Abstract
The global demographic transition toward an ageing population has necessitated substantive reforms in dental education, particularly within the field of geriatric prosthodontics. Conventional curricula have frequently prioritized technical competencies while insufficiently addressing the integration of biological, psychosocial, and ethical complexities inherent in the care of older adults. This scoping review critically examined these curricular deficiencies by synthesizing evidence from 34 peer-reviewed studies, employing Bloom’s Taxonomy as a conceptual framework to inform a systematic and pedagogically grounded curriculum redesign. The primary aim was to identify existing gaps in undergraduate and postgraduate education, evaluate the efficacy of active and simulation-based learning modalities, assess the utility of reflective practices and standardised assessment tools, and formulate strategic, taxonomy-aligned pedagogical guidelines. Following the PRISMA-ScR methodology, the included studies were thematically analysed and categorized across the six cognitive levels of Bloom’s Taxonomy. Findings highlighted the effectiveness of integrated educational strategies, including Case-Based Learning, interprofessional education, virtual simulations, and structured assessments such as Objective Structured Clinical Examinations (OSCE). Furthermore, reflective models such as “What? So What? Now What?” fostered higher-order cognitive processes, ethical reasoning, and self-directed learning. By aligning cognitive levels—from foundational knowledge recall to innovative creation—ten evidence-based educational guidelines were developed. These guidelines are pedagogically sound, empirically supported, and adaptable to diverse curricular contexts. The proposed framework ensures a deliberate, progressive trajectory from theoretical comprehension to clinical expertise and ethical leadership. Future research should explore longitudinal outcomes and develop scalable, culturally responsive models to support the broader implementation of curricular reform in geriatric dental education.
1. Introduction
Global population ageing is one of the most significant demographic and public health shifts of the 21st century. For the first time, older adults now outnumber children worldwide, driven by increased life expectancy, from around 50 years in the early 1900s to over 79 in many developed countries. While these advances represent remarkable progress in medicine and public health, they also create complex challenges, especially in supporting the rapidly growing “oldest old” (aged 85+), whose increasing numbers are exerting unprecedented pressure on both medical and social infrastructures [1]. This demographic shift has led to a more diverse older population, characterised by significant differences in age, health, education, socioeconomic status, culture, and values. Ageing often comes with multiple chronic conditions that have atypical or overlapping symptoms, making diagnosis and treatment more difficult. Common geriatric syndromes—such as falls, cognitive issues, incontinence, and loss of independence—further weaken physical and mental health, increasing vulnerability and lowering quality of life. Although non-communicable diseases (NCDs) are more prevalent now, they are being diagnosed earlier and managed more effectively, allowing many older adults to live longer with improved functioning. However, they may experience more prolonged periods of illness [2]. In response to these challenges, the World Health Organisation [3] promotes the concept of healthy and active ageing, advocating for inclusive, supportive, and socially connected environments. Dentistry—particularly prosthodontics—plays a vital role within this broader context. Older adults retain more natural teeth, leading to increasingly complex restorative, periodontal, and prosthodontic needs. Chronic systemic diseases such as cardiovascular conditions, diabetes, cancer, and neurodegenerative disorders, along with age-related changes like mucosal atrophy, sensory decline, polypharmacy, and alterations in oral microbiota, further complicate dental treatment [4,5,6,7,8,9].
Medication-induced xerostomia increases caries risk, impairs mastication, and worsens nutritional deficiencies. Edentulism alone has been linked to a 21% increased risk of malnutrition, significantly lowering quality of life and speeding up systemic decline [10].
Impaired chewing capacity (ICC) has been linked to reduced diet quality and accelerated ageing, leading to an increased mortality risk. Consequently, dietary interventions and oral rehabilitation may support healthy longevity, though further research is necessary to confirm these effects [11].
The role of the dental prosthodontist is therefore evolving. Beyond restoring form and function, prosthodontists now also manage frail, vulnerable older adults by evaluating their oral and systemic health and determining their capacity to handle clinical procedures. This work must occur within a broader framework that integrates oral health into overall health and positions oral health as a crucial part of healthy ageing, possibly a new “geriatric giant” [12].
Despite the increasing importance of gerodontology, it remains inadequately covered in many dental curricula worldwide. Dental education has generally been traditional, emphasising technical skills specific to the prosthodontic discipline but rarely incorporating biopsychosocial considerations for seniors. In response to these deficits in educational offerings, contemporary curricula have evolved toward competence-based instructional blueprints focused on lifelong learning, patient safety, and professionalism. These approaches are increasingly in line with global efforts to promote lifelong learning and encourage the creation of evidence-based health policies. Within the undergraduate area, there is a growing emphasis on the provision of interdisciplinary and evidence-based education in geriatric oral care. The integration of new holistic approaches in teaching curricula guides comprehensive and patient-centred care designed to accommodate the individual aspects of ageing, such as the What Matters, Medication, Mentation, and Mobility (4Ms) framework [13,14,15,16,17,18,19,20]. To effectively meet the needs of ageing populations, dental education must undergo substantial reform, embedding these principles into academic and clinical training environments by integrating foundational biomedical knowledge into real-world contexts, supporting reflective practice, and fostering interprofessional collaboration. Active learning methodologies, including Case-Based Learning, simulation, and digital tools like serious games and virtual reality, have shown promise in enhancing diagnostic reasoning and clinical competence [21,22]. Equally important is the integration of soft skills such as empathy, communication, and cultural sensitivity, which are essential to navigating the ethical and interpersonal complexities of geriatric care [23].
The motivation for conducting this scoping review stems from the pressing need to enhance educational approaches that tackle the intricate oral health issues faced by ageing populations. While there is an increasing clinical recognition of geriatric care, numerous dental education programs still lack comprehensive and interdisciplinary frameworks that adequately encompass the diverse, multifactorial, and biopsychosocial dimensions of ageing. Thus, this scoping review aims to identify and consolidate current educational standards, advancements in curricula, and innovative teaching methods within geriatric dental education, ultimately contributing to the creation of integrated, evidence-based curricula. Guided by the principles proposed by the Integrated Care for Older People (ICOPE) guidance for person-centred assessment and pathways in primary care, and organised according to Bloom’s Taxonomy, the review evaluates the degree to which interdisciplinary and person-centred strategies are utilised to meet the complex oral health requirements of older adults.
The objectives were to (1) identify gaps in undergraduate and postgraduate dental education, focusing on how biological, psychological, and social factors of ageing are integrated into geriatric prosthodontics; (2) evaluate the effectiveness of active, evidence-based learning methods—such as Case-Based Learning (CBL), Problem-Based Learning (PBL), simulation-based training, and interprofessional education—in developing higher-order thinking, diagnostic, and decision-making skills; (3) assess the impact of standardised assessment tools, including Objective Structured Clinical Examinations (OSCE) and reflective models (e.g., “What? So What? Now What?”), on enhancing clinical competence and self-directed learning; and (4) propose structured teaching guidelines for a spiral curriculum based on Bloom’s Taxonomy, aimed at promoting the development of ethical, person-centred care competencies in the management of complex geriatric cases.
2. Materials and Methods
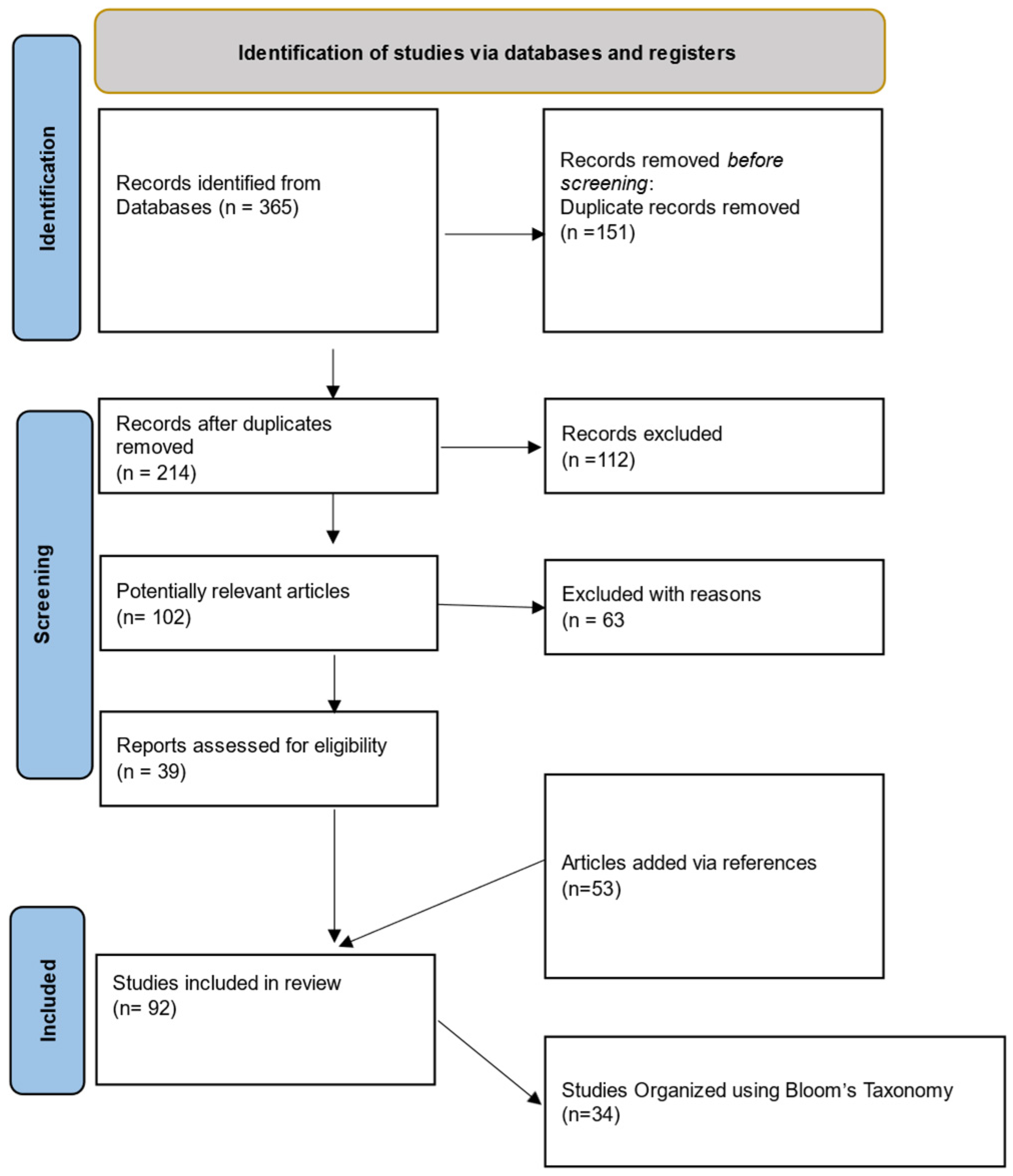
This scoping review was conducted following the PRISMA-ScR 2020 (extension for scoping reviews) guidelines to ensure methodological rigour, transparency, and reproducibility (Figure 1).
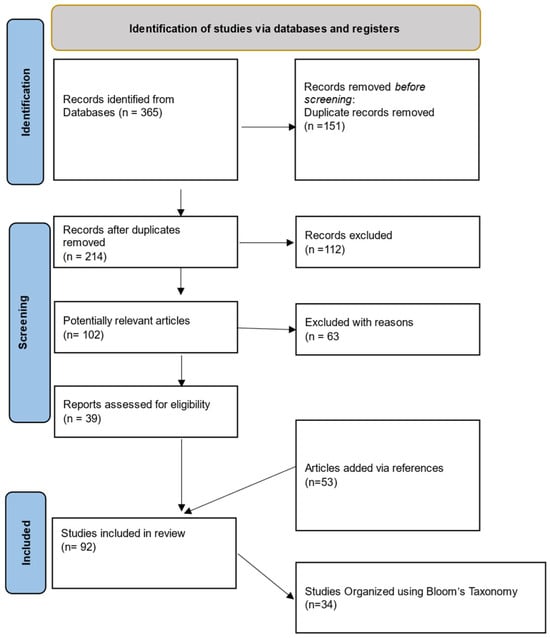
Figure 1.
