Stress Distribution in a Mandibular Kennedy Class I with Bilateral Implant-Assisted Removable Partial Denture: A Finite Element Analysis
Abstract
1. Introduction
2. Materials and Methods
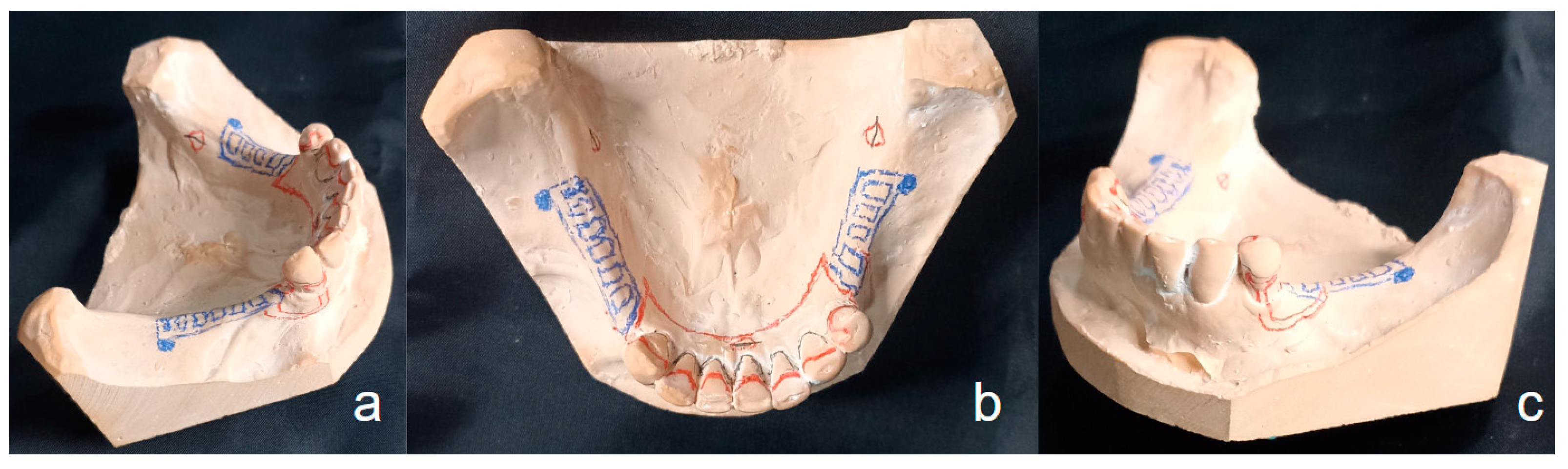
2.1. Plaster Model Preparation
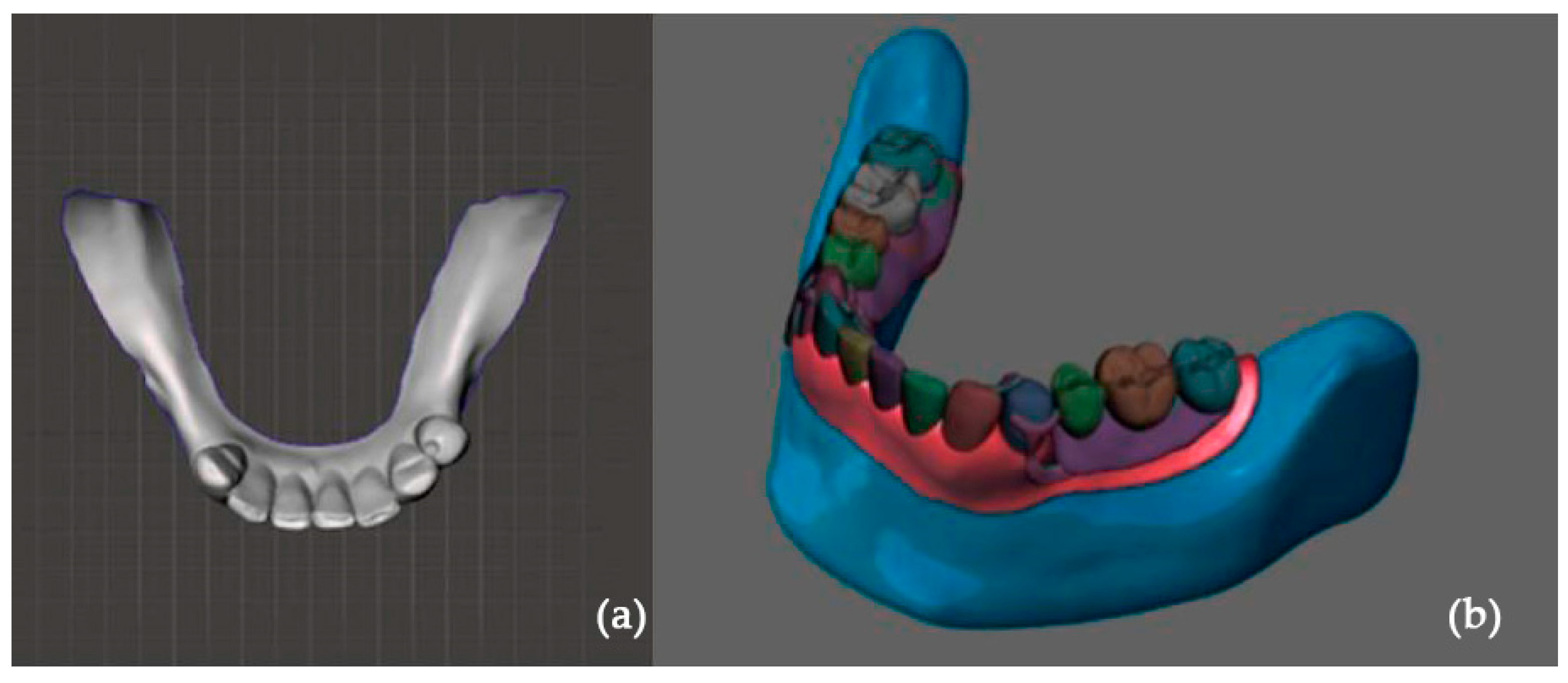
2.2. Digital Preparation
2.3. Finite Element Analysis
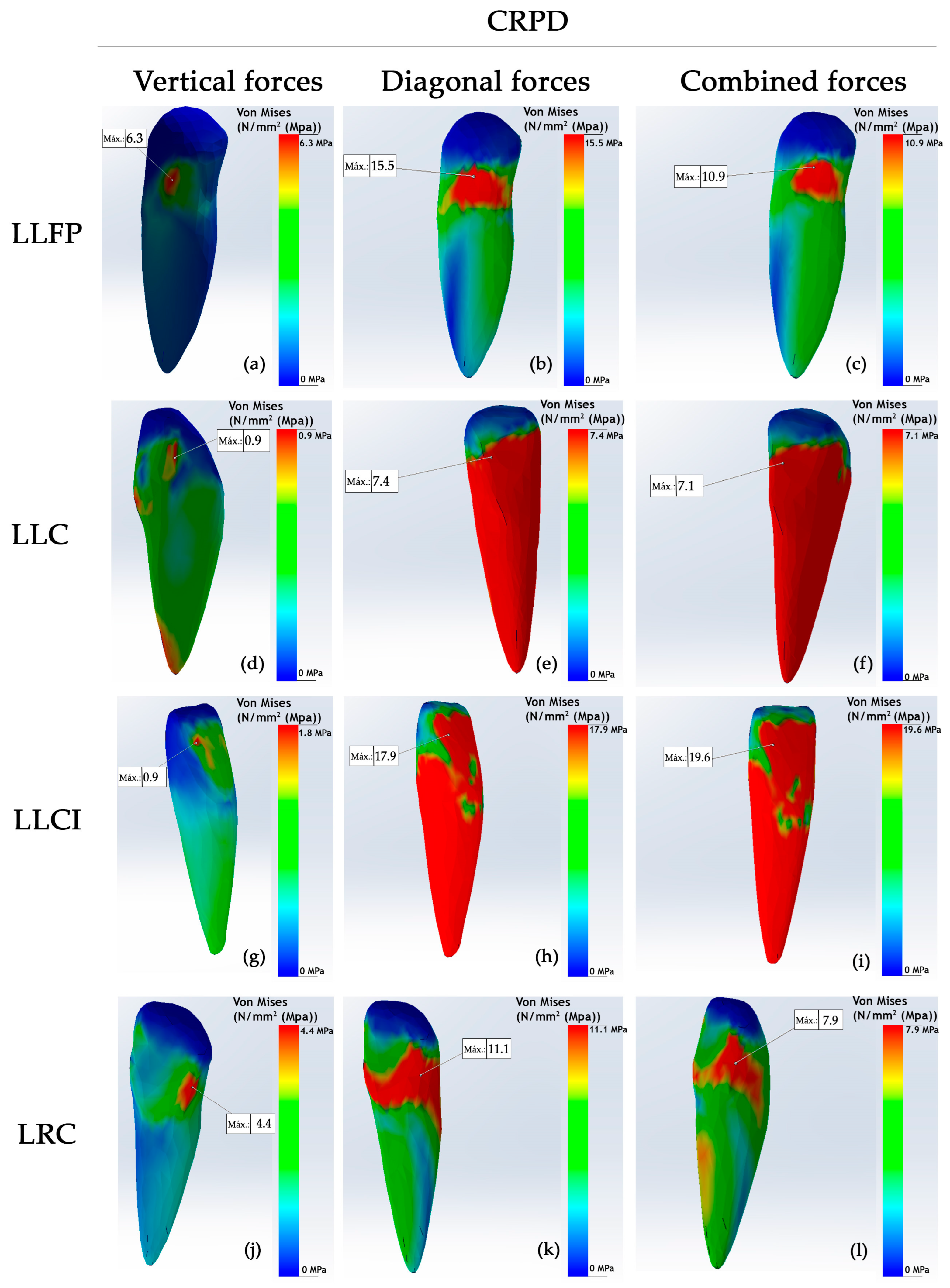
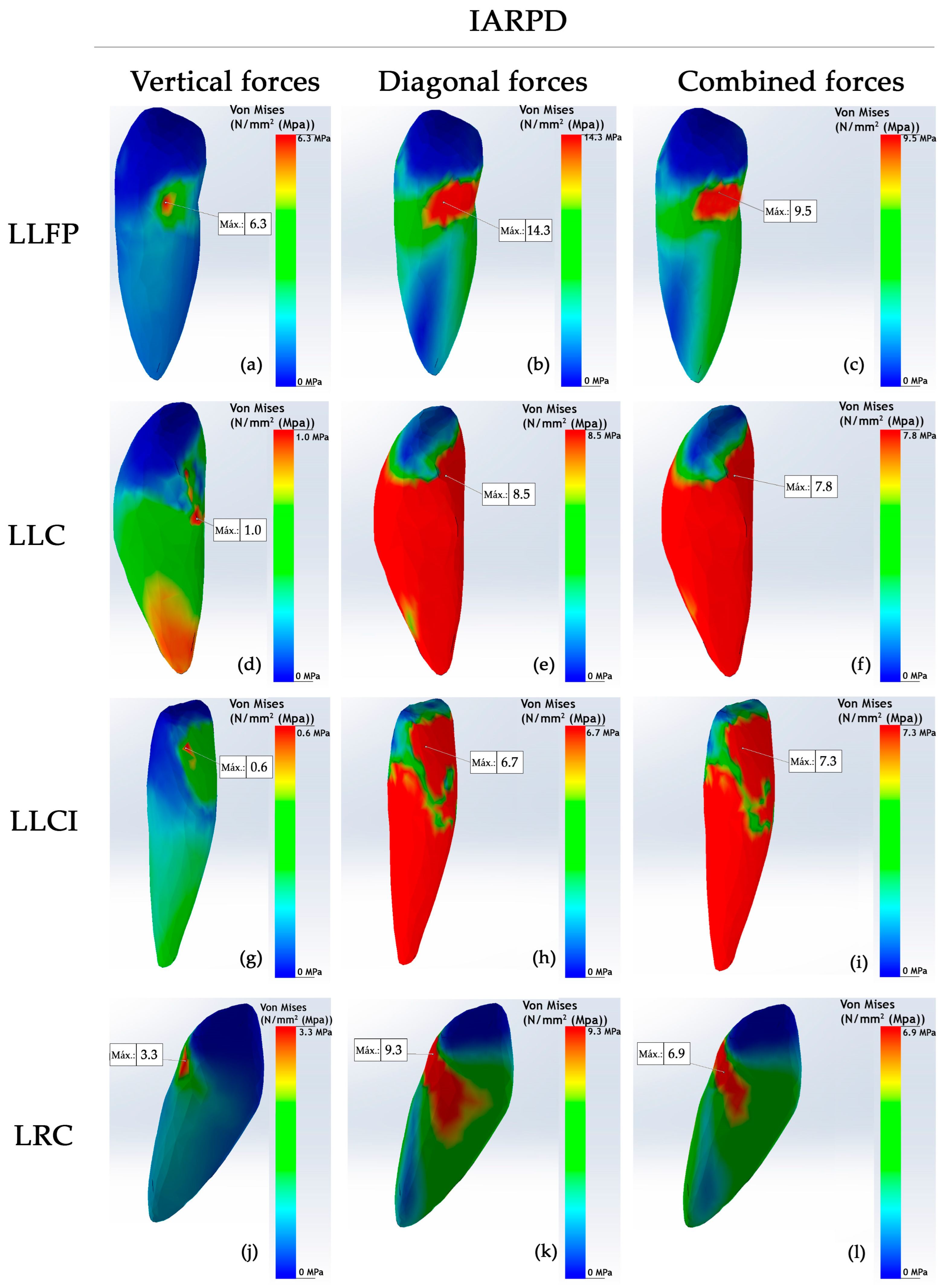
3. Results
4. Discussion
Clinical Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CRPD | Conventional removable partial denture |
| IARPD | Implant-assisted removable partial denture |
| LLFP | Lower left first premolar |
| LLC | Lower left canine |
| LLLI | Lower left lateral incisor |
| LLCI | Lower left central incisor |
| LRCI | Lower right central incisor |
| LRLI | Lower right lateral incisor |
| LRC | Lower right canine |
References
- Araujo, R.; Zancopé, K.; Moreira, R.; Barreto, T.; Neves, F. Mandibular implant-assisted removable partial denture—Kennedy Class I to Class III modification—Case series with masticatory performance and satisfaction evaluation. J. Clin. Exp. Dent. 2023, 15, e71–e78. [Google Scholar] [CrossRef] [PubMed]
- Kumar, N.; Kuma Koli, D.; Jain, V.; Nanda, A. Stress distribution and patient satisfaction in flexible and cast metal removable partial dentures: Finite element analysis and randomized pilot study. J. Oral Biol. Craniofac. Res. 2021, 11, 478–485. [Google Scholar] [CrossRef]
- Putra, A.Y.; Goto, T.; Iwawaki, Y.; Ishida, Y.; Watanabe, M.; Ichikawa, T. Treatment outcomes of implant-assisted removable partial denture with distal extension based on the Kennedy classification and attachment type: A systematic review. Int. J. Implant. Dent. 2021, 7, 111. [Google Scholar] [CrossRef]
