Reforming Dental Curricula: A Student-Centred Novel Approach Integrating Prosthodontic Care for Older Adults
Abstract
1. Introduction
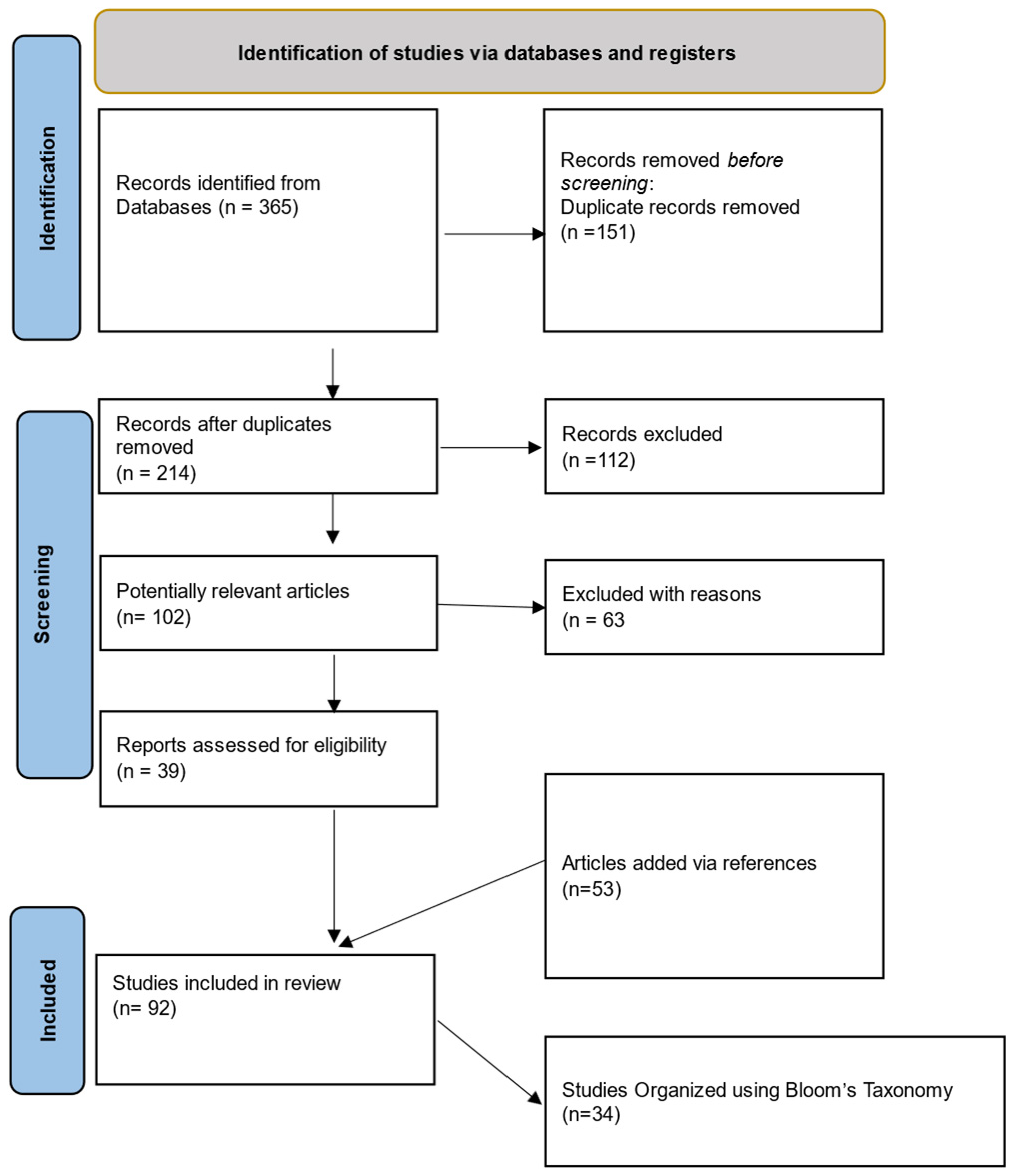
2. Materials and Methods
3. Results
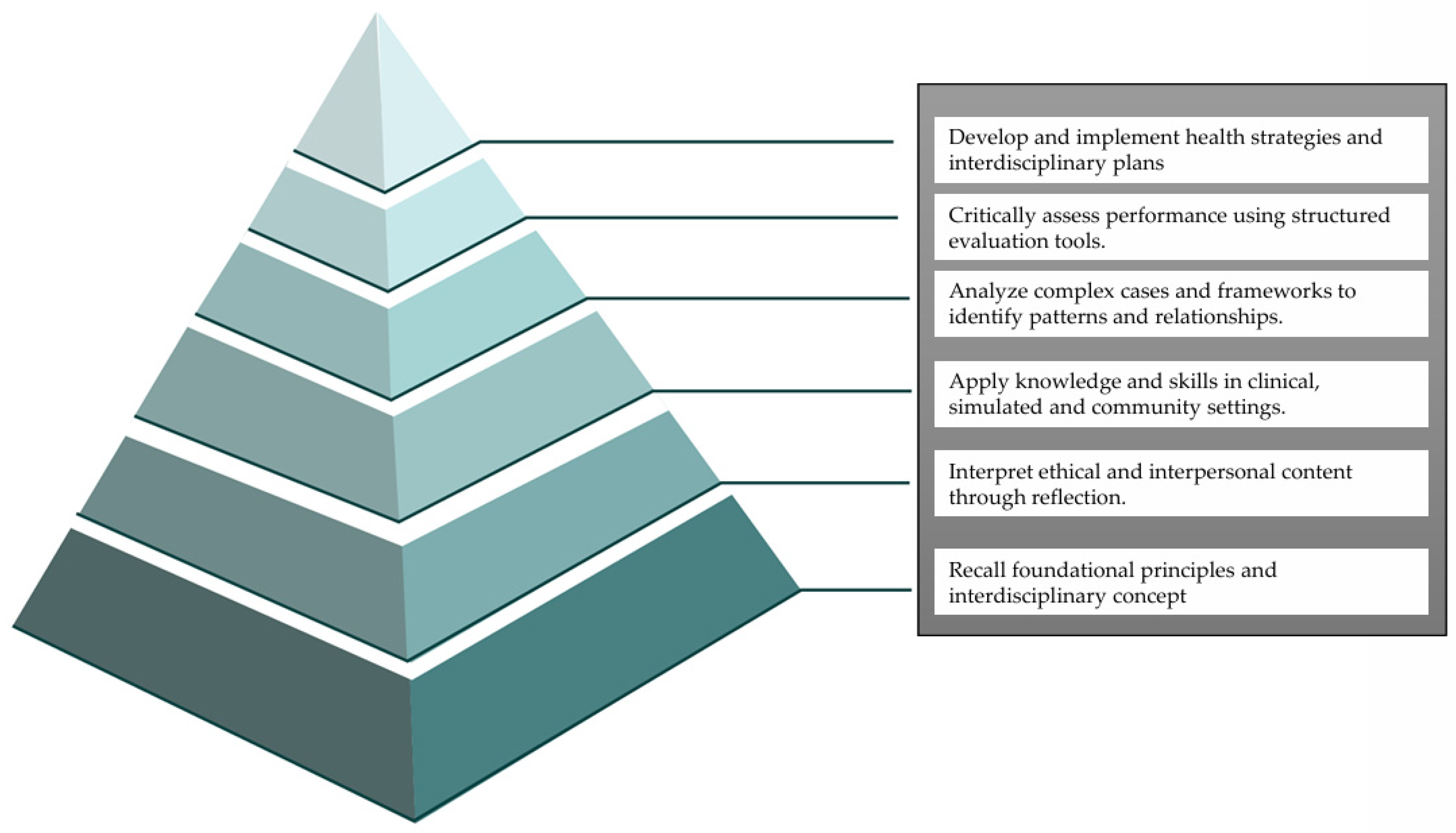
3.1. Foundations in Cognitive Recall Memory
3.1.1. Student Recall of Foundational Knowledge from Memory
3.1.2. Faculty Recall of Foundational Knowledge
3.1.3. Recall of Basic Science Concepts in Clinical Contexts
3.1.4. Student Recall of Perceived Clarity and Motivation in Integrated Learning
3.2. Developing Understanding of Interdisciplinary Frameworks
3.2.1. Assessment-Informed Learning Design
3.2.2. Learning Strategy Evaluation
3.2.3. Case-Based and Didactic Integration
3.2.4. Faculty-Student Communication
3.3. Apply Knowledge in Practical, Clinical, and Team-Based Settings
3.3.1. Standardised Clinical Tools
3.3.2. Motivational Learning
3.3.3. Retrieval-Based Practice
3.3.4. Multimedia Clinical Integration
3.3.5. Interdisciplinary Physiology
3.3.6. Digital-Game-Based Learning
3.3.7. Evidence-Based Instruction
3.3.8. VR-Haptic Technology Integration
3.4. Analysing Knowledge to Dissect Complex Cases and Frameworks and Identify Patterns and Relationships
3.4.1. Integrated Preclinical and Clinical Curriculum
3.4.2. Higher-Order Thinking
3.4.3. Curriculum-Integrated Research Seminars
3.4.4. Critical Thinking Curriculum
3.4.5. Cross-Disciplinary Assessment Models
3.4.6. Oral Health as a Cognitive Decline Indicator
3.4.7. Preventive Domiciliary Dental Care