PRISMA-ScR flowchart.
The review was structured using the PICO framework, guiding the identification and synthesis of studies focusing on educational innovations in geriatric prosthodontics. The population of interest included older adults aged 65 and above, as well as educators and dental and medical students engaged in patient training. The interventions evaluated comprised competence-based and integrated pedagogical strategies, such as Case-Based Learning (CBL), Objective Structured Clinical Examinations (OSCE), virtual simulations, and interprofessional education. Comparisons were made between traditional medical and dental curricula—characterised by fragmented content delivery and limited clinical integration—and more modern, cohesive educational approaches. The primary outcomes measured included improvements in cognitive and procedural skills, development of critical thinking, student engagement, and readiness to provide holistic, person-centred care to ageing populations.
A comprehensive literature search was performed across four electronic databases: PubMed, Scopus, Web of Science, and Cochrane CENTRAL. The search strategy combined Medical Subject Headings (MeSH) and the free-text keywords “geriatric dentistry,” “geriatric prosthodontics,” “dental education,” “curriculum reform,” “Bloom’s Taxonomy,” “active learning,” “Objective Structured Clinical Examination (OSCE),” and “reflective practice.”, targeting studies published in English. To ensure comprehensiveness, the search also included relevant key documents, reference lists from included articles, and policy documents from organisations such as the World Health Organisation (WHO).
Study selection involved a two-phase independent screening process by two reviewers. First, titles and abstracts were assessed against predefined inclusion and exclusion criteria aligned with the PICO framework. Studies meeting initial eligibility moved to full-text review in the second phase. Disagreements regarding inclusion were resolved or, if necessary, resolved by consulting a third reviewer.
Studies (n = 92) were included if they were published in English, focused on medical or dental students in institutional training, and evaluated integrated, competence-based educational strategies, without a chronological timeframe. Outcomes related to cognitive development or skill acquisition, connected to pedagogical frameworks, were required. Studies were excluded if they focused solely on clinical outcomes without an educational component or were non-peer-reviewed sources such as opinion pieces or editorials.
A standardised data extraction form was used on the final set of 34 studies. Data collected included the type of educational intervention, study design, and referenced frameworks. These data were organised and analysed thematically in the Section 3, with summaries presented in Table 1, Table 2, Table 3, Table 4, Table 5 and Table 6.

Table 1.
Bloom’s Taxonomy- “Remember” Level.

Table 2.
Bloom’s Taxonomy-“Understand” Level.

Table 3.
Bloom’s Taxonomy-Apply” Level.

Table 4.
Bloom’s Taxonomy-“Analyse” level.

Table 5.
Bloom’s Taxonomy-“Evaluate” level.

Table 6.
Bloom’s Taxonomy-“Create” level.
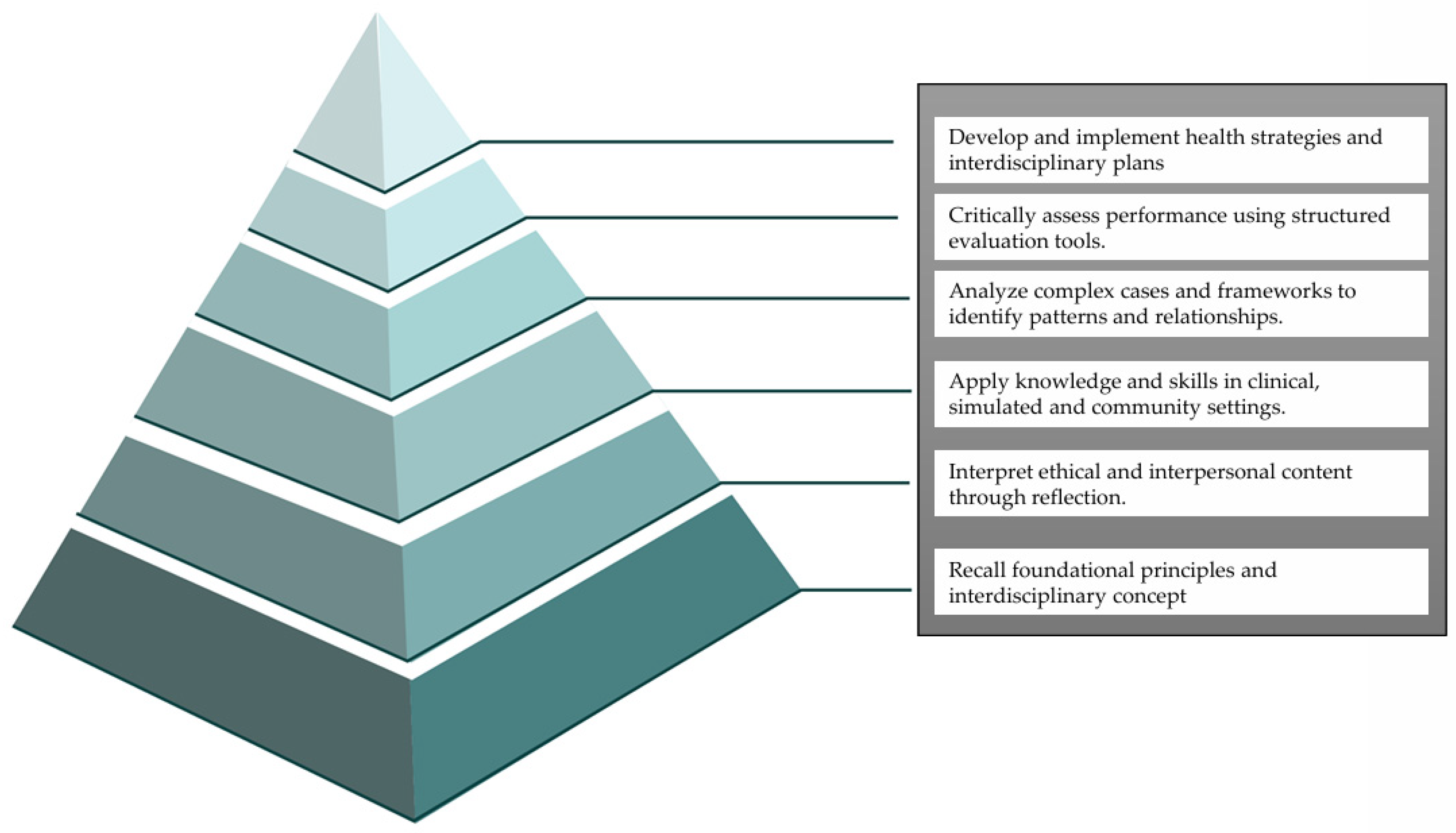
Finally, the strategies and outcomes of each study were examined according to the six domains of Bloom’s Taxonomy (Figure 2): Remember, Understand, Apply, Analyse, Evaluate, and Create. The latter aimed to determine whether the educational innovations effectively promoted knowledge, skills, interdisciplinary collaboration, and higher-order thinking, crucial for delivering effective geriatric dental care.
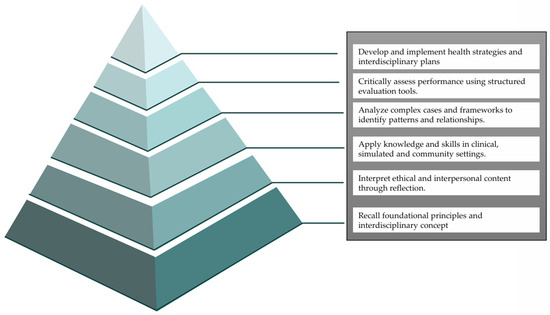
Figure 2.
Organisation of studies according to the six levels of Bloom’s Taxonomy.
3. Results
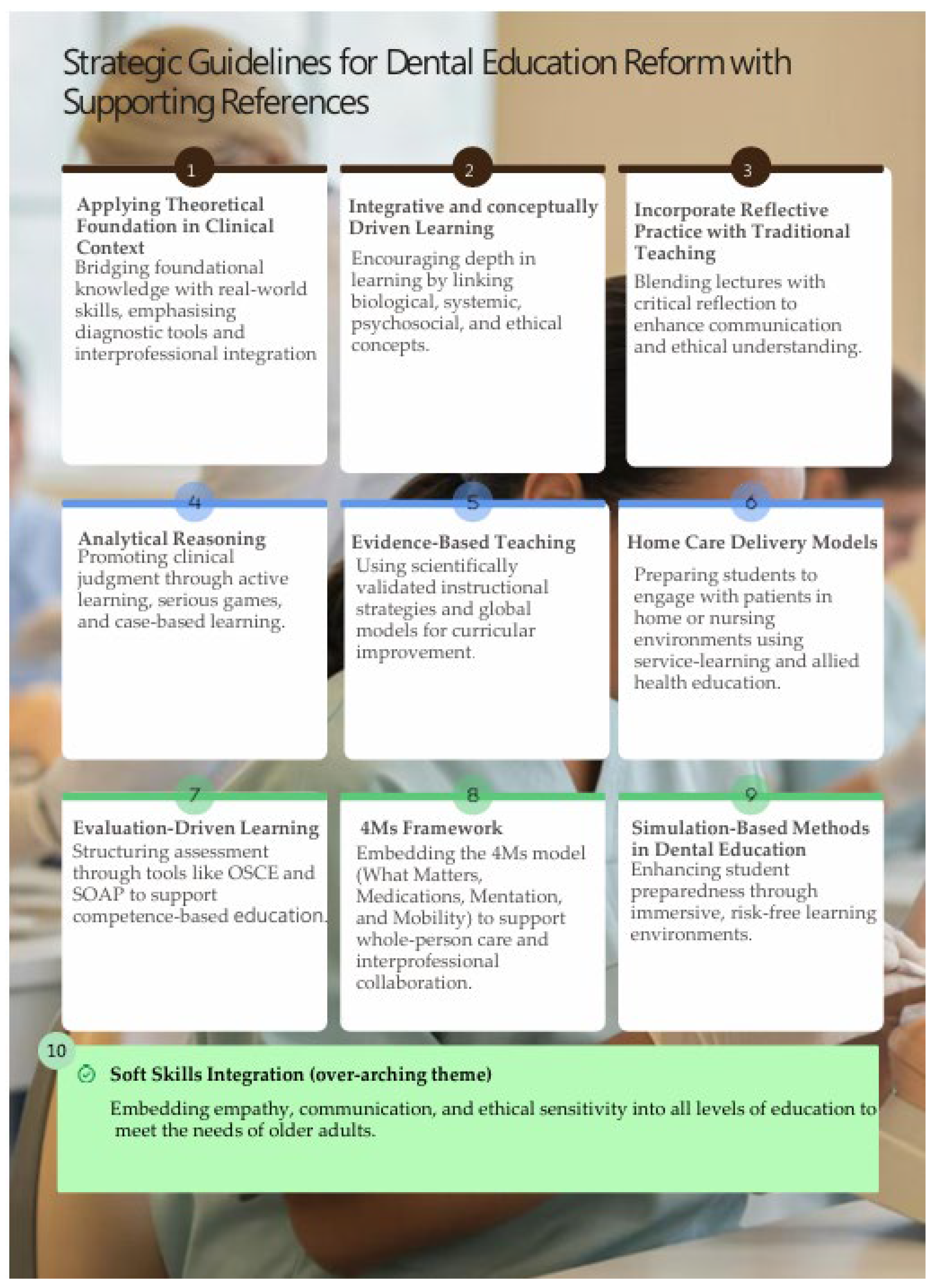
The 34 specific studies included in this scoping review were organised according to the six levels of Bloom’s Taxonomy (Figure 2) and are presented in Table 1, Table 2, Table 3, Table 4, Table 5 and Table 6, providing a structured framework to assess the cognitive complexity and pedagogical strategies used in gerodontology education. Using Bloom’s categorisation, the review identified strategic educational guidelines intended to improve teaching and learning effectiveness in dentistry. These guidelines, designed to boost the effectiveness and efficiency of academic practices, were synthesised and are summarised in Figure 3.
