Usage of Chelating Gels in Root Canal Preparation: A Survey of Australian Clinicians
Abstract
1. Introduction
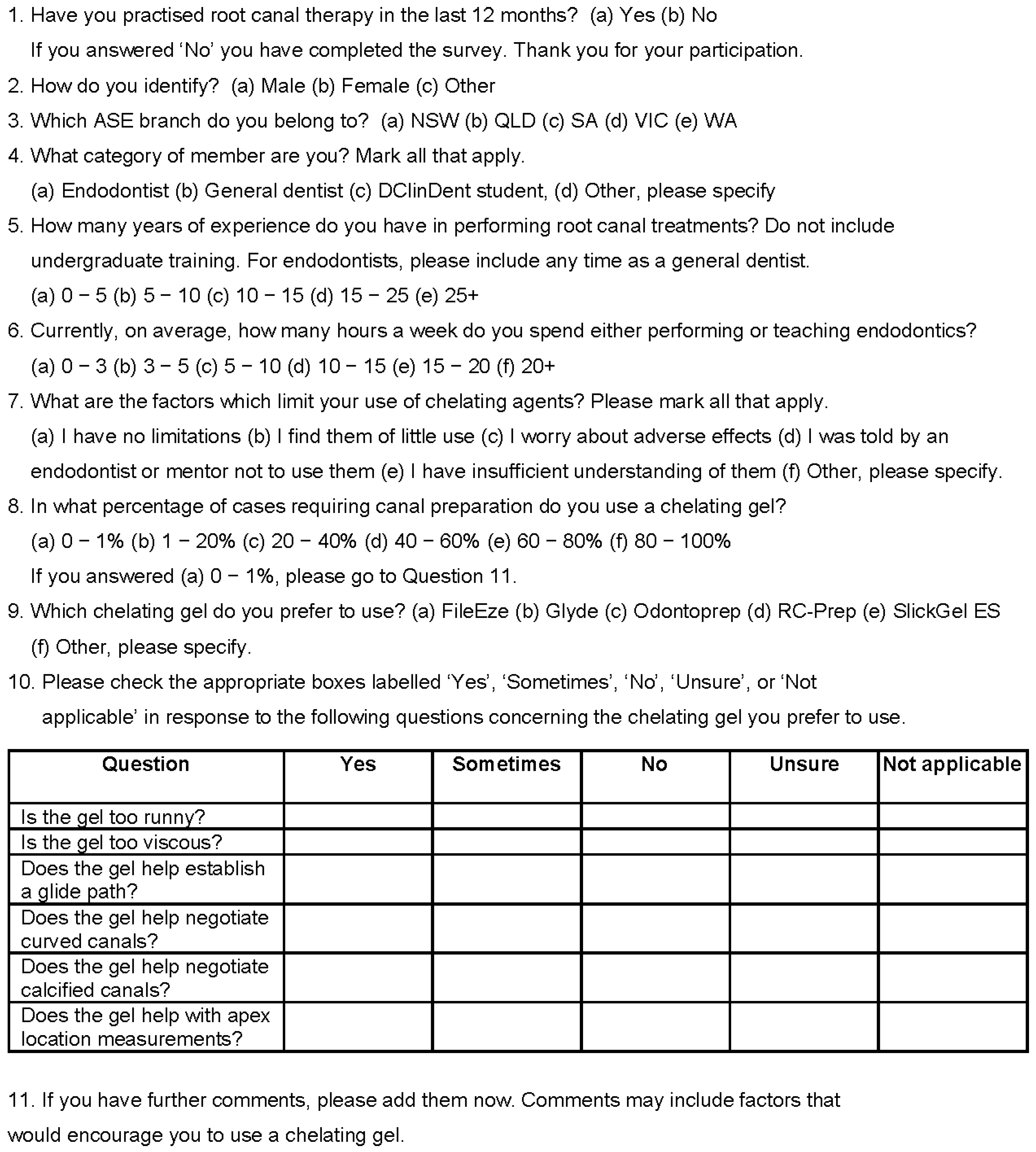
2. Materials and Methods
2.1. Survey Administration and Design
2.2. Statistical Analysis
3. Results
3.1. Reponse
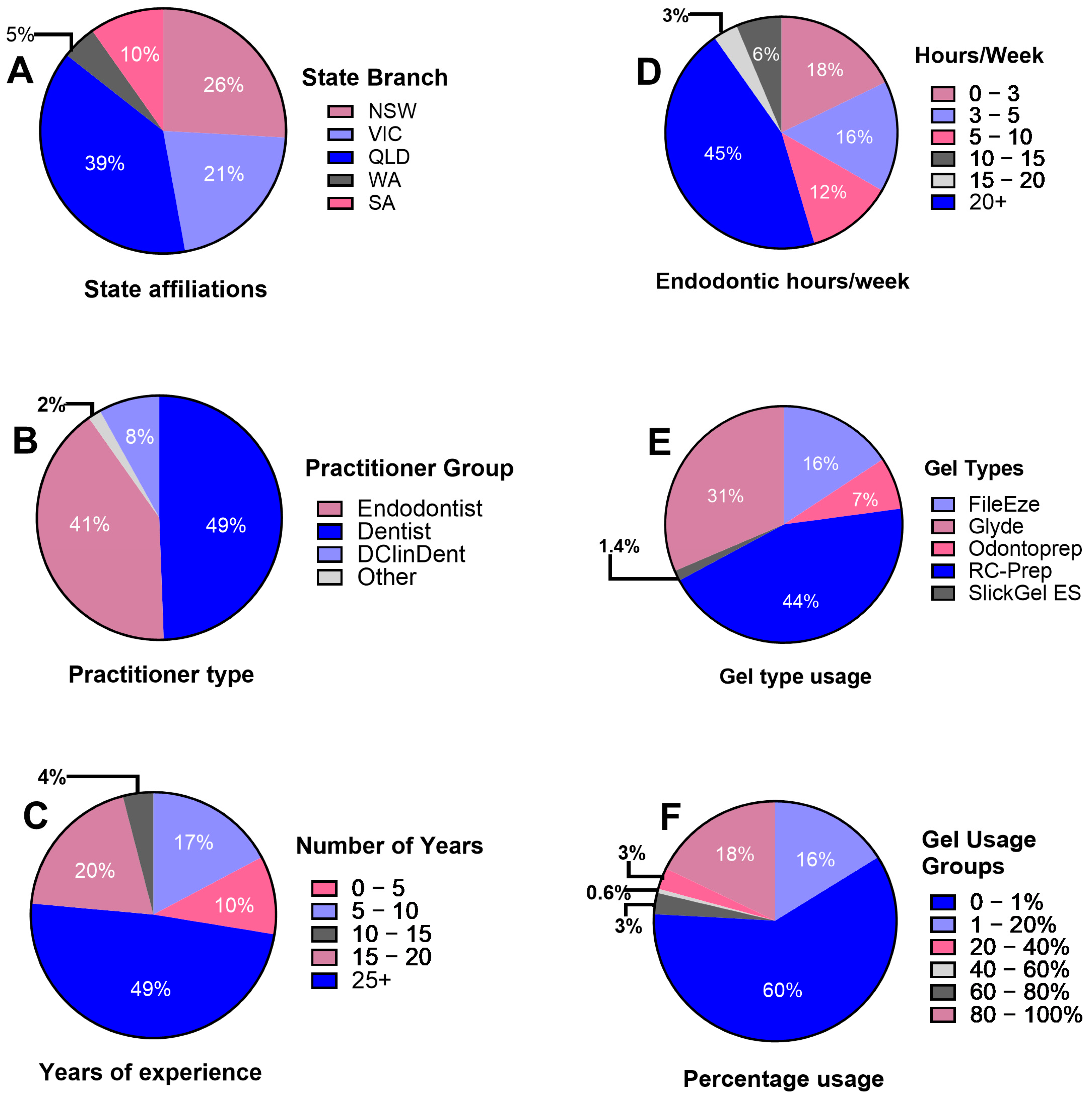
3.2. Respondent Demographics, Practicing Characteristics, Experience, and Chelating Gel Usage Characteristics
3.3. Chelaing Gel Usage Patterns
3.4. Limitations on the Use of Chelating Agents
3.5. Satisfaction with Gel Properties and Usefulness
3.6. Comments
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Blackman, A.; Bottle, S.; Schmid, S.; Mocerino, M.; Wille, U. Chemistry, 5th ed.; John Wiley & Sons: Milton, Australia, 2023; pp. 632–635. [Google Scholar]
- Nygaard-Ostby, B. Chelation in root canal therapy. Ethylendiamine tetraacetic acid for cleansing and widening of root canals. Odontol. Tidskr. 1957, 65, 3–11. [Google Scholar]
- Haapasalo, M.; Shen, Y.; Wang, Z.; Gao, Y. Irrigation in endodontics. Br. Dent. J. 2014, 216, 299–303. [Google Scholar] [CrossRef] [PubMed]
- Chandler, N.; Chellappa, D. Lubrication during root canal treatment. Aust. Endod. J. 2019, 45, 106–110. [Google Scholar] [CrossRef]
- Chen, G.; Chang, Y.-C. Effects of liquid-and paste-type EDTA on smear-layer removal during rotary root-canal instrumentation. J. Dent. Sci. 2011, 6, 41–47. [Google Scholar] [CrossRef]
- Peters, O.A.; Boessler, C.; Zehnder, M. Effect of liquid and paste-type lubricants on torque values during simulated rotary root canal instrumentation. Int. Endod. J. 2005, 38, 223–229. [Google Scholar] [CrossRef]
- Qian, W.; Shen, Y.; Haapasalo, M. Quantitative analysis of the effect of irrigant solution sequences on dentin erosion. J. Endod. 2011, 37, 1437–1441. [Google Scholar] [CrossRef]