3.5. Critical Evaluation of Knowledge: Making Informed Judgments Based on Established Criteria and Evidence
3.5.1. Revised Bloom’s Taxonomy for Curriculum Coherence
3.5.2. Curriculum Evaluation and Consensus Building
3.5.3. Evaluation of Integrated Curriculum Modules
3.5.4. Assessment of Student Attitudes in Geriatric Dentistry
3.5.5. Evaluation of the 4Ms Geriatric Framework
3.5.6. Simulation-Based Preclinical Training
3.6. Creating Frameworks for Student-Centred Older Care: Designing and Developing Care Plans and Interventions
3.6.1. Blooming Anatomy Tool for Assessment Design
3.6.2. Session Integration Tool (SIT) for Integrated Learning
3.6.3. Simulation-Based Communication Training
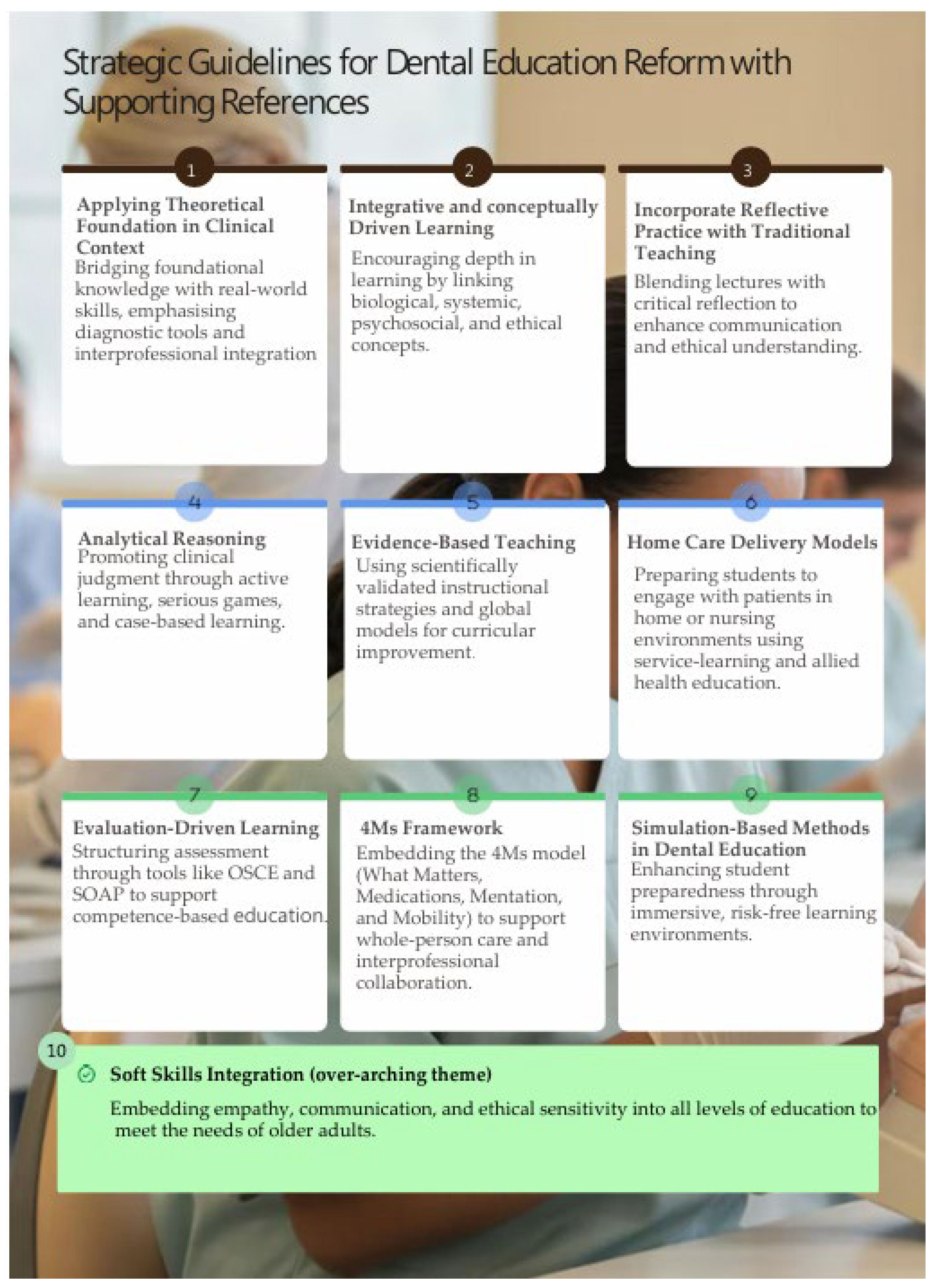
3.7. Generating Student-Centred Guidelines for Dental Curriculum Reform in Older Adult Prosthodontic Care
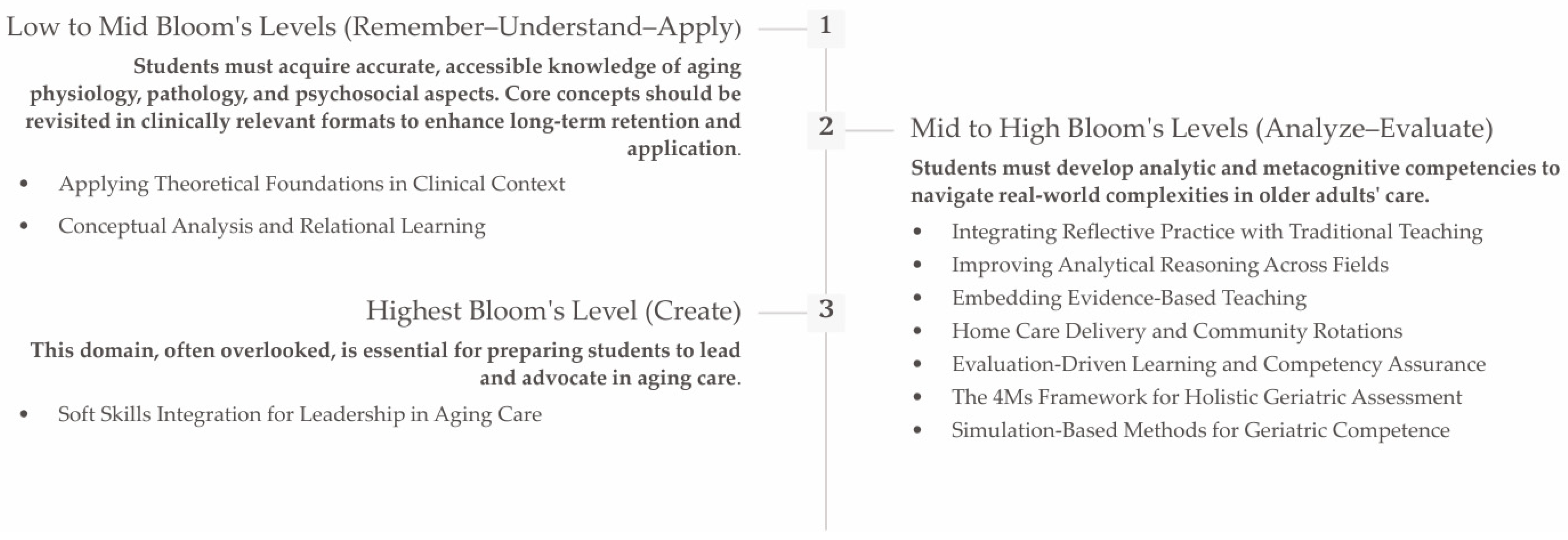
4. Discussion
4.1. Reforming Geriatric Prosthodontic Education Through Bloom’s Taxonomy and Strategic Guidelines
4.1.1. Low to Mid Bloom’s Levels (Remember–Understand–Apply): Building Cognitive Foundations for Geriatric Understanding
4.1.2. Mid-to-High Bloom’s Levels (Analyse–Evaluate): Enhancing Clinical Reasoning and Reflective Capacity
4.1.3. Highest Bloom’s Level (Create): Fostering Innovation and Humanistic Leadership
4.2. Limitations of the Present Scoping Review
5. Conclusions
6. Future Directions for Implementation
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
| AETCOM | Attitude, Ethics, and Communication |
| ADEE | Association for Dental Education in Europe |
| AI | Artificial Intelligence |
