1. Introduction
Normal eruption in human dentition refers to the axial movement of a tooth from its initial non-functional, developmental position in the alveolar bone to its final functional position within the oral cavity in occlusion to its antagonist [
1]. Tooth eruption is an intricate, genetically determined process [
2,
3,
4]. Variations in the actual age and sequence of tooth eruption have been documented in the literature, depending on factors such as race, gender, and the presence of both local and systemic conditions [
5,
6,
7]. In order to provide effective orthodontic treatment, knowledge regarding times of tooth eruption is essential [
4]. Any alteration regarding the order or timing during the eruption process needs to be identified, monitored, and appropriately managed to eliminate possible adverse effects that may contribute to serious orthodontic disorders [
8].
Delayed tooth eruption (DTE) is described as the appearance of a tooth into the oral cavity at a time that greatly exceeds what is considered normal for different races, ethnic backgrounds, and sexes [
4,
9]. DTE may affect deciduous and/or permanent teeth, and its clinical manifestation can be any of the following conditions: the standard eruption time has been exceeded, a tooth is absent in the dental arch with no evidence of potential for eruption, an unerupted tooth has complete root formation, or a contralateral tooth has been erupted for at least 6 months [
10]. Profitt and Vig described a condition known as primary or idiopathic eruption failure, in which non-ankylosed teeth fail to erupt completely or partially due to an abnormality in the eruption process [
11]. Although it appears to be no obstruction to eruption, this phenomenon occurs and is attributed to a substantial defect in the eruptive mechanism [
11,
12].
The aetiology of DTE is still under investigation. Associations between delayed eruption and other dental anomalies of known genetic origin suggest that DTE may have a significant genetic component. Recent research has identified specific genes, parathyroid hormone receptor 1 (PTH1R), and lysine methyltransferase 2C (KMT2C), which are responsible for familial cases of primary failure of eruption (PFE). These findings suggest that other abnormalities in tooth eruption that do not involve a physical obstruction, such as mechanical failure of eruption or lateral tongue pressure, may have a genetic background [
13,
14].
The pathogenesis of DTE has been associated with local, systemic, and genetic factors [
4,
15]. Supernumerary teeth, gingival fibromatosis/gingival hyperplasia, mucosal barrier/scar tissue from trauma/surgery, oral clefts, regional odontodysplasia, arch-length deficiency, and odontomas and other tumours have been identified as some of the local conditions that may lead to DTE. Regional odontodysplasia, commonly known as “ghost teeth”, is a rare dental anomaly that may be caused by a somatic mutation or a latent virus in the odontogenic epithelium [
16,
17]. Affected teeth delay or completely fail to erupt, and exhibit considerably altered shape, quite irregular, often with indications of defective mineralization. The most frequently affected teeth are central incisors, lateral incisors, and canines in either the maxillary or mandibular arch, and deciduous and permanent teeth can be affected [
16]. Systemic conditions associated with DTE are vitamin D-resistant rickets, endocrine disorders, cerebral palsy, drugs, long-term chemotherapy, anaemia, or it may be idiopathic. In addition, supernumerary teeth, tumors and cysts in the jaws have been linked to DTE in several genetic disorders, such as Apert syndrome, cleidocranial dysostosis, osteopetrosis, growth retardation, alopecia, pseudoanodontia and optic atrophy (GAPO) syndrome, Gorlin syndrome, cherubism, and Gardner syndrome, since they can interfere with tooth eruption process [
4,
18].
For an accurate diagnosis and an effective management of DTE, clinicians should thoroughly evaluate the patient’s history in addition to clinical and radiographic examination. When teeth do not erupt at the predicted chronologic and dental age, local and systemic conditions as well as genetic disorders related to the patient’s familial history should be carefully investigated. Clinical examination should be performed methodically, starting with an overall physical evaluation of the patient and progressing to intraoral examination, which includes inspection, palpation, and percussion. In the radiographic examination, a panoramic radiograph should be obtained to assess the extent of dental development and the location of developing teeth, estimate the time of teeth emergence into the oral cavity, and screen for radiolucent lesions associated with unerupted crowns [
4,
9].
Table 1 summarizes the important factors that contribute to DTE.
In cases where DTE is considered, congenital tooth agenesis should be examined in the differential diagnosis as well. Tooth agenesis has been reported at a rate of 0.5% to 0.9% in deciduous dentition and 1.6% to 9.6% in permanent dentition (when third molars are excluded) of the general population. The teeth with the highest prevalence of congenital agenesis, following third molars, are mandibular second premolars and maxillary lateral incisors. Upon confirming the clinical diagnosis of chronologic DTE (>2 standard deviations, SD), a panoramic radiograph should be performed, since it will reveal the tooth’s developmental stage and exclude the possibility of tooth agenesis [
4].
Orthodontic treatment planning of DTE can be very challenging and management of these cases requires an interdisciplinary approach considering the patient’s overall characteristics. The main therapeutic considerations for patients with DTE are (a) the choice to extract or maintain and surgically expose the affected teeth, (b) application of orthodontic traction, (c) the need for space opening and maintenance, (d) surgical removal of obstructions, and (e) diagnosis and treatment of an underlying systemic condition that leads to DTE [
4]. Removal of primary teeth should not be carried out too early, and the therapy must be justified by radiographs to assess the stage of root development. In this case, primary tooth extraction could instigate slow axial movement of their successors and alignment of teeth. If primary teeth are not extracted on time, eruption may fail [
19]. Self-esteem of patients with DTE may also be affected, especially when anterior teeth are delayed for eruption and aesthetics are compromised [
20].
Several published articles have highlighted the importance of DTE as a clinical problem [
4,
8]. Early diagnosis and intervention in cases of DTE are crucial for several reasons, as they can help address potential underlying health issues and prevent complications. More specifically, DTE may be a sign of other health conditions, such as genetic disorders (e.g., Down syndrome), endocrine disorders (e.g., hypothyroidism), or systemic diseases [
4,
18]. Early diagnosis allows healthcare providers to identify these underlying health issues, which might otherwise go unnoticed. In addition, early intervention contributes to prevent or address issues of malocclusions, crowding, or misalignment of teeth, and eliminates the risk of complications, such as dental abscesses, cysts, or other infections that may derive from delayed eruption. Improved psychological and social development of the affected children is another important aspect of timely DTE treatment [
20]. By identifying delayed eruption early on, dental clinicians can provide appropriate guidance and more effective treatment options, leading to successful treatment in long-term dental alignment and better outcomes for both oral health and overall well-being of the patients. Interceptive orthodontic interventions during the period of mixed dentition followed by surgical exposure (if needed) of the affected teeth and orthodontic traction should be considered in the treatment planning of patients with DTE. This case report presents the orthodontic treatment of a girl diagnosed with tooth agenesis and delayed tooth eruption.