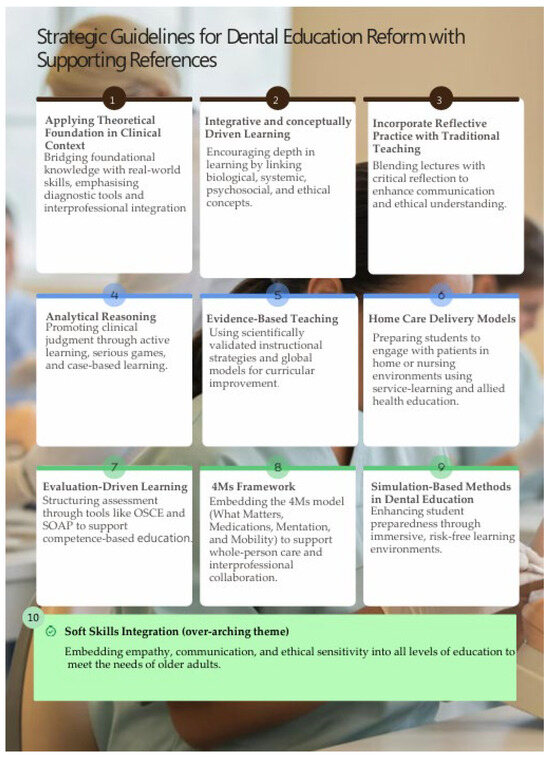
Figure 3.
Strategic Guidelines for Dental Education Reform and Supporting References, 1: Chalmers et al. (2002) [32]; Maharjan et al. (2018) [27]; Tebcherany and Khocht (2024) [38]; Bencharit et al. (2025) [39], 2: Lajber et al. (2020) [28]; Maharjan et al. (2018) [27]; Kerosuo et al. (2001) [40]; Chambers (2009) [43], 3: Estrela et al. (2024) [31]; Chambers (2009) [43], 4: Parikh et al. (2022) [21]; Lin and Yang (2023) [37]; Kerosuo et al. (2001) [40]; Manchery et al. (2022) [45]; Nagatani et al. (2023) [46]; Allenspach et al. (2024) [47], 5: Morton et al. (2017) [29]; Bansal et al. (2021) [30]; Tebcherany and Khocht (2024) [38]; Al Khalaf et al. (2022) [49], 6: Allenspach et al. (2024) [47]; Arany et al. (2024) [52], 7: Anderson et al. (2000) [48]; Al Khalaf et al. (2022) [49]; Nayak et al. (2023) [50]; Singh et al. (2024) [51]; Hadjichristou et al. (2022) [53], 8: Arany et al. (2024) [52], 9: Hadjichristou et al. (2022) [53]; Bock et al. (2024) [56]; Bencharit et al. (2025) [39], 10: Parikh et al. (2022) [22]; Estrela et al. (2024) [31]; Bock et al. (2024) [56]; Nayak et al. (2023) [50]; Singh et al. (2024) [51].
3.1. Foundations in Cognitive Recall Memory
Research into cognitive processes like “Remembering” has highlighted how students and educators perceive and recall curricular structures, which is key for developing student-centred models of integrated care for older adults.
3.1.1. Student Recall of Foundational Knowledge from Memory
Early qualitative studies by Beattie et al. (1997) and Marton et al. (1976) [24,25] demonstrated that factors beyond simple categories, such as deep or surface learning, influence learners’ memories of their educational experiences. Beattie et al. [24] challenged these simplistic labels, promoting more nuanced, student-responsive approaches. Similarly, Marton [25] emphasised the impact of variation in recall and expression on learning outcomes, particularly in multidisciplinary settings.
3.1.2. Faculty Recall of Foundational Knowledge
Strandell (1980) [26] found that faculty often remembered using integrated teaching methods, reflecting a shared understanding of curricular goals. These memories help build institutional knowledge and guide curricular reforms aligned with interdisciplinary geriatric care needs.
3.1.3. Recall of Basic Science Concepts in Clinical Contexts
Maharjan et al. (2018) [27] investigated faculty and student perceptions around the integration of basic sciences into clinical education. They argued that organ-system-based curricula, supplemented by Problem-Based Learning (PBL), increase proficiency in knowledge retention with conceptually driven learning. Their results highlighted the importance of evidence-based teaching methods, with outcomes aligned to learning goals, for collaboration in curriculum vertical integration and the creation of supportive learning environments. The traditional lectures are contrasted with the theoretical foundation applied to clinical strategies, which combine an active and integrative engagement in bridging theory to practice.
3.1.4. Student Recall of Perceived Clarity and Motivation in Integrated Learning
Lajber et al. (2020) [28] further examined medical students’ views on integration, reporting that 90% recognised an improved understanding and motivation, even though only 3% provided positive feedback on the overall integrated curriculum. Their study described pedagogical methods like Case-Based Learning (CBL), which offers structured guidance and emphasises application, and Team-Based Learning (TBL), which encourages collaboration and readiness. These insights, derived from integrative and conceptually driven learning, support curricular clarity and manageability, which are essential for enhancing cognitive retention and practical application in geriatric education.
Overall, these studies emphasised the importance of incorporating cognitive principles into curriculum development to improve knowledge retention, student engagement, and clinical relevance. These components are critical for equipping professionals to provide integrated care for older adults, where interdisciplinary teamwork and a solid grounding in core knowledge are crucial (Table 1).
3.2. Developing Understanding of Interdisciplinary Frameworks
At Bloom’s “Understanding” level, the focus shifts from simple recall to the ability of students and educators to interpret, contextualise, and connect ideas across disciplines, crucial for developing dental curricula that support integrated geriatric care.
3.2.1. Assessment-Informed Learning Design
Morton et al. (2017) [29] demonstrated that assessment formats significantly influence learning behaviours, particularly in anatomy and physiology. Their findings support the implementation of evidence-based teaching practices that align assessments with strategies that promote interpretive thinking and integrated understanding, moving beyond rote memorisation to prepare students for the complexities of caring for older adults, blending didactic and reflective approaches to foster ethical and communication skills. These practices combine both theoretical and reflective methods to cultivate ethical reasoning and communication abilities. Consequently, this not only promotes ethical and communicative skills but also improves the overall quality of teaching while ensuring the curriculum remains coherent and compelling.
3.2.2. Learning Strategy Evaluation
Bansal et al. (2021) [30] found that students employing deep and strategic learning methods performed better academically (p < 0.05), while low achievers relied on surface approaches (p < 0.05). A Student’s t-test was conducted to detect statistical differences in the learning approaches of low and high achievers, and point-biserial correlation was used to examine the relationship between academic performance and learning approaches. Notably, fear of failure was more common among high achievers, and gender differences appeared in subscales such as lack of purpose, syllabus-bound behaviours, unrelated memorisation, time management, and organised studying. These results deepen conceptual understanding and highlight the need to foster deeper engagement to improve clinical reasoning in student-centred, evidence-based geriatric teaching.
3.2.3. Case-Based and Didactic Integration
Parikh et al. (2022) [21] reported that 83% of dental students believed that a combined didactic and case-based model improved their understanding (p < 0.001), with 75% noting increased engagement and critical thinking (p < 0.001) and 69% favouring full curriculum integration (p < 0.001). Data were tested with Pearson’s chi-squared tests, as well as Kruskal-Wallis rank sum tests at a statistical significance of 95%. Significant differences across academic years for p-values < 0.01 indicated that students better understood complex concepts when such concepts were applied in real-time clinical settings. The combination of theoretical knowledge and practical application, rooted in a solid pedagogical framework, promotes thorough and contextual comprehension by utilising theoretical principles in clinical settings. This method incorporates clinical reasoning, professionalism, interprofessional collaboration, and holistic care throughout the curriculum, facilitating the incorporation of soft skills crucial for successful healthcare practice.
3.2.4. Faculty-Student Communication
Estrela et al. (2024) [31] emphasised that effective faculty–student communication improves understanding and engagement. The study gathered data from questionnaires filled out by third- to fifth-year undergraduate dentistry students and professors. Responses were statistically analysed using a significance level of 95%. The student’s t-test compared reactions between groups. However, significant perception gaps existed between students and faculty (p < 0.001), with 47% of students feeling neutral or dissatisfied with teaching methods, 24% citing limited use of technology, and many reporting low ratings for communication and support. These results highlighted the significance of communication and constructive feedback, stressing the benefits of combining reflective practice with conventional teaching methods to enhance adaptive instruction. Such a strategy cultivates trust and aids in the incorporation of soft skills, directly connecting education to patient-centred care in geriatrics.
Overall, these studies support redesigning dental curricula to include integrated assessments, interactive tools, and strong faculty–student engagement, thereby preparing students for interdisciplinary, empathetic, and context-aware care in an ageing population (Table 2).
3.3. Apply Knowledge in Practical, Clinical, and Team-Based Settings
At Bloom’s “Applying” level, research increasingly stresses active, interdisciplinary learning that fosters student-centred education for integrated care of older adults.
3.3.1. Standardised Clinical Tools
Chalmers et al. (2002) [32] validated the Oral Health Assessment Tool (OHAT) in residential aged care, highlighting its reliability and usefulness in training students to carry out standardised oral assessments. This is an essential aspect of geriatric care, as it establishes the foundation for practical skills and guarantees that students can implement theoretical concepts in clinical environments by making informed choices and collaborating effectively.
3.3.2. Motivational Learning
Prat-Sala and Redford (2010) [33] demonstrated that motivation and self-efficacy significantly influence the application of knowledge, highlighting the importance of self-regulated learning strategies in interdisciplinary education focused on older adult care.
3.3.3. Retrieval-Based Practice
Through experimental methods, Agarwal (2019) [34] confirmed that retrieval practice improves learning outcomes, supporting its integration into health education to strengthen factual recall and clinical application in older populations.
3.3.4. Multimedia Clinical Integration
Miller and Metz (2015) [35] utilised clinical scenario videos to bridge the gap between basic science and practice. First-year dental students showed a 6.2% improvement in clinical scores, and 96% valued physiology more than did fourth-year students (57%). Students initially struggled to apply physiological knowledge but improved significantly in two of three modules, indicating that enhanced multimedia materials help integrate complex content like age-related topics and pathophysiology.
3.3.5. Interdisciplinary Physiology
Hobbins et al. (2020) [36] emphasised the importance of interdisciplinary, higher-level physiology instruction for training students to handle complex health issues in older adults.
3.3.6. Digital-Game-Based Learning
Lin and Yang (2023) [37] demonstrated that digital-game-based learning, which combines behavioural science and clinical communication, improves student engagement and knowledge application. Descriptive statistics summarised participant data. Non-parametric tests, at a statistical significance level of 95%, included Wilcoxon signed-rank (pre/post), Mann–Whitney U (groups), and Spearman’s rho (correlations), with Bonferroni correction (α = 0.008) and effect sizes estimated. The clinical dentist-patient communication (CDPC) game increased motivation and self-efficacy among preclinical students (p < 0.05), with motivation being linked to beliefs (p = 0.024) and self-efficacy (p = 0.001). This method promoted the development of clinical judgment, critical thinking, and diagnostic precision—essential aspects of analytical reasoning—while also equipping students to manage the intricacies of communicating with geriatric patients.