| CBL | Case-Based Learning |
| CDPC | Clinical Dentist–Patient Communication |
| COST | Cooperation in Science and Technology |
| DentCPD | Dental Continuing Professional Development. |
| Delhi-NCR | Delhi–National Capital Region. |
| EBTA | Evidence-Based Teaching Approach |
| EBP | Evidence-Based Practice |
| ECG | European College of Gerodontology |
| EPAs | Entrustable Professional Activities |
| FDR | False Discovery Rate |
| HPE | Health Professional Education |
| ICC | Impaired Chewing Capacity |
| ICOPE | Integrated Care for Older People (ICOPE) |
| IPE | Interprofessional Education |
| NCDs | Non-Communicable Diseases |
| OHAT | Oral Health Assessment Tool |
| OSCE | Objective Structured Clinical Examination |
| PBL | Problem-Based Learning |
| PICO | Population, Intervention, Comparison, and Outcome |
| PRISMA | Preferred Reporting Items for Systematic reviews and Meta-Analyses |
| PROGRAMMING | PROmoting GeRiAtric Medicine |
| SIT | Session Integration Tool |
| SOAP | Subjective Objective Assessment Plan |
| TBL | Team-Based Learning |
| TOC | Total Occlusal Convergence |
| VR-haptic preclinical tool | Virtual Reality Haptic Tool |
| WHO | World Health Organization |
| 4Ms | What Matters, Medications, Mentation, Mobility |
References
- Anastasiadou, V.; Naka, O.; Pantelidou-Papadopoulou, O.; Sakellari, D.; Topitsoglou, V.; Tortopidis, D. Management of Complex Conditions in the Context of Geriatric Dentistry, 1st ed.; Hellenic Academic Libraries Link (HEAL-Link): Zografou, Greece, 2020; pp. 18–23. ISBN 978-960-603-244-8.
