Abstract
Background: The influence of medical and dental factors on jaw clicking within the South Australian population remains unexplored, and there is a lack of research on the impact of occlusal therapy on dynamic jaw movement parameters in this population. Purpose: This study investigated the potential significant associations between specific aspects of patient histories, occlusal therapy, and self-reported or observed jaw clicking in a population from the state of South Australia. Methods: Seventy individuals aged 18 to 65 participated in a cross-sectional study. Data collection included comprehensive medical, social, and dental histories, followed by evaluations of jaw function. Twenty-six out of the seventy individuals reported jaw clicking. Electrognathography assessed maximum mouth opening, surface electromyography evaluated masticatory muscle function, and joint vibration analysis measured individual joint vibration amplitudes and integrals. Logistic regression models analysed overall variable effects, while sub-models focused on predictors related to occlusal therapy, specifically orthodontic intervention. Independent t-tests and Mann–Whitney U tests compared jaw functions between participants who received occlusal therapy and those who did not. Results: The number of third molars extracted, vitamin D deficiency, and self-reported mental health disorders (R2 = 0.414, p = 0.048) emerged as significant predictors for jaw clicking. Factors associated with occlusal therapy showed no significant association with jaw clicking (R2 = 0.59, p = 0.027). Furthermore, there were no significant differences observed in mouth opening (t-stat = −0.439, p = 0.662), muscle activity, and joint vibration analysis between participants who underwent occlusal therapy and those who did not. Conclusions: Within the selected study population and limited sample size, the number of third molars extracted, vitamin D deficiency, and self-reported mental health disorders were associated with jaw clicking.
1. Introduction
Occlusal therapy encompasses any dental procedure that alters the alignment of the teeth when in occlusion [1]. Jaw movement and TMJ function are influenced by a multitude of factors, including genetics, heredity, and environmental variables [2]. Dental and medical interventions, such as occlusal therapy following restorative and orthodontic procedures, also contribute to alterations in jaw movement kinematics [1]. The complexity of jaw movement, coupled with the diverse range of variables at play, including parafunctional habits, makes it challenging to identify consistent trends [3]. For example, orthodontic malocclusion and alterations in masticatory muscle functions have been reported to produce variations in mandibular motion, adding complexity to the relationship. However, an objective quantitative assessment of medical history in conjunction with analyses of hard and soft tissue components of the TMJ complex was not possible until the advent of modern deep learning technologies [3,4,5].
1.1. The Current Knowledge on Occlusal Therapy
Previous research has explored the impact of occlusal therapy [1], particularly that produced by orthodontic treatment, on jaw motion, especially in adolescents with crossbites, where treatment led to improved masticatory efficiency [6]. However, there is a need to expand our knowledge beyond a pure functional association to incorporate modern-day factors that receive concurrent therapeutic intervention, such as those treating hormonal and mental health conditions in adulthood. These contemporary influences can potentially predispose individuals to parafunctional habits, affecting jaw motion in conjunction with altered psychological states or medication use [7]. Despite the connection between symptoms of temporomandibular dysfunction syndrome (TMDS), parafunctional habits, orthodontic management, and psychological well-being among adolescents, a quantitative assessment of their combined impact on maximum mouth opening during adulthood remains largely unexplored [8]. Recent research on this subject is limited, and further investigation is required into variables such as parafunctional habits, interventive exodontia, mouth opening, and TMJ function in adulthood for occlusal therapy [9]. Poorly adapted occlusion or relapse following orthodontic treatment may predispose patients to bruxism and clenching [10]. This, alongside existing parafunctional habits, can introduce dental rearrangement that is also thought to be a key variable responsible for temporomandibular joint dysfunction with the possibility of jaw clicking [10,11,12].
1.2. Assessment of Jaw Function
Jaw function is often quantified by assessing the static skeletal relationships of the maxilla and mandible, alongside scored Indices of Orthodontic treatment needs [13,14]. Dynamic assessments involve evaluating jaw functions during the movement of the jaws and incorporate soft tissue parameters, such as muscle activity during mouth opening and chewing, along with mandibular hard tissue translation, most frequently during vertical displacements like mouth opening [15]. To quantitatively assess mandibular function during movement, certain parameters such as maximum mouth opening (MMO), masticatory muscle activities, and independent joint vibration integrals and amplitude values exceeding 300 Hz can be measured [16,17]. Clinically, while definitive diagnoses of the TMJ can only be made through magnetic imaging, these parameters can aid in the preliminary non-invasive guidance towards considering possible temporomandibular disorders (TMDs) using the Piper’s classification system [16].
Jaw clicking is typically associated with disruptions in the normal functioning of the temporomandibular joint (TMJ) complex that can affect jaw movement in varying degrees [10]. It is one of the very few symptoms that can be both observed and self-reported without necessitating complex imaging modalities and is therefore free from false negative assessments. These clicks can range from subtle ‘cracking’ or audible ‘popping’ sounds during jaw movement and ‘crunching’ noises during activities like chewing. Incidences of self-reported or clinically observed jaw clicking were therefore used as output variables when classifying and evaluating the predictor variables.