2. Case Presentation
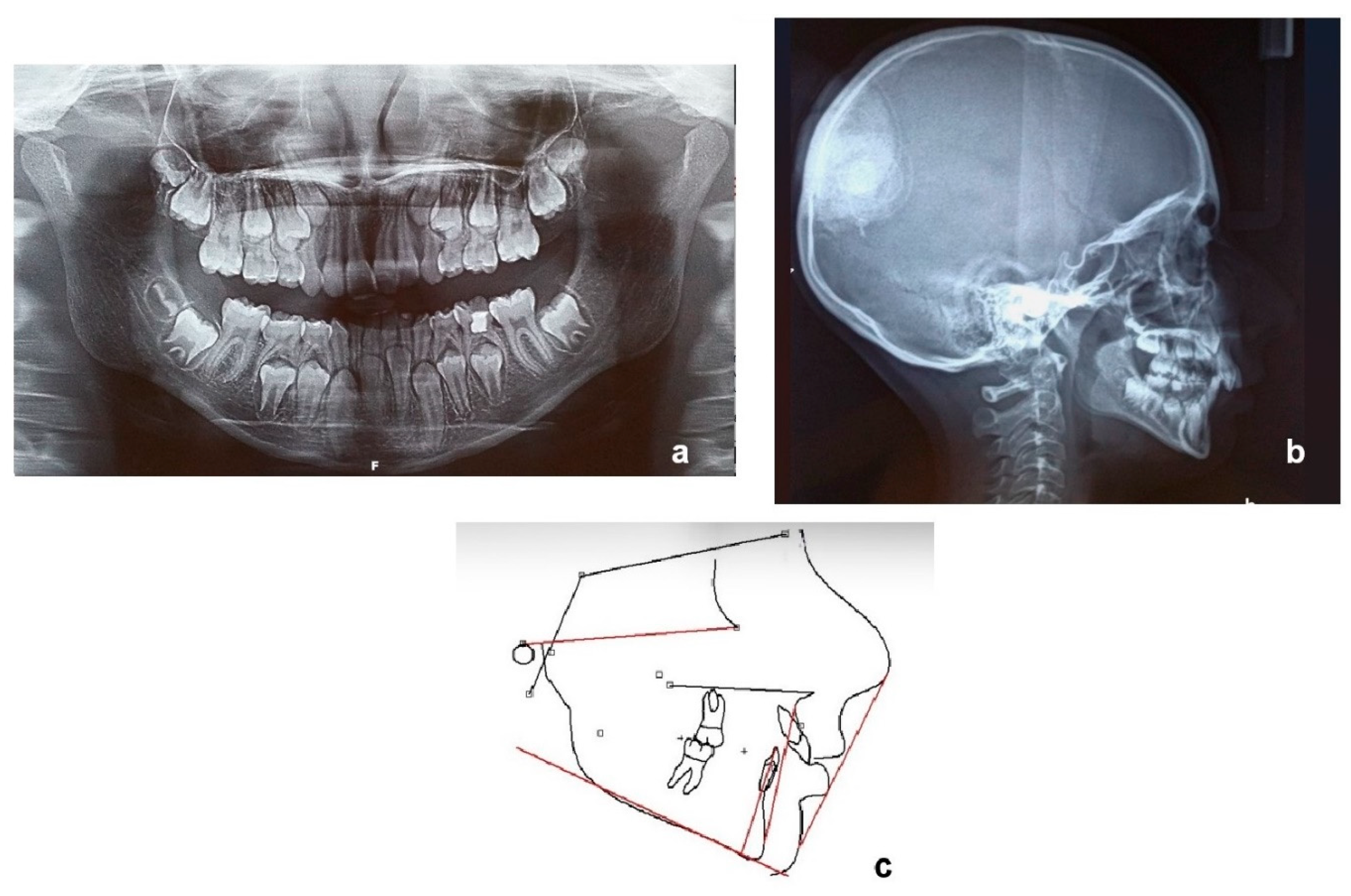
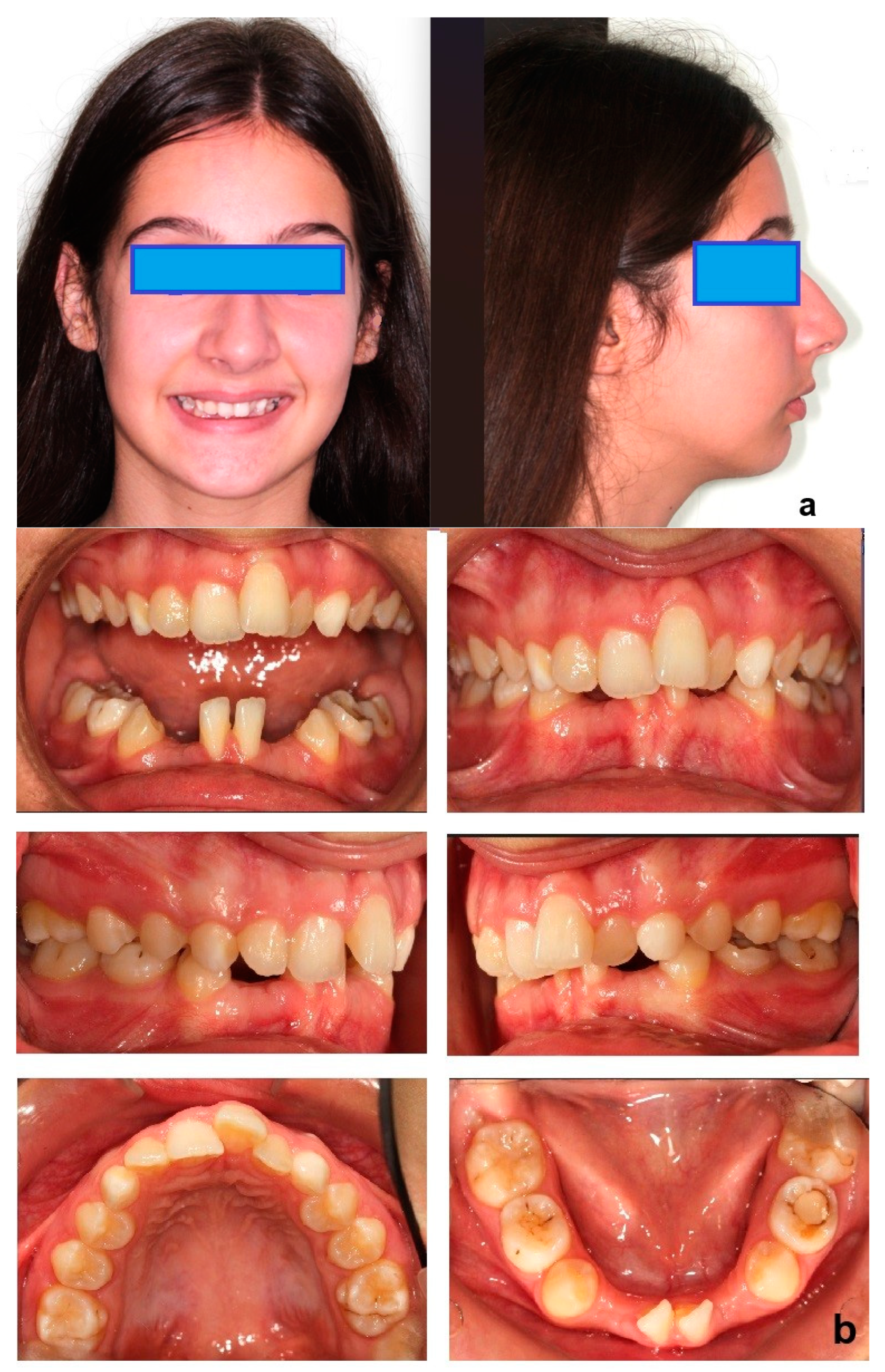
An 11-year-old female patient presented with a Class II molar relationship and a Class II skeletal relationship due to downward and backward rotation of the mandible. Increased overjet (21–71) was recorded, and deciduous lower central incisors and canines were in place while in the upper arch incisors had normally erupted. Upper canines had not been erupted yet and deciduous molars were in place in the lower arch. Radiographic examination with panoramic and lateral cephalometric X-ray in the beginning (
Figure 1) revealed that lower central incisors were congenitally missing, and later incisors and canines had their root almost fully formatted. The medical records that were provided indicated that right after birth the newborn was admitted to the neonatal intensive care unit for a cleft of the soft palate and a significant lower jaw retrognathism. Initial cytogenetic report was normal and the check for pathologic findings on chromosome 22, which possibly