- Shahmiri, R.; Aarts, J.; Bennani, V.; Atieh, M.; Swain, M. Finite Element Analysis of an Implant-Assisted Removable Partial Denture. J. Prosthodont. 2013, 22, 550–555. [Google Scholar] [CrossRef] [PubMed]
- Rendon-Yúdice, R. Prótesis Parcial Removible. Conceptos actuales. Atlas de diseño. 1° Ed. México. In Chapter 3: Difference Between Tooth-Supported and Dentomucosal (or Distal Extension) Removable Partial Dentures; Editorial Médica Panamericana: Buenos Aires, Argentina, 2006; pp. 9–11. [Google Scholar]
- Park, J.; Lee, J.; Shin, S.; Kim, H. Effect of conversion to implant-assisted removable partial denture in patients with mandibular Kennedy classification Ⅰ: A systematic review and meta-analysis. Clin. Oral Implant. Res. 2020, 31, 360–373. [Google Scholar] [CrossRef]
- Bandiaky, O.; Lokossou, D.; Soueidan, A.; Le Bars, P.; Gueye, M.; Mbodj, E.; Le Guéhennec, L. Implant-supported removable partial dentures compared to conventional dentures: A systematic review and meta-analysis of quality of life, patient satisfaction, and biomechanical complications. Clin. Exp. Dent. Res. 2022, 8, 294–312. [Google Scholar] [CrossRef] [PubMed]
- Silveira, R.; Laprida, A.; Macedo, A.; Chiarello, M.; Ribeiro, R. Retention and stress distribution in distal extension removable partial dentures with and without implant association. J. Prosthodont. Res. 2013, 57, 24–29. [Google Scholar] [CrossRef]
- Girotra, M.; Yadav, B.; Malhotra, P.; Ritwal, P.; Singh, D.; Madan, R. Comparative Evaluation of the Stresses on the Terminal Abutment and Edentulous Ridge in Unilateral Distal Extension Condition when Restored with Different ProstheticOptions: An FEA Analysis. J. Prosthodont. Restor. Dent. 2023, 13, 58–64. [Google Scholar] [CrossRef]