1.3. Study Objectives
The present study aimed to explore the associative relationships of medical, social, and dental histories; mouth opening and TMJ complex dynamic function; occlusal therapy through orthodontic treatment; and previous third molar extractions to identify factors accompanying the clinical presentation of jaw clicking in South Australian residents with the goal of generating a prediction model.
Due to a lack of access to large-scale national data, it was imperative to select an output variable that could be easily assessed and relatively free from false positive assessments. Jaw clicking was therefore considered an appropriate choice for the output variable. Additionally, a second aim was developed: to compare jaw movement functional analyses across participants who reportedly received orthodontic treatment during earlier years and compare them to participants who received no such treatment. The goal was to identify whether any significant differences existed between the two groups in a cross-sectional retrospective evaluation.
The null hypothesis stated that there would be no significant predictor variables associated with jaw clicking in the selected population. It was also hypothesised that occlusal therapy would have no significant influence on jaw movement parameters.
2. Materials and Methods
The cross-sectional study was conducted as part of a project approved by the institution’s Human Research Ethics Committee (H-2022-185). For the current study, a large effect size of d = 0.80 (Cohen’s D) [18], α = 0.05, and power = 0.90 were considered. It was estimated that a minimum sample size of 56 participants would be required for this proactive evaluation. Considering logistical constraints, an additional 14 participants were planned to be recruited to accommodate dropouts and ensure the generation of high-quality signal data. The final sample size was of 70 participants. However, a larger participant population would have been desirable for a more descriptive predictive model.
2.1. Eligibility Criteria
Eligibility criteria ensured inclusion of individuals with most of their natural permanent dentition, allowing for a maximum of one missing space in each quadrant. If a first molar was absent, all other teeth in the arch had to be present. Exclusion criteria comprised individuals with long-span edentulous arches, shortened dental arches [19], retained deciduous molars, and those with two or more fixed partial dentures or dental crowns.
Perceived symptoms or existing medical conditions were not used as exclusion criteria to promote participant randomisation and prevent accidental omission of individuals exhibiting clinical signs of clicking but not self-reporting the condition [20]. Although existing medical conditions alone were not grounds for exclusion, given the study’s advertisement throughout the institution’s clinical research facility, it was deemed important to document participants’ prescribed medications. The invitation to participate encouraged individuals who were curious or concerned about their jaw movements to observe these movements on screen in real time while performing specific tasks. This ensured adequate participant engagement and a clear understanding of what was expected of them, thus helping to avoid procedural errors that could introduce biases.
On the day of data collection, eligibility screening was conducted, and written consent was obtained from participants. They were then allowed to view and interact with the data being collected to ensure accuracy in self-reported details. Data collection concluded after reaching 70 participants.
After obtaining written consent, participants’ histories were collected, encompassing information regarding jaw clicking, lockout, jaw pain, and parafunctional habits. Detailed accounts of orthodontic treatment and restorative and endodontic statuses, as well as comprehensive medical histories spanning the past 10 years, were obtained.
2.2. Jaw Movement Analyses
Subsequently, participants underwent a series of jaw movement analyses (Figure 1). These analyses included the following:
- An electrognathography test (J-T 3D; BioResearch Associates Inc., Brown Deer, WI, USA) to assess range of motion.
- Surface electromyography (BioEMG III, BioResearch Associates Inc., Brown Deer, WI, USA) to record masticatory muscle activity during mouth opening and closing.
- Joint vibration analysis (JVA; BioResearch Associates Inc., Brown Deer, WI, USA) to evaluate TMJ function, producing mean vibration integrals and amplitudes above 300 Hz to assess joint complex quality during opening [16,21].
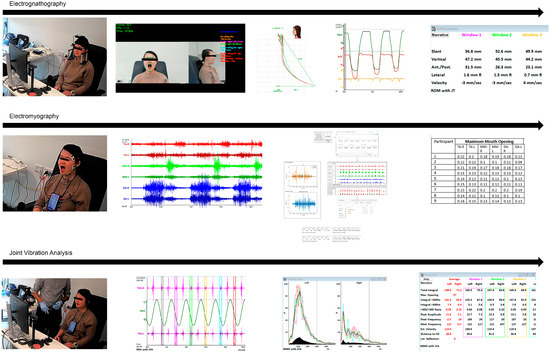
Figure 1.
Workflow of jaw movement analyses conducted in the current investigation.
During the electrognathography test, participants’ mandibular movements were recorded using a digital electrognathograph (JT-3D; BioResearch Associates Inc., Brown Deer, WI, USA) while performing maximum mouth opening, repeated three times without assistance or resistance. Jaw movement was tracked in real-time using two tracking cameras linked to in-house deep learning software [22,23]. This software identified points of maximum mouth opening and trends in facial feature changes, which were then traced back to corresponding hard tissue outputs of electrognathography. The software-based tracking system was calibrated using the following linear measurements in millimetres, which were manually measured for each participant: inter-zygion distance, nasion to pogonion distance, subnasale to pogonion distance, and distance of the ala-tragus line [22].