applies to Di George syndrome (22q11.2 region), was negative. No other local or systemic factors were identified. The cleft was surgically treated at the 15th month of age. The case was characterized as presenting delayed tooth eruption alongside the skeletal and dental Class II relationship.
It was decided to monitor the case for a while with just ordering the extraction of deciduous teeth in order to evaluate the potential of spontaneous eruption of the permanent ones. A progress panoramic X-ray was obtained at that time (
Figure 2). Lower deciduous lateral incisors, lower deciduous canines as well as upper and lower first deciduous molars were first extracted.
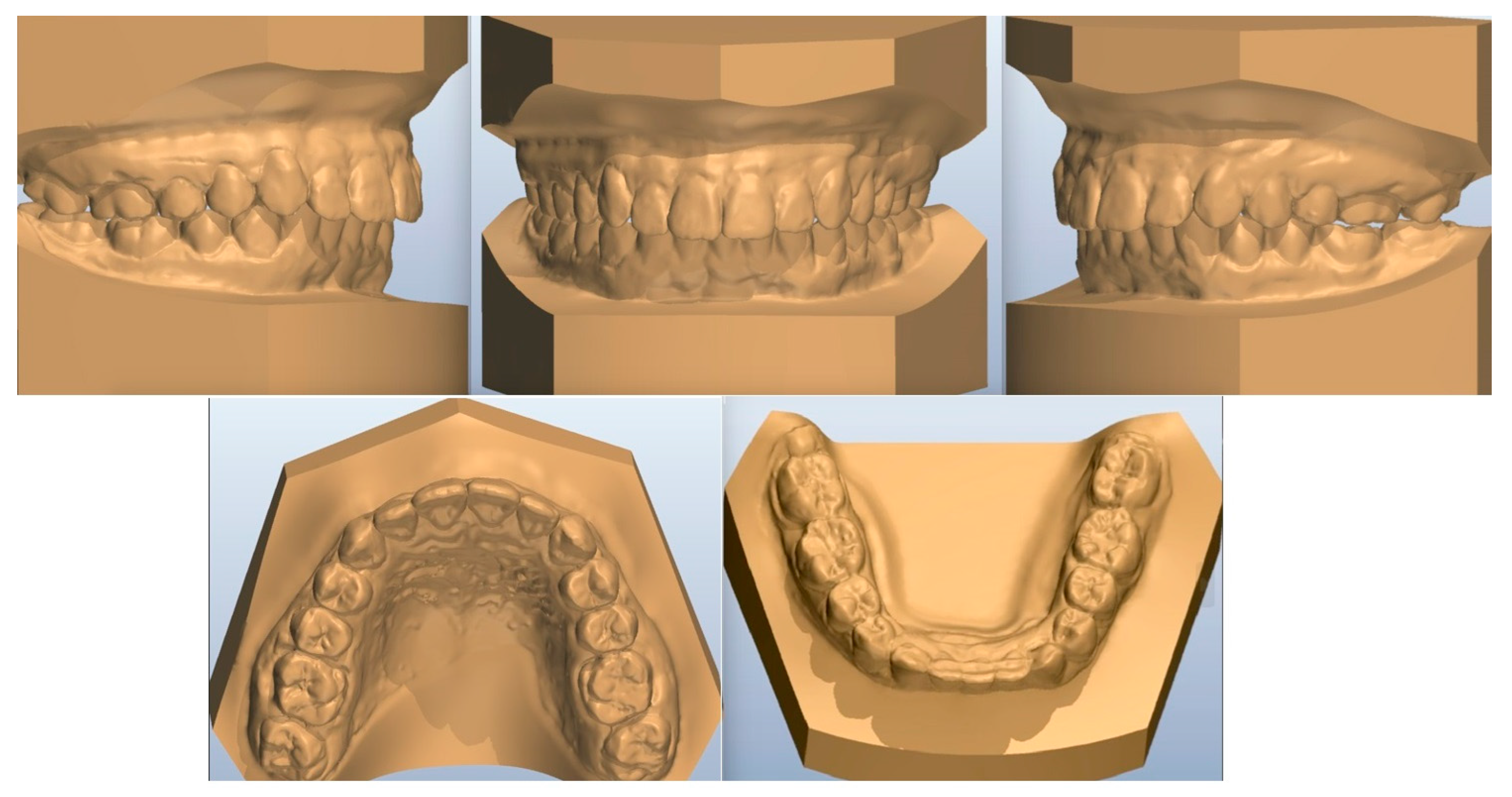
When permanent upper and lower premolars erupted after several months (
Figure 3), orthodontic treatment started by placing fixed appliances (0.22 slot edgewise appliance). Digital models, acquired some months later, are presented in
Figure 4). Aesthetic pontics (33, 43) with brackets on them were adjusted on the orthodontic wire for social reasons (
Figure 5).