- Huang, X.; Kang, L.; Bi, J. Epidemiology of oral health in older adults aged 65 or over: Prevalence, risk factors and prevention. Aging Clin. Exp. Res. 2025, 37, 193. [Google Scholar] [CrossRef]
- World Health Organization. Integration of Oral Health Into Universal Healthcare; WHO Technical Report Series; WHO: Geneva, Switzerland, 2024; p. 1024.
- Petersen, P.E.; Yamamoto, T. Improving the oral health of aging populations. Int. Dent. J. 2005, 55, 253–257. [Google Scholar] [CrossRef]
- Petersen, P.E.; Baehni, P.C.; Ogawa, H. Train-the-Trainer programs for nursing home staff. Community Dent. Oral Epidemiol. 2023, 51, 145–152. [Google Scholar]
- Yamamoto-Kuramoto, T.; Aida, J.; Kondo, K. Tooth loss and functional disability in elderly. J. Am. Geriatr. Soc. 2023, 71, 1123–1131. [Google Scholar] [CrossRef]
- Guiglia, R.; Musciotto, A.; Compilato, D.; Procaccini, M.; Lo Russo, L.; Ciavarella, D.; Lo Muzio, L.; Cannone, V.; Pepe, I.; D’Angelo, M.; et al. Aging and oral health: Effects in hard and soft tissues. Curr. Pharm. Des. 2010, 16, 619–630. [Google Scholar] [CrossRef]
- Wolff, A.; Joshi, R.K.; Ekström, J.; Aframian, D.; Pedersen, A.M.; Proctor, G.; Narayana, N.; Villa, A.; Sia, Y.W.; Aliko, A.; et al. A Guide to Medications Inducing Salivary Gland Dysfunction, Xerostomia, and Subjective Sialorrhea: A Systematic Review Sponsored by the World Workshop on Oral Medicine VI. Drugs RD 2017, 17, 1–28. [Google Scholar] [CrossRef]
- Sarafidou, K.; Baechle, M.; Ferrucci, L. Oral microbiome changes in aging. J. Dent. Res. 2024, 103, 45–52. [Google Scholar]
- Zelig, R.; Goldstein, S.; Touger-Decker, R.; Firestone, E.; Golden, A.; Johnson, Z.; Kaseta, A.; Sackey, J.; Tomesko, J.; Parrott, J.S. Tooth Loss and Nutritional Status in Older Adults: A Systematic Review and Meta-analysis. JDR Clin. Transl. Res. 2022, 7, 4–15. [Google Scholar] [CrossRef] [PubMed]
- Du, M.; Deng, K.; Yin, J.; Wu, C.; Hu, S.; Guo, L.; Luo, Z.; Tonetti, M.; Tjakkes, G.E.; Visser, A.; et al. Association Between Chewing Capacity and Mortality Risk: The Role of Diet and Ageing. J. Clin. Periodontol. 2025, 52, 695–706. [Google Scholar] [CrossRef]
- van der Putten, G.J.; de Baat, C.; De Visschere, L.; Schols, J. Poor oral health, a potential new geriatric syndrome. Gerodontology 2014, 31 (Suppl. S1), 17–24. [Google Scholar] [CrossRef]
- Field, J.; Vital, S.; Dixon, J.; Murphy, D.; Davies, J. The Graduating European Dentist Curriculum Framework: A 7-Year Review. Eur. J. Dent. Educ. Off. J. Assoc. Dent. Educ. Eur. 2025, 29, 155–161. [Google Scholar] [CrossRef]
- Kossioni, A.; McKenna, G.; Müller, F. European College of Gerodontology undergraduate curriculum guidelines. Eur. J. Dent. Educ. 2017, 21, 3–9. [Google Scholar] [CrossRef]
- Kossioni, A.E.; Hajto-Bryk, J.; Maggi, S.; McKenna, G.; Petrovic, M.; Roller-Wirnsberger, R.E.; Schimmel, M.; Tamulaitienè, M.; Vanobbergen, J.; Müller, F. An Expert Opinion from the European College of Gerodontology and the European Geriatric Medicine Society: European Policy Recommendations on Oral Health in Older Adults. J. Am. Geriatr. Soc. 2018, 66, 609–613. [Google Scholar] [CrossRef] [PubMed]
- Kossioni, A.; Vanobbergen, J.; Newton, J.P. Gerodontology education in European dental schools. Eur. J. Dent. Educ. 2018, 22, e1–e6. [Google Scholar] [CrossRef]
- Lamprecht, R.; Smith, J.; Wilson, M. Global oral health trends in aging populations. Community Dent. Oral Epidemiol. 2020, 48, 215–223. [Google Scholar] [CrossRef]
- Lamprecht, R.; Guse, J.; Schimmel, M.; Müller, F.; Heydecke, G.; Reissmann, D.R. Benefits of combined quantitative and qualitative evaluation of learning experience in a gerodontology course for dental students. BMC Med. Educ. 2020, 20, 281. [Google Scholar] [CrossRef]
- Xavier, I.; Ettinger, R.L.; Proença, L.; Botelho, J.; Machado, V.; Rua, J.; Delgado, A.S.; Mendes, J.J. Geriatric Dentistry Curriculum in Six Continents. Int. J. Environ. Res. Public Health 2020, 17, 4682. [Google Scholar] [CrossRef]
- Arany, P.; Kossioni, A.; Müller, F. Implementing the 4Ms framework in geriatric dental practice. J. Dent. Educ. 2024, 88, 602–610. [Google Scholar]
- Parikh, N.; Risinger, D.; Holland, J.N.; Molony, D.A.; van der Hoeven, D. Evaluating dental students’ perspectives on the concurrent teaching of didactic and case-based courses. J. Dent. Educ. 2022, 86, 1643–1652. [Google Scholar] [CrossRef] [PubMed]
- Arruzza, E.; Chau, M. A scoping review of randomised controlled trials to assess the value of gamification in the higher education of health science students. J. Med. Imaging Radiat. Sci. 2021, 52, 137–146. [Google Scholar] [CrossRef]
- Dalaya, M.; Ishaquddin, S.; Ghadage, M.; Hatte, G. An interesting review on soft skills and dental practice. J. Clin. Diagn. Res. JCDR 2015, 9, ZE19–ZE21. [Google Scholar] [CrossRef]
- Beattie, V.; Collins, B.; McInnes, B. Deep and surface learning: A simple or simplistic dichotomy? Account. Educ. 1997, 6, 1–12. [Google Scholar] [CrossRef]
- Marton, F.; Säljö, R. On qualitative differences in learning: I—Outcome and process. Br. J. Educ. Psychol. 1976, 46, 4–11. [Google Scholar] [CrossRef]
- Strandell, C.H. Nursing Faculty Perceptions of an Integrated Curriculum and Implementation of the Curriculum. Degree Doctor of Philosophy Field of Education. Ph.D. Thesis, Northwestern University, Evanston, IL, USA, 1980. [Google Scholar]
- Maharjan, B.; Bhandary, S.; Upadhyay, S.; Ghimire, S.; Shrestha, I.; Joshi, M.; Vaidya, S.; Pradhan, P. Developing tool and measuring integration characteristics of basic science curriculum to improve curriculum integration. Kathmandu Univ. Med. J. 2018, 64, 338–344. Available online: https://www.researchgate.net/publication/333162902 (accessed on 28 August 2025).