Following that, participants were recorded using a 6-channel surface electromyography device (BioEMG III; BioResearch Associates Inc., Brown Deer, WI, USA), with electrodes placed on the temporalis, masseter, and digastric muscles after cleaning sebaceous secretions and cosmetic layers. Grounding was established on the right wrist. Each activity was recorded three times for a duration of 10 s each, and the mean output was extracted in post-processing.
Next, participants wore a TMJ vibration analyser (JVA; BioResearch Associates Inc.) and performed the same activities for six consecutive cycles. The mean integral and amplitude values of the cycles were extracted for both the right and left TMJ, and the mean difference between the two joints was documented.
2.3. Data Processing
Readings from all instruments were obtained using proprietary software (Biopak; BioResearch Associates Inc.), capturing an averaged value for each activity. Due to the complexity and inability to extract time-series data directly from the proprietary interface, muscle activity sweeps were first saved in JPEG format and processed through Dental Loop Signals, a component of the authors’ in-house software suite tailored to standardise masticatory muscle activity [24]. This software employs deep learning-based variational encoders and cluster-based deep learning methods to convert muscle activity into normalised signals and generate quotients for each muscle activity. The mean quotient of each bilateral muscle group was then documented.
2.4. Statistical Analyses
Logistic regression models were initially applied to test all variables on the included participants. Subsequently, the models were run exclusively on the parameters for individuals who had received orthodontic treatment to determine predictor values for jaw clicking. Tests for normality were conducted using the Kolmogorov–Smirnov test and observation of distribution charts. Independent t-tests and Mann–Whitney U tests were performed to evaluate differences in jaw movement analyses between groups with a history of occlusal therapy and those without such a history. All models were designed and implemented using R v2023.03.1 Build 446 [25].
3. Results
Seventy participants aged 18 to 65 were recruited for the study between June and August 2023 from the state of South Australia with a mean and median age of 34.6 years and 33.5 years, respectively. Among these participants, 26 reported a positive history of jaw clicking, with 8 reporting bilateral symptoms. Table 1 provides details on the ethnic backgrounds of the participants, and Figure 2 illustrates their distribution.

Table 1.
Distribution of participants according to ethnic origin.
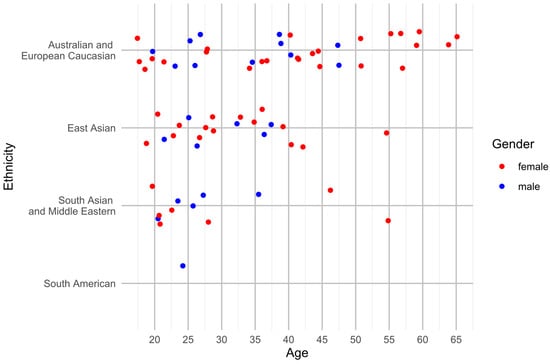
Figure 2.
Demographic distribution of participants according to age, gender, and ethnicity.
Additionally, Figure 3 illustrates the distribution of reasons for participating, with 20% of participants citing existing “jaw problems” affecting their quality of life. Among the 70 participants, 35 had undergone corrective occlusal therapy, while 35 had not. The medication documented is detailed in Table 2. The possibility of drug interactions was not evaluated in the current assessment.
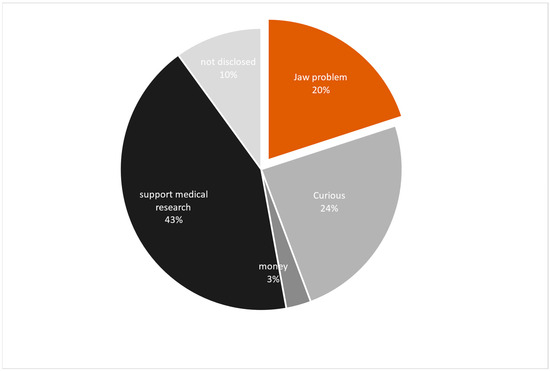
Figure 3.
Motivation of participants for signing up for the research project.

Table 2.
Prescribed medications used by participants for a duration of six months or longer at the time of study.
Logistic regression was used to analyse variables influencing jaw clicking (Table 3). The results showed significance for the number of third molars extracted in their lifetime, vitamin D deficiency, and a positive diagnosis of self-reported mental health disorders with prescribed medication. The overall model demonstrated significant clinical relevance (p = 0.048), with 41.4% of the incidences of clicking being explained by the dependent variables (R2 = 0.414). The analysis compared ethnicities using ‘Australian and European Caucasian’ as the standard. Data from a single participant of ‘South American’ origin were excluded due to a high standard error. Additionally, a positive medical history of hypertension and hyperlipidaemia were excluded due to a high standard error and a poor fit caused by a small subset of occurrences. Figure 4 illustrates the fitted model, demonstrating appropriate predicted incidences of clicking versus a positive history of clicking despite an irregularly distributed dataset.

