The Fracture Strength of Acrylic Palatal Prostheses After Microwave and Chlorhexidine Disinfection: A Comparative In Vitro Study
Abstract
1. Introduction
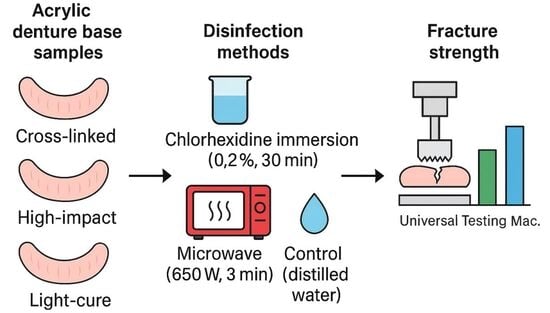
2. Materials and Methods
2.1. Fabrication of Test Specimens
- Conventional heat-cure acrylic resin;
- High-impact acrylic resin;
- Light-cure acrylic resin.
2.2. Specimen Grouping and Disinfection Protocols
- Group I (Control Group): Specimens were stored in distilled water at room temperature (25 ± 0.5 °C) for four weeks before testing.
- Group II: Specimens were disinfected by immersion in 160 mL of 0.20% chlorhexidine digluconate solution (Kin, Laboratorios Kin, Barcelona, Spain) for 30 min, twice weekly, over four weeks [9].
- Group III: Specimens underwent disinfection using a conventional household microwave at 650 W for three minutes, twice weekly, for four weeks [9,17,18]. Each specimen was placed in a 250 mL glass flask containing 160 mL of distilled water. The microwave used was a standard unmodified domestic model (Kenwood MW577), equipped with a rotating turntable to ensure even exposure, with the flask consistently positioned at the centre of the turntable. Its specifications included a power consumption of 1450 W, an output power of 900 W, a turntable diameter of 316 mm, and an operating voltage of 230 V at 60 Hz (Kenwood Ltd., Havant, Hampshire, UK).

2.3. Fracture Strength Testing
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
- Cross-linked acrylic demonstrated the highest reliability in fracture strength across all disinfection protocols.
- High-impact acrylic showed comparable average strength but was more sensitive to the type of disinfection applied.
- Microwave disinfection led to a statistically significant reduction in fracture strength, particularly in light-cured acrylics, though all materials remained within clinically acceptable limits.
- Immersion in 0.2% chlorhexidine for 30 min, twice weekly, had no significant impact on fracture strength, indicating its compatibility with the mechanical integrity of acrylic resins.
- Importantly, repeated chlorhexidine exposure and uncontrolled microwave parameters (power and duration) may adversely affect the structural integrity of denture base materials, underscoring the need for proper disinfection protocols and strict regulation of concentration, immersion time, and irradiation settings.
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ANOVA | A one-way analysis of variance |
| Chx | Chlorhexidine |
| g | Gram |
| h | Hour(s) |
| Hz | Hertz |
| ISO | International Organization for Standardization |
| KN | Kilonewton |
| Mac. | Machine |
| min | Minute(s) |
| mL | Millilitre |
| mm | Millimetre |
| N | Newton |
| n | Number |
| p | p-value (the calculated probability) |
| PMMA | Poly(methyl methacrylate) |
| PEEK | Polyetheretherketone |
| SD | Standard Deviation |
| SE | Standard Error |
| SPSS | Statistical Package for the Social Sciences |
| T | t-statistic |
| UTM | Universal Testing Machine |
| UV | Ultraviolet curing |
| V | Volt (Voltage) |
| W | Watt |
| wt% | Weight Percentage |
| °C | Degree Celsius |
| % | Percent |
| = | Equals |
| < | Less than |
| 3D | Three-Dimensional |
| α | (alpha) is the threshold for significance, commonly set at 0.05. |
References
- Deb, S. Polymers in dentistry. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 1998, 212, 453–464. [Google Scholar] [CrossRef] [PubMed]
- Al-Kadi, F.K.; Adbulkareem, J.F.; Azhdar, B.A. Evaluation of the Mechanical and Physical Properties of Maxillofacial Silicone Type A-2186 Impregnated with a Hybrid Chitosan–TiO2 Nanocomposite Subjected to Different Accelerated Ageing Conditions. Biomimetics 2023, 8, 539. [Google Scholar] [CrossRef]