- Zancopé, K.; Abrão, G.; Karam, F.; Neves, F. Placement of a distal implant to convert a mandibular removable Kennedy class I to an implant-supported partial removable Class III dental prosthesis: A systematic review. J. Prosthet. Dent. 2015, 113, 528–533.e3. [Google Scholar] [CrossRef]
- Ortiz-Puigpelat, O.; Lázaro-Abdulkarim, A.; de Medrano-Reñé, J.-M.; Gargallo-Albiol, J.; Cabratosa-Termes, J.; Hernández-Alfaro, F. Influence of Implant Position in Implant-Assisted Removable Partial Denture: A Three-Dimensional Finite Element Analysis. J. Prosthodont. 2019, 28, e675–e681. [Google Scholar] [CrossRef]
- Rocca, S.; Tanaka, N.; Watanabe, R.; Cueva, L. Removable partial dentures associated with dental implants: Literature review. KIRU 2023, 20, 190–196. [Google Scholar] [CrossRef]
- Tun Naing, S.; Kanazawa, M.; Hada, T.; Iwaki, M.; Komagamine, Y.; Miyayasu, A.; Uehara, Y.; Minakuchi, S. In vitro study of the effect of implant position and attachment type on stress distribution of implant-assisted removable partial dentures. J. Dent. Sci. 2022, 17, 1697–1703. [Google Scholar] [CrossRef] [PubMed]
- Payne, A.; Tawse-Smith, A.; Wismeijer, D.; De Silva, R.; Sunyoung, M. Multicentre prospective evaluation of implant-assisted mandibular removable partial dentures: Surgical and prosthodontic outcomes. Clin. Oral Implant. 2017, 28, 116–125. [Google Scholar] [CrossRef]
- Mousa, M.; Abdullah, J.; Jamayet, N.; El-Anwar, M.; Ganji, K.; Alam, M.; Husein, A. Biomechanics in Removable Partial Dentures: A Literature Review of FEA-Based Studies. BioMed Res. Int. 2021, 2021, 5699962. [Google Scholar] [CrossRef] [PubMed]
- Rungsiyakull, C.; Rungsiyakull, P.; Suttiat, K.; Duangrattanaprathip, N. Stress Distribution Pattern in Mini Dental Implant-Assisted RPD with Different Clasp Designs: 3D Finite Element Analysis. Int. J. Dent. 2022, 2022, 2416888. [Google Scholar] [CrossRef]
- Messias, A.; Neto, M.; Amaro, A.; Lopes, V.; Nicolau, P. Mechanical Evaluation of Implant-Assisted Removable Partial Dentures in Kennedy Class I Patients: Finite Element Design Considerations. Appl. Sci. 2021, 11, 659. [Google Scholar] [CrossRef]
- Lemos, C.; Nunes, R.; Santiago-Júnior, J.; Gomes, J.; Oliveira, J.; Rosa, C.; Verri, F.; Pellizzer, E. Are implant-supported removable partial dentures a suitable treatment for partially edentulous patients? A systematic review and meta-analysis. J. Prosthet. Dent. 2023, 129, 538–546. [Google Scholar] [CrossRef]
- Solano, K.; Orejuela-Ramírez, F.; Castillo, D. Frecuencia de tratamientos con prótesis convencional y sobre implantes en pacientes atendidos en el centro dental de una universidad privada en Lima, Perú, por un período de cuatro años. Rev. Estomatol. Herediana 2024, 34, 221–231. [Google Scholar] [CrossRef]
- Cespedes, S.; Peche, N. Oral Rehabilitation with Removable Partial Dentures in Partially Edentulous Patients (2020–2023): A Bibliometric Analysis. Bachelor’s Thesis, Señor de Sipan University, Pimentel, Peru, 2024. [Google Scholar]
- Romanyk, D.; Vafaeian, B.; Addison, O.; Adeeb, S. The use of finite element analysis in dentistry and orthodontics: Critical points for model development and interpreting results. Semin. Orthod. 2020, 26, 162–173. [Google Scholar] [CrossRef]
- Shivakumar, S.; Kudagi, V.S.; Talwade, P. Applications of finite element analysis in dentistry: A review. J. Int. Oral Health 2021, 13, 415–422. [Google Scholar]