Table 3.
Logistic regression of the variables considered and their association with jaw clicking (n = 69).
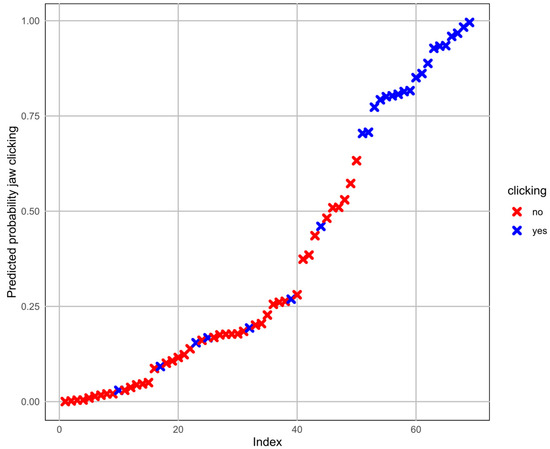
Figure 4.
Model prediction performance on predicted incidences of clicking versus positive diagnosis of clicking.
A follow-up model explored variables directly related to corrective occlusal therapy of occlusion, in particular orthodontic intervention. The overall model was clinically relevant (P = 0.027), with 59% (R2 = 0.59) of the incidences of clicking explained by the dependent variables. A positive history of parafunctional clenching and the choice of retainer were strongly associated with jaw clicking, with removable appliances showing lesser associations with causing jaw clicks (Table 4). The duration of wearing a retainer was not a significant contributor; however, estimates suggested that wearing retainers for more than four years decreased associations with jaw clicking. A recent study suggested that obesity can significantly impede physiological masticatory function and affect jaw movement [26]. Therefore, BMI and maximum mouth opening were included in the current model to account for anatomical variations.

Table 4.
Logistic regression for the likelihood of dental variables, jaw function parameters, and parafunctional habits associated with jaw clicking in patients with a positive history of corrective occlusal therapy (n = 34).
Jaw movement parameters were compiled from electrognathography, surface electromyography, and joint vibration analysis for 66 participants. Four EMG readings out of seventy participants were deemed suboptimal and discarded. The Table S1 in the Supplementary File presents the metadata of jaw kinematics synthesised from the 66 participants. Each component of the jaw movement analysis was independently evaluated and compared between two groups: those with a history of corrective occlusal therapy and those without treatment. Overall, there were no significant differences across all parameters evaluated (Table 5). However, participants with a history of corrective occlusal therapy showed greater variations in joint vibration integral differences between the left and right TMJ (occlusal therapy IQR = 11.65, no treatment IQR = 7.18) and higher median vibration frequency difference between the left and right TMJ (median = -0.20 Hz, IQR = 1.27). In contrast, participants who did not receive corrective occlusal therapy exhibited less variance in median vibration frequency (median = -0.10 Hz, IQR = 0.65). Occlusal therapy was associated with a reduction in mean normalised temporalis muscle activity but a slight increase in masseter muscle activity. However, none of the muscle function changes demonstrated significant differences.

Table 5.
Variances in jaw kinematic parameters among participants who received corrective occlusal therapy (n = 34) compared to those who did not undergo treatment (n = 32). (Vibration Integral differences represent residual values obtained from calculating the disparities between the right and left temporomandibular joint. Normalised muscle activity refers to the average activity observed in both the right and left muscle groups.)
4. Discussion
This study identified significant predictors for jaw clicking within the selected South Australian population, leading to the rejection of the first null hypothesis. However, there were no significant differences observed in jaw movement analysis parameters between participants with a positive history of occlusal therapy and those without such treatment, resulting in the acceptance of the second null hypothesis.
The current study utilised quantitative electronic jaw tracking systems and multiple deep learning software to generate jaw movement parameters across a diverse population subset in the state of South Australia. To the best of the authors’ knowledge, a study of this nature has not been previously conducted on the target population. The authors acknowledge that definitive diagnoses for temporomandibular joint disorders, such as disc derangement, require imaging investigations. However, the primary focus of the current study was not to propose a diagnostic method for temporomandibular dysfunctions but rather to identify trends in history that may correlate with self-reported or observed clicking. This is particularly relevant as clicking can be apparent without the need for robust imaging modalities and can be detected either directly or through joint vibration analyses, especially when the clicks are subtle.
4.1. Awareness of Jaw Clicking
To ensure a random cohort of participants and prevent biases, the current eligibility criteria intentionally did not specify awareness of clicking. During the history-taking process, additional inquiries were made to understand the motivations of the participants in the study. Of note, some participants were unaware of the source of the clicking and crunching sounds and had visited medical practitioners and ENT specialists, only to be diagnosed with temporomandibular dysfunction later. This may indicate that little has changed in terms of public awareness of conditions leading to clicking since 1983 [10], likely because most dental practitioners and trainees worldwide do not receive specific training on raising awareness about the long-term effects of clicking during the screening process or TMD management [27].