- Hülsmann, M.; Heckendorff, M.; Schäfers, F. Comparative in-vitro evaluation of three chelator pastes. Int. Endod. J. 2002, 35, 668–679. [Google Scholar] [CrossRef]
- Orstavik, D. Essential Endodontology: Prevention and Treatment of Apical Periodontitis; John Wiley & Sons: Hoboken, NJ, USA, 2019; p. 294. [Google Scholar]
- Peters, O.A.; Arias, A. Shaping, disinfection, and obturation for molars. In The Guidebook to Molar Endodontics; Peters, O., Ed.; Springer: Berlin/Heidelberg, Germany, 2017; pp. 133–167. [Google Scholar]
- Kim, H.J.; Park, S.J.; Park, S.H.; Hwang, Y.C.; Yu, M.K.; Min, K.S. Efficacy of flowable gel-type EDTA at removing the smear layer and inorganic debris under manual dynamic activation. J. Endod. 2013, 39, 910–914. [Google Scholar] [CrossRef] [PubMed]
- Maillefer Instruments Holding. Glyde File Prep Safety Data Sheet, Version 4.2. Available online: https://gerl-dental.de/media/pdf/81/42/c2/Glyde_File_Prep_20221215_GB.pdf (accessed on 25 May 2024).
- Tokuda, M.; Kawakami, Y.; Morimoto-Yamashita, Y.; Torii, M. Subcutaneous emphysema caused by sodium hypochlorite plus RC-prep. Open J. Stomatol. 2014, 4, 527–532. [Google Scholar] [CrossRef]
- Dutner, J.; Mines, P.; Anderson, A. Irrigation trends among american association of endodontists members: A web-based survey. J. Endod. 2012, 38, 37–40. [Google Scholar] [CrossRef]
- Virdee, S.S.; Ravaghi, V.; Camilleri, J.; Cooper, P.; Tomson, P. Current trends in endodontic irrigation amongst general dental practitioners and dental schools within the United Kingdom and Ireland: A cross-sectional survey. Br. Dent. J. 2020, 1–7. [Google Scholar] [CrossRef]
- Savani, G.M.; Sabbah, W.; Sedgley, C.M.; Whitten, B. Current trends in endodontic treatment by general dental practitioners: Report of a United States national survey. J. Endod. 2014, 40, 618–624. [Google Scholar] [CrossRef]
