimentary pneumatization, so they can be conchal (1–3% of the cases), presellar (10% of the cases), or postsellar (90% of he cases of hypoplasia) [56]. Additionally, ethmoidal sinus hypoplasia has been described in seldom cases associated with other sinus anomalies [57]. So that, although sinus aplasia and hypoplasia cannot per se lead to a positive identification, the fact of presenting this rare anomaly is valuable information, which, combined with other skeletal traits, can result in a positive identification. Moreover, these frequencies can offer a quantitative approach in the identification, through random match probabilities or likelihood ratios calculation [53].
As mentioned above, changes in the paranasal sinus morphology can occur as a result of trauma and acquired diseases. Fractures involving the maxillofacial structures, such as orbital or Le Fort fractures, can affect the paranasal walls and change their morphology by displacement of the septa or new bone formation in the fracture callus [58]. Chronic inflammatory processes and infections, such as sinusitis and otitis, have been related to sinus hypoplasia. Additionally, surgeries performed in the sinus region, such as maxillary sinus lift previous to dental implant placement, tumor excision, and other maxillofacial procedures affecting the paranasal sinuses, can change the sinus morphology [54]. Forensic practitioners should be familiar with these types of procedures in order to identify them and conduct a proper interpretation of the sinus changes and their causes.
Finally, another limitation of the use of paranasal sinuses in forensic human identification is that the comparison between antemortem and postmortem imaging should be conducted once the sinuses have completed their development. So, sinus morphology in cases involving juvenile individuals, where the sinuses are under development, is not reliable. Developing structures lack informative structures for identification purposes. Moreover, research efforts are geared towards adults; thus, no scientific evidence or validation is available for juvenile individuals.
7. Conclusions
The anatomy and development of the four paranasal sinuses (frontal, maxillary, sphenoidal, and ethmoidal) is a complicated process that results in a high degree of variability. This high variability makes the paranasal sinuses a great region of interest to forensic practitioners looking to utilize the sinuses as a means of positive identification. The frontal and maxillary sinuses have been extensively researched due to their unique architecture and convenient assessment in several cranial radiographic projections. All their morphological variations, including the sinus outline, number and location of septa, asymmetries, and relationship with nearby anatomical structures, are highly individualistic and not influenced by sex or population affinity. The sphenoidal and ethmoidal sinuses have been less explored, likely due to their difficult visualization in some cranial radiographic projections. In general terms, 3D imaging techniques are often preferred for their assessment, although they are not always accessible in forensic institutions (such as medical examiners/coroners’ offices or institutes of legal medicine). Imaging comparison of the sinuses can come with challenges, especially because of poor quality imges or when different imaging modalities are used in the comparison of the AM and PM images; Additionally, developmental anomalies such as hypoplasia and aplasia, although rare, lack of distinctive traits for personal identification alone; postnatal changes such as acquired diseases or surgical procedures are limitations that must be taken into account when using paranasal sinuses in forensic identification casework. Moreover, frontal and maxillary sinuses shouldn’t be used in individuals younger than 20 years until their complete development. Sphenoidal and ethmoidal sinuses, although less informative, can be used in younger individuals (from 12 years old onwards). Understanding the development of paranasal sinuses, the imaging techniques applied for their visualization, as well as the principles of identification, is key to conducting proper antemortem vs. postmortem comparisons and effectively utilizing paranasal sinuses in forensic identification contexts.