- Madruga, C.F.L.; Ramos, G.F.; Borges, A.L.S.; Saavedra, G.d.S.F.A.; Souza, R.O.; Marinho, R.M.d.M.; Penteado, M.M. Stress Distribution in Modified Veneer Crowns: 3D Finite Element Analysis. Oral 2021, 3, 272–280. [Google Scholar] [CrossRef]
- Murashima, N.; Takayama, Y.; Nogawa, T.; Yokoyama, A.; Sakaguchi, K. Mechanical Effect of an Implant Under Denture Base in Implant-Supported Distal Free-End Removable Partial Dentures. Dent. J. 2024, 12, 358. [Google Scholar] [CrossRef] [PubMed]
- Hedeșiu, M.; Pavel, D.G.; Almășan, O.; Pavel, S.G.; Hedeșiu, H.; Rafiroiu, D. Three-Dimensional Finite Element Analysis on Mandibular Biomechanics Simulation under Normal and Traumatic Conditions. Oral 2022, 3, 221–237. [Google Scholar] [CrossRef]
- Tribst, J.P.; de Araújo, R.M.; Ramanzine, N.P.; Santos, N.R.; Dal Piva, A.O.; Borges, A.L.; da Silva, J.M. Mechanical behavior of implant assisted removable partial denture for Kennedy class II. J. Clin. Exp. Dent. 2020, 12, e38–e45. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Matsudate, Y.; Yoda, N.; Nanba, M.; Ogawa, T.; Sasaki, K. Load distribution on abutment tooth, implant and residual ridge with distal-extension implant-supported removable partial denture. J. Prosthodont. Res. 2016, 60, 282–288. [Google Scholar] [CrossRef]
- Abdulkaremm, J.; Salloomi, K.; Faraj, S.; Al-Zahawi, A.; Abdullah, O.; Tulunoglu, I. Finite element analysis of class II mandibular unilateral distal extension partial dentures. J. Mech. Eng. Sci. 2022, 236, 9407–9418. [Google Scholar] [CrossRef]
- Yi, Y.; Heo, S.J.; Koak, J.Y.; Kim, S.K. Clinical Outcomes of Implant-Assisted Removable Partial Dentures According to Implant Strategic Position. J. Prosthodont. 2023, 32, 401–410. [Google Scholar] [CrossRef]