3.3.7. Evidence-Based Instruction
Tebcherany and Khocht (2024) [38] found that the use of theoretical frameworks and interdisciplinary ideas in clinical practices, along with the incorporation of evidence-based teaching methods in periodontics, enhanced students’ understanding (p = 0.0001), attitudes (p = 0.0001), evidence access (p = 0.01), and confidence (p = 0.009), and they significantly higher final grades (p = 0.001), validating the role of research-informed instruction in clinical practice readiness. For the results’ analysis, descriptive and inferential methods were used. Normality was checked with goodness-of-fit. Paired t-tests, Wilcoxon signed-rank, McNemar’s, and Pearson chi-square tests were applied. statistical significance level was set at 95% with False Discovery Rate (FDR) correction for domain-, item-, and performance-level comparisons.
3.3.8. VR-Haptic Technology Integration
Bencharit et al. (2025) [39] conducted a comprehensive review of the worldwide implementation of VR-haptic technologies, highlighting numerous international initiatives. Their findings indicated that simulator-based approaches in dental education are interactive and practical, effectively bridging the gap between theoretical instruction and hands-on experience. These methods are primarily applied in preclinical courses, with 94% typically occurring within restorative and prosthodontic modules. The use of VR-haptics was linked to enhanced skill development and the capacity to transfer knowledge acquired in the classroom to real-world patient care, thereby facilitating advancement into more sophisticated clinical responsibilities. Conversely, simulation-based strategies faced challenges related to expenses, technological constraints, and barriers to adoption. To improve overall efficacy and accessibility, recommendations included the incorporation of AI for personalised learning experiences and the use of gamification techniques.
Collectively, these studies supported student-centred, experiential teaching methods rooted in interdisciplinary integration, clinical engagement, and real-world relevance, which are essential for preparing dental professionals to serve ageing populations (Table 3).
3.4. Analysing Knowledge to Dissect Complex Cases and Frameworks and Identify Patterns and Relationships
At Bloom’s “Analysing” level, students enhance critical thinking by dissecting information, recognising relationships, and interpreting data—crucial skills for interdisciplinary, student-centred care for older adults. Over time, analytic learning has significantly contributed to curriculum development and better clinical outcomes (Table 4).
3.4.1. Integrated Preclinical and Clinical Curriculum
Kerosuo et al. (2001) [40] presented an early model of curriculum reform consisting of a two-year integrated preclinical course and 1440 h of competence-based clinical training. Student feedback favoured a team-based approach with self-evaluation, and evidence showed that clinical competence had not declined. Results indicated that the integration of biomedical knowledge with casework is supported through analytical reasoning and conceptually driven learning, which can be used to promote student application in clinical practice and collaborative decision-making.
3.4.2. Higher-Order Thinking
Crowe et al. (2008) [41] found that higher-order thinking in biology enhances student learning.
3.4.3. Curriculum-Integrated Research Seminars
Kingsley et al. (2008) [42] expanded this by integrating research projects into early dental education. These structured seminars, though challenged by logistical and funding constraints, increased student engagement and promoted deeper analysis of biomedical and geriatric clinical concepts.
3.4.4. Critical Thinking Curriculum
Chambers (2009) [43] utilised qualitative approaches to evaluate a critical thinking course for eight years. The findings indicated that critical thinking encompasses knowledge, skills, and values, and is shaped by individual personality traits and practical experience. The research advocated for incorporating reflective practice in conjunction with traditional teaching methods, suggesting that the development of analytical reasoning and the integration of interdisciplinary content are essential for cultivating the comprehensive skills necessary to navigate the medical, ethical, and social challenges in the care of older adults.
3.4.5. Cross-Disciplinary Assessment Models
Rougas et al. (2014) [44] evaluated a hands-on workshop that improved health professions education researchers’ ability to apply theoretical frameworks. Participants reported increased confidence and valued the active learning methods adaptable across disciplines.
3.4.6. Oral Health as a Cognitive Decline Indicator
Manchery et al. (2022) [45] and Nagatani et al. (2023) [46] utilised analytical reasoning frameworks to investigate the relationship between oral health and cognitive decline. Their research highlighted key findings, including the clinical significance of chewing capacity and tongue pressure. These insights demonstrated how students can leverage diagnostic information to formulate preventive strategies related to dementia, underscoring the necessity of fostering clinical judgment and critical thinking skills.
3.4.7. Preventive Domiciliary Dental Care
Allenspach et al. (2024) [47] illustrated that employing analytical reasoning within collaborative and preventive strategies enhanced oral health in home care environments. Their study underscored the importance of training students to critically evaluate and implement home care delivery models for institutionalised older adults.
3.5. Critical Evaluation of Knowledge: Making Informed Judgments Based on Established Criteria and Evidence
The evaluating level of Bloom’s Taxonomy focuses on critical judgment and decision-making, key skills for providing comprehensive, patient-centred care to older adults. A timeline of studies highlights how evaluation-focused learning improves curriculum innovation, interdisciplinary teamwork, and clinical practice outcomes.
3.5.1. Revised Bloom’s Taxonomy for Curriculum Coherence
Anderson et al. (2000) [48] provided a foundational revision of Bloom’s Taxonomy applicable across disciplines, highlighting how evaluation-based frameworks enhance teaching effectiveness, learning outcomes, and curricular coherence. This evaluation-driven learning model supported educational strategies that enable learners to assess clinical priorities and ethical considerations, especially in geriatric settings.
3.5.2. Curriculum Evaluation and Consensus Building
Al Khalaf et al. (2022) [49] carried out a Delphi study with the participation of 23 senior academics in prosthodontics from 11 different countries. The study achieved a response rate of 78.3% and reached a consensus (≥70%) on 92.6% of the 189 pedagogical statements examined. The results produced expert-backed recommendations aimed at globally standardising undergraduate education in prosthodontics. These outcomes have the potential to minimise educational inequalities, enhance patient care, and reinforce the connection between evidence-based teaching and assessment-driven learning models.
3.5.3. Evaluation of Integrated Curriculum Modules
Nayak et al. (2023) [50] evaluated the AETCOM (Attitudes, Ethics, and Communication) module’s impact on medical students at various training stages. Using attitude scales and feedback, the research indicated an enhancement in communication attitudes, especially among interns, with 80% indicating that the modules were pertinent to clinical practice, demonstrating a successful incorporation of soft skills. Faculty recognised the importance of the module but also proposed improvements, which is consistent with an evaluation-driven learning model.
3.5.4. Assessment of Student Attitudes in Geriatric Dentistry
Singh et al. (2024) [51] conducted a survey involving 312 dental students from the Delhi–NCR area, which showed a predominantly empathetic perspective towards geriatric care, suggesting the incorporation of soft skills. Postgraduate students exhibited notably greater confidence and readiness to provide care for older adults. Nevertheless, all groups of students stressed the importance of enhanced geriatric education, advocating for workshops and practical clinical experiences, thereby underscoring the tenets of a learning model focused on evaluation.
3.5.5. Evaluation of the 4Ms Geriatric Framework
Arany et al. (2024) [52] reported on the early adoption of the 4Ms framework—What Matters, Medications, Mentation, and Mobility- in dental clinics. While lacking statistical information, the research highlighted improved interdisciplinary collaboration and stressed the importance of student involvement in assessing comprehensive care strategies, which correspond to home care delivery frameworks.
3.5.6. Simulation-Based Preclinical Training
Hadjichristou et al. [53] compared crown preparation of typodont and haptic simulators (as a simulation-based technique) among 54 second-year dental students. The total occlusal convergence (TOC) angles were slightly greater using haptic simulators, although all methods satisfied the clinically accepted norms. Students appreciated the benefits of haptic technology during their learning process, but still preferred typodonts. This suggested that haptic-enabled tools were helpful, but they served better as a supplement to traditional preclinical prosthodontic education in an assessment-intensive context.
Collectively, these studies highlight the importance of evaluative thinking in developing adaptive, student-centred curricula that focus on high-quality, interdisciplinary care for ageing populations (Table 5).
3.6. Creating Frameworks for Student-Centred Older Care: Designing and Developing Care Plans and Interventions
At Bloom’s Creating level, innovation and synthesis drive the development of new educational strategies, tools, and frameworks that support student-centred learning within integrated geriatric care.
3.6.1. Blooming Anatomy Tool for Assessment Design
Thompson and O’Loughlin (2015). [54] advanced curriculum design through the Blooming Anatomy Tool, a flexible framework for creating anatomy assessments across cognitive levels. Initially designed for anatomical sciences, its adaptable structure supported interdisciplinary curricula, enabling scaffolded assessments that improve clinical understanding, key to teaching integrated care for older adults.
3.6.2. Session Integration Tool (SIT) for Integrated Learning
Heck and Chase (2021) [55] introduced the Session Integration Tool (SIT) to aid educators in designing, evaluating, and refining integrated session plans. Although lacking statistical data, SIT structured learning environments encourage cross-disciplinary synthesis, preparing students to create comprehensive care strategies for ageing populations.
3.6.3. Simulation-Based Communication Training
Bock et al. [56], for instance, provided a prospective cohort study involving 34 dental students and demonstrated that simulation-based techniques are effective in the training of dentists. Data were analysed at a statistical significance level of 95% using Wilcoxon signed-rank (within groups), Mann–Whitney U (between surveys), and Kendall’s W (interrater reliability) tests. The video-game-based learning intervention incorporated communication skills through an educational package that resulted in clinically significant improvements after a lecture and two hands-on simulated patient encounters for the students’ use of soft skills (p < 0.001), with a trend toward increased open-ended questions (p = 0.0245). The students realised that this training would not be confined to a library setting but would instead enhance their personal and professional development, including the adaptation of communication styles for older adults. The interactive nature of this experience allowed each student to see how the didactic material could be translated into clinical skills and ultimately empathy.
In sum, the results of these studies illustrated a hierarchical curriculum path that began with the lowest types of cognitive ability (i.e., memory and comprehension) and progressed to more complex forms of mental processing (i.e., critical thinking, clinical reasoning, problem-solving). Using simulated case-based learning, students transitioned from rote memorisation to problem-solving scenarios. The curriculum was inspired by evidence-supported clinical reasoning [53], as dentistry is becoming more interprofessional and systematic. This shift requires better integration with general health concepts, ultimately leading to competencies necessary for effective dental practice.
Overall, the evidence highlighted the growing importance of innovative educational methods in encouraging student-centred, integrative learning in geriatric oral health and interdisciplinary care. The resulting academic implementations derived from these findings are presented in Table 6.
3.7. Generating Student-Centred Guidelines for Dental Curriculum Reform in Older Adult Prosthodontic Care
To derive practical information from the literature, a systematic analytical method was employed to produce 10 tips for teachers based on 34 selected works (Figure 3).
Aligning with the aims of a scoping review, the approach aimed at demonstrating the range of different educational strategies and teaching designs, as opposed to conducting statistical comparisons of outcomes.
The criteria were developed using deductive and inductive reasoning. The studies were arranged deductively according to Bloom’s Revised Taxonomy, which includes six cognitive levels: Remember, Understand, Apply, Analyse, Evaluate, and Create. This inductive analysis of themes in each level focused on common instructional strategies, assessment practices, and employments. Each article’s methods, results, and discussion sections were examined in detail before being coded and systematically categorised. Themes that emerged were rated for frequency, clarity, and relevance to different fields of study, namely prosthodontics, gerodontology (oral care for older adults), interprofessional education, and educational psychology. The guidelines encompassed cognitive development, instructional design, student engagement, interdisciplinary integration, and ethical competencies in geriatric prosthodontics. Guidelines supporting evidence matrices (Table 7, Figure 4) illustrate the levels of Bloom’s Taxonomy that the studies relate to and their contributions to the themes.

Table 7.