- Lajber, M.; Mahboob, U.; Lajber, F.; Khan, M.; Waseem Badshah Bukhari, S. Student’s perception regarding an integrated curriculum at a public sector medical college. PJMHS 2020, 14, 1196–1199. Available online: https://pjmhsonline.com/2020/july-sep/1196.pdf (accessed on 28 August 2025).
- Morton, D.A.; Colbert-Getz, J.M. Measuring the impact of the flipped anatomy classroom: The importance of categorizing an assessment by Bloom’s taxonomy. Anat. Sci. Educ. 2017, 10, 170–175. [Google Scholar] [CrossRef]
- Bansal, S.; Bansal, M.; White, S. Association Between Learning Approaches and Medical Student Academic Progression During Preclinical Training. Adv. Med. Educ. Pract. 2021, 12, 1343–1351. [Google Scholar] [CrossRef]
- Estrela, C.; Oshita, M.G.B.; Perazzo, M.F.; Alencar, A.H.G.; Silva, J.A.; Estrela, L.R.; Cintra, L.T.; Estrela, C.R. Quality of Communication Between Professors and University Students in the Process of Learning. Braz. Dent. J. 2024, 35, e246081. [Google Scholar] [CrossRef]
- Chalmers, J.M.; Carter, K.D.; Spencer, A.J. Oral health assessment tools for elderly patients. Spec. Care Dent. 2002, 22, 11–20. [Google Scholar] [CrossRef]
- Prat-Sala, M.; Redford, P. The interplay between motivation, self-efficacy, and approaches to studying. Br. J. Educ. Psychol. 2010, 80, 283–305. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, P.K. Retrieval practice & Bloom’s taxonomy: Do students need fact knowledge before higher order learning? J. Educ. Psychol. 2019, 111, 189–209. [Google Scholar] [CrossRef]
- Miller, C.J.; Metz, M.J. Can clinical scenario videos improve dental students’ perceptions of the basic sciences and ability to apply content knowledge? J. Dent. Educ. 2015, 79, 1452–1460. [Google Scholar] [CrossRef]
- Hobbins, J.O.; Murrant, C.L.; Snook, L.A.; Tishinsky, J.M.; Ritchie, K.L. Incorporating higher order thinking and deep learning in a large, lecture-based human physiology course: Can we do it? Adv. Physiol. Educ. 2020, 44, 637–644. [Google Scholar] [CrossRef]
- Lin, C.S.; Yang, C.C. Evaluation of a digital game for teaching behavioral aspects of clinical communication in dentistry. BMC Med. Educ. 2023, 23, 78. [Google Scholar] [CrossRef]
- Tebcherany, H.; Khocht, A. An evidence-based teaching approach enhances student learning of periodontal disease pathogenesis. J. Dent. Educ. 2024, 88, 304–313. [Google Scholar] [CrossRef]
- Bencharit, S.; Quinn, B.; Sittoni-Pino, M.F.; Arias-Herrera, S.; Schick, S.G.; Rampf, S.; Byrne, S.; Shazib, M.A.; Örtengren, U.; Lam, W.Y.H.; et al. Insights from the global education survey on the use of VR-haptics in dental education. Front. Dent. Med. 2025, 6, 1576646. [Google Scholar] [CrossRef]
- Kerosuo, E.; Ruotoistenmäki, J.; Murtomaa, H. Report on the development of a new dental curriculum at Helsinki. Eur. J. Dent. Educ. 2001, 5, 23–30. [Google Scholar] [CrossRef]
- Crowe, A.; Dirks, C.; Wenderoth, M.P. Biology in bloom: Implementing Bloom’s Taxonomy to enhance student learning in biology. CBE Life Sci. Educ. 2008, 7, 368–381. [Google Scholar] [CrossRef] [PubMed]
- Kingsley, K.; O’Malley, S.; Stewart, T.; Howard, K.M. Research enrichment: Evaluation of structured research in the curriculum for dental medicine students as part of the vertical and horizontal integration of biomedical training and discovery. BMC Med. Educ. 2008, 8, 9. [Google Scholar] [CrossRef]
- Chambers, D.W. Lessons from students in a critical thinking course: A case for the third pedagogy. J. Dent. Educ. 2009, 73, 65–82. [Google Scholar] [CrossRef] [PubMed]
- Rougas, S.; Berry, A.; Bierer, S.B.; Blanchard, R.D.; Cianciolo, A.T.; Colbert-Getz, J.M.; Han, H.; Lipner, K.; Teal, C.R. Applying Conceptual and Theoretical Frameworks to Health Professions Education Research: An Introductory Workshop. MedEdPORTAL J. Teach. Learn. Resour. 2022, 18, 11286. [Google Scholar] [CrossRef] [PubMed]
- Manchery, N.; Henry, J.D.; Lam, B.C.P.; Kochan, N.A.; Deutsch, A.; Brodaty, H.; S Sachdev, P.; Nangle, M.R. Memory decline in older individuals predicts an objective indicator of oral health: Findings from the Sydney Memory and Ageing Study. BMC Oral Health 2022, 22, 93. [Google Scholar] [CrossRef] [PubMed]
- Nagatani, M.; Tanaka, T.; Son, B.K.; Kawamura, J.; Tagomori, J.; Hirano, H.; Shirobe, M.; Iijima, K. Oral frailty as a risk factor for mild cognitive impairment in community-dwelling older adults: Kashiwa study. Exp. Gerontol. 2023, 172, 112075. [Google Scholar] [CrossRef]
- Allenspach, P.; Srinivasan, M. Oral health status of institutionalized older adults receiving domiciliary dental care: A cross-sectional retrospective study. Spec. Care Dent. 2024, 44, 1444–1455. [Google Scholar] [CrossRef]
- Anderson, L.; Krathwohl, D.; Bloom, B. A Taxonomy for Learning, Teaching, and Assessing: A Revision of Bloom’s Taxonomy of Educational Objectives. 2000. Available online: http://lst-iiep.iiep-unesco.org/cgi-bin/wwwi32.exe/[in=epidoc1.in]/?t2000=015556/(100) (accessed on 28 August 2025).