- Mikheikina, A.; Novozhilova, N.; Polyakova, M.; Sokhova, I.; Mun, A.; Zaytsev, A.; Babina, K.; Makeeva, I. Knowledge, attitude, and practice towards chelating agents in endodontic treatment among dental practitioners. Dent. J. 2023, 11, 156. [Google Scholar] [CrossRef] [PubMed]
- Bartlett, J.; Kotrlik, J.; Higgins, C. Organizational research: Determining appropriate sample size in survey research. Inf. Technol. Learn. Perform. J. 2001, 19, 43. [Google Scholar]
- Beasley, T.M.; Schumacker, R.E. Multiple regression approach to analyzing contingency tables: Post hoc and planned comparison procedures. J. Exp. Educ. 1995, 64, 79–93. [Google Scholar] [CrossRef]
- Bulmer, J.A.; Currell, S.D.; Peters, C.I.; Peters, O.A. Endodontic knowledge, attitudes and referral patterns in Australian general dentists. Aust. Dent. J. 2022, 67 (Suppl. S1), S24–S30. [Google Scholar] [CrossRef]
- Cheung, M.C.; Peters, O.A.; Parashos, P. Global survey of endodontic practice and adoption of newer technologies. Int. Endod. J. 2023, 56, 1517–1533. [Google Scholar] [CrossRef]
- Peters, O.A.; Rossi-Fedele, G.; George, R.; Kumar, K.; Timmerman, A.; Wright, P.P. Guidelines for non-surgical root canal treatment. Aust. Endod. J. 2024. online ahead of print. [Google Scholar] [CrossRef]
- Duncan, H.F.; Kirkevang, L.L.; Peters, O.A.; El-Karim, I.; Krastl, G.; Del Fabbro, M.; Chong, B.S.; Galler, K.M.; Segura-Egea, J.J.; Kebschull, M. Treatment of pulpal and apical disease: The European Society of Endodontology (ESE) S3-level clinical practice guideline. Int. Endod. J. 2023, 56 (Suppl. S3), 238–295. [Google Scholar] [CrossRef]
- American Association of Endodontists. Treatment Standards: Executive Summary. Available online: https://www.aae.org/specialty/wp-content/uploads/sites/2/2019/11/EndoCompetency_2019.pdf (accessed on 10 July 2024).