Educational Guidelines Mapped to Bloom’s Levels and Supporting Literature. Cross-reference matrix aligning the ten strategic educational guidelines with Bloom’s cognitive taxonomy levels and the studies providing empirical support. This mapping highlights the multidimensional contributions of each study to geriatric prosthodontic education.
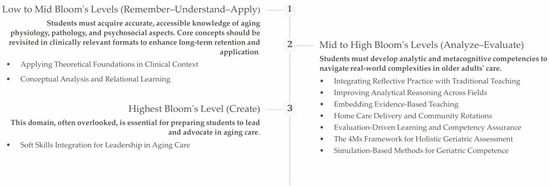
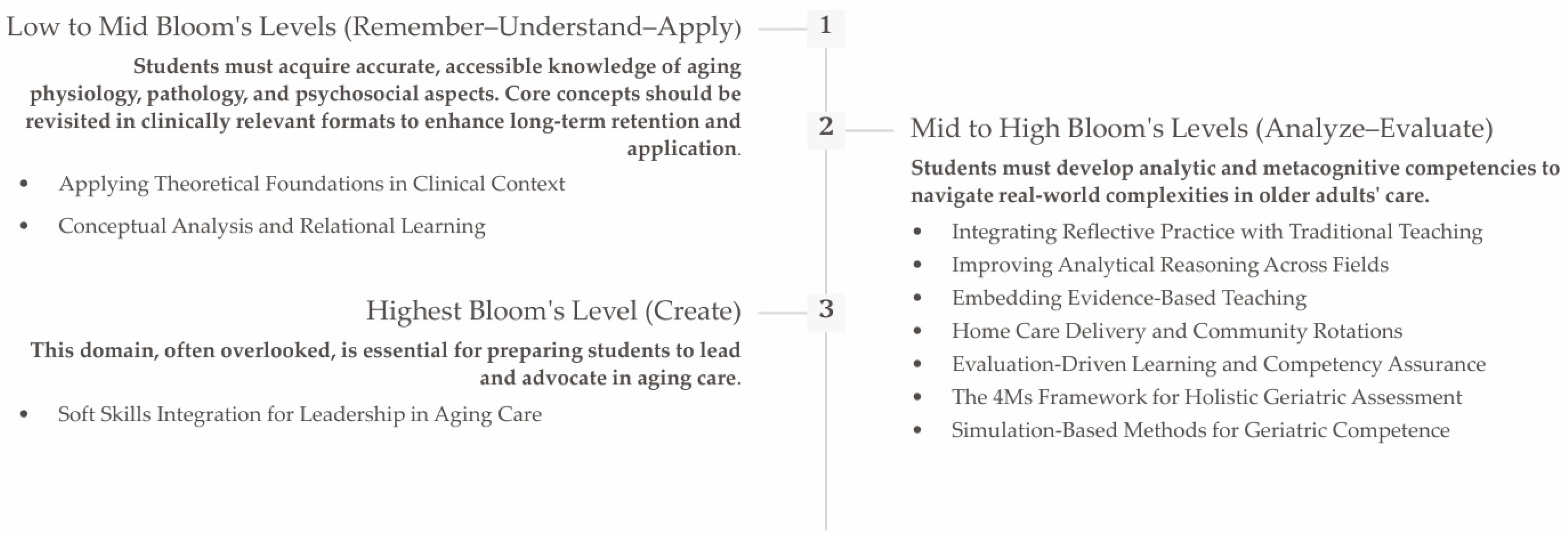
Figure 4.
Reforming Geriatric Prosthodontic Education Through Bloom’s Taxonomy and Strategic Guidelines.
Through an already structured framework stipulated in Bloom’s Taxonomy of educational objectives with deductive insights, the integrated process effectively captured coherence and diversity in innovation in education. This produced a suite of general, evidence-informed guidelines relevant to multiple curricular landscapes.
4. Discussion
Reforming geriatric prosthodontic education in the 21st century must extend beyond proficiency in “art and science” and integrate the essential dimension of soft skills. As Dalaya et al. (2015) [23] asserted, soft skills—including communication, empathy, problem-solving, and emotional intelligence—are crucial for establishing trust, managing patient care, and cultivating collaborative clinical environments. These interpersonal and intrapersonal attributes are not mere supplements but foundational to successful prosthodontic practice, particularly in the care of older adults, where nuanced communication, ethical sensitivity, and cultural competence are indispensable. In the context of an ageing population with complex medical needs, future dental professionals must be prepared with scientific and procedural knowledge and the ability to engage compassionately, adaptively, and reflectively.
4.1. Reforming Geriatric Prosthodontic Education Through Bloom’s Taxonomy and Strategic Guidelines
Reforming geriatric prosthodontic education requires a cognitively structured and clinically responsive approach, grounded in the realities of ageing care. Traditional dental education has often focused on biomedical skills, but the complexity of ageing patients calls for a reconceptualisation of the curriculum through Bloom’s Taxonomy. By aligning cognitive levels—from knowledge recall to creation—with ten strategic guidelines, educators can ensure a deliberate progression from foundational theory to clinical expertise and ethical leadership.
Bloom’s Taxonomy helped identify gaps in the curriculum and areas where instruction may become stagnant, especially regarding ageing-related content. A revised curriculum must combine cognitive scaffolding with experiential learning and interdisciplinary exposure. The proposed guidelines follow this progression, ensuring that the curriculum prepares learners to think, act, and innovate with older adults in mind.
4.1.1. Low to Mid Bloom’s Levels (Remember–Understand–Apply): Building Cognitive Foundations for Geriatric Understanding
At the foundation of the taxonomy, students must acquire accurate, accessible knowledge of ageing physiology, pathology, and psychosocial aspects. Core concepts should be revisited in clinically relevant formats to enhance long-term retention and clinical application.
1. Applying Theoretical Foundations in Clinical Context
Applying biomedical science in the context of ageing involves more than recalling facts—it requires connecting foundational knowledge with clinical reasoning. This connection is vital in geriatrics, where systemic decline affects oral function and prosthodontic adaptability [27,32,38,39]. Simulation-enhanced education and long-term case mapping help illustrate biological principles such as immunosenescence, neuromuscular decline, and polypharmacy.
However, the persistent theory–practice gap remains a barrier in dental and health professions education [57]. Students often experience disjointed transitions between classroom knowledge and clinical realities, which can decrease confidence and lead to fragmented care. Educational reforms must therefore address institutional and pedagogical inconsistencies, especially those that hinder the integration of didactic and practical instruction [58]. Additionally, therapeutic communication should be developed early to support the emotional and cognitive vulnerabilities of older patients.
2. Integrative and Conceptually Driven Learning
Shifting students away from rote memorization towards integrative thinking necessitates the use of strategies that encourage a more profound comprehension of interconnected ideas. Adopting a systems-based perspective can change how students recognize systemic interdependence, exemplified by the relationships among inflammation, nutrition, and oral frailty [24,25,27,28,40,43].
Techniques such as mind mapping and concept mapping were shown to improve information retrieval and synthesis [59,60]. Incorporating these strategies into teaching encourages learners to analyse complex geriatric cases and build a longitudinal understanding across time and systems. This promotes deeper learning aligned with spiral curriculum models and competence-based progression.
4.1.2. Mid-to-High Bloom’s Levels (Analyse–Evaluate): Enhancing Clinical Reasoning and Reflective Capacity
As students move beyond foundational knowledge, they must develop analytic and metacognitive competencies to navigate the complexities of caring for older adults in the real world.
3. Reflective Practice with Traditional Teaching
Reflective education improves ethical reasoning and emotional intelligence, especially in the morally complex field of ageing care. Clinical diaries, debriefings, and reflections on patient interactions foster metacognitive awareness [31,43]. Reflective frameworks or structured portfolios help students analyse their values, assumptions, and emotional responses [61], strengthening their capacity to handle end-of-life discussions and cognitive impairments compassionately.
4. Improving Analytical Reasoning Across Fields
Clinical complexity in geriatrics often covers functional, diagnostic, and social aspects. Building analytical reasoning skills, therefore, requires exposure to multi-domain thinking. Matrix reasoning tasks and simulations involving layered geriatric conditions (e.g., comorbidities, cognitive decline, financial barriers) help students combine diverse data into clear treatment plans [21,37,40,45,46,47]. Research in AI-supported decision tools and multi-domain outcome integration confirms that training in high-dimensional reasoning enhances patient-specific treatment results [62,63].
5. Embedding Evidence-Based Teaching
Teaching students how to navigate geriatric literature—often complicated by confounding comorbidities—is essential. Critical appraisal tools and structured evidence-based modules promote analytic literacy [29,30,38,49]. Studies showed that incorporating Evidence-Based Practice (EBP) instruction into clinical rotations, primarily through cases involving frailty or prosthetic failure, greatly improves decision-making skills [64,65].
6. Home Care Delivery and Community Rotations
Traditional dental education is mainly clinic-based. However, older adults often need care at home or in long-term care settings. Training students in home care models and offering rotations in residential facilities prepares them for different care environments [47,52]. These settings promote team-based care and help students identify environmental, social, and cognitive barriers [66,67].
7. Evaluation-Driven Learning and Competence Assurance
A key theme in this review is the move toward evaluation-driven learning, which promotes competence-based, student-centred education. Assessment tools like Objective Structured Clinical Examinations (OSCE) [68] offer structured, standardised ways to evaluate students’ decision-making and clinical reasoning skills [48,49,50,51,53]. Moreover, the Subjective–Objective–Assessment–Plan (SOAP) framework enhances clinical documentation and facilitates patient care tracking [69]. The “Subjective” part records the patient’s reported symptoms and medical history; the “Objective” section notes measurable clinical findings and observable data; the “Assessment” combines this information to develop a diagnosis and treatment plan; and the “Plan” details treatment options, maintenance strategies, long-term outlook, and future care steps. Excellent SOAP documentation practices focus on clarity, timeliness, concise language, and avoiding subjective or irrelevant information.
Curricular innovations increasingly encourage students to evaluate health policies, reflect on interprofessional dynamics, and develop comprehensive care strategies. These assessment practices promote accountability and ensure learners acquire essential skills aligned with the demands of geriatric prosthodontics. Competence-based education relies on strong assessment methods. In addition to OSCE and SOAP notes, Entrustable Professional Activities (EPAs), adapted from nursing education, confirm that students demonstrate independence in key geriatric tasks before progressing [70,71]. These tools provide consistent, repeatable frameworks for evaluating critical thinking, communication, clinical judgment, and adaptability in real-world care environments.
8. The 4Ms Framework for Holistic Geriatric Assessment
The 4Ms—What Matters, Medication, Mentation, and Mobility—serve as a foundation for students in holistic geriatric care. This framework guides clinicians to align treatment with older adults’ goals, abilities, and values [52,72]. Dental educators should integrate the 4Ms into clinical assessments and treatment-planning exercises, ensuring each plan considers the patient’s overall health and priorities [73,74]. Using the 4Ms promotes both interprofessional teamwork and value-based care.
9. Simulation-Based Methods for Geriatric Competence
Simulation is a powerful tool for training in complex scenarios such as those involving dementia, caregiver dynamics, and palliative decisions. However, its use in prosthodontics remains limited. Emerging technologies like haptics, VR simulations, and standardised patient encounters should be incorporated into both formative and summative assessments [39,56]. Research has shown that simulation improves technical skills and interpersonal judgment [53,75,76,77].
In preclinical stages, simulation helps identify struggling students early and offers targeted remediation. In advanced stages, it assesses readiness for real-world clinical encounters [78,79]. Longitudinal virtual cases and risk-focused simulations (e.g., fall prevention, dysphagia management) could prepare learners for uncertainty and variability in ageing populations [80,81,82,83].