- Al Khalaf, K.; Moore, C.; McKenna, G.; Da Mata, C.; Lynch, C.D. Undergraduate teaching and assessment methods in prosthodontics curriculum: An international Delphi survey. J. Dent. 2022, 123, 104207. [Google Scholar] [CrossRef]
- Nayak, V.; Nayak, K.R.; Goyal, S.; Jain, S.; Prabhath, S.; Palimar, V.; Komattil, R. Tangible impact of patient communication modules on medical students and interns. Adv. Physiol. Educ. 2024, 48, 40–48. [Google Scholar] [CrossRef]
- Singh, S.; Gupta, R.; Gill, S.; Naaz, Z.; Longdo, M.; Pathak, A.; Kusuma, J. Perception and Attitude of Dental Students Towards Geriatric Care: A Questionnaire-Based Survey. Cureus 2024, 16, e67297. [Google Scholar] [CrossRef]
- Arany, S.; Cavalcanti, L.; Phildor, D.; Watson, G.E.; Kopycka-Kedzierawski, D.T.; Eliav, E.; Medina-Walpole, A.; Caprio, T. Implementation of a 4Ms approach in age-friendly oral health care at an Academic Specialty Care Dental Clinic. J. Am. Geriatr. Soc. 2024, 72 (Suppl. S3), S68–S75. [Google Scholar] [CrossRef] [PubMed]
- Hadjichristou, C.; Kokoti, M.; Bakopoulou, A. Haptics in fixed prosthodontics and their role in dental education: A literature review. J. Dent. Educ. 2024, 88, 1020–1028. [Google Scholar] [CrossRef]
- Thompson, A.R.; O’Loughlin, V.D. The Blooming Anatomy Tool (BAT): A discipline-specific rubric for utilizing Bloom’s taxonomy in the design and evaluation of assessments in the anatomical sciences. Anat. Sci. Educ. 2015, 8, 493–501. [Google Scholar] [CrossRef]
- Heck, A.J.; Chase, A.J. A Tool for Evaluating Session-Level Integration in Medical Education. Med. Sci. Educ. 2021, 31, 647–654. [Google Scholar] [CrossRef]
- Bock, A.; Wagenknecht, N.; Winnand, P.; Katz, M.S.; Ooms, M.; Heitzer, M.; Hölzle, F.; Modabber, A. Improvement of students’ communication skills through targeted training and the use of simulated patients in dental education-a prospective cohort study. BMC Med. Educ. 2024, 24, 820. [Google Scholar] [CrossRef] [PubMed]
- Tambunan, E.H. Theory-Practice Gap During Clinical Learning: A Descriptive Qualitative Study of Nursing Students’ Experiences and Perceptions. J. Caring Sci. 2024, 13, 74–81. [Google Scholar] [CrossRef]
- Mercan, N.; Mersin, S. Evaluating the therapeutic communication skills of nursing students in the clinical setting: The experiences of students, patients and patients’ relatives. Heliyon 2025, 11, e41677. [Google Scholar] [CrossRef]
- Jabade, M.; Nadaf, H. Assessing the efficacy of mind mapping as a learning technique to enhance information retrieval in nursing students. J. Educ. Health Promot. 2024, 13, 371. [Google Scholar] [CrossRef]
- Shanmugarajah, M.M.; Mondal, H.; Das, T. From Fragmented Facts to Unified Knowledge: Exploring Concept Mapping in Neuromuscular Physiology Among First-Year Medical Students. Cureus 2024, 16, e74711. [Google Scholar] [CrossRef] [PubMed]
- Machost, H.; Stains, M. Reflective Practices in Education: A Primer for Practitioners. CBE Life Sci. Educ. 2023, 22, es2. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Zeng, D.; Xu, T.; Wang, Y. Representation Learning for Integrating Multi-domain Outcomes to Optimize Individualized Treatments. Adv. Neural Inf. Process. Syst. 2020, 33, 17976–17986. [Google Scholar]
- Chen, Y.; Zeng, D.; Wang, Y. Optimizing personalized treatments for targeted patient populations across multiple domains. Int. J. Biostat. 2024, 20, 437–453. [Google Scholar] [CrossRef]
- Dusin, J.; Melanson, A.; Mische-Lawson, L. Evidence-based practice models and frameworks in the healthcare setting: A scoping review. BMJ Open 2023, 13, e071188. [Google Scholar] [CrossRef]
- Haavisto, E.; Siltanen, H.; Tolvanen, A.; Holopainen, A. Instruments for assessing healthcare professionals’ knowledge and skills of evidence-based practice: A scoping review. J. Clin. Nurs. 2023, 32, 4391–4407. [Google Scholar] [CrossRef] [PubMed]
- Denecke, K.; Kushniruk, A.W.; Borycki, E.M. A Comprehensive Framework for Hospital@Home Care Models. Stud. Health Technol. Inform. 2024, 314, 27–31. [Google Scholar] [CrossRef] [PubMed]
- Health Quality Ontario Team. Based Models for End-of-Life Care: An Evidence-Based Analysis. Ont. Health Technol. Assess. Ser. 2014, 14, 1–49. [Google Scholar]
- Al-Hashimi, K.; Said, U.N.; Khan, T.N. Formative Objective Structured Clinical Examinations (OSCEs) as an Assessment Tool in UK Undergraduate Medical Education: A Review of Its Utility. Cureus 2023, 15, e38519. [Google Scholar] [CrossRef] [PubMed]
- Podder, V.; Lew, V.; Ghassemzadeh, S. SOAP Notes. [Updated 28 August 2023]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: https://www.ncbi.nlm.nih.gov/books/NBK482263/ (accessed on 28 August 2025).