4.2. Mental Health and Jaw Clicking
The study indicated that 15.22% of the incidence of clicking could be significantly explained by a history of mental health disorders. These findings underscore the deterioration of mental health in the community, as evidenced by the significant influence of self-reported mental health on jaw clicking, along with the self-reported use of prescribed medication to manage these conditions. Psychological state modifiers such as selective serotonin reuptake inhibitors (SSRIs) and amphetamines can lead to the development of involuntary jaw activities and parafunctional habits and subsequent TMJ dysfunction [28]. Previous studies have documented that antidepressant-associated bruxism remains an underrecognized phenomenon and lacks adequate communication for dose adjustment to relieve additional effects on the temporomandibular joint complex [29].
4.3. Medical Conditions and Jaw Clicking
Predisposing medical conditions and subsequently prescribed medication can alter the physiology of jaw kinematics [2]. Estrogen and progesterone supplements, frequently prescribed to female participants, have been demonstrated in several instances to alter jaw kinematics [2]. Vitamin D deficiency, contributing to 14.97% of the incidences of jaw clicking in the current study, affects one third of the Australian population [30]. Deficiencies can impact musculoskeletal health, leading to issues such as masticatory muscle weakness, premature spasm, and degradation of bone quality. In severe cases, it can even result in bone-related disorders like osteoporosis. Conversely, prescription of Vitamin D supplements to address such deficiencies can be beneficial in addressing existing TMJ dysfunction [31]. While there is evidence linking Vitamin D deficiency to TMJ dysfunction, further investigation is needed to establish definitive correlations [32].
4.4. Influence of Tooth Extraction on Jaw Clicking
The number of previous third molars extracted was a significant predictor of jaw clicking explaining 15.21% of all incidences. Premolar extractions were not however significant predictors, despite recent reports suggesting that premolar extractions led to changes in jaw kinematics on the anteroposterior place [33]. It is likely that premolar extraction may have a more pronounced role in anteroposterior kinematics, while third molar extraction might affect vertical kinematics such as mouth opening more frequently. Extraction of all four premolars followed by orthodontic space closure enables a form of balance and compensation that might prevent disruption of vertical kinematics, whereas a single third molar extraction does the opposite. Many authors therefore recommend the prophylactic extraction of all four third molars while asymptomatic to prevent disruption of physiological jaw movement [34]. However, there is insufficient evidence to support or dismiss prophylactic third molar extraction, and therefore retention of asymptomatic third molars cannot be made into a routine recommendation as a means of preventing jaw clicking [34].
4.5. The Relation of Jaw Clicking to Occlusal Therapy
Occlusal therapy, particularly orthodontic treatments, have previously been linked to temporomandibular disorders [5]. Although the present study did not find significant differences in jaw movement analysis supporting this claim, it is still valuable to examine some of the findings. The study suggests that removable orthodontic retainers worn for more than four years after successful treatment completion were less associated with jaw clicking issues compared to fixed retainers. However, it is important to note that removable retainers are less convenient and often have documented issues with patient compliance [35]. While it would not be appropriate to exclusively prescribe removable retainers, practitioners should actively discuss with their patients the possibility of experiencing jaw clicking and encourage them to seek professional advice if such issues arise. This is especially important considering specific cases where overjet correction followed by fixed lingual retainers may result in undesired tooth movement if not adequately monitored and addressed [36]. On the other hand, fixed retainers may inadvertently exacerbate existing parafunctional habits. The favourable findings in the current study for removable retainers may be attributed to their limited daily wear time, resulting in a lower likelihood of jaw clicking.
4.6. Sociodemographic Factors and Jaw Clicking
It is important to discuss the multicultural demographics of the state of South Australia, which is inhabited by members of Asian, European, and American descent, alongside Aboriginal members of the First Nation. The current study collected data from a diverse demographic, predominantly females, which also serves as a limitation. From a social preference perspective, it has been proposed that patients identifying with Asian backgrounds tend to seek treatment only when there is a significant oral health issue, rather than using dental services for screening and preventive intervention; however, this may be viewed as a generalisation [37]. In some cases, the desire for aesthetic outcomes takes precedence over a proper occlusal function, even when painful symptoms are present in Asian populations [38]. This suggests that the initial source of jaw clicking may go unnoticed until painful manifestations occur later. From a psychological well-being perspective, clicking and occlusal therapy could be linked to stressful circumstances and untreated mental health conditions, as well as poor sleep quality, rather than dental treatment being a causative factor, as seen in the current investigation [39]. However, it is important to note that research on this subject matter is considered very limited, and drawing meaningful conclusions requires further investigation and future research [9,40].