- You-Kyoung, O.; Eun-Bin, B.; Jung-Bo, H. Retrospective clinical evaluation of implant-assisted removable partial dentures combined with implant surveyed prostheses. J. Prosthet. Dent. 2021, 126, 76–82. [Google Scholar] [CrossRef]
- Toro, M.; Chaple-Gil, A.; Romo, F.; Díaz, L. Performance and Maximum Functional Masticatory Force in Patients with Dentomucosal-supported and Implant-supported Removable Partial Dentures. Rev. Cuba. Estomatol. 2024, 61, e4917. [Google Scholar]
- Ichikawa, H.; Yoda, N.; Ogawa, T.; Iwamoto, M.; Kawata, T.; Egusa, H.; Sasaki, K. Impact of implant location on load distribution of implant-assisted removable partial dentures: A review of in vitro model and finite-element analysis studies. Int. J. Implant Dent. 2023, 9, 31. [Google Scholar] [CrossRef]
- Jia-Mahasap, W.; Rungsiyakull, C.; Bumrungsiri, W.; Sirisereephap, N.; Rungsiyakull, N. Effect of Number and Location on Stress Distribution of Mini Dental Implant-Assisted Mandibular Kennedy Class I Removable Partial Denture: Three-Dimensional Finite Element Analysis. Int. J. Dent. 2022, 2022, 4825177. [Google Scholar] [CrossRef] [PubMed]
- Kuroshima, S.; Ohta, Y.; Uto, Y.; Al-Omari, F.; Sasaki, M.; Sawase, T. Implant-assisted removable partial dentures: Part I. A scoping review of clinical applications. J. Prosthodont. Res. 2024, 68, 20–39. [Google Scholar] [CrossRef] [PubMed]
- Kuroshima, S.; Sasaki, M.; Al-Omari, F.A.; Uto, Y.; Ohta, Y.; Uchida, Y.; Sawase, T. Implant-assisted removable partial dentures: Part II. a systematic review of the effects of implant position on the biomechanical behavior. J. Prosthodont. Res. 2024, 68, 40–49. [Google Scholar] [CrossRef] [PubMed]
- Duong, H.; Roccuzzo, A.; Stähli, A.; Salvi, G.; Lang, N.; Sculean, A. Oral health-related quality of life of patients rehabilitated with fixed and removable implant-supported dental prostheses. Perio 2000. 2022, 88, 201–237. [Google Scholar] [CrossRef]