- Al-Moteri, M. Entrustable professional activities in nursing: A concept analysis. Int. J. Nurs. Sci. 2020, 7, 277–284. [Google Scholar] [CrossRef]
- Alexander, N.; Maaz, A.; Peters, H.; Kottner, J. Entrustable professional activities in nursing education: A scoping review protocol. BMJ Open 2022, 12, e061451. [Google Scholar] [CrossRef]
- Emery-Tiburcio, E.E.; Mack, L.; Zonsius, M.C.; Carbonell, E.; Newman, M. The 4Ms of an Age-Friendly Health System An evidence-based framework to ensure older adults receive the highest quality care. Home Healthc. Now 2022, 40, 252–257. [Google Scholar] [CrossRef]
- Carbonell, E.; Zonsius, M.C.; Rodriguez-Morales, G.; Newman, M.; Emery-Tiburcio, E.E. Addressing What Matters Aligning care with the priorities of older adults and their caregivers. Home Healthc. Now 2022, 40, 258–263. [Google Scholar] [CrossRef]
- Thombley, R.L.; Rogers, S.E.; Adler-Milstein, J. Developing electronic health record-based measures of the 4Ms to support implementation and evidence generation for Age-Friendly Health Systems. J. Am. Geriatr. Society. 2023. Advance online publication. [Google Scholar] [CrossRef]
- Baxmann, M.; Baráth, Z.; Kárpáti, K. Efficacy of typodont and simulation training in orthodontic education: A systematic review. BMC Med. Educ. 2024, 24, 1443. [Google Scholar] [CrossRef]
- Higgins, D.; Hayes, M.; Taylor, J.; Wallace, J. A scoping review of simulation-based dental education. MedEdPublish 2020, 9, 36. [Google Scholar] [CrossRef]
- Manav, E.Y.; Akbiyik, S.Y.; Ceylan, A.B.; Çakiroğlu, A.E.Y.; Tuncer, D. Effects of virtual reality and layered tooth model training on manual dexterity in preclinical dental education. BMC Med. Educ. 2025, 25, 1020. [Google Scholar] [CrossRef] [PubMed]
- Pang, M.; Zhao, X.; Lu, D.; Dong, Y.; Jiang, L.; Li, J.; Ji, P. Preliminary User Evaluation of a New Dental Technology Virtual Simulation System: Development and Validation Study. JMIR Serious Games 2022, 10, e36079. [Google Scholar] [CrossRef] [PubMed]
- Kononowicz, A.A.; Woodham, L.A.; Edelbring, S.; Stathakarou, N.; Davies, D.; Saxena, N.; Tudor Car, L.; Carlstedt-Duke, J.; Car, J.; Zary, N. Virtual Patient Simulations in Health Professions Education: Systematic Review and Meta-Analysis by the Digital Health Education Collaboration. J. Med. Internet Res. 2019, 21, e14676. [Google Scholar] [CrossRef]
- Serrano, C.M.; Bakker, D.R.; Zamani, M.; de Boer, I.R.; Koopman, P.; Wesselink, P.R.; Berkhout, E.; Vervoorn, J.M. Virtual reality and haptics in dental education: Implementation progress and lessons learned after a decade. Eur. J. Dent. Educ. Off. J. Assoc. Dent. Educ. Eur. 2023, 27, 833–840. [Google Scholar] [CrossRef] [PubMed]
- Slaidina, A.; Ozolins, K.; Berzina, S.; Abeltins, A. Patient-specific virtual simulation in the clinical training for prosthetic dentistry. Eur. J. Dent. Educ. Off. J. Assoc. Dent. Educ. Eur. 2023. Advance online publication. [Google Scholar] [CrossRef]
- Patil, S.; Bhandi, S.; Awan, K.H.; Licari, F.W.; Di Blasio, M.; Ronsivalle, V.; Cicciù, M.; Minervini, G. Effectiveness of haptic feedback devices in preclinical training of dental students-a systematic review. BMC Oral Health 2023, 23, 739. [Google Scholar] [CrossRef]
- Tang, T.; Li, X.; Lin, Y.; Liu, C. Comparing digital real-time versus virtual simulation systems in dental education for preclinical tooth preparation of molars for metal-ceramic crowns. BMC Oral Health 2025, 25, 814. [Google Scholar] [CrossRef]
- Kodali, M.V.R.M.; Kodali, U.S.; Gadicherla, S.; Smriti, K.; Singh, A.; Khurshid, Z. The Role of Soft Skills in Dental Education: Challenges and Importance. Eur. J. Dent. 2025, 19, 851–859. [Google Scholar] [CrossRef]
- Carey, J.A.; Madill, A.; Manogue, M. Communications skills in dental education: A systematic research review. Eur. J. Dent. Educ. Off. J. Assoc. Dent. Educ. Eur. 2010, 14, 69–78. [Google Scholar] [CrossRef]
- Hanks, S.; Marples, C.; Wall, E. Reflections on learning and enhancing communication skills through community engagement: A student perspective. Br. Dent. J. 2016, 221, 81–85. [Google Scholar] [CrossRef]
- Jiménez, J.D.; Guillén-Guzmán, E.; Oliva, V.; Ballesteros-Urpi, A.; Pardo-Hernandez, H. Theoretical approaches to the engagement with patients in case-management programmes and assertive outreach teams: A systematic review of the literature. J. Psychiatr. Ment. Health Nurs. 2022, 29, 647–658. [Google Scholar] [CrossRef]
- Ogliari, G.; Masud, T.; Herghelegiu, A.M.; Pavic, T.; Wissendorff Ekdahl, A.; Piotrowicz, K.; Duque, S.; Benetos, A.; Bogdanovic, N.; Bonin-Guillaume, S.; et al. Collaborators of the PROGRAMMING survey on educational needs Educational Needs in Geriatric Medicine Among Health Care Professionals and Medical Students in COST Action 21122 PROGRAMMING: Mixed-Methods Survey Protocol. JMIR Res. Protoc. 2025, 14, e64985. [Google Scholar] [CrossRef] [PubMed]
- WHO. Integrated Care for Older People (ICOPE): Guidance for Person-Centred Assessment and Pathways in Primary Care, 2nd ed.; WHO: Geneva, Switzerland, 2025. Available online: https://www.who.int/publications/i/item/9789240103726 (accessed on 28 August 2025).
