Brown Tumor in Jaw Associated with Hyperparathyroidism: A Case Report
Abstract
1. Introduction
2. Case Report
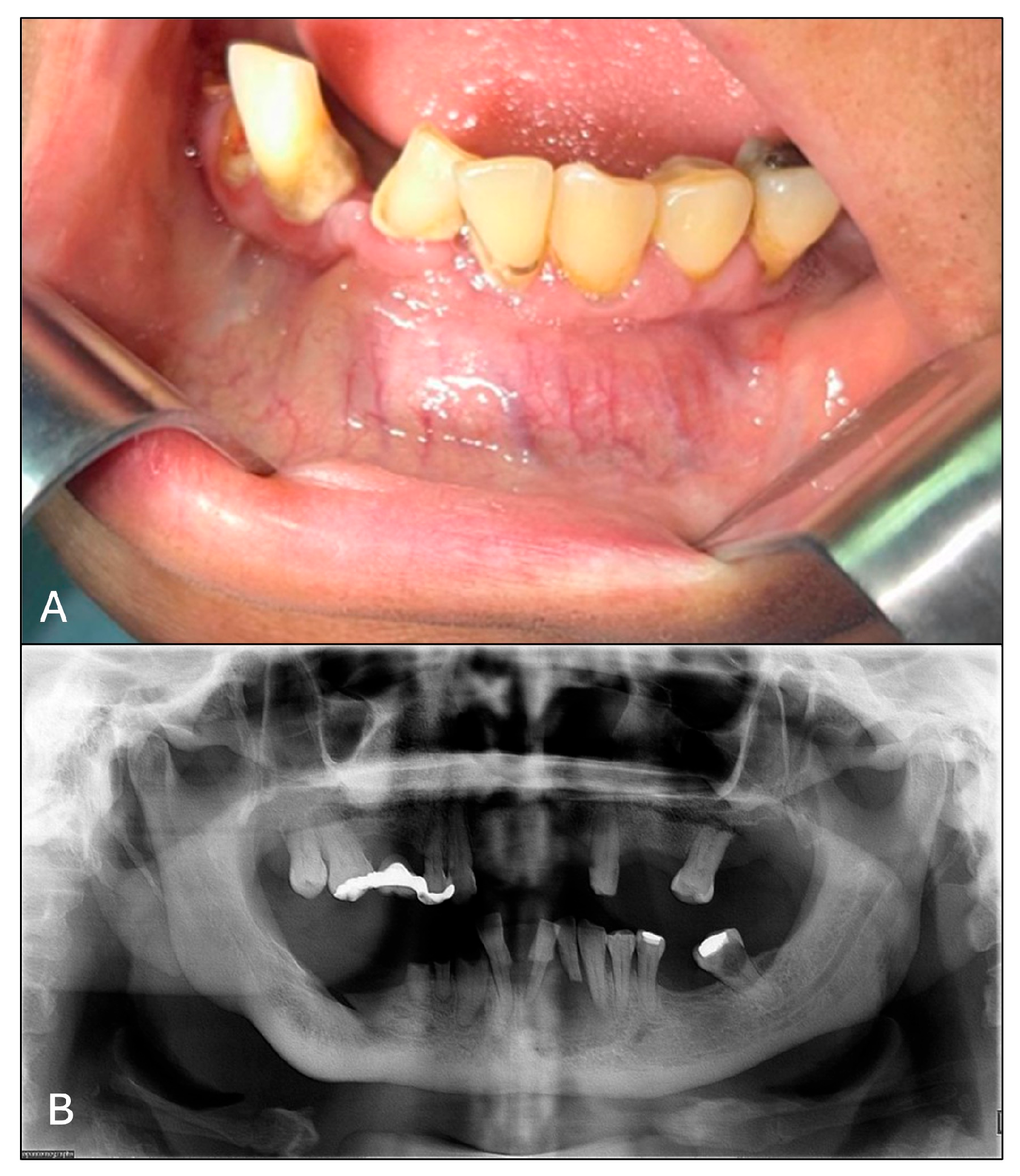
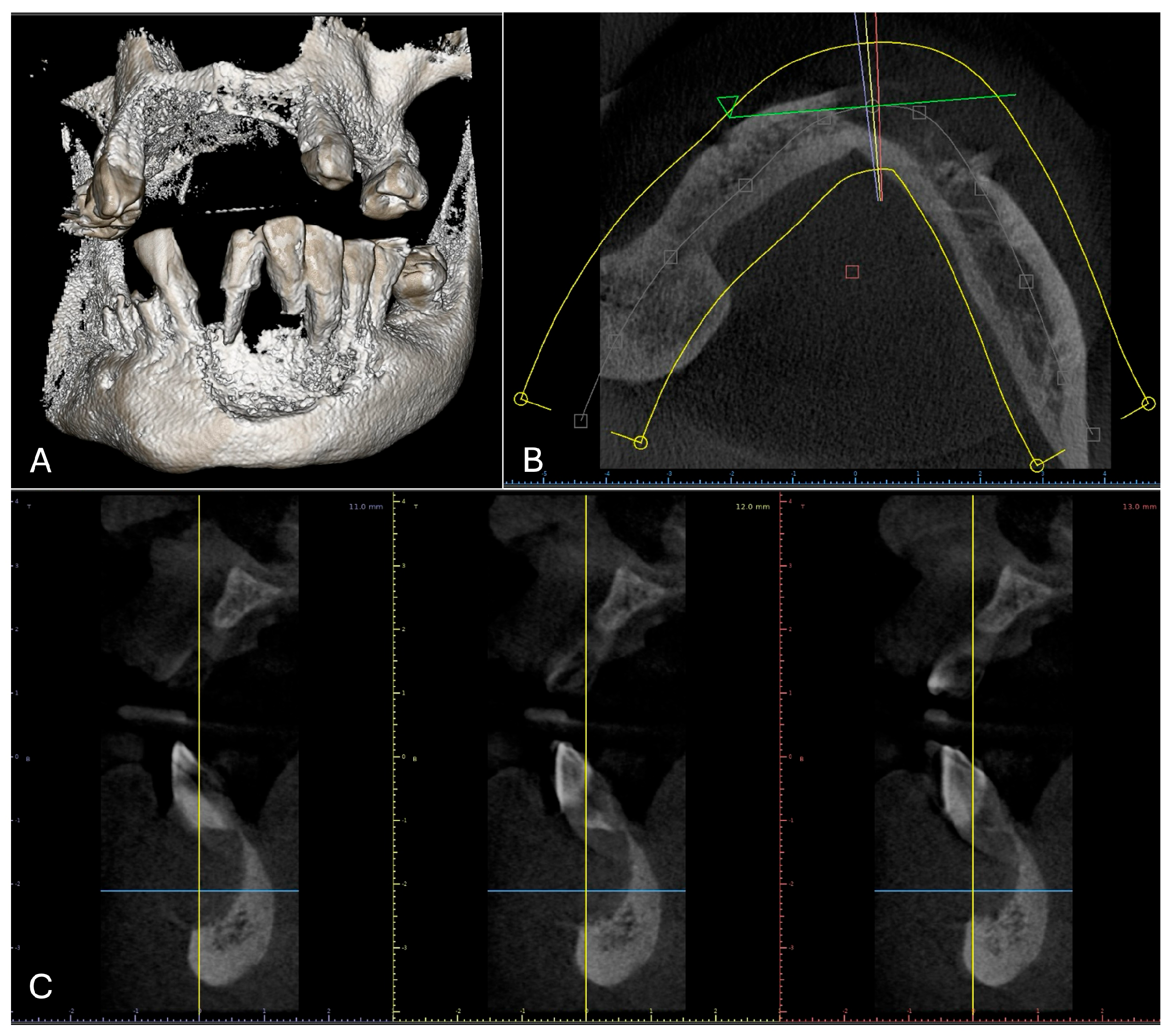
2.1. Examination
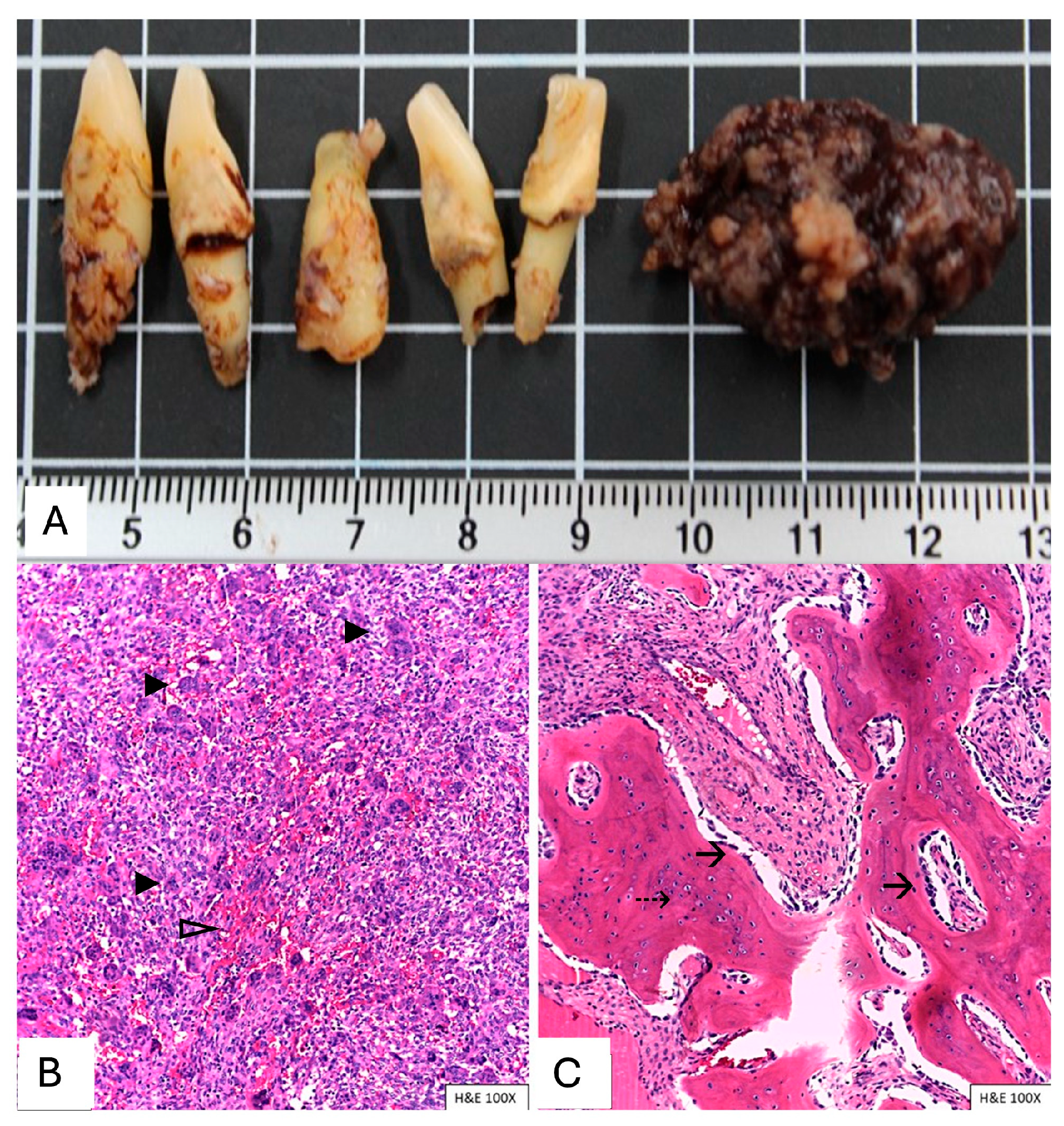
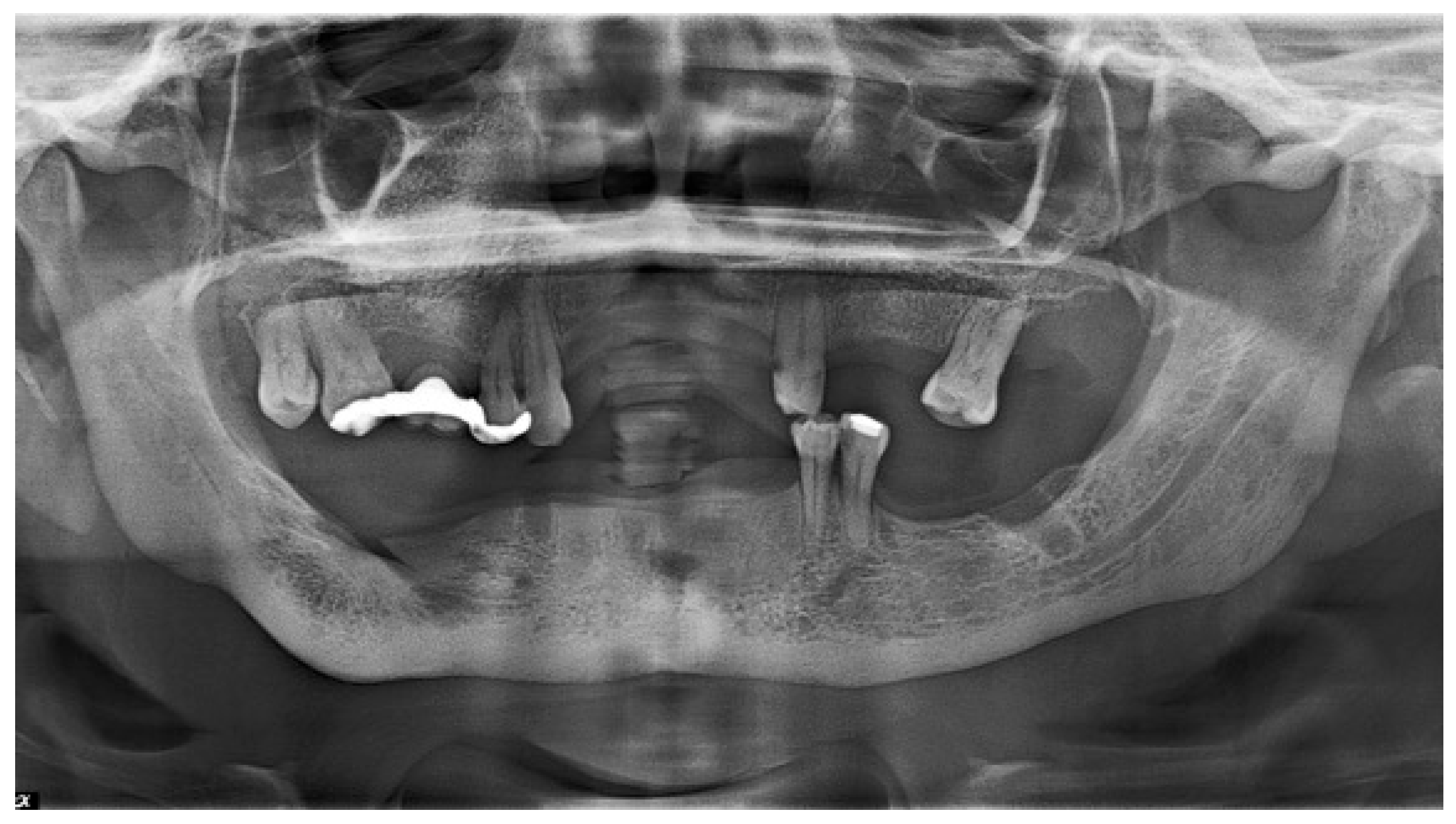
2.2. Treatment Procedures and Histopathological Results
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Shetty, A.D.; Namitha, J.; James, L. Brown tumor of mandible in association with primary hyperparathyroidism: A case report. J. Int. Oral Health 2015, 7, 50–52. [Google Scholar] [PubMed]
- Pham, M.; Bhatt, P.; Purvey, T.A. Massive Exophytic Brown’s Tumor of the Bilateral Maxilla with Mandibular Involvement. J. Craniofac. Surg. 2022, 33, 897–900. [Google Scholar] [CrossRef] [PubMed]
- Pati, A.R.; Mubeen, K.V.; Singh, C. Diagnosis and clinico-radiological presentation in an aggressive maxillary brown tumour. J. Clin. Diagn. Res. 2014, 8, ZD13–ZD15. [Google Scholar] [CrossRef] [PubMed]
- Martínez Díaz-Guerra, G.; Hawkins Carranza, F. Concept, etiology and epidemiology of primary hyperparathyroidism. Endocrinol. Nutr. 2009, 56 (Suppl. S1), 2–7. [Google Scholar] [CrossRef]