- Lahoud, T.; Yu, A.Y.; King, S. Masticatory dysfunction in older adults: A scoping review. J. Oral Rehabil. 2023, 50, 724–737. [Google Scholar] [CrossRef]
- Zelig, R.; Goldstein, S.; Touger-Decker, R.; Firestone, E.; Golden, A.; Johnson, Z.; Kaseta, A.; Sackey, J.; Tomesko, J.; Parrott, J.S. Tooth Loss and Nutritional Status in Older Adults: A Systematic Review and Meta-analysis. JDR Clin. Trans. Res. 2022, 7, 4–15. [Google Scholar] [CrossRef]
- Murakami, K.; Ayukawa, Y.; Ogino, Y.; Nakagawa, A.; Horikawa, T.; Yamaguchi, E.; Takaki, K.; Koyano, K. Clinical effectiveness of implant support for distal extension removable partial dentures: Functional evaluation using occlusal force measurement and masticatory efficiency. Int. J. Implant Dent. 2021, 7, 101. [Google Scholar] [CrossRef]

| Characteristic | Mandibular Bone | Teeth | Chrome–Cobalt Metal Structure |
|---|---|---|---|
| Young’s modulus (GPa) | 4.5 | 18.6 | 206.9 |
| Poisson’s ratio | 0.3 | 0.30 | 0.33 |
| Direction of Forces | Type | Maximum Stress Level (MPa) |
|---|---|---|
| Vertical | CRPD | 7 |
| IARPD | 4.2 | |
| Diagonal | CRPD | 32.4 |
| IARPD | 12.2 | |
| Combined | CRPD | 26.3 |
| IARPD | 12.3 |
| Direction of Forces | RPD Type | Teeth | ||||||
|---|---|---|---|---|---|---|---|---|
| LLFP | LLC | LLLI | LLCI | LRCI | LRLI | LRC | ||
| Vertical | CRPD | 6.3 | 0.9 | 0.6 | 1.8 | 0.4 | 0.9 | 4.4 |
| IARPD | 6.3 | 1.0 | 0.6 | 0.6 | 0.3 | 0.9 | 3.3 | |
| Diagonal | CRPD | 15.5 | 7.4 | 3.4 | 17.9 | 4.5 | 4.4 | 11.1 |
| IARPD | 14.3 | 8.5 | 3.7 | 6.7 | 4.2 | 4.5 | 9.3 | |
| Combined | CRPD | 10.9 | 7.1 | 3.3 | 19.6 | 4.5 | 3.8 | 7.9 |