4.7. Study Limitations
In the present study, several limitations were documented as some variables exhibited higher standard errors compared to others due to the relatively small dataset covering numerous variables of heterogenous distribution. The specific limitations included the following:
- Data heterogeneity: Despite the good fit of the model, cross-validation and odds ratio analyses were considered inappropriate due to the small sample size and variations within the dataset, resulting in large confidence intervals. A cause-and-effect relationship model was not designed based on a time sequence because the exact time of clicking commencement could not be established from history alone. Furthermore, the precise reasons why participants underwent orthodontic treatment could not be verified as participant histories were reliant on self-report and details of the dental treatment practices were not recorded to preserve privacy and avoid biased claims. Therefore, the historical term “occlusal therapy” was used instead, as it encompasses various aspects of dentistry, primarily orthodontic treatment, but can also include prosthetic rehabilitation, paediatric prophylactic extractions, and surgical management [1].
- A lack of imaging data: The study did not involve computed tomography as input data to observe anatomical changes or magnetic resonance imaging for diagnosing disc displacement during opening or closing, and thus, confirmatory diagnoses was not made for any of the participants. The focus was instead directed towards evaluating the joint complex function. Points of maximum vibration during mouth opening were recorded. Data augmentation was not performed to stay true to the current demographic distribution and should be a topic of future deep learning applications [41].
- A lack of longitudinal data: The study did not facilitate a pre- and post-comparison of jaw movement and joint function following dental or specialist treatment, instead opting for a randomised cross-sectional approach. Future longitudinal studies, incorporating investigative imaging and assessments of orthodontic treatment needs, could be designed to evaluate the true impact of orthodontic correction across various clinical classifications of malocclusion. An additional investigation will be carried out to quantify occlusal parameters such as arch perimeters, overjet, and overbite, which were beyond the scope of the current investigation and warranted a separate study.
5. Conclusions
In the selected study population, the following can be inferred from the data generated:
- Predictors such as the number of third molars extracted, history of vitamin D deficiency, and self-reported mental health disorders were associated with incidences of jaw clicking.
- A positive history of parafunctional clenching and the choice of dental prostheses showed noteworthy associations with the likelihood of experiencing jaw clicking, with removable appliances demonstrating lower associations and warrants further investigation.
- Wearing retainers for longer periods may reduce the likelihood of jaw clicking.
- The current study is limited in its capacity to determine whether occlusal therapy is ineffective in addressing jaw clicking or if it contributes to the condition. The small sample size would diminish confidence in the concluding statement. This aspect cannot be ascertained within the current study design and requires further investigation in future longitudinal research with larger population data to instil greater confidence.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/oral4020018/s1, Table S1: the metadata of jaw kinematics synthesised from the 66 participants.
Author Contributions
Conceptualization: T.H.F., J.D.; Methodology Design: T.H.F., L.R.; Data Collection: T.H.F., L.R.; Data Processing: T.H.F., L.R.; Codes and Metadata synthesis: T.H.F.; Data Interpretation: T.H.F., J.D.; Manuscript writing: T.H.F.; Manuscript revision: J.D.; Final Approval for Submission: J.D. All authors have read and agreed to the published version of the manuscript.
Funding
The study was supported by the University of Adelaide Kwok Paul Lee Bequest (350-75134777) and Early Grant Development funds (340-13133234).
Institutional Review Board Statement
The study was approved by the University of Adelaide Human Research and Ethics Committee (HREC H-2022-185). Written consent was obtained from every participant included in the study.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