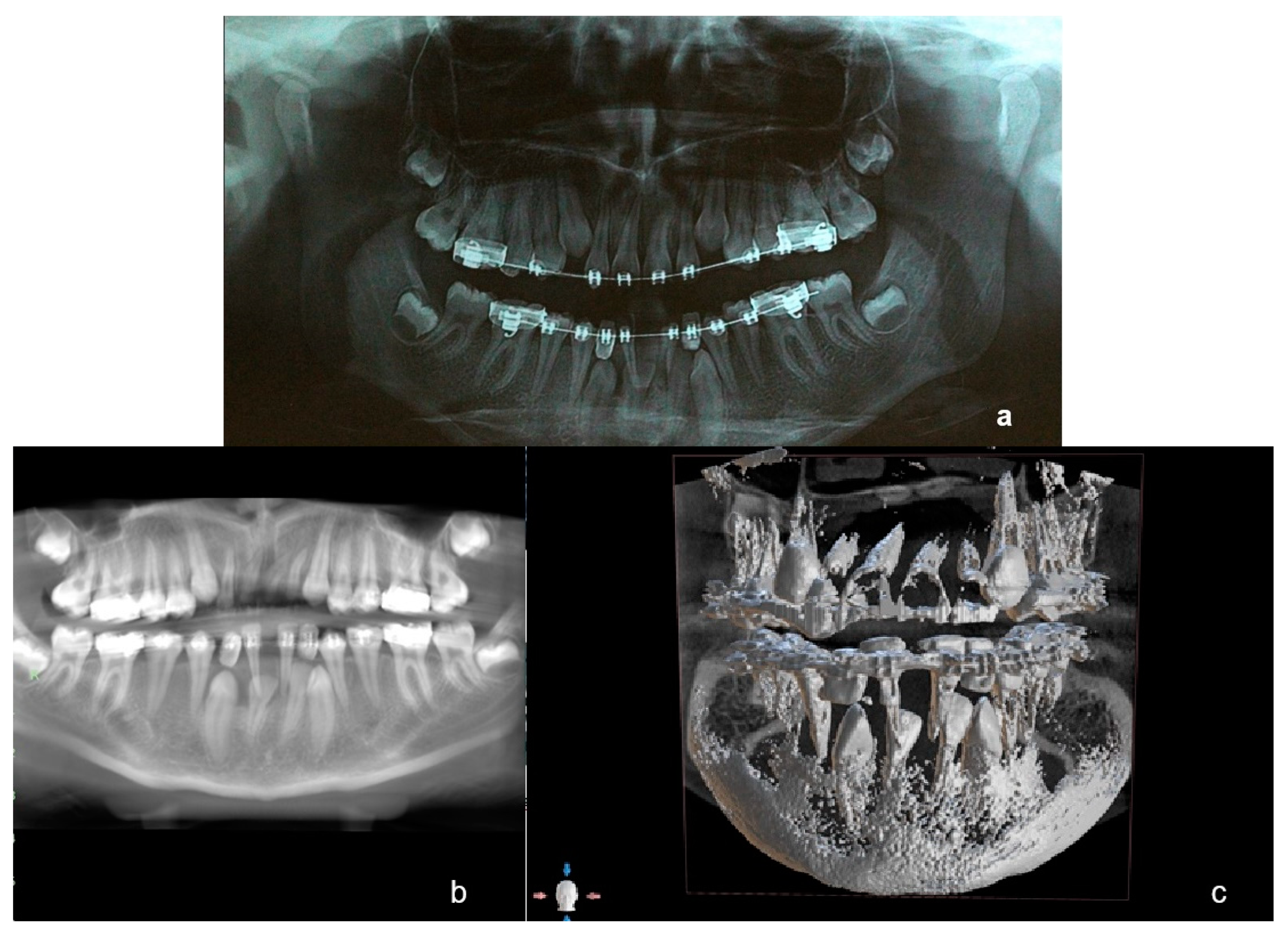
Several months later a new panoramic radiograph (
Figure 6a) and a subsequent (3 months later) cone-beam computed tomography (CBCT) (
Figure 6b,c) were performed. The shape and configuration of the roots of 11 and 21 was noted on those illustrations as they presented significant deformation, while 42 had a decreased size of the root. As the roots of lower deciduous central incisors were intact, it was decided not to extract them for the moment, as they could be utilized to enhance anchorage for the orthodontic traction of impacted incisors and canines. It was also decided to open the space between them in order to obtain space in the arch as there might be a spontaneous eruption of 42. Additionally, a high pull headgear was fitted in order to achieve an upwards rotation of the mandible and deal with the skeletal Class II relationship.
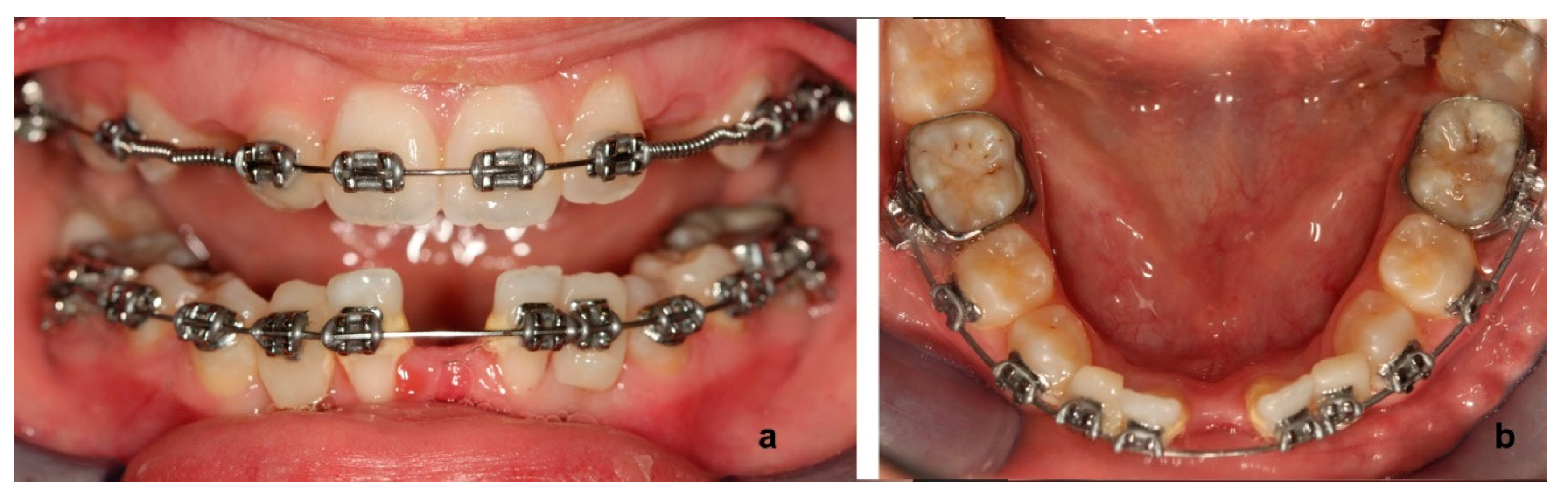
After alignment was completed and space was opened for upper and lower unerupted teeth, only 13 and 23 were spontaneously erupted. Thus, surgical exposure and orthodontic traction was scheduled for 33, 32, 42, and 43.
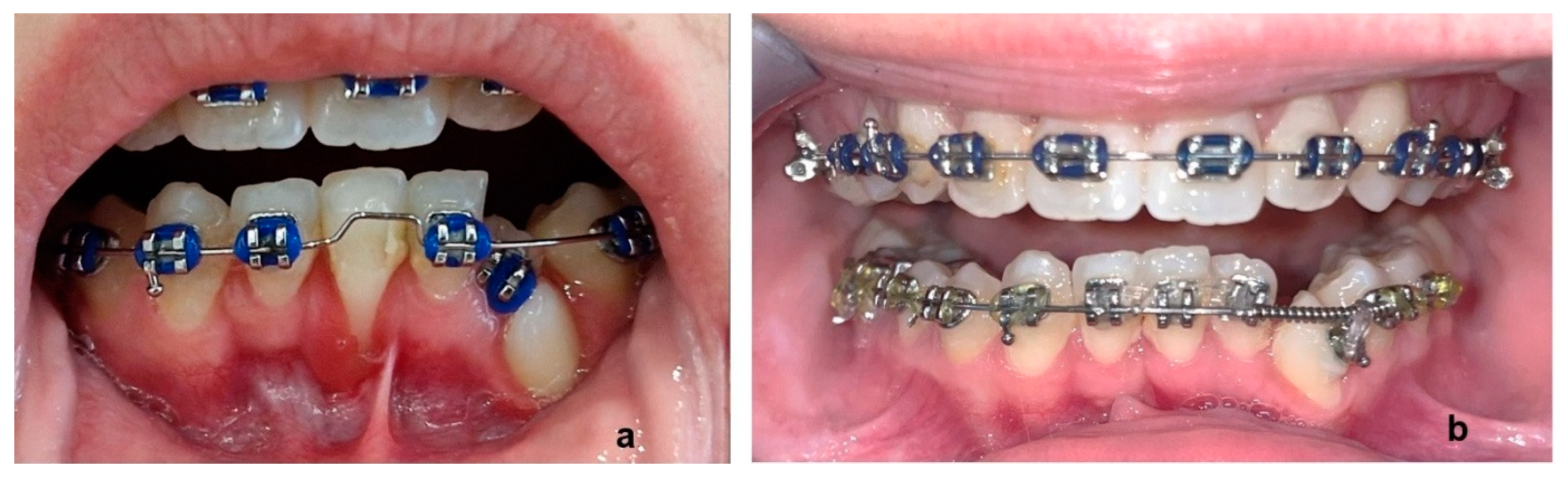
The closed eruption technique was chosen. Lower canines and the two incisors were surgically exposed, and a gold chain apparatus was bonded on each one (
Figure 7a). A 0.17 × 0.25 SS wire, leaning on the buccal tubes of the lower molar bands, was properly fitted around them and on the lingual side of the lower teeth crown (
Figure 7b). This was chosen in order to suspend (in conjunction with the labial brackets and wires) either an elastic chain or a super-elastic wire from the certain wire in order to facilitate traction of the impacted teeth (
Figure 7c). This was performed for 43, 42, 32, and 33 separately one after the other, in that order.
After 43, 42, 32 were brought into the lower arch, it was decided to extract 81, which presented a significant recession (
Figure 8a) of the labial gum due to inclination and the general surcharge that it was subjected during mechanotherapy. In this way, additional space was gained for 32 and 33 (
Figure 8b).