- Xu, X.; He, L.; Zhu, B.; Li, J.; Li, J. Advances in polymeric materials for dental applications. Polym. Chem. 2017, 8, 807–823. [Google Scholar] [CrossRef]
- Hassan, M.; Asghar, M.; Din, S.U.; Zafar, M.S. Chapter 8. In Thermoset Polymethacrylate-Based Materials for Dental Applications; Elsevier: Amsterdam, The Netherlands, 2019; pp. 273–308. [Google Scholar]
- Modiga, C.; Stoia, A.; Leretter, M.T.; Chiş, A.C.; Ardelean, A.-V.; Azar, E.-R.; Kapor, G.; Pop, D.-M.; Romînu, M.; Sinescu, C.; et al. Mechanical Assessment of Denture Polymers Processing Technologies. J. Funct. Biomater. 2024, 15, 234. [Google Scholar] [CrossRef] [PubMed]
- Zafar, M.S. Prosthodontic Applications of Polymethyl Methacrylate (PMMA): An Update. Polymers 2020, 12, 2299. [Google Scholar] [CrossRef] [PubMed]
- Alqutaibi, A.Y.; Baik, A.; Almuzaini, S.A.; Farghal, A.E.; Alnazzawi, A.A.; Borzangy, S.; Aboalrejal, A.N.; AbdElaziz, M.H.; Mahmoud, I.I.; Zafar, M.S. Polymeric Denture Base Materials: A Review. Polymers 2023, 15, 3258. [Google Scholar] [CrossRef]
- Elshereksi, N.W.; Kundie, F.A.; Muchtar, A.; Azhari, C.H. Protocols of improvements for PMMA denture base resin: An overview. J. Met. Mater. Miner. 2022, 32, 1–11. [Google Scholar] [CrossRef]
- Gupta, R.; Aggarwal, R.; Aeran, H. Comparison of Various Methods of Disinfecting Acrylic Dentures: Assessment of Antimicrobial Efficacy and Dimensional Changes. Int. J. Oral Health Dent. 2016, 2, 143. [Google Scholar] [CrossRef]
- Elhagali, A.F.; Sharaf, M.Y.; Abd El-Aziz, M.E.-S.A.; Ali Bayiumy, A.S.; Refaei, M.A.A.; Al-Agamy, A.H.; Ali, A.; Elakel, A.; Altayyar, R.; Alzahrani, R.; et al. The Effects of Different Chemical Disinfectants on the Strength, Surface, and Color Properties of Conventional and 3D-Printed Fabricated Denture Base Materials. Prosthesis 2025, 7, 24. [Google Scholar] [CrossRef]
- Çakmak, G.; Hess, J.A.; Dönmez, M.B.; Yılmaz, D.; Alhotan, A.; Schimmel, M.; Peutzfeldt, A.; Yilmaz, B. Effect of polishing and denture cleansers on the surface roughness of new-generation denture base materials and their colour change after cleansing. J. Prosthodont. 2024, 33, 783–790. [Google Scholar] [CrossRef]
- Webb, B.C.; Thomas, C.J.; Harty, D.W.S.; Willcox, M.D. Effectiveness of two methods of denture sterilisation. J. Oral Rehabil. 1998, 25, 416–423. [Google Scholar] [CrossRef] [PubMed]
- Polyzios, G.L.; Zissis, A.J.; Yannikakis, S.A. The effect of glutaraldehyde and microwave disinfection on some properties of acrylic denture resin. Int. J. Prosthodont. 1995, 8, 150–154. [Google Scholar]
- Andrucioli, M.C.; deMacedo, L.D.; Panzeri, H.; Lara, E.G.; Paranhos, H.D. Comparison of two cleansing pastes for the removal of biofilm from dentures and palatal lesions in patients with atrophic chronic candidiasis. Braz. Dent. J. 2004, 15, 220–224. [Google Scholar] [CrossRef] [PubMed]
- Pavan, S.; Arioli Filho, J.N.; dos Santos, P.H.; de Mollo, F.A., Jr. Effect of microwave treatments on dimensional accuracy of maxillary acrylic resin denture base. Braz. Dent. J. 2005, 16, 119–123. [Google Scholar] [CrossRef]
- Basavanna, J.M.; Jujare, R.H.; Varghese, R.K.; Singh, D.; Gaurav, A. Effects of Laboratory Disinfecting Agents on Dimensional Stability of Three Commercially Available Heat-Cured Denture Acrylic Resins in India: An In-Vitro Study. J. Clin. Diagn. Res. 2016, 10, ZC27–ZC31. [Google Scholar] [CrossRef]
- Yildirim-Bicer, A.Z.; Peker, I.; Akca, G.; Celik, I. In Vitro Antifungal Evaluation of Seven Different Disinfectants on Acrylic Resins. BioMed Res. Int. 2014, 519098. [Google Scholar] [CrossRef]
- Consani, R.L.X.; Vieira, E.H.M.; Mesquita, M.F.; Mendes, W.B.; Arioli-Filho, J.N. Effect of microwave disinfection on physical and mechanical properties of acrylic resins. Braz. Dent. J. 2008, 19, 348–353. [Google Scholar] [CrossRef]
- Al-Kadi, F.K.A.; Abdulkareem, J.F.; Al-jmoor, C.A. Fracture Strength of Palatal Denture Base Constructed from Different Acrylic Denture Base Materials. Eur. Sci. J. 2015, 11, 346–354. [Google Scholar]
- Prasad, D.K.; Dogra, E.S.; Hegde, C. A Study to Evaluate Midline Fracture Resistance of Maxillary Acrylic Denture Base Reinforced with Metal Pattern in Various Palatal Contours. World J. Dent. 2020, 11, 287–293. [Google Scholar] [CrossRef]
- Prombonas, A.; Poulis, N.A.; Yannikakis, S.A. The Impact of Notches on the Fracture Strength of Complete Upper Dentures: A Novel Biomechanical Approach. Eur. Sci. J. 2019, 15, 433. [Google Scholar] [CrossRef]
- Hamouda, I.M.; Ahmed, S.A. Effect of Microwave Disinfection on Mechanical Properties of Denture Base Acrylic Resin. J. Mech. Behav. Biomed. Mater. 2010, 3, 480–487. [Google Scholar] [CrossRef]
- Gaol, E.L.; Ritonga, P.W.U. Effect of Chlorhexidine and Castor Oil on Surface Roughness of Heat-Cured Acrylic Resin Denture Base. J. Dent. Syiah Kuala 2023, 8, 24–30. [Google Scholar] [CrossRef]
- ISO 20795-1:2013; Denture Base Polymers. ISO: Geneva, Switzerland, 2013.
- Craig, R.G.; Powers, J.M. Restorative Dental Materials, 11th ed.; Mosby: St. Louis, MO, USA, 2002. [Google Scholar]
- Zappini, G.; Kammann, A.; Wachter, W. Influence of acrylic resin polymerisation methods on fracture resistance of denture bases. J. Prosthet. Dent. 2003, 90, 256–260. [Google Scholar] [CrossRef]
- Anusavice, K.J.; Shen, C.; Rawls, H.R. Phillips’ Science of Dental Materials, 12th ed.; Elsevier: St. Louis, MO, USA, 2012. [Google Scholar]
- De Souza, R.F.; Paranhos, H.F.O.; Lovato da Silva, C.H.; Ito, I.Y. Effects of immersion solution on biofilm formation on acrylic resin denture base surfaces. Braz. Dent. J. 2009, 20, 127–131. [Google Scholar] [CrossRef]
- Polyzois, G.L.; Frangou, M.J. Influence of curing method, reinforcement, and fluoride treatment on some properties of denture base materials. J. Oral Rehabil. 2001, 28, 426–432. [Google Scholar] [CrossRef]
- Polychronakis, N.; Yannikakis, S.; Zissis, A. The effect of repeated microwaving disinfection on the dimensional stability of acrylic dentures. Acta Stomatol. Croat. 2014, 48, 279–284. [Google Scholar] [CrossRef] [PubMed]
- Campanha, N.H.; Pavarina, A.C.; Vergani, C.E.; Machado, A.L.; Giampaolo, E.T. Temperature rise in dentures during microwave disinfection. Braz. Dent. J. 2005, 16, 115–120. [Google Scholar] [CrossRef]
- Machado, A.L.; Giampaolo, E.T.; Pavarina, A.C.; Jorge, J.H. Simultaneous microwave disinfection and drying of complete dentures. J. Prosthodont. 2009, 18, 589–593. [Google Scholar] [CrossRef]
- Lima, J.F.M.; Orsi, I.A.; Borie, E.; Cândido, L.M.; Compagnoni, M.A. Effect of microwave disinfection on dimensional stability of a denture base acrylic resin. J. Prosthodont. 2009, 18, 123–129. [Google Scholar] [CrossRef]
- Basso, M.F.M.; Giampaolo, E.T.; Machado, A.L.; Pavarina, A.C.; Vergani, C.E. Evaluation of the occlusion vertical dimension of complete dentures after microwave disinfection. Gerodontology 2011, 29, e611–e617. [Google Scholar] [CrossRef]
- Da Silva, F.C.; Kimpara, E.T.; Mancini, M.N.G.; Balducci, I.; Jorge, A.O.C.; Koga-Ito, C.Y. Effectiveness of six different disinfectants on removing five microbial species and effects on the topographic characteristics of acrylic resin. J. Prosthodont. 2008, 17, 627–633. [Google Scholar] [CrossRef]
- Schwindling, F.S.; Rammelsberg, P.; Stober, T. Effect of Chemical Disinfection on the Surface Roughness of Hard Denture Base Materials: A Systematic Literature Review. Int. J. Prosthodont. 2014, 27, 215–225. [Google Scholar] [CrossRef] [PubMed]