- Alwani, M.M.; Monaco, G.N.; Harmon, S.M.; Nwosu, O.I.; Vortmeyer, A.O.; Payner, T.D.; Ting, J. A Systematic Review of Sellar and Parasellar Brown Tumors: An Analysis of Clinical, Diagnostic, and Management Profiles. World Neurosurg. 2019, 132, e423–e429. [Google Scholar] [CrossRef]
- Pokhrel, B.; Leslie, S.W.; Levine, S.N. Primary Hyperparathyroidism. In StatPearls; StatPearls Publishing: Petersburg, FL, USA, 2024. [Google Scholar]
- Gallana Álvarez, S.; Salazar Fernandez, C.I.; Avellá Vecino, F.J.; Torres Gómez, J.; Pérez Sanchez, J.M. Tumor pardo maxilar: Elemento diagnóstico de hiperparatiroidismo primario. Rev. Esp. Cirug. Oral y Maxilofac. 2005, 27, 225–230. [Google Scholar] [CrossRef][Green Version]
- Majic Tengg, A.; Cigrovski Berkovic, M.; Zajc, I.; Salaric, I.; Müller, D.; Markota, I. Expect the unexpected: Brown tumor of the mandible as the first manifestation of primary hyperparathyroidism. World J. Clin. Cases 2024, 12, 1200–1204. [Google Scholar] [CrossRef]
- Liu, Z.; Yang, H.; Tan, H.; Song, R.; Zhang, Y.; Zhao, L. Brown tumor of the cervical spine with primary hyperparathyroidism: A case report and literature review. Medicine 2023, 102, e32768. [Google Scholar] [CrossRef]