4.1.3. Highest Bloom’s Level (Create): Fostering Innovation and Humanistic Leadership
10. Soft Skills Integration for Leadership in Ageing Care
The Create domain is often overlooked in dental curricula, yet it is essential for preparing students to lead and advocate. Soft skills—empathy, adaptability, negotiation, and resilience—are not just supplementary but fundamental to ethical and effective prosthodontics [22,31,50,51,56]. Students should be encouraged to co-develop community outreach initiatives, participate in policy advocacy, and collaborate on research with older adults [84,85,86,87].
Humanistic leadership should be integrated from the beginning and continuously reinforced through opportunities that empower students to act as agents of change. Reflection, mentorship, and service-learning promote these qualities and help view dental professionals as clinicians and public health contributors in ageing societies.
Viewed through Bloom’s lens, geriatric prosthodontic education currently emphasizes mid-level competencies such as application and evaluation. While these are essential for effective clinical practice, overlooking foundational knowledge and creative innovation risks producing capable clinicians but not truly innovative visionaries.
The ten strategic guidelines provide a structured, evidence-based roadmap for reallocating cognitive focus across the taxonomy. From core biological concepts and reflective analysis to simulation-based mastery and leadership development, each step equips students for the diverse challenges of ageing care. Reform must be iterative, deliberate, and rooted in the real-world complexities of older adults—only then can dental education genuinely serve an ageing population.
4.2. Limitations of the Present Scoping Review
Despite its rigorous methodology, this scoping review has limitations. The broad scope of geriatric prosthodontic education justified a scoping approach, but future research should consider systematic reviews or meta-analyses to evaluate specific teaching methods and educational technologies. The field’s interdisciplinary nature—covering geriatrics, prosthodontics, educational psychology, and technology—makes developing narrowly focused questions for systematic reviews difficult. Protocols for bias and quality assessment were not used, as the review aimed to map and synthesise educational guidelines, not to evaluate individual studies. Unlike systematic reviews focusing on rigour, this review prioritised conceptual relevance to capture diverse educational practices. Studies were selected based on relevance to current frameworks rather than publication date, reflecting the evolving pedagogical landscape from passive, didactic instruction to modern, learner-centred, technology-enhanced methods.
The absence of a standardised framework in geriatric dental education has led to fragmented practices and inconsistent integration of essential competencies. This review aimed to identify existing gaps, propose strategic directions, and foster innovation, ultimately serving as both a foundation and a strategic tool for curriculum reform toward integrated, active, and competence-based learning. The latter curricular gaps stand in stark contrast to the recommendations of the Integrated Care for Older People (ICOPE): guidance for person-centred assessment and pathways in primary care, which advocates for educational models that are holistic, person-centred, and rooted in evidence-based gerontological competencies [88,89]. Competence-based dental education emphasises integrated knowledge and skills, promoting holistic clinical practice. This approach moves beyond isolated, competencies-focused models and supports the development of fully competent practitioners capable of providing comprehensive, person-centred care [90].
Therefore, despite acknowledging the limitations, the scoping review effectively utilises relevant literature data, offering a possibility to develop a competency framework for advancing better practices and transformative qualifications in geriatric oral health care.
Within this concept, Miller’s pyramid [91] serves as a framework for evaluating clinical competence in medical and health professions education, comprising four hierarchical levels that progress from knowledge to actual performance. The base, “knows,” signifies factual knowledge, while “knows how” indicates the ability to apply that knowledge in problem-solving situations. The “shows how” level assesses the demonstration of skills in controlled or simulated environments, such as Objective Structured Clinical Examinations (OSCE). At the top, “does” reflects genuine performance in real clinical practice. The model emphasises the importance of progressing from knowledge and simulation-based assessments to measuring real-world workplace competence.
The proposed 10 guidelines could be utilised for developing comprehensive methods such as rubrics and rotational student self-evaluation exercises in clinical university settings to assess and promote skills, critical thinking, and overall better comprehensive clinical training.
The outcomes of studies also identified the role that developing and implementing relevant curricula, clinical training, and educational strategies play in enhancing geriatric education by satisfying the learning needs of current and future health professionals. By aligning the PRISMA 2020 extension with Bloom’s Taxonomy, this study introduces a novel framework for organising the literature review, enabling a structured, stepwise progression from foundational knowledge to contemporary pedagogical strategies.
International cooperation for curricula standardisation, student mobility, and quality assurance is one of the global factors that shape educational reform. These factors often lead to a wide range of initiatives that may benefit from the same frameworks, such as those involving standardising degree structures or forms of recognition and credit transfer.
Demographic changes such as ageing populations and declining birth rates present challenges in designing education and workforce preparation programs. In countries with publicly funded and centrally managed educational systems, the capability for administrative efficiency favours the occurrence of far-reaching reforms. Many of these reforms are grounded in academic literature and seek to espouse the ethos of lifelong learning. Evidence-informed policy and governance structures aim to harmonise higher education standards, aligning with demographic pressures on employability, mobility, and the narrowing of skills, as part of a comprehensive reform agenda [92].
5. Conclusions
The reviewed evidence revealed the necessity of transforming dental education to meet the demands of the 21st century. Curricula that previously relied on passive content delivery were found to be insufficient for preparing professionals to address the complex needs of ageing populations. Educational strategies increasingly emphasise integration, critical thinking, simulation, interprofessional collaboration, and technological competence. (1) Gaps in undergraduate and postgraduate training were identified, particularly in integrating biological, psychological, and social aspects of ageing within geriatric prosthodontics. (2) Evidence-based instructional methods—such as Case-Based Learning, Problem-Based Learning, simulation-based training, and interprofessional education—have been shown to enhance higher-order thinking, clinical reasoning, and decision-making. (3) Using standardised assessment tools, including OSCE and reflective models, effectively supported the development of clinical competence and lifelong learning. (4) Aligning cognitive levels from basic recall to innovation led to ten evidence-based, adaptable educational guidelines that are pedagogically sound and empirically supported. These findings collectively validate a comprehensive, forward-looking framework aimed at realigning dental education with changing public health priorities and the realities of a globally ageing population.
6. Future Directions for Implementation
Future studies should evaluate longitudinal outcomes of integrated geriatric dental curricula, including educational and clinical competencies in ageing care. Research should examine simulation-based learning, interprofessional education, and digital tools like VR and AI for student preparedness. Further work is needed on the impact of competence-based training on health outcomes in older adults, especially in managing oral-systemic diseases. Studies should also identify barriers to curriculum reform globally and develop scalable models for resource-limited settings. Emphasis should be placed on creating inclusive, adaptable, and culturally sensitive approaches to geriatric prosthodontic education.
To enhance the practical application of this review, a comprehensive and fully integrated curriculum in geriatric prosthodontic education is essential from the outset. Reforms must move beyond incremental or fragmented efforts, which lack coherence and fail to ensure sustained competence. A unified approach should concurrently address faculty development, curriculum alignment with educational frameworks such as Bloom’s Taxonomy, incorporating structured assessments (e.g., OSCE), and integrating interdisciplinary models like the 4Ms framework.
This should be embedded within a spiral, competence-based curriculum aligned with accreditation standards and public health priorities. Partial implementations are insufficient; only a cohesive, system-wide model can adequately prepare graduates for the complexities of ageing populations. Institutional collaboration with regulatory and healthcare bodies will be vital to achieving sustainable, high-quality geriatric dental education.
Author Contributions
Conceptualization, P.C. and V.A.; methodology, P.C. and V.A.; software, P.C. and L.C.P.; validation, P.C., L.C.P. and V.A.; formal analysis, P.C. and V.A.; investigation, P.C. and L.C.P.; resources, P.C. and L.C.P.; data curation, P.C. and L.C.P.; writing—original draft preparation, P.C. and O.N.; writing—review and editing, P.C., V.A. and O.N.; visualization, P.C. and V.A.; supervision, V.A. and O.N.; project administration, V.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on request.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript in alphabetical order:
| AETCOM | Attitude, Ethics, and Communication |
| ADEE | Association for Dental Education in Europe |
| AI | Artificial Intelligence |
| CBL | Case-Based Learning |
| CDPC | Clinical Dentist–Patient Communication |
| COST | Cooperation in Science and Technology |
| DentCPD | Dental Continuing Professional Development. |
| Delhi-NCR | Delhi–National Capital Region. |
| EBTA | Evidence-Based Teaching Approach |
| EBP | Evidence-Based Practice |
| ECG | European College of Gerodontology |
| EPAs | Entrustable Professional Activities |
| FDR | False Discovery Rate |
| HPE | Health Professional Education |
| ICC | Impaired Chewing Capacity |
| ICOPE | Integrated Care for Older People (ICOPE) |
| IPE | Interprofessional Education |
| NCDs | Non-Communicable Diseases |
| OHAT | Oral Health Assessment Tool |
| OSCE | Objective Structured Clinical Examination |
| PBL | Problem-Based Learning |
| PICO | Population, Intervention, Comparison, and Outcome |
| PRISMA | Preferred Reporting Items for Systematic reviews and Meta-Analyses |
| PROGRAMMING | PROmoting GeRiAtric Medicine |
| SIT | Session Integration Tool |
| SOAP | Subjective Objective Assessment Plan |
| TBL | Team-Based Learning |
| TOC | Total Occlusal Convergence |
| VR-haptic preclinical tool | Virtual Reality Haptic Tool |
| WHO | World Health Organization |
| 4Ms | What Matters, Medications, Mentation, Mobility |
References
- Anastasiadou, V.; Naka, O.; Pantelidou-Papadopoulou, O.; Sakellari, D.; Topitsoglou, V.; Tortopidis, D. Management of Complex Conditions in the Context of Geriatric Dentistry, 1st ed.; Hellenic Academic Libraries Link (HEAL-Link): Zografou, Greece, 2020; pp. 18–23. ISBN 978-960-603-244-8.
- Huang, X.; Kang, L.; Bi, J. Epidemiology of oral health in older adults aged 65 or over: Prevalence, risk factors and prevention. Aging Clin. Exp. Res. 2025, 37, 193. [Google Scholar] [CrossRef]
- World Health Organization. Integration of Oral Health Into Universal Healthcare; WHO Technical Report Series; WHO: Geneva, Switzerland, 2024; p. 1024.