All metadata utilised to derive quantitative conclusions in the present study have been provided as a supplementary file accompanying the manuscript. However, demographic data and medical history cannot be shared due to due to privacy and ethical restrictions.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Clark, G.T.; Adler, R.C. A critical evaluation of occlusal therapy: Occlusal adjustment procedures. J. Am. Dent. Assoc. 1985, 110, 743–750. [Google Scholar] [CrossRef] [PubMed]
- Farook, T.H.; Dudley, J. Neuroendocrine Influencers and Associated Factors That Shape Jaw Movement and Growth in Temporomandibular Joint Disorder Management: A Systematic Review of Clinical and Radiographic Evidence. J. Pers. Med. 2023, 13, 840. [Google Scholar] [CrossRef] [PubMed]
- Sivaraman, K.; Chopra, A.; Venkatesh, S.B. Clinical importance of median mandibular flexure in oral rehabilitation: A review. J. Oral. Rehabil. 2016, 43, 215–225. [Google Scholar] [CrossRef] [PubMed]
- Farook, T.H.; Rashid, F.; Ahmed, S.; Dudley, J. Clinical machine learning in parafunctional and altered functional occlusion: A systematic review. J. Prosthet. Dent. 2023. [Google Scholar] [CrossRef] [PubMed]
- Farook, T.H.; Rashid, F.; Alam, M.K.; Dudley, J. Variables influencing the device-dependent approaches in digitally analysing jaw movement—A systematic review. Clin. Oral. Investig. 2022, 27, 489–504. [Google Scholar] [CrossRef] [PubMed]
- Sohn, B.W.; Miyawaki, S.; Noguchi, H.; Takada, K. Changes in jaw movement and jaw closing muscle activity after orthodontic correction of incisor crossbite. Am. J. Orthod. Dentofac. Orthop. 1997, 112, 403–409. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Cai, B.; Fan, S.; Lu, S.; Dai, K. Association of oral behaviors with anxiety, depression, and jaw function in patients with temporomandibular disorders in China: A cross-sectional study. Med. Sci. Monit. 2021, 27, e929985-1. [Google Scholar] [CrossRef] [PubMed]
- Atsü, S.S.; Güner, S.; Palulu, N.; Bulut, A.C.; Kürkçüoğlu, I. Oral parafunctions, personality traits, anxiety and their association with signs and symptoms of temporomandibular disorders in the adolescents. Afr. Health Sci. 2019, 19, 1801–1810. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.K.; Abutayyem, H.; Almuhyi, N.H.S.; Alsabilah, K.A.S.; Alkubaydan, F.S.T.; Alswairki, H.J.; Awawdeh, M.A.; Hajeer, M.Y.; Alzabni, K.M.D.D.; Awawdeha, M. The Impact of Temporomandibular Disorders on Orthodontic Management: A Systematic Review and Meta-Analysis. Cureus 2023, 15, e44243. [Google Scholar] [CrossRef]
- Sigaroudi, K.; Knap, F.J. Analysis of jaw movements in patients with temporomandibular joint click. J. Prosthet. Dent. 1983, 50, 245–250. [Google Scholar] [CrossRef]
- Cioffi, I. Biological and psychological factors affecting the sensory and jaw motor responses to orthodontic tooth movement. Orthod. Craniofac Res. 2023, 26, 55–63. [Google Scholar] [CrossRef]
- Serafim, I.; Rode, S.; Lopes, S.; Oliveira, W.; Pinho, S.; Silva, E.; Winocur, E.; E Cruz, M.M. Impact of bruxism on craniomandibular morphology: A cone-beam computed tomographic study. CRANIO® 2023, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Borzabadi-Farahani, A.; Olkun, H.K.; Eslamian, L.; Eslamipour, F. Functional needs in orthognathic patients with different sagittal skeletal discrepancies. Oral Surg. Oral. Med. Oral Pathol. Oral Radiol. 2024. [Google Scholar] [CrossRef] [PubMed]
- Matsuda, S.D.; Yamaguchi, T.D.; Mikami, S.D.; Yoshimura, H.D.; Gotouda, A.D. Can malocclusion provide clinicians with information for differential diagnosis of temporomandibular joint diseases?: A review. Medicine 2022, 101, e29247. [Google Scholar] [CrossRef]
- Lujan-Climent, M.; Martinez-Gomis, J.; Palau, S.; Ayuso-Montero, R.; Salsench, J.; Peraire, M. Influence of static and dynamic occlusal characteristics and muscle force on masticatory performance in dentate adults. Eur. J. Oral. Sci. 2008, 116, 229–236. [Google Scholar] [CrossRef]
- Kondrat, W.; Sierpińska, T.; Radke, J. Assessment of the temporomandibular joint function in young adults without complaints from the masticatory system. Int. J. Med. Sci. 2018, 15, 161. [Google Scholar] [CrossRef] [PubMed]
- Farook, T.H.; Haq, T.M.; Ramees, L.; Dudley, J. Deep learning and predictive modelling for generating normalised muscle function parameters from signal images of mandibular electromyography. Med. Biol. Eng. Comput. 2024, 20, 1–7. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical power analyses using G* Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Klineberg, I.; Eckert, S. Functional Occlusion in Restorative Dentistry and Prosthodontics; Elsevier Health Sciences: Amsterdam, The Netherlands, 2015. [Google Scholar]
- Lim, C.-Y.; In, J. Randomization in clinical studies. Korean J. Anesthesiol. 2019, 72, 221–232. [Google Scholar] [CrossRef]