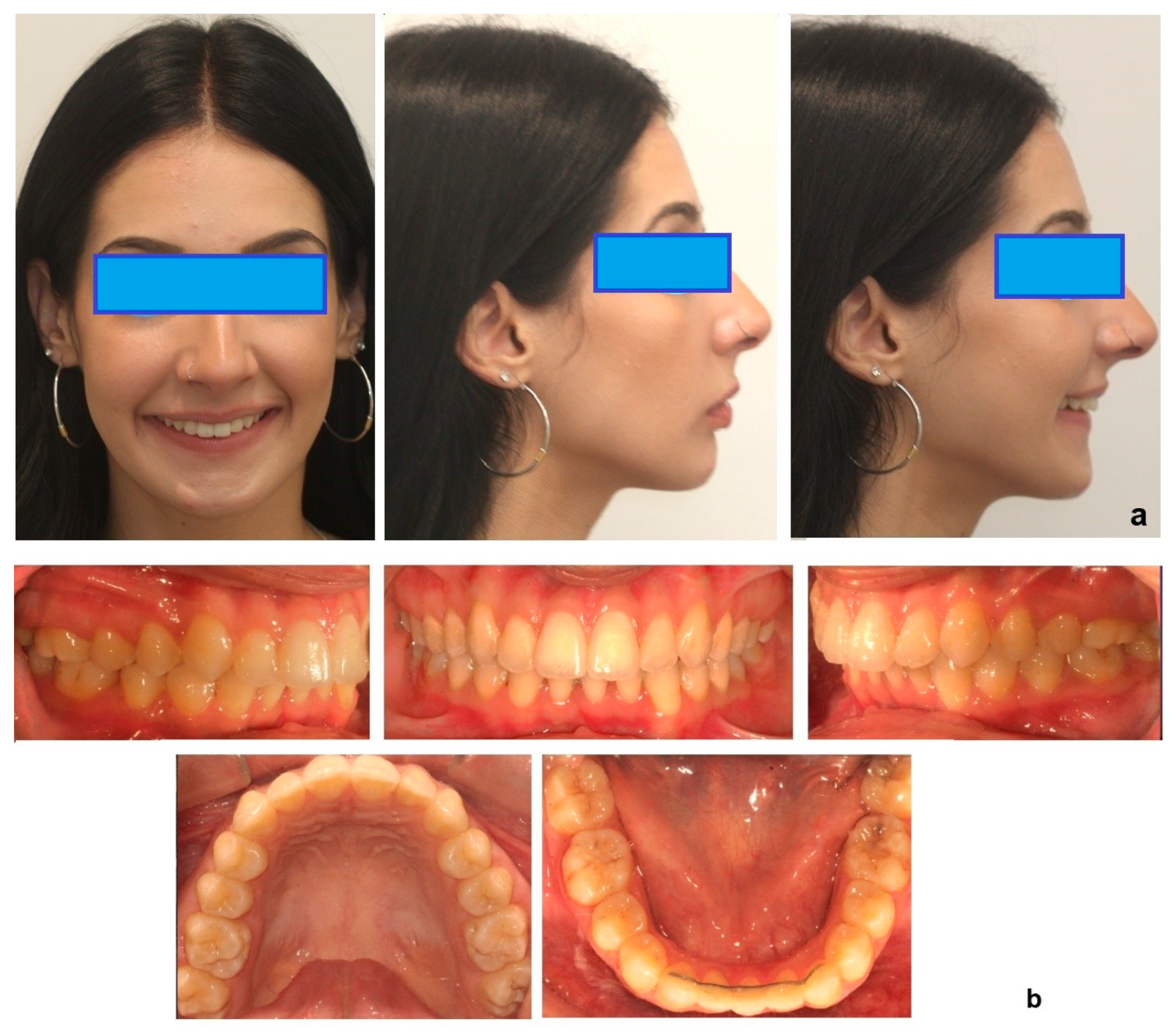
At the end of treatment, the impacted teeth were restored to their proper place. As only three incisors were present in the lower jaw, inter-proximal reduction was performed in the upper arch in the anterior region, in order to deal with the increased overjet.
The periodontal status of the patient at the beginning of the treatment with fixed appliances was sound and no swollen or bleeding gums were detected, nor pathological probing depths. Some signs of mild gingivitis were detected later on, mainly in the incisor area of the lower arch, when multiple wires were fitted during orthodontic traction of unerupted teeth. This was addressed by regular dentist care. After extraction of 81 and space closure, the periodontal status of the region significantly improved.
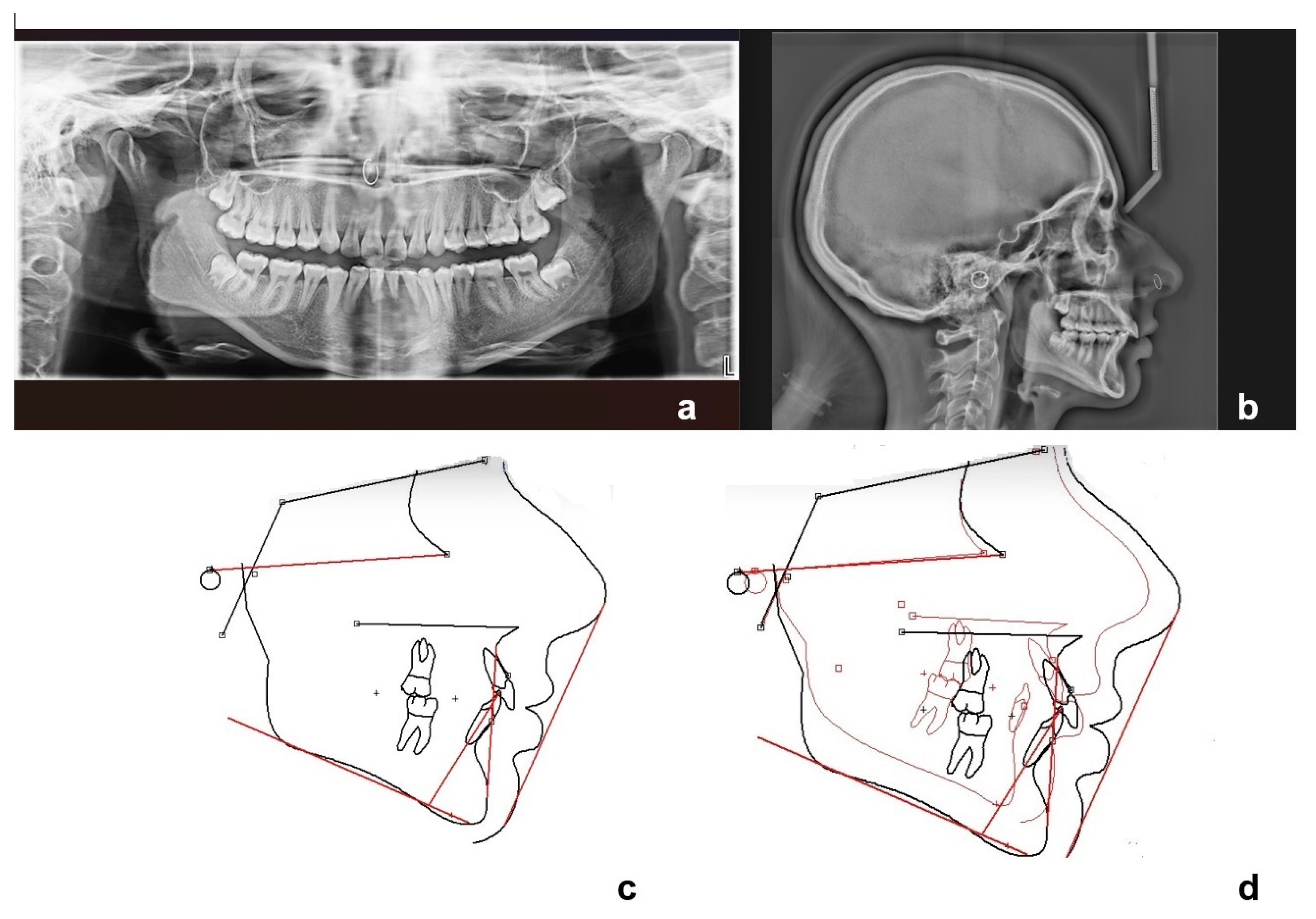
Final panoramic (
Figure 9a) and lateral cephalometric X-ray (
Figure 9b) and tracing (
Figure 9c), as well as before and after treatment tracing superimposition (
Figure 9d), are presented in
Figure 9. Skeletal Class II relationship was reduced (ANB was calculated 5° at the end of therapy from 8° at the beginning (
Table 2)), while Class I molar and canine relationships were achieved (
Figure 10 and
Figure 11). In
Figure 12, a graphical abstract of the timeline of the steps that were followed in the treatment of this DTE case is presented.
After removal of the appliances, a fixed retainer was fitted in the lower arch (3–3) and Essix retainers were provided for the upper and lower arch. The patient was advised to wear the retainers at nighttime and follow-up bimonthly appointments were scheduled. As the case has just finished, only the first follow-up visit has taken place. A strict oral hygiene routine of thorough everyday brushing, flossing, and regular visits for dental care was prescribed. When stability of the result is recorded, longer follow-up intervals will be attained.
3. Discussion
DTE presents the highest prevalence among the aberrations in timing of tooth eruption [
4], and it is one of the more serious issues that can arise during the mixed dentition period, causing considerable concern for children and their parents [
9]. The eruption of teeth in proper sequence and on time is essential to decide the appropriate methodology implemented during orthodontic treatment and the optimal timing of the therapeutic procedures [
4,
9]. DTE may be the primary or the only indication of a local or systemic pathologic disorder [
15]. A delay in eruption can have a substantial impact on accurate diagnosis and treatment planning, as well as the duration of overall treatment for the orthodontic patient. Thus, DTE is a serious clinical issue that can directly affect a patient’s proper orthodontic and general health care [
9]
.Several research findings suggest that dental development and eruption of permanent teeth in patients with tooth agenesis may deviate when compared with the general population [
20,
21,
22,
23,
24]. It appears that tooth agenesis (hypodontia) has been associated with a delay of approximately 1.51 years in tooth development [
21,
22]. Therefore, it is essential for clinicians to be aware that patients with tooth agenesis may experience an overall delay in dental development, which appears to be more prominent in severely affected patients. In some cases, it may be necessary to defer treatment decisions for 1 to 2 years to establish whether teeth are truly missing or present with significant delay [
21].
The diagnosis of DTE is based on two fundamental parameters: (a) estimated time of tooth eruption (chronologic age) based on population studies, and (b) biologic eruption, which is determined by the rate of root development. Suri et al. proposed a diagnostic algorithm that would enable the clinician to perform an accurate and thorough orthodontic diagnosis of the patient with DTE [
4]. The first step includes the patient’s age and clinically visible dentition examination. Chronologic DTE is defined as the eruption time that exceeds two SDs from the mean predicted eruption time for a specific tooth (chronologic norm of eruption). This should be followed by a second step of excluding any local and systemic factors for a possible mechanical impairment of the eruption. In addition, it is crucial to determine any potential factor that interferes with tooth development. Thus, the clinician is urged to consider certain diseases that lead to defects of tooth structure, size, shape, and color. In case none of such factors have impacted tooth development, the third step is to assess the patient’s dental age, as demonstrated by root formation. Normal biologic eruption initiates when the dental root reaches around 2/3 of its final length. In delayed biologic eruption, although 2/3 or more of the dental root has developed, the tooth has not erupted. Therefore, a patient presenting with chronologic delayed eruption could merely be of a dental age that does not meet the standards (root length is less than 2/3) [
4].
In the presented case, the lower lateral incisors and canines had their roots formatted beyond 2/3 at the patient’s age of 11 years old and no other mechanical impairment for their eruption was recorded. We should underline the altered shape of the roots of 11, 12, 22 that had, however, normally erupted, the congenitally missing of lower central incisors, and the decreased size of the root of 42 as it was recorded in the CBCT examination.
Lately, CBCT is a valuable diagnostic medium that can determine not only the stages of tooth development and the precise location of deciduous and erupting permanent teeth, but also the amount of bone adjacent to developing permanent teeth and root resorption of deciduous teeth [
4,
9]. Evidence suggests that all impacted teeth should be regarded as having an increased risk of external apical root resorption [
25]. Additionally, a causative association of delayed tooth eruption with pulp necrosis, ankylosis, and external apical root resorption has been reported [
25]. This reflects the important contribution of CBCT assessment in the diagnostic process of such cases, as it was indeed utilized in this treatment procedure.