- Petersen, P.E.; Yamamoto, T. Improving the oral health of aging populations. Int. Dent. J. 2005, 55, 253–257. [Google Scholar] [CrossRef]
- Petersen, P.E.; Baehni, P.C.; Ogawa, H. Train-the-Trainer programs for nursing home staff. Community Dent. Oral Epidemiol. 2023, 51, 145–152. [Google Scholar]
- Yamamoto-Kuramoto, T.; Aida, J.; Kondo, K. Tooth loss and functional disability in elderly. J. Am. Geriatr. Soc. 2023, 71, 1123–1131. [Google Scholar] [CrossRef]
- Guiglia, R.; Musciotto, A.; Compilato, D.; Procaccini, M.; Lo Russo, L.; Ciavarella, D.; Lo Muzio, L.; Cannone, V.; Pepe, I.; D’Angelo, M.; et al. Aging and oral health: Effects in hard and soft tissues. Curr. Pharm. Des. 2010, 16, 619–630. [Google Scholar] [CrossRef]
- Wolff, A.; Joshi, R.K.; Ekström, J.; Aframian, D.; Pedersen, A.M.; Proctor, G.; Narayana, N.; Villa, A.; Sia, Y.W.; Aliko, A.; et al. A Guide to Medications Inducing Salivary Gland Dysfunction, Xerostomia, and Subjective Sialorrhea: A Systematic Review Sponsored by the World Workshop on Oral Medicine VI. Drugs RD 2017, 17, 1–28. [Google Scholar] [CrossRef]
- Sarafidou, K.; Baechle, M.; Ferrucci, L. Oral microbiome changes in aging. J. Dent. Res. 2024, 103, 45–52. [Google Scholar]
- Zelig, R.; Goldstein, S.; Touger-Decker, R.; Firestone, E.; Golden, A.; Johnson, Z.; Kaseta, A.; Sackey, J.; Tomesko, J.; Parrott, J.S. Tooth Loss and Nutritional Status in Older Adults: A Systematic Review and Meta-analysis. JDR Clin. Transl. Res. 2022, 7, 4–15. [Google Scholar] [CrossRef] [PubMed]
- Du, M.; Deng, K.; Yin, J.; Wu, C.; Hu, S.; Guo, L.; Luo, Z.; Tonetti, M.; Tjakkes, G.E.; Visser, A.; et al. Association Between Chewing Capacity and Mortality Risk: The Role of Diet and Ageing. J. Clin. Periodontol. 2025, 52, 695–706. [Google Scholar] [CrossRef]
- van der Putten, G.J.; de Baat, C.; De Visschere, L.; Schols, J. Poor oral health, a potential new geriatric syndrome. Gerodontology 2014, 31 (Suppl. S1), 17–24. [Google Scholar] [CrossRef]
- Field, J.; Vital, S.; Dixon, J.; Murphy, D.; Davies, J. The Graduating European Dentist Curriculum Framework: A 7-Year Review. Eur. J. Dent. Educ. Off. J. Assoc. Dent. Educ. Eur. 2025, 29, 155–161. [Google Scholar] [CrossRef]
- Kossioni, A.; McKenna, G.; Müller, F. European College of Gerodontology undergraduate curriculum guidelines. Eur. J. Dent. Educ. 2017, 21, 3–9. [Google Scholar] [CrossRef]
- Kossioni, A.E.; Hajto-Bryk, J.; Maggi, S.; McKenna, G.; Petrovic, M.; Roller-Wirnsberger, R.E.; Schimmel, M.; Tamulaitienè, M.; Vanobbergen, J.; Müller, F. An Expert Opinion from the European College of Gerodontology and the European Geriatric Medicine Society: European Policy Recommendations on Oral Health in Older Adults. J. Am. Geriatr. Soc. 2018, 66, 609–613. [Google Scholar] [CrossRef] [PubMed]
- Kossioni, A.; Vanobbergen, J.; Newton, J.P. Gerodontology education in European dental schools. Eur. J. Dent. Educ. 2018, 22, e1–e6. [Google Scholar] [CrossRef]
- Lamprecht, R.; Smith, J.; Wilson, M. Global oral health trends in aging populations. Community Dent. Oral Epidemiol. 2020, 48, 215–223. [Google Scholar] [CrossRef]
- Lamprecht, R.; Guse, J.; Schimmel, M.; Müller, F.; Heydecke, G.; Reissmann, D.R. Benefits of combined quantitative and qualitative evaluation of learning experience in a gerodontology course for dental students. BMC Med. Educ. 2020, 20, 281. [Google Scholar] [CrossRef]
- Xavier, I.; Ettinger, R.L.; Proença, L.; Botelho, J.; Machado, V.; Rua, J.; Delgado, A.S.; Mendes, J.J. Geriatric Dentistry Curriculum in Six Continents. Int. J. Environ. Res. Public Health 2020, 17, 4682. [Google Scholar] [CrossRef]
- Arany, P.; Kossioni, A.; Müller, F. Implementing the 4Ms framework in geriatric dental practice. J. Dent. Educ. 2024, 88, 602–610. [Google Scholar]
- Parikh, N.; Risinger, D.; Holland, J.N.; Molony, D.A.; van der Hoeven, D. Evaluating dental students’ perspectives on the concurrent teaching of didactic and case-based courses. J. Dent. Educ. 2022, 86, 1643–1652. [Google Scholar] [CrossRef] [PubMed]
- Arruzza, E.; Chau, M. A scoping review of randomised controlled trials to assess the value of gamification in the higher education of health science students. J. Med. Imaging Radiat. Sci. 2021, 52, 137–146. [Google Scholar] [CrossRef]
- Dalaya, M.; Ishaquddin, S.; Ghadage, M.; Hatte, G. An interesting review on soft skills and dental practice. J. Clin. Diagn. Res. JCDR 2015, 9, ZE19–ZE21. [Google Scholar] [CrossRef]
- Beattie, V.; Collins, B.; McInnes, B. Deep and surface learning: A simple or simplistic dichotomy? Account. Educ. 1997, 6, 1–12. [Google Scholar] [CrossRef]
- Marton, F.; Säljö, R. On qualitative differences in learning: I—Outcome and process. Br. J. Educ. Psychol. 1976, 46, 4–11. [Google Scholar] [CrossRef]
- Strandell, C.H. Nursing Faculty Perceptions of an Integrated Curriculum and Implementation of the Curriculum. Degree Doctor of Philosophy Field of Education. Ph.D. Thesis, Northwestern University, Evanston, IL, USA, 1980. [Google Scholar]
- Maharjan, B.; Bhandary, S.; Upadhyay, S.; Ghimire, S.; Shrestha, I.; Joshi, M.; Vaidya, S.; Pradhan, P. Developing tool and measuring integration characteristics of basic science curriculum to improve curriculum integration. Kathmandu Univ. Med. J. 2018, 64, 338–344. Available online: https://www.researchgate.net/publication/333162902 (accessed on 28 August 2025).
- Lajber, M.; Mahboob, U.; Lajber, F.; Khan, M.; Waseem Badshah Bukhari, S. Student’s perception regarding an integrated curriculum at a public sector medical college. PJMHS 2020, 14, 1196–1199. Available online: https://pjmhsonline.com/2020/july-sep/1196.pdf (accessed on 28 August 2025).
- Morton, D.A.; Colbert-Getz, J.M. Measuring the impact of the flipped anatomy classroom: The importance of categorizing an assessment by Bloom’s taxonomy. Anat. Sci. Educ. 2017, 10, 170–175. [Google Scholar] [CrossRef]
- Bansal, S.; Bansal, M.; White, S. Association Between Learning Approaches and Medical Student Academic Progression During Preclinical Training. Adv. Med. Educ. Pract. 2021, 12, 1343–1351. [Google Scholar] [CrossRef]
- Estrela, C.; Oshita, M.G.B.; Perazzo, M.F.; Alencar, A.H.G.; Silva, J.A.; Estrela, L.R.; Cintra, L.T.; Estrela, C.R. Quality of Communication Between Professors and University Students in the Process of Learning. Braz. Dent. J. 2024, 35, e246081. [Google Scholar] [CrossRef]
- Chalmers, J.M.; Carter, K.D.; Spencer, A.J. Oral health assessment tools for elderly patients. Spec. Care Dent. 2002, 22, 11–20. [Google Scholar] [CrossRef]
- Prat-Sala, M.; Redford, P. The interplay between motivation, self-efficacy, and approaches to studying. Br. J. Educ. Psychol. 2010, 80, 283–305. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, P.K. Retrieval practice & Bloom’s taxonomy: Do students need fact knowledge before higher order learning? J. Educ. Psychol. 2019, 111, 189–209. [Google Scholar] [CrossRef]
- Miller, C.J.; Metz, M.J. Can clinical scenario videos improve dental students’ perceptions of the basic sciences and ability to apply content knowledge? J. Dent. Educ. 2015, 79, 1452–1460. [Google Scholar] [CrossRef]
- Hobbins, J.O.; Murrant, C.L.; Snook, L.A.; Tishinsky, J.M.; Ritchie, K.L. Incorporating higher order thinking and deep learning in a large, lecture-based human physiology course: Can we do it? Adv. Physiol. Educ. 2020, 44, 637–644. [Google Scholar] [CrossRef]
- Lin, C.S.; Yang, C.C. Evaluation of a digital game for teaching behavioral aspects of clinical communication in dentistry. BMC Med. Educ. 2023, 23, 78. [Google Scholar] [CrossRef]
- Tebcherany, H.; Khocht, A. An evidence-based teaching approach enhances student learning of periodontal disease pathogenesis. J. Dent. Educ. 2024, 88, 304–313. [Google Scholar] [CrossRef]
- Bencharit, S.; Quinn, B.; Sittoni-Pino, M.F.; Arias-Herrera, S.; Schick, S.G.; Rampf, S.; Byrne, S.; Shazib, M.A.; Örtengren, U.; Lam, W.Y.H.; et al. Insights from the global education survey on the use of VR-haptics in dental education. Front. Dent. Med. 2025, 6, 1576646. [Google Scholar] [CrossRef]
- Kerosuo, E.; Ruotoistenmäki, J.; Murtomaa, H. Report on the development of a new dental curriculum at Helsinki. Eur. J. Dent. Educ. 2001, 5, 23–30. [Google Scholar] [CrossRef]
- Crowe, A.; Dirks, C.; Wenderoth, M.P. Biology in bloom: Implementing Bloom’s Taxonomy to enhance student learning in biology. CBE Life Sci. Educ. 2008, 7, 368–381. [Google Scholar] [CrossRef] [PubMed]
- Kingsley, K.; O’Malley, S.; Stewart, T.; Howard, K.M. Research enrichment: Evaluation of structured research in the curriculum for dental medicine students as part of the vertical and horizontal integration of biomedical training and discovery. BMC Med. Educ. 2008, 8, 9. [Google Scholar] [CrossRef]
- Chambers, D.W. Lessons from students in a critical thinking course: A case for the third pedagogy. J. Dent. Educ. 2009, 73, 65–82. [Google Scholar] [CrossRef] [PubMed]
- Rougas, S.; Berry, A.; Bierer, S.B.; Blanchard, R.D.; Cianciolo, A.T.; Colbert-Getz, J.M.; Han, H.; Lipner, K.; Teal, C.R. Applying Conceptual and Theoretical Frameworks to Health Professions Education Research: An Introductory Workshop. MedEdPORTAL J. Teach. Learn. Resour. 2022, 18, 11286. [Google Scholar] [CrossRef] [PubMed]
- Manchery, N.; Henry, J.D.; Lam, B.C.P.; Kochan, N.A.; Deutsch, A.; Brodaty, H.; S Sachdev, P.; Nangle, M.R. Memory decline in older individuals predicts an objective indicator of oral health: Findings from the Sydney Memory and Ageing Study. BMC Oral Health 2022, 22, 93. [Google Scholar] [CrossRef] [PubMed]
- Nagatani, M.; Tanaka, T.; Son, B.K.; Kawamura, J.; Tagomori, J.; Hirano, H.; Shirobe, M.; Iijima, K. Oral frailty as a risk factor for mild cognitive impairment in community-dwelling older adults: Kashiwa study. Exp. Gerontol. 2023, 172, 112075. [Google Scholar] [CrossRef]
- Allenspach, P.; Srinivasan, M. Oral health status of institutionalized older adults receiving domiciliary dental care: A cross-sectional retrospective study. Spec. Care Dent. 2024, 44, 1444–1455. [Google Scholar] [CrossRef]
- Anderson, L.; Krathwohl, D.; Bloom, B. A Taxonomy for Learning, Teaching, and Assessing: A Revision of Bloom’s Taxonomy of Educational Objectives. 2000. Available online: http://lst-iiep.iiep-unesco.org/cgi-bin/wwwi32.exe/[in=epidoc1.in]/?t2000=015556/(100) (accessed on 28 August 2025).