- Hasan, A. Competence-based dental education. Br. Dent. J. 2024, 236, 933. [Google Scholar] [CrossRef] [PubMed]
- Witheridge, A.; Ferns, G.; Scott-Smith, W. Revisiting Miller’s pyramid in medical education: The gap between traditional assessment and diagnostic reasoning. Int. J. Med. Educ. 2019, 10, 191–192. [Google Scholar] [CrossRef] [PubMed]
- Shams, F.; Huisman, J.; Hsieh, C.C.; Wilkins, S.; Adelman, C. The Bologna process and its impact in the European Higher Education Area and beyond. In SAGE Knowledge; SAGE: Newcastle upon Tyne, UK, 2012. [Google Scholar] [CrossRef]
| No | Implementation Type | Methods | Sources |
|---|---|---|---|
| 1 and 2 | Student Recall of Foundational Knowledge from Memory | Qualitative studies on learner experiences and perceptions | [24,25] |
| 3 | Faculty Recall of Foundational Knowledge | Curriculum inventory and shared understanding of teaching approaches | [26] |
| 4 | Recall of Basic Science Concepts in Clinical Contexts | Organ-system curriculum, PBL, aligned assessments, collaborative planning | [27] |
| 5 | Student Recall of Perceived Clarity and Motivation in Integrated Learning | Survey on clarity, manageability, and motivational aspects of integrated learning | [28] |
| No | Implementation Type | Methods | Sources |
|---|---|---|---|
| 6 | Assessment-Informed Learning Design | Analysis of how assessment types influence understanding and learning behaviours in anatomy and physiology | [29] |
| 7 | Learning Strategy Evaluation | Cohort study on deep vs. surface learning strategies and academic outcomes | [30] |
| 8 | Case-Based and Didactic Integration | Survey on student perceptions of simultaneous didactic and case-based instruction | [21] |
| 9 | Faculty-Student Communication | Evaluation of cross-disciplinary dialogue, perceptions of engagement, and use of technology | [31] |
| No | Implementation Type | Methods | Sources |
|---|---|---|---|
| 10 | Standardised Clinical Tools | Cross-sectional study validating OHAT for student training in elder care assessments | [32] |
| 11 | Motivational Learning | Correlational study on motivation, self-efficacy, and strategic learning | [33] |
| 12 | Retrieval-Based Practice | Experimental study on the impact of retrieval practice on knowledge retention and application | [34] |
| 13 | Multimedia Clinical Integration | Use of clinical scenario videos in physiology and dental emergency training | [35] |
| 14 | Interdisciplinary Physiology | Applied physiology course to promote integration in complex health scenarios | [36] |
| 15 | Digital-Game-Based Learning | Intervention study using the CDPC game to enhance motivation, self-efficacy, and communication skills | [37] |
| 16 | Evidence-Based Instruction | Implementation of EBTA in periodontics: analysis of student knowledge, attitudes, and confidence | [38] |
| 17 | VR-Haptic Technology Integration | Global survey on the use of VR-haptics in preclinical dental education | [39] |
| No | Implementation Type | Methods | Sources |
|---|---|---|---|
| 18 | Integrated Preclinical and Clinical Curriculum | Curriculum reform; program evaluation; student feedback | [40] |
| 19 | Higher-Order Thinking | Experimental research: student learning outcomes | [41] |
| 20 | Curriculum-Integrated Research Seminars | Structured research seminars, curricular integration challenges and outcomes | [42] |
| 21 | Critical Thinking Curriculum | Qualitative, longitudinal reflection over 8 years; narrative student experiences | [43] |
| 22 | Cross-Disciplinary Assessment Models | Systematic review of conceptual and disciplinary assessment frameworks | [44] |
| 23 and 24 | Oral Health as a Cognitive Decline Indicator | Analytical clinical frameworks linking oral health (e.g., chewing, tongue pressure) to frailty/dementia | [45,46] |
| 25 | Preventive Domiciliary Dental Care | Evaluation of care models; analysis of clinical outcomes in institutional settings | [47] |
| No | Implementation Type | Methods | Sources |
|---|---|---|---|
| 26 | Revised Bloom’s Taxonomy for Curriculum Coherence | Systematic review; framework application across disciplines | [48] |
| 27 | Curriculum Evaluation and Consensus Building | International Delphi survey of dental educators on teaching and assessment in prosthodontics | [49] |
| 28 | Evaluation of Integrated Curriculum Modules | Qualitative feedback from students and faculty on module structure and implementation | [50] |
| 29 | Assessment of Student Attitudes in Geriatric Dentistry | Cohort study; biopsychosocial metrics; multiple p-values for attitude change | [51] |
| 30 | Evaluation of the 4Ms Geriatric Framework | Cohort study; interdisciplinary team feedback and implementation in dental clinic settings | [52] |
| 31 | Simulation-based preclinical training | Experimental comparison of typodonts vs. haptic simulators for crown preparation | [53] |
| No | Implementation Type | Methods | Sources |
|---|---|---|---|
| 32 | Blooming Anatomy Tool for Assessment Design | Curriculum tool development; scaffolded assessment creation | [54] |
| 33 | Session Integration Tool (SIT) for Integrated Learning | Framework development; instructional design | [55] |
| 34 | Simulation-Based Communication Training | Prospective cohort study; lecture, practical sessions, simulated patient interaction | [56] |
| Educational Guideline | Bloom’s Level(s) | Supporting Studies |
|---|---|---|
| 1. Theoretical Foundations in Clinical Context | Remember, Understand, Apply | [27,32,38,39] |
| 2. Integrative and conceptually driven learning | Remember, Understand, Analyse | [24,25,27,28,40,43] |
| 3. Reflective Practice with Traditional Teaching | Understand, Analyse, Evaluate | [31,43] |
| 4. Analytical Reasoning | Apply, Analyse, Evaluate | [21,37,40,43,45,46,47] |
| 5. Embedding Evidence-Based Teaching | Understand, Apply, Evaluate | [29,30,38,49] |
| 6. Home Care Delivery Models | Apply, Analyse, Evaluate | [47,52] |
| 7. Evaluation-Driven Learning | Apply, Analyse, Evaluate | [48,49,50,51,53] |
| 8. 4Ms Framework | Apply, Evaluate | [52] |
| 9. Simulation-Based Methods | Apply, Analyse, Evaluate | [39,53,56] |
| 10. Soft Skills Integration | Understand, Evaluate, Create | [21,31,50,51,56] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Naka, O.; Chatzidou, P.; Pezarou, L.C.; Anastassiadou, V. Reforming Dental Curricula: A Student-Centred Novel Approach Integrating Prosthodontic Care for Older Adults. Oral 2025, 5, 73. https://doi.org/10.3390/oral5040073
Naka O, Chatzidou P, Pezarou LC, Anastassiadou V. Reforming Dental Curricula: A Student-Centred Novel Approach Integrating Prosthodontic Care for Older Adults. Oral. 2025; 5(4):73. https://doi.org/10.3390/oral5040073
Chicago/Turabian StyleNaka, Olga, Panagiota Chatzidou, Lisa Christina Pezarou, and Vassiliki Anastassiadou. 2025. "Reforming Dental Curricula: A Student-Centred Novel Approach Integrating Prosthodontic Care for Older Adults" Oral 5, no. 4: 73. https://doi.org/10.3390/oral5040073
APA StyleNaka, O., Chatzidou, P., Pezarou, L. C., & Anastassiadou, V. (2025). Reforming Dental Curricula: A Student-Centred Novel Approach Integrating Prosthodontic Care for Older Adults. Oral, 5(4), 73. https://doi.org/10.3390/oral5040073