- Kannaiyan, K.; Rakshit, P.; Bhat, M.P.S.; Sadasiva, S.K.K.; Babu, S.C.; Ummer, H. Effect of Different Disinfecting Agents on Surface Roughness and Colour Stability of Heat-Cured Acrylic Denture Material: An In Vitro Study. J. Contemp. Dent. Pract. 2023, 24, 68–74. [Google Scholar] [CrossRef]
- Hashem, M.; Alsaleem, S.O.; Assery, M.K.; Abdeslam, E.B.; Vellappally, S.; Anil, S. A comparative study of the mechanical properties of the light-cure and conventional denture base resins. Oral Health Dent. Manag. 2014, 13, 311–315. [Google Scholar] [PubMed]
- Qasim, S.; Al-Khuraif, S.; Kumar, R. An Investigation into the Impact and Flexural Strength of Light-Cure Denture Resin Reinforced with Carbon Nanotubes. World Appl. Sci. J. 2012, 18, 808–812. [Google Scholar] [CrossRef]
- Mumcu, E.; Cilingir, A.; Gencel, B.; Sülün, T. Flexural Properties of a Light-Cure and a Self-Cure Denture Base Material Compared to Conventional Alternatives. J. Adv. Prosthodont. 2011, 3, 136–139. [Google Scholar] [CrossRef]
- AlQahtani, M.; Haralur, S.B. Influence of Different Repair Acrylic Resin and Thermocycling on the Flexural Strength of Denture Base Resin. Medicina 2020, 56, 50. [Google Scholar] [CrossRef]
| Material Type | Commercial Brand/Manufacturer | Mixing Ratio/Polymerisation Method |
|---|---|---|
| Conventional Heat-Cure Acrylic Resin | Villacryl H Plus, Zhermack, Italy | 24 g powder: 10.5 mL liquid |
| High-Impact Acrylic Resin | Vertex Dental, Netherlands | 21 g powder: 10 mL liquid |
| Light-Cure Acrylic Resin | Cavex, Netherlands | Light polymerisation time: 3–5 min, using 27 W Dental Lab Light Curing Unit (Denshine, Guangzhou, China) with UVA bulbs. |
| Disinfection Protocols | Denture Base Materials | Specimen Numbers (n) | Mean (Std) | ANOVA |
|---|---|---|---|---|
| Water (control) | Cross-linked acrylic denture base | 5 | 1.74 (0.44) | p-value = 0.069 |
| High-impact acrylic denture base | 5 | 1.36 (0.17) | ||
| Light-cure acrylic denture base | 5 | 0.76 (0.08) | ||
| Chemical cleaner (0.2% chlorhexidine disinfection) | Cross-linked acrylic denture base | 5 | 1.19 (0.19) | |
| High-impact acrylic denture base | 5 | 1.72 (0.4) | ||
| Light-cure acrylic denture base | 5 | 0.62 (0.07) | ||
| Microwave | Cross-linked acrylic denture base | 5 | 1.16 (0.18) | |
| High-impact acrylic denture base | 5 | 1.35 (0.28) | ||
| Light-cure acrylic denture base | 5 | 0.62 (0.02) |
| Denture Base Materials | Mean Difference | Std. Error | T | p |
|---|---|---|---|---|
| Cross-linked acrylic denture base—High-impact acrylic denture base | −0.11 | 0.06 | −1.75 | 0.316 |
| Cross-linked acrylic denture base—Light-cure acrylic denture base | 0.7 | 0.06 | 11.15 | <0.001 |
| High-impact acrylic denture base—Light-cure acrylic denture base | 0.81 | 0.06 | 12.9 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Kadi, F.K.; Abdulkareem, J.F.; Esmael, S.K. The Fracture Strength of Acrylic Palatal Prostheses After Microwave and Chlorhexidine Disinfection: A Comparative In Vitro Study. Oral 2025, 5, 78. https://doi.org/10.3390/oral5040078
Al-Kadi FK, Abdulkareem JF, Esmael SK. The Fracture Strength of Acrylic Palatal Prostheses After Microwave and Chlorhexidine Disinfection: A Comparative In Vitro Study. Oral. 2025; 5(4):78. https://doi.org/10.3390/oral5040078
Chicago/Turabian StyleAl-Kadi, Faten Khalid, Jwan Fateh Abdulkareem, and Saja Kareem Esmael. 2025. "The Fracture Strength of Acrylic Palatal Prostheses After Microwave and Chlorhexidine Disinfection: A Comparative In Vitro Study" Oral 5, no. 4: 78. https://doi.org/10.3390/oral5040078
APA StyleAl-Kadi, F. K., Abdulkareem, J. F., & Esmael, S. K. (2025). The Fracture Strength of Acrylic Palatal Prostheses After Microwave and Chlorhexidine Disinfection: A Comparative In Vitro Study. Oral, 5(4), 78. https://doi.org/10.3390/oral5040078