Author Contributions
Conceptualization: J.A.-G.; Case Analysis: J.A.-G., H.S. and B.M.; Writing, review, and editing: J.A.-G., H.S. and B.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were generated in this article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Adserias-Garriga, J.; Feirstein, S.; Bell, D.; Skropits, H.; Dirkmaat, D.C. Human identification through forensic skeletal analysis: Three case reviews. Forensic Sci. Res. 2024, 9, owae053. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Palamenghi, A.; Borlando, A.; De Angelis, D.; Sforza, C.; Cattaneo, C.; Gibelli, D. Exploring the potential of cranial non-metric traits as a tool for personal identification: The never-ending dilemma. Int. J. Leg. Med. 2021, 135, 2509–2518. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Verna, E.; Piercecchi-Marti, M.D.; Chaumoitre, K.; Bartoli, C.; Leonetti, G.; Adalian, P. Discrete traits of the sternum and ribs: A useful contribution to identification in forensic anthropology and medicine. J. Forensic Sci. 2013, 58, 571–577. [Google Scholar] [CrossRef] [PubMed]
- Macaluso, P.J.; Lucena, J. Morphological variations of the anterior thoracic skeleton and their forensic significance: Radiographic findings in a Spanish autopsy sample. Forensic Sci. Int. 2014, 241, 220-e1. [Google Scholar] [CrossRef] [PubMed]
- Cappella, A.; Gibelli, D.; Cellina, M.; Mazzarelli, D.; Oliva, A.G.; De Angelis, D.; Sforza, C.; Cattaneo, C. Three-Dimensional Analysis of Sphenoid Sinus Uniqueness for Assessing Personal Identification: A Novel Method Based on 3D-3D Superimposition. Int. J. Leg. Med. 2019, 133, 1895–1901. [Google Scholar] [CrossRef]
- da Silva, R.F.; Prado, F.B.; Caputo, I.G.; Devito, K.L.; Botelho, T.L.; Daruge, J.E. The forensic importance of frontal sinus radiographs. J. Forensic Leg. Med. 2009, 16, 18–23. [Google Scholar] [CrossRef] [PubMed]
- Christensen, A.M.; Anderson, B.E. Methods of Personal Identification. In Forensic Anthropology: An Introduction; Tersigni-Tarrant, M.A., Shirley, N.R., Eds.; CRC Press: Boca Raton, FL, USA, 2013; pp. 397–420. [Google Scholar]
- Murphy, W.A.; Spruill, F.G.; Gantner, G.E. Radiologic identification of unknown human remains. J. Forensic Sci. 1980, 25, 727–735. [Google Scholar] [CrossRef] [PubMed]
- Whyte, A.; Boeddinghaus, R. The maxillary sinus: Physiology, development and imaging anatomy. Dentomaxillofac Radiol. 2019, 48, 20190205, Erratum in Dentomaxillofac Radiol. 2019, 48, 20190205c. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cappello, Z.J.; Minutello, K.; Dublin, A.B. Anatomy, Head and Neck, Nose Paranasal Sinuses. [Updated 11 February 2023]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: https://www.ncbi.nlm.nih.gov/books/NBK499826/ (accessed on 15 March 2025).
- Jones, N. The nose and paranasal sinuses physiology and anatomy. Adv. Drug Deliv. Rev. 2001, 51, 5–19. [Google Scholar] [CrossRef] [PubMed]
- Ogle, O.E.; Weinstock, R.J.; Friedman, E. Surgical anatomy of the nasal cavity and paranasal sinuses. Oral Maxillofac. Surg. Clin. N. Am. 2012, 24, 155–166, vii. [Google Scholar] [CrossRef] [PubMed]
- Vaid, S.; Vaid, N. Normal Anatomy and Anatomic Variants of the Paranasal Sinuses on Computed Tomography. Neuroimaging Clin. N. Am. 2015, 25, 527–548. [Google Scholar] [CrossRef] [PubMed]
- Zalzal, H.G.; O’Brien, D.C.; Zalzal, G.H. Pediatric Anatomy: Nose and Sinus. Oper. Tech. Otolaryngol.-Head Neck Surg. 2018, 29, 44–50. [Google Scholar] [CrossRef]
- Márquez, S.; Tessema, B.; Clement, P.A.; Schaefer, S.D. Development of the ethmoid sinus and extramural migration: The anatomical basis of this paranasal sinus. Anat. Rec. 2008, 291, 1535–1553. [Google Scholar] [CrossRef] [PubMed]
- Alqahtani, H.; Basuhail, S.; Alsulaimani, F.; Zawawi, K.H.; Barayan, M.; Al Turki, G.; Abbassy, M.A. The Relationship Between Maxillary Sinus Volume and Different Cephalometric Characteristics in Orthodontics. Contemp. Clin. Dent. 2023, 14, 191–200. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lee, S.; Fernandez, J.; Mirjalili, S.A.; Kirkpatrick, J. Pediatric paranasal sinuses—Development, growth, pathology & functional endoscopic sinus surgery. Clin. Anat. 2022, 35, 745–761. [Google Scholar] [CrossRef]