- Antin, F.; Bakhos, D.; Jegoux, F.; Merkouza, M.; Laccourreye, L. Maxillofacial brown tumours: Series of 5 cases. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2018, 135, 227–230. [Google Scholar] [CrossRef]
- WHO Classification of Tumours Editorial Board. Giant Cell Lesions and Bone Cysts, Central Giant Cell Granuloma. In Head and Neck Tumours WHO Classification of Tumours, 5th ed.; IARC: Lyon, France, 2022; Volume 9. [Google Scholar]
- Genovesi, E.; Lerena, V.S.; Torres, I.C.; Paes De Lima, A.; Lucas, S.P.; Diaz, A.G. Brown tumors of the jaw: An atypical manifestation of primary hyperparathyroidism. Medicina (B Aires) 2023, 83, 462–466. [Google Scholar]
- Flanagan, A.M.; Speight, P.M. Giant cell lesions of the craniofacial bones. Head Neck Pathol. 2014, 8, 445–453. [Google Scholar] [CrossRef] [PubMed]
- Boffano, P.; Neirotti, F.; Brucoli, M.; Ruslin, M.; Stathopoulos, P.; Tsekoura, K.; Laco, J.; Mottl, R.; Dediol, E.; Kos, B.; et al. Diagnosis and management of central giant cell granulomas of the jaws: A European and multicenter study. J. Craniomaxillofac. Surg. 2025, 53, 1455–1462. [Google Scholar] [CrossRef]