- Keyes, K.M.; Utz, R.L.; Robinson, W.; Li, G. What is a cohort effect? Comparison of three statistical methods for modeling cohort effects in obesity prevalence in the United States, 1971–2006. Soc. Sci. Med. 2010, 70, 1100–1108. [Google Scholar] [CrossRef]
- Ju, X.; Spencer, A.J.; Brennan, D.S. Dentist age, period and cohort effects on provision of dental services in Australia: 1983-84 to 2009-10. Community Dent. Oral Epidemiol. 2017, 45, 242–250. [Google Scholar] [CrossRef] [PubMed]
- Kirkwood, B.; Sterne, J. Essential Medical Statistics, 2nd ed.; Blackwell Science: Carlton, Australia, 2003; p. 171. [Google Scholar]
- Premier Dental. RC-Prep®. Available online: https://www.premierdentalco.com/product/endo/chemo-mechanical-preparation/rc-prep/ (accessed on 18 June 2024).
- Clarkson, R.M.; Podlich, H.M.; Moule, A.J. Influence of ethylenediaminetetraacetic acid on the active chlorine content of sodium hypochlorite solutions when mixed in various proportions. J. Endod. 2011, 37, 538–543. [Google Scholar] [CrossRef]
- Wright, P.P.; Cooper, C.; Kahler, B.; Walsh, L.J. From an assessment of multiple chelators, clodronate has potential for use in continuous chelation. Int. Endod. J. 2020, 53, 122–134. [Google Scholar] [CrossRef] [PubMed]
- Zehnder, M.; Schmidlin, P.; Sener, B.; Waltimo, T. Chelation in root canal therapy reconsidered. J. Endod. 2005, 31, 817–820. [Google Scholar] [CrossRef] [PubMed]
- Ultradent Products. Safety Data Sheet File-Eze. Available online: https://www.ultradent.com/Resources/GetSds?key=21-001-09.82735475-en-gb (accessed on 25 May 2024).
- Utradent Products. File-Eze™EDTA Chelating & Filing Lubricant Instructions for Use. Available online: https://assets.ctfassets.net/wfptrcrbtkd0/53ba3c2e-8e18-4e91-a9ab-c0d7d03671bf/0bbc938116f42cd0532c93bb5b1a7953/File-Eze-EDTA-File-Lubricant-IFU-10187-UAR10.pdf (accessed on 18 June 2024).