- Abdulrazak, N.; Butaric, L.N.; Garvin, H.M. Age-Related Changes to Frontal Sinus Traits and Implications for Forensic Identification. Forensic Anthropol. 2023, 6, 192. [Google Scholar] [CrossRef]
- Whaites, E. Essentials of Dental Radiography and Radiology, 3rd ed; Chruchill Livingston-Elsevier: London, UK, 2003; pp. 15–25. [Google Scholar]
- Kardjodkar, F.R. (Ed.) Textbook of Dental and Maxillofacial Radiology; Jaypee Borthers Medical Publishers: New Delhi, India, 2009; pp. 145–208. [Google Scholar]
- Scarfe, W.C.; Angelopoulos, C. Cone Beam Computed Tomography: Principles and Applications in Dentistry. J. Calif. Dent. Assoc. 2018, 46, 7–13. [Google Scholar]
- Dieckmeyer, M.; Sollmann, N.; Kupfer, K.; Löffler, M.T.; Paprottka, K.J.; Kirschke, J.S.; Baum, T. Computed Tomography of the Head: A Systematic Review on Acquisition and Reconstruction Techniques to Reduce Radiation Dose. Clin. Neuroradiol. 2023, 33, 591–610. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bushberg, J.T.; Seibert, J.A.; Leidholdt, E.M.; Boone, J.M. The Essential Physics of Medical Imaging, 3rd ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2012. [Google Scholar]
- Bansal, G.J. Digital radiography. A comparison with modern conventional imaging. Postgrad. Med. J. 2006, 82, 425–428. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Seeram, E. Physical Principles and Quality Control. In Digital Radiography; Springer Nature: Dordrecht, The Netherlands, 2019. [Google Scholar] [CrossRef]
- Decker, S.J.; Braileanu, M.; Dey, C.; Lenchik, L.; Pickup, M.; Powell, J.; Tucker, M.; Probyn, L. Forensic Radiology: A Primer. Acad. Radiol. 2019, 26, 820–830. [Google Scholar] [CrossRef] [PubMed]
- Sonoda, M.; Takano, M.; Miyahara, J.; Kato, H. Computed radiography utilizing scanning laser stimulated luminescence. Radiology 1983, 148, 833–838. [Google Scholar] [CrossRef] [PubMed]
- Martin, C. Optimization in general radiography. Biomed. Imaging Interv. J. 2007, 3, e18. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Willemink, M.J.; Noël, P.B. The evolution of image reconstruction for CT—From filtered back projection to artificial intelligence. Eur. Radiol. 2019, 29, 2185–2195. [Google Scholar] [CrossRef] [PubMed]
- Smith-Bindman, R.; Miglioretti, D.L.; Johnson, E.; Lee, C.; Feigelson, H.S.; Flynn, M.; Greenlee, R.T.; Kruger, R.L.; Hornbrook, M.C.; Roblin, D.; et al. Use of diagnostic imaging studies and associated radiation exposure for patients enrolled in large integrated health care systems, 1996–2010. JAMA 2012, 307, 2400–2409. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Siegel, E.; Reiner, B. Work flow redesign: The key to success when using PACS. Am. J. Roentgenol. 2002, 178, 563–566. [Google Scholar] [CrossRef] [PubMed]
- Hounsfield, G.N. Computerized transverse axial scanning (tomography): Part 1. Description of system. Br. J. Radiol. 1973, 46, 1016–1022. [Google Scholar] [CrossRef] [PubMed]
- Christensen, A.M. Assessing the variation in individual frontal sinus outlines. Am. J. Phys. Anthr. 2005, 127, 291–295. [Google Scholar] [CrossRef] [PubMed]
- Ubelaker, D.H.; Shamlou, A.; Kunkle, A. Contributions of forensic anthropology to positive scientific identification: A critical Review. Forensic Sci. Res. 2018, 4, 45–50. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Park, J.A.; Lee, Y.J.; Yeo, I.S.; Koh, K.S.; Song, W.C. Three-dimensional linear and volumetric computed tomography analysis of the frontal sinus. Anat. Cell Biol. 2022, 55, 142–147. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Butaric, L.N.; Campbell, J.L.; Garvin, H.M. Visual assessment for frontal sinus radiographic identifications: Documenting accuracy and exploring the effects of experience. J. Forensic Sci. 2025, 70, 415–429. [Google Scholar] [CrossRef]
- Butaric, L.N.; Richman, A.; Garvin, H.M. The Effects of Cranial Orientation on Forensic Frontal Sinus Identification as Assessed by Outline Analyses. Biology 2022, 11, 62. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shamlou, A.A.; Tallman, S.D. Frontal Sinus Morphological and Dimensional Variation as Seen on Computed Tomography Scans. Biology 2022, 11, 1145. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Palamenghi, A.; Cappella, A.; Cellina, M.; De Angelis, D.; Sforza, C.; Cattaneo, C.; Gibelli, D. Assessment of Anatomical Uniqueness of Maxillary Sinuses Through 3D–3D Superimposition: An Additional Help to Personal Identification. Biology 2023, 12, 1018. [Google Scholar] [CrossRef]