- Khaoula, B.A.; Kaouther, B.A.; Ines, C.; Sami, T.; Zakraoui, L.; Khedher, A. An unusual presentation of primary hyperparathyroidism: Pathological fracture. Case Rep. Orthop. 2011, 2011, 521578. [Google Scholar] [CrossRef] [PubMed]
- Reséndiz-Colosia, J.A.; Alvarado-Cabrero, I.; Flores-Díaz, R.; Juan, M.H.; Barroso-Bravo, S.; Gómez-Acosta, F.; Rodríguez-Cuevas, S.A. Multiple maxillofacial brown tumors as primary hyperparathyroidism manifestation. Gac. Med. Mex. 2008, 144, 155–160. [Google Scholar]
- Hakkou, F.; Benjelloun, L.; Hallab, L.; Chbicheb, S. Brown tumor of the jaw as a rare manifestation of hyperparathyroidism: Two case reports and literature review. Int. J. Surg. Case Rep. 2023, 111, 108823. [Google Scholar] [CrossRef]
- Batra, S.; Srivastava, A.; Shukla, S. Unmasking the Archnemesis: Primary Hyperparathyroidism Presenting As Brown Tumors of the Jaws. Cureus 2025, 17, e84427. [Google Scholar] [CrossRef] [PubMed]
- Mastrapasqua, S.; Hendel, I. Maxillary brown tumor in secondary hyperparathyroidism. Nefrologia 2006, 26, 647–648. [Google Scholar]
- Fontseré Baldellou, N.; Andrés Santamaría, M.; Bella Cueto, F.; Ramírez de Arellano Serna, M. Brown tumour of the mandible and asymptomatic severe hypercalcemia as atypical forms of presentation of primary hyperparathyroidism. An. Med. Interna 2007, 24, 561–562. [Google Scholar]