- Farook, T.H.; Ahmed, S.; Talukder, M.S.I.; Dudley, J. A 3D printed electronic wearable device to generate vertical, horizontal and phono-articulatory jaw movement parameters: A concept implementation. PLoS ONE 2023, 18, e0290497. [Google Scholar] [CrossRef]
- Farook, T.H.; Saad, F.H.; Ahmed, S.; Dudley, J. Dental Loop FLT: Facial landmark tracking. SoftwareX 2023, 24, 101531. [Google Scholar] [CrossRef]
- Farook, T.H.; Saad, F.H.; Ahmed, S.; Dudley, J. Dental loop SnP: Speech and phonetic pattern recognition. SoftwareX 2023, 24, 101604. [Google Scholar] [CrossRef]
- Farook, T.H.; Haq, T.M.; Dudley, J. Dental loop signals: Image-to-signal processing for mandibular electromyography. Software Impacts 2024, 19, 100631. [Google Scholar] [CrossRef]
- R Development Core Team. R: A Language and Environment for Statistical Computing; R-Project; R Foundation for Statistical Computing: Vienna, Austria, 2010. [Google Scholar]
- Li, R.; Kato, C.; Fujita, A.; Abe, Y.; Ogawa, T.; Ishidori, H.; Misawa, E.; Okihara, H.; Kokai, S.; Ono, T. Effect of Obesity on Masticatory Muscle Activity and Rhythmic Jaw Movements Evoked by Electrical Stimulation of Different Cortical Masticatory Areas. J. Clin. Med. 2023, 12, 3856. [Google Scholar] [CrossRef] [PubMed]
- Xiong, X.; Xiao, C.; Zhou, X.; Li, X.; Wang, J.; Yi, Y. Knowledge and Attitudes regarding Temporomandibular Disorders among Postgraduate Dental Students and Practicing Dentists in Western China: A Questionnaire-Based Observational Investigation. Pain. Res. Manag. 2023, 2023, 7886248. [Google Scholar] [CrossRef] [PubMed]
- Dimitroulis, G. Management of temporomandibular joint disorders: A surgeon’s perspective. Aust. Dent. J. 2018, 63, S79–S90. [Google Scholar] [CrossRef]
- Garrett, A.R.; Hawley, J.S. SSRI-associated bruxism: A systematic review of published case reports. Neurol. Clin. Pract. 2018, 8, 135–141. [Google Scholar] [CrossRef]
- Daly, R.M.; Gagnon, C.; Lu, Z.X.; Magliano, D.J.; Dunstan, D.W.; Sikaris, K.A.; Zimmet, P.Z.; Ebeling, P.R.; Shaw, J.E. Prevalence of vitamin D deficiency and its determinants in Australian adults aged 25 years and older: A national, population-based study. Clin. Endocrinol. 2012, 77, 26–35. [Google Scholar] [CrossRef] [PubMed]
- Kui, A.; Buduru, S.; Labunet, A.; Balhuc, S.; Negucioiu, M. Vitamin D and temporomandibular disorders: What do we know so far? Nutrients 2021, 13, 1286. [Google Scholar] [CrossRef]
- Ferrillo, M.; Lippi, L.; Giudice, A.; Calafiore, D.; Paolucci, T.; Renò, F.; Migliario, M.; Fortunato, L.; Invernizzi, M.; de Sire, A. Temporomandibular disorders and vitamin D deficiency: What is the linkage between these conditions? A systematic review. J. Clin. Med. 2022, 11, 6231. [Google Scholar] [CrossRef]
- Londoño, A.; Assis, M.; Fornai, C.; Greven, M. Premolar Extraction Affects Mandibular Kinematics. Eur. J. Dent. 2022, 17, 756–764. [Google Scholar] [CrossRef] [PubMed]
- Ghaeminia, H.; Perry, J.; Nienhuijs, M.E.; Toedtling, V.; Tummers, M.; Hoppenreijs, T.J.; Van der Sanden, W.J.; Mettes, T.G. Surgical removal versus retention for the management of asymptomatic disease-free impacted wisdom teeth. Cochrane Database Syst. Rev. 2016, 5, CD003879. [Google Scholar] [CrossRef]
- Al-Moghrabi, D.; Salazar, F.C.; Pandis, N.; Fleming, P.S. Compliance with removable orthodontic appliances and adjuncts: A systematic review and meta-analysis. Am. J. Orthod. Dentofac. Orthop. 2017, 152, 17–32. [Google Scholar] [CrossRef]
- Wolf, M.; Schulte, U.; Küpper, K.; Bourauel, C.; Keilig, L.; Papageorgiou, S.N.; Dirk, C.; Kirschneck, C.; Daratsianos, N.; Jäger, A. Post-treatment changes in permanent retention. J. Orofac. Orthop. Fortschritte Der Kieferorthopädie 2016, 77, 446–453. [Google Scholar] [CrossRef]
- Arora, G.; Mackay, D.F.; Conway, D.I.; Pell, J.P. Ethnic differences in oral health and use of dental services: Cross-sectional study using the 2009 Adult Dental Health Survey. BMC Oral Health 2017, 17, 1. [Google Scholar] [CrossRef] [PubMed]
- Supakomonnun, S.; Mitrirattanakul, S.; Chintavalakorn, R.; Saengfai, N.N. Influence of functional and esthetic expectations on orthodontic pain. J. Orofac. Orthop./Fortschritte Der Kieferorthopadie 2021, 84, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Lei, J.; Fu, J.; Yap, A.U.J.; Fu, K.-Y. Temporomandibular disorders symptoms in Asian adolescents and their association with sleep quality and psychological distress. CRANIO® 2016, 34, 242–249. [Google Scholar] [CrossRef]
- Butani, Y.; Weintraub, J.A.; Barker, J.C. Oral health-related cultural beliefs for four racial/ethnic groups: Assessment of the literature. BMC Oral Health 2008, 8, 26. [Google Scholar] [CrossRef]
- Van Dyk, D.A.; Meng, X.-L. The art of data augmentation. J. Comput. Graph. Stat. 2001, 10, 1–50. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).