| IARPD | 9.5 | 7.8 | 3.6 | 7.3 | 4.1 | 3.8 | 6.9 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ochoa-Escate, D.; Valdez-Jurado, F.; Watanabe, R.; Pineda-Mejía, M.; Córdova Huayanay, E.A.; Ventocilla Huasupoma, M.S.; Herrera Cisneros, M.; Lujan Larreátegui, G.; Quispe-Salcedo, A.; Salcedo-Moncada, D.; et al. Stress Distribution in a Mandibular Kennedy Class I with Bilateral Implant-Assisted Removable Partial Denture: A Finite Element Analysis. Oral 2025, 5, 31. https://doi.org/10.3390/oral5020031
Ochoa-Escate D, Valdez-Jurado F, Watanabe R, Pineda-Mejía M, Córdova Huayanay EA, Ventocilla Huasupoma MS, Herrera Cisneros M, Lujan Larreátegui G, Quispe-Salcedo A, Salcedo-Moncada D, et al. Stress Distribution in a Mandibular Kennedy Class I with Bilateral Implant-Assisted Removable Partial Denture: A Finite Element Analysis. Oral. 2025; 5(2):31. https://doi.org/10.3390/oral5020031
Chicago/Turabian StyleOchoa-Escate, Dagny, Freddy Valdez-Jurado, Romel Watanabe, Martha Pineda-Mejía, Edwin Antonio Córdova Huayanay, Maria Soledad Ventocilla Huasupoma, Marcos Herrera Cisneros, Giovanna Lujan Larreátegui, Angela Quispe-Salcedo, Doris Salcedo-Moncada, and et al. 2025. "Stress Distribution in a Mandibular Kennedy Class I with Bilateral Implant-Assisted Removable Partial Denture: A Finite Element Analysis" Oral 5, no. 2: 31. https://doi.org/10.3390/oral5020031
APA StyleOchoa-Escate, D., Valdez-Jurado, F., Watanabe, R., Pineda-Mejía, M., Córdova Huayanay, E. A., Ventocilla Huasupoma, M. S., Herrera Cisneros, M., Lujan Larreátegui, G., Quispe-Salcedo, A., Salcedo-Moncada, D., & Ochoa Tataje, J. J. (2025). Stress Distribution in a Mandibular Kennedy Class I with Bilateral Implant-Assisted Removable Partial Denture: A Finite Element Analysis. Oral, 5(2), 31. https://doi.org/10.3390/oral5020031