- Mora-Escudero, I.; Gato-Díez, A.; Blázquez-Cabrera, J.A.; Lozano-Setien, E.; García de la Torre, J.P. Pretibial brown tumors as first manifestation of primary hyperparathyroidism. Rev. Clin. Esp. 2012, 212, e15–e18. [Google Scholar] [CrossRef]
- Zhong, Y.; Huang, Y.; Luo, J.; Ye, Y. Misdiagnosis of brown tumour caused by primary hyperparathyroidism: A case report with literature review. BMC Endocr. Disord. 2022, 22, 66. [Google Scholar] [CrossRef]
- Dinoi, E.; Prete, A.; Sardella, C.; Pierotti, L.; Della Valentina, S.; Dal Lago, A.; Borsari, S.; Pardi, E.; Caligo, M.A.; Michelucci, A.; et al. The challenge of the differential diagnosis between brown tumors and metastases in parathyroid carcinoma: A case report. Front. Endocrinol. 2024, 15, 1414896. [Google Scholar] [CrossRef] [PubMed]
| Results | Reference Value | |
|---|---|---|
| Parathormone | 120.00 pg/mL * | 15–65 pg/mL |
| Calcium | 8.80 mg/dL | 8.50–10.40 mg/dL |
| Phosphorus | 3.60 mMol/L | 2.50–4.50 mMol/L |
| Alkaline phosphatase | 93.00 U/L | 40.0–279.00 U/L |