- Al Khalaf, K.; Moore, C.; McKenna, G.; Da Mata, C.; Lynch, C.D. Undergraduate teaching and assessment methods in prosthodontics curriculum: An international Delphi survey. J. Dent. 2022, 123, 104207. [Google Scholar] [CrossRef]
- Nayak, V.; Nayak, K.R.; Goyal, S.; Jain, S.; Prabhath, S.; Palimar, V.; Komattil, R. Tangible impact of patient communication modules on medical students and interns. Adv. Physiol. Educ. 2024, 48, 40–48. [Google Scholar] [CrossRef]
- Singh, S.; Gupta, R.; Gill, S.; Naaz, Z.; Longdo, M.; Pathak, A.; Kusuma, J. Perception and Attitude of Dental Students Towards Geriatric Care: A Questionnaire-Based Survey. Cureus 2024, 16, e67297. [Google Scholar] [CrossRef]
- Arany, S.; Cavalcanti, L.; Phildor, D.; Watson, G.E.; Kopycka-Kedzierawski, D.T.; Eliav, E.; Medina-Walpole, A.; Caprio, T. Implementation of a 4Ms approach in age-friendly oral health care at an Academic Specialty Care Dental Clinic. J. Am. Geriatr. Soc. 2024, 72 (Suppl. S3), S68–S75. [Google Scholar] [CrossRef] [PubMed]
- Hadjichristou, C.; Kokoti, M.; Bakopoulou, A. Haptics in fixed prosthodontics and their role in dental education: A literature review. J. Dent. Educ. 2024, 88, 1020–1028. [Google Scholar] [CrossRef]
- Thompson, A.R.; O’Loughlin, V.D. The Blooming Anatomy Tool (BAT): A discipline-specific rubric for utilizing Bloom’s taxonomy in the design and evaluation of assessments in the anatomical sciences. Anat. Sci. Educ. 2015, 8, 493–501. [Google Scholar] [CrossRef]
- Heck, A.J.; Chase, A.J. A Tool for Evaluating Session-Level Integration in Medical Education. Med. Sci. Educ. 2021, 31, 647–654. [Google Scholar] [CrossRef]
- Bock, A.; Wagenknecht, N.; Winnand, P.; Katz, M.S.; Ooms, M.; Heitzer, M.; Hölzle, F.; Modabber, A. Improvement of students’ communication skills through targeted training and the use of simulated patients in dental education-a prospective cohort study. BMC Med. Educ. 2024, 24, 820. [Google Scholar] [CrossRef] [PubMed]
- Tambunan, E.H. Theory-Practice Gap During Clinical Learning: A Descriptive Qualitative Study of Nursing Students’ Experiences and Perceptions. J. Caring Sci. 2024, 13, 74–81. [Google Scholar] [CrossRef]
- Mercan, N.; Mersin, S. Evaluating the therapeutic communication skills of nursing students in the clinical setting: The experiences of students, patients and patients’ relatives. Heliyon 2025, 11, e41677. [Google Scholar] [CrossRef]
- Jabade, M.; Nadaf, H. Assessing the efficacy of mind mapping as a learning technique to enhance information retrieval in nursing students. J. Educ. Health Promot. 2024, 13, 371. [Google Scholar] [CrossRef]
- Shanmugarajah, M.M.; Mondal, H.; Das, T. From Fragmented Facts to Unified Knowledge: Exploring Concept Mapping in Neuromuscular Physiology Among First-Year Medical Students. Cureus 2024, 16, e74711. [Google Scholar] [CrossRef] [PubMed]
- Machost, H.; Stains, M. Reflective Practices in Education: A Primer for Practitioners. CBE Life Sci. Educ. 2023, 22, es2. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Zeng, D.; Xu, T.; Wang, Y. Representation Learning for Integrating Multi-domain Outcomes to Optimize Individualized Treatments. Adv. Neural Inf. Process. Syst. 2020, 33, 17976–17986. [Google Scholar]
- Chen, Y.; Zeng, D.; Wang, Y. Optimizing personalized treatments for targeted patient populations across multiple domains. Int. J. Biostat. 2024, 20, 437–453. [Google Scholar] [CrossRef]
- Dusin, J.; Melanson, A.; Mische-Lawson, L. Evidence-based practice models and frameworks in the healthcare setting: A scoping review. BMJ Open 2023, 13, e071188. [Google Scholar] [CrossRef]
- Haavisto, E.; Siltanen, H.; Tolvanen, A.; Holopainen, A. Instruments for assessing healthcare professionals’ knowledge and skills of evidence-based practice: A scoping review. J. Clin. Nurs. 2023, 32, 4391–4407. [Google Scholar] [CrossRef] [PubMed]
- Denecke, K.; Kushniruk, A.W.; Borycki, E.M. A Comprehensive Framework for Hospital@Home Care Models. Stud. Health Technol. Inform. 2024, 314, 27–31. [Google Scholar] [CrossRef] [PubMed]
- Health Quality Ontario Team. Based Models for End-of-Life Care: An Evidence-Based Analysis. Ont. Health Technol. Assess. Ser. 2014, 14, 1–49. [Google Scholar]
- Al-Hashimi, K.; Said, U.N.; Khan, T.N. Formative Objective Structured Clinical Examinations (OSCEs) as an Assessment Tool in UK Undergraduate Medical Education: A Review of Its Utility. Cureus 2023, 15, e38519. [Google Scholar] [CrossRef] [PubMed]
- Podder, V.; Lew, V.; Ghassemzadeh, S. SOAP Notes. [Updated 28 August 2023]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: https://www.ncbi.nlm.nih.gov/books/NBK482263/ (accessed on 28 August 2025).
- Al-Moteri, M. Entrustable professional activities in nursing: A concept analysis. Int. J. Nurs. Sci. 2020, 7, 277–284. [Google Scholar] [CrossRef]
- Alexander, N.; Maaz, A.; Peters, H.; Kottner, J. Entrustable professional activities in nursing education: A scoping review protocol. BMJ Open 2022, 12, e061451. [Google Scholar] [CrossRef]
- Emery-Tiburcio, E.E.; Mack, L.; Zonsius, M.C.; Carbonell, E.; Newman, M. The 4Ms of an Age-Friendly Health System An evidence-based framework to ensure older adults receive the highest quality care. Home Healthc. Now 2022, 40, 252–257. [Google Scholar] [CrossRef]
- Carbonell, E.; Zonsius, M.C.; Rodriguez-Morales, G.; Newman, M.; Emery-Tiburcio, E.E. Addressing What Matters Aligning care with the priorities of older adults and their caregivers. Home Healthc. Now 2022, 40, 258–263. [Google Scholar] [CrossRef]
- Thombley, R.L.; Rogers, S.E.; Adler-Milstein, J. Developing electronic health record-based measures of the 4Ms to support implementation and evidence generation for Age-Friendly Health Systems. J. Am. Geriatr. Society. 2023. Advance online publication. [Google Scholar] [CrossRef]
- Baxmann, M.; Baráth, Z.; Kárpáti, K. Efficacy of typodont and simulation training in orthodontic education: A systematic review. BMC Med. Educ. 2024, 24, 1443. [Google Scholar] [CrossRef]
- Higgins, D.; Hayes, M.; Taylor, J.; Wallace, J. A scoping review of simulation-based dental education. MedEdPublish 2020, 9, 36. [Google Scholar] [CrossRef]
- Manav, E.Y.; Akbiyik, S.Y.; Ceylan, A.B.; Çakiroğlu, A.E.Y.; Tuncer, D. Effects of virtual reality and layered tooth model training on manual dexterity in preclinical dental education. BMC Med. Educ. 2025, 25, 1020. [Google Scholar] [CrossRef] [PubMed]
- Pang, M.; Zhao, X.; Lu, D.; Dong, Y.; Jiang, L.; Li, J.; Ji, P. Preliminary User Evaluation of a New Dental Technology Virtual Simulation System: Development and Validation Study. JMIR Serious Games 2022, 10, e36079. [Google Scholar] [CrossRef] [PubMed]
- Kononowicz, A.A.; Woodham, L.A.; Edelbring, S.; Stathakarou, N.; Davies, D.; Saxena, N.; Tudor Car, L.; Carlstedt-Duke, J.; Car, J.; Zary, N. Virtual Patient Simulations in Health Professions Education: Systematic Review and Meta-Analysis by the Digital Health Education Collaboration. J. Med. Internet Res. 2019, 21, e14676. [Google Scholar] [CrossRef]
- Serrano, C.M.; Bakker, D.R.; Zamani, M.; de Boer, I.R.; Koopman, P.; Wesselink, P.R.; Berkhout, E.; Vervoorn, J.M. Virtual reality and haptics in dental education: Implementation progress and lessons learned after a decade. Eur. J. Dent. Educ. Off. J. Assoc. Dent. Educ. Eur. 2023, 27, 833–840. [Google Scholar] [CrossRef] [PubMed]
- Slaidina, A.; Ozolins, K.; Berzina, S.; Abeltins, A. Patient-specific virtual simulation in the clinical training for prosthetic dentistry. Eur. J. Dent. Educ. Off. J. Assoc. Dent. Educ. Eur. 2023. Advance online publication. [Google Scholar] [CrossRef]
- Patil, S.; Bhandi, S.; Awan, K.H.; Licari, F.W.; Di Blasio, M.; Ronsivalle, V.; Cicciù, M.; Minervini, G. Effectiveness of haptic feedback devices in preclinical training of dental students-a systematic review. BMC Oral Health 2023, 23, 739. [Google Scholar] [CrossRef]
- Tang, T.; Li, X.; Lin, Y.; Liu, C. Comparing digital real-time versus virtual simulation systems in dental education for preclinical tooth preparation of molars for metal-ceramic crowns. BMC Oral Health 2025, 25, 814. [Google Scholar] [CrossRef]
- Kodali, M.V.R.M.; Kodali, U.S.; Gadicherla, S.; Smriti, K.; Singh, A.; Khurshid, Z. The Role of Soft Skills in Dental Education: Challenges and Importance. Eur. J. Dent. 2025, 19, 851–859. [Google Scholar] [CrossRef]
- Carey, J.A.; Madill, A.; Manogue, M. Communications skills in dental education: A systematic research review. Eur. J. Dent. Educ. Off. J. Assoc. Dent. Educ. Eur. 2010, 14, 69–78. [Google Scholar] [CrossRef]
- Hanks, S.; Marples, C.; Wall, E. Reflections on learning and enhancing communication skills through community engagement: A student perspective. Br. Dent. J. 2016, 221, 81–85. [Google Scholar] [CrossRef]
- Jiménez, J.D.; Guillén-Guzmán, E.; Oliva, V.; Ballesteros-Urpi, A.; Pardo-Hernandez, H. Theoretical approaches to the engagement with patients in case-management programmes and assertive outreach teams: A systematic review of the literature. J. Psychiatr. Ment. Health Nurs. 2022, 29, 647–658. [Google Scholar] [CrossRef]
- Ogliari, G.; Masud, T.; Herghelegiu, A.M.; Pavic, T.; Wissendorff Ekdahl, A.; Piotrowicz, K.; Duque, S.; Benetos, A.; Bogdanovic, N.; Bonin-Guillaume, S.; et al. Collaborators of the PROGRAMMING survey on educational needs Educational Needs in Geriatric Medicine Among Health Care Professionals and Medical Students in COST Action 21122 PROGRAMMING: Mixed-Methods Survey Protocol. JMIR Res. Protoc. 2025, 14, e64985. [Google Scholar] [CrossRef] [PubMed]
- WHO. Integrated Care for Older People (ICOPE): Guidance for Person-Centred Assessment and Pathways in Primary Care, 2nd ed.; WHO: Geneva, Switzerland, 2025. Available online: https://www.who.int/publications/i/item/9789240103726 (accessed on 28 August 2025).
- Hasan, A. Competence-based dental education. Br. Dent. J. 2024, 236, 933. [Google Scholar] [CrossRef] [PubMed]
- Witheridge, A.; Ferns, G.; Scott-Smith, W. Revisiting Miller’s pyramid in medical education: The gap between traditional assessment and diagnostic reasoning. Int. J. Med. Educ. 2019, 10, 191–192. [Google Scholar] [CrossRef] [PubMed]
- Shams, F.; Huisman, J.; Hsieh, C.C.; Wilkins, S.; Adelman, C. The Bologna process and its impact in the European Higher Education Area and beyond. In SAGE Knowledge; SAGE: Newcastle upon Tyne, UK, 2012. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).