| (A) | ||||||||
| Gel Usage Categories | ||||||||
| Clinician Type | 0–1% | 1–20% | 20–40% | 40–60% | 60–80% | 80–100% | Total | |
| Endodontist | Count | 53 | 6 | 1 | 0 | 1 | 10 | 71 |
| % of endodontists | 74.60% | 8.50% | 1.40% | 0.00% | 1.40% | 14.10% | 100% | |
| Dentist | Count | 39 | 19 | 3 | 1 | 4 | 20 | 86 |
| % of dentists | 45.30% | 22.10% | 3.50% | 1.20% | 4.70% | 23.30% | 100% | |
| Resident | Count | 12 | 1 | 0 | 0 | 0 | 1 | 14 |
| % of residents | 85.70% | 7.10% | 0.00% | 0.00% | 0.00% | 7.10% | 100% | |
| Other | Count | 0 | 2 | 1 | 0 | 0 | 0 | 3 |
| % of others | 0.00% | 66.70% | 33.30% | 0.00% | 0.00% | 0.00% | 100% | |
| Total | Count | 104 | 28 | 5 | 1 | 5 | 31 | 174 |
| % of clinician type | 59.80% | 16.10% | 2.90% | 0.60% | 2.90% | 17.80% | 100% | |
| (B) | ||||||||
| Gel Usage Categories | ||||||||
| 0–1% | 1–80% | 80–100% | Total | |||||
| Clinician Type | Endodontist | Count | 53 | 8 | 10 | 71 | ||
| Adjusted residual | 3.71 | −3.02 | −1.45 | |||||
| p value | 0.0002 * | 0.0025 * | 0.1471 | |||||
| Dentist | Count | 39 | 27 | 20 | 86 | |||
| Adjusted residual | −3.71 | 3.02 | 1.45 | |||||
| p value | 0.0002 * | 0.0025 * | 0.1471 | |||||
| Total | Count | 92 | 35 | 30 | 157 | |||
| Gel Usage Categories | ||||||
|---|---|---|---|---|---|---|
| 0–1% | 1–80% | 80–100% | Total | |||
| Years of Endodontic Experience | 0–25 Years | Count | 60 | 20 | 9 | 89 |
| % with 0–25 years | 67.4% | 22.5% | 10.1% | 100% | ||
| Adjusted residual | 2.10 | 0.02 | −2.72 | |||
| p value | 0.0357 | 0.9840 | 0.0065 * | |||
| 25+ Years | Count | 44 | 19 | 22 | 85 | |
| % with 25+ years | 51.8% | 22.4% | 25.9% | 100% | ||
| Adjusted residual | −2.10 | −0.02 | 2.72 | |||
| p value | 0.0357 | 0.9840 | 0.0065 * | |||
| Total | Count | 104 | 39 | 31 | 174 | |
| % of years of experience | 59.8% | 22.4% | 17.8% | 100% | ||
| Yes | Sometimes | No | Unsure | N/A | Total | |
|---|---|---|---|---|---|---|
| Is the gel too runny? | 0 (0%) | 8 (12%) | 58 (85%) | 1 (1%) | 1 (1%) | 68 |
| Is the gel too viscous? | 5 (7%) | 16 (23%) | 47 (68%) | 0 (0%) | 1 (1%) | 69 |
| Does the gel help establish a glide path? | 27 (39%) | 25 (36%) | 6 (9%) | 9 (13%) | 2 (3%) | 69 |
| Does the gel help negotiate curved canals? | 18 (26%) | 21 (30%) | 14 (20%) | 12 (17%) | 4 (6%) | 69 |
| Does the gel help negotiate calcified canals? | 20 (29%) | 24 (34%) | 14 (20%) | 11 (16%) | 1 (1%) | 70 |
| Does the gel help with apex location measurements? | 3 (4%) | 9 (13%) | 32 (46%) | 16 (23%) | 10 (14%) | 70 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wright, P.P.; Diamond, E.S.; Peters, O.A. Usage of Chelating Gels in Root Canal Preparation: A Survey of Australian Clinicians. Oral 2024, 4, 315-324. https://doi.org/10.3390/oral4030026
Wright PP, Diamond ES, Peters OA. Usage of Chelating Gels in Root Canal Preparation: A Survey of Australian Clinicians. Oral. 2024; 4(3):315-324. https://doi.org/10.3390/oral4030026
Chicago/Turabian StyleWright, Patricia P., Elise S. Diamond, and Ove A. Peters. 2024. "Usage of Chelating Gels in Root Canal Preparation: A Survey of Australian Clinicians" Oral 4, no. 3: 315-324. https://doi.org/10.3390/oral4030026
APA StyleWright, P. P., Diamond, E. S., & Peters, O. A. (2024). Usage of Chelating Gels in Root Canal Preparation: A Survey of Australian Clinicians. Oral, 4(3), 315-324. https://doi.org/10.3390/oral4030026