In case of delayed tooth eruption based on both dental and chronologic ages (mean ± 2 SD), there is a low probability that the permanent tooth will emerge without orthodontic intervention [
4,
9]. An impacted tooth no longer has the capacity to spontaneously erupt once the root apex has been fully formed [
26,
27]. In such an event, the impacted permanent tooth should be surgically exposed and bonded with an orthodontic appliance to guide it into the dental arch. Orthodontic treatment duration may be extended in patients with DTE while waiting for the teeth to erupt. If anterior teeth are affected, DTE may have psychological consequences for the patient. Hence, sufficient space for the emerging tooth should be preserved by utilizing an esthetic pontic, and any systemic problems should be reassessed [
4,
9]. In this case, such pontics were utilized for 33 and 43 before their traction to appropriate places in the arch. Alternative treatment options would be the surgical extraction of all the impacted teeth or some of them (31–41) and the prosthetic rehabilitation of the patient with dental implants. However, extractions of all impacted teeth would have a negative impact on bone level in that area of the arch and a bone graft should be considered before the final fixed prosthesis. On the other hand, the parents of the patient were informed about the possibility of ankylosis of the impacted teeth. A decision was made to attempt the orthodontic traction solution based on the patient’s age since the probability of ankylosis was low in a growing patient [
28]. A prosthesis would be considered if some of the teeth failed to be orthodontically moved to their proper place in the arch.
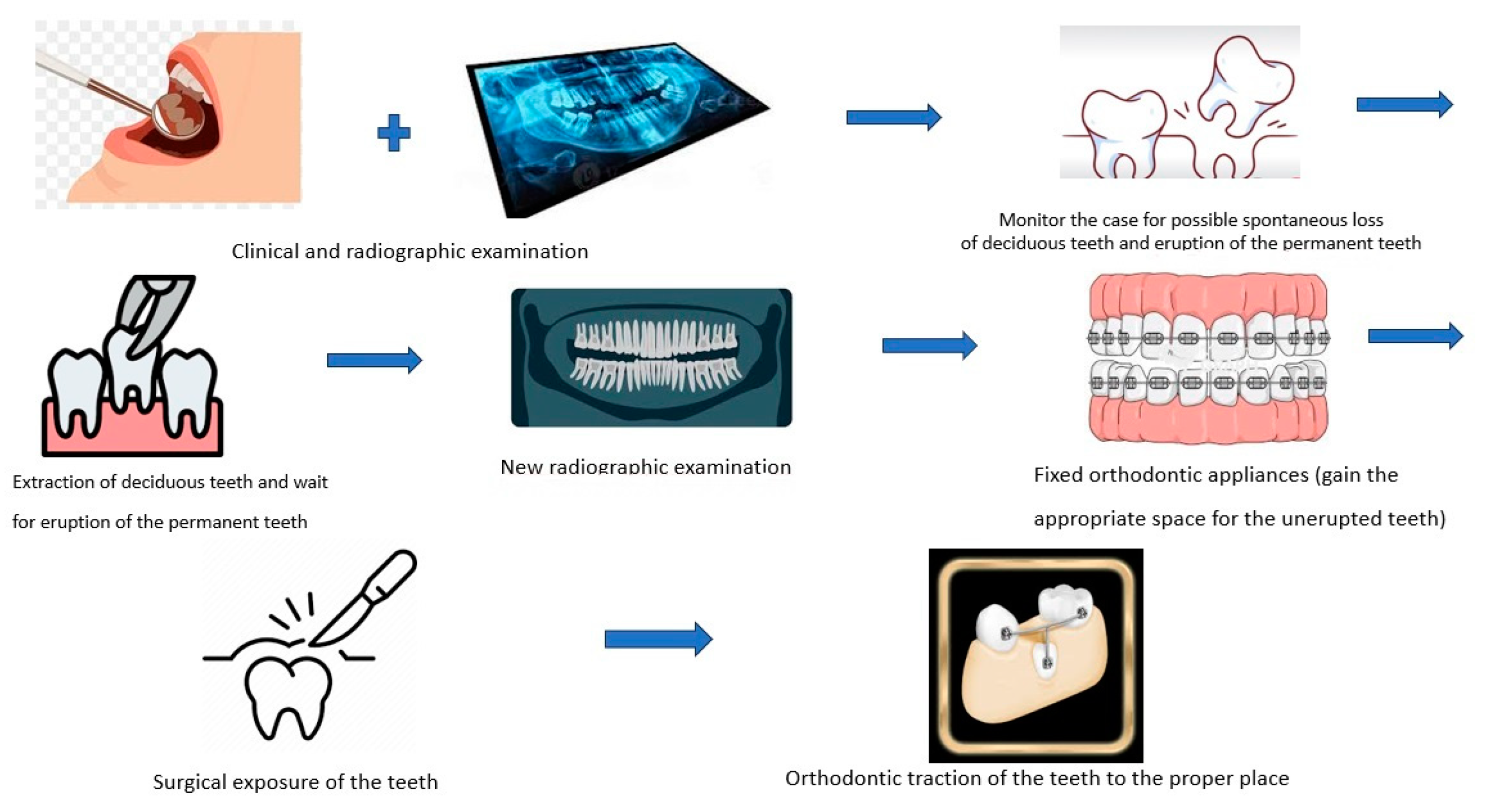
This case report presents the specific procedures that were followed in this patient, and though a certain timetable action is recommended (
Figure 12), limitations exist, based on individual responses. In this case of multiple impacted teeth, the orthodontic traction procedure involved enhancing anchorage by placing a 0.17 × 0.25 SS wire on the lingual side of the lower teeth alongside the labial appliances and the esthetic pontics that were fitted. This had a serious impact on the patient’s oral hygiene as a greater effort and often dental care was needed. Even the social life of the patient was affected as the treatment time was expanded. Possible gingival recession around the orthodontically erupted teeth is a common implication. Fortunately, in this case such an event was avoided, and the final result was not compromised. Long-term and frequent follow-up visits of such cases should contribute to the evaluation and preservation of the results.