| Calcitonin | <2.0 pg/mL | 0.00–11.5 pg/mL |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silva-Gutiérrez, V.M.; Macías-Jiménez, J.B.; Molotla-Fragoso, A.; Mejía-Velázquez, C.P.; Estévez-González, G.L.; Jacinto-Alemán, L.F. Brown Tumor in Jaw Associated with Hyperparathyroidism: A Case Report. Oral 2025, 5, 59. https://doi.org/10.3390/oral5030059
Silva-Gutiérrez VM, Macías-Jiménez JB, Molotla-Fragoso A, Mejía-Velázquez CP, Estévez-González GL, Jacinto-Alemán LF. Brown Tumor in Jaw Associated with Hyperparathyroidism: A Case Report. Oral. 2025; 5(3):59. https://doi.org/10.3390/oral5030059
Chicago/Turabian StyleSilva-Gutiérrez, Verónica Montserrat, Judith Berenice Macías-Jiménez, Adriana Molotla-Fragoso, Claudia Patricia Mejía-Velázquez, Gabriel Levi Estévez-González, and Luis Fernando Jacinto-Alemán. 2025. "Brown Tumor in Jaw Associated with Hyperparathyroidism: A Case Report" Oral 5, no. 3: 59. https://doi.org/10.3390/oral5030059
APA StyleSilva-Gutiérrez, V. M., Macías-Jiménez, J. B., Molotla-Fragoso, A., Mejía-Velázquez, C. P., Estévez-González, G. L., & Jacinto-Alemán, L. F. (2025). Brown Tumor in Jaw Associated with Hyperparathyroidism: A Case Report. Oral, 5(3), 59. https://doi.org/10.3390/oral5030059