- Robles, M.; Nakhaeizadeh, S.; Rando, C.; Morgan, R.M. Human identification: An investigation of 3D models of paranasal sinuses to establish a biological profile on a modern UK population. Int. J. Legal. Med. 2024, 138, 1411–1424. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jablonski, N.G.; Shum, B.S. Identification of unknown human remains by comparison of antemortem and postmortem radiographs. Forensic Sci. Int. 1989, 42, 221–230. [Google Scholar] [CrossRef] [PubMed]
- Itokawa, T.; Yamaguchi, K.; Yagi, K.; Araki, K.; Sato, D.; Munakata, M. Changes in Maxillary Sinus Structure Due to Tooth Loss and the Effects of Sex and Aging on CBCT Before Maxillary Sinus Augmentation: A Cross-Sectional Study of 120 Patients. Bioengineering 2025, 12, 240. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yamaguchi, K.; Munakata, M.; Kataoka, Y.; Uesugi, T.; Shimoo, Y. Effects of missing teeth and nasal septal deviation on maxillary sinus volume: A pilot study. Int. J. Implant Dent. 2022, 8, 19. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lim, H.C.; Kim, S.; Kim, D.H.; Herr, Y.; Chung, J.H.; Shin, S.I. Factors affecting maxillary sinus pneumatization following posterior maxillary tooth extraction. J. Periodontal Implant Sci. 2021, 51, 285–295. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ford, J.; Decker, S. Computed tomography slice thickness and its effects on three-dimensional reconstruction of anatomical structures. J. Forensic Radiol. Imaging 2016, 4, 43–46. [Google Scholar] [CrossRef]
- Heinrich, A. Automatic personal identification using a single CT image. Eur. Radiol. 2025, 35, 2422–2433. [Google Scholar] [CrossRef] [PubMed]
- Heimer, J.; Gascho, D.; Gentile, S.; Hatch, G.M.; Thali, M.J.; Ruder, T.D. Antemortem identification by fusion of MR and CT of the paranasal sinuses. Forensic Sci. Med. Pathol. 2017, 13, 375–378. [Google Scholar] [CrossRef] [PubMed]
- Kalabalık, F.; Aytugar, E. Total Aplasia of the Paranasal Sinuses: A Rare Presentation. J. Res. Med. Dent. Sci. 2022, 10, 01–04. [Google Scholar]
- Joshi, A.; Sundarray, C.; Sahoo, K.A. Bilateral total aplasia of paranasal sinuses: A rare case report. Clin. Rhinol. Int. J. 2015, 8, 124–126. [Google Scholar] [CrossRef]
- Celik, H.H.; Altan, A. Total aplasia of the paranasal sinuses. J. Clin. Anal. Med. 2013, 4, 195–197. [Google Scholar]
- Yüksel Aslier, N.G.; Karabay, N.; Zeybek, G.; Keskinoğlu, P.; Kiray, A.; Sütay, S.; Ecevit, M.C. The classification of frontal sinus pneumatization patterns by CT-based volumetry. Surg. Radiol. Anat. 2016, 38, 923–930. [Google Scholar] [CrossRef] [PubMed]
- Ali, B.; Nadeem, Z.; Naeem, M.; Arif, K.; Zaman, A.; Noor, A.; Zahid, M.H.; Mustafa, R.; Akilimali, A.; Ago, J.L. Evaluation of the Frequency of Anatomic Variations of the Paranasal Sinus Region by Using Multidetector Computed Tomography: A Hospital-Based Cross-Sectional Study. Health Sci. Rep. 2025, 8, e70535. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Trant, M.; Christensen, A.M. Frontal Sinus Absence Rates in Various Populations Implications for Forensic Identification. In Forensic Anthropology; University of Florida: Gainesville, FL, USA, 2018; Volume 1. [Google Scholar]
- Erdem, T.; Aktas, D.; Erdem, G.; Miman, M.C.; Ozturan, O. Maxillary sinus hypoplasia. Rhinology 2002, 40, 150–153. [Google Scholar] [PubMed]
- Cakur, B.; Sümbüllü, M.A.; Yılmaz, A.B. A retrospective analysis of sphenoid sinus hypoplasia and agenesis using dental volumetric CT in Turkish individuals. Diagn. Interv. Radiol. 2011, 17, 205–208. [Google Scholar] [CrossRef] [PubMed]
- Peele, J.C. Unusual anatomical variations of the sphenoid sinuses. Laryngoscope 1957, 67, 208–237. [Google Scholar] [CrossRef] [PubMed]
- Güven, D.G.; Yilmaz, S.; Ulus, S.; Subaşi, B. Combined aplasia of sphenoid, frontal, and maxillary sinuses accompanied by ethmoid sinus hypoplasia. J. Craniofacial Surg. 2010, 21, 1431–1433. [Google Scholar] [CrossRef] [PubMed]
- Lenkeit, C.P.; Lofgren, D.H.; Shermetaro, C. Maxillary Sinus Fracture (Archived). In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).