1. Introduction
To date, mini-screws are a valuable anchorage device used by clinicians to improve orthodontic mechanics [
1,
2,
3]. Concerning biomechanical requirements, some authors have proposed various sites for mini-screws’ insertion: palatal bone, maxillary alveolar process, mandibular buccal shelf, retromolar trigone [
4,
5,
6,
7,
8], and infra-zygomatic ridge [
4,
6,
7,
9]. Anatomical characteristics of the insertion site may affect the failure of mini-screws [
10,
11,
12]. In particular, the success of mini-screw placement is influenced by the amount of bone, cortical bone thickness, bone density [
11,
13], and the anatomical proximity of the roots [
14], nerves, vessels [
15], sinuses, nasal cavities [
16], and frenula [
17]; also, the characteristics of soft tissues [
18] can influence the success of a mini-screw insertion procedure. Some authors have proposed the insertion site localized in the posterior area of the mandible behind the third molar area for the dentoalveolar correction of class 3 malocclusion [
19]. The buccal shelf insertion site was extensively evaluated in the orthodontic literature [
4,
7,
19]. However, the mentioned study did not evaluate bone characteristics posterior to the second molar. This study aimed to evaluate the anatomical characteristics of a posterior area in the mandible localized distally to the second molars and extending in the vestibular direction toward the bony step, which we define as “buccal step”, in a patient with different skeletal patterns.
The secondary aim was to assess whether there is a correlation between buccal step insertion site characteristics and facial skeletal patterns.
2. Materials and Methods
This retrospective study follows the guidelines of the Declaration of Helsinki. The protocol of this study was approved by an ethical committee (Prot. 33-2020) on June 29, 2020. The sample of this study included 85 CBCT (cone beam computed tomography) records selected by an experienced orthodontic clinician from the Polyclinic digital archive of the University of Messina and the digital archive of private practice. The CBCT exams selected had to have the following inclusion criteria: Caucasian subjects, age between 25 and 65 y.o., absence of craniofacial anomaly, agenesis of teeth except for third molars, and absence of amalgam fillings in the teeth. The CBCT exams of patients that met these inclusion criteria were included. The total number of patients that met the inclusion criteria was 85 (51 female and 34 male, mean age 29.22 ± 8.7), with 33 patients having no third molars and 52 having third molars. According to the diagnostic records, 19 patients with hyperdivergency, 25 patients with normo-divergency, and 41 patients with hypodivergency were identified in the sample, of which 32 were in skeletal class I, 36 were in skeletal class II, and 17 were in skeletal class III. Patients were divided into four groups according to gender and the presence of mandibular third molars. The patients included in each of the four groups were sorted according to age, from youngest to oldest; facial types and skeletal classes were not considered in this subdivision. A random sequence generator (
http://www.randomizer.org, accessed on 16 January 2023) was used to generate four lists of randomized numbers to create two final gender-balanced groups: group 1 with patients with the presence of third molars and group 2 with patients with the absence of third molars. All CBCT examinations were performed with the i-CAT CBCT scanner (Imaging Sciences International, Hatfield, PA, USA) after setting the acquisition parameters as follows: 120 kV, 5 mA, and 4 to 6 s exposure times. All considered records were converted into digital imaging and communications in medicine (DICOM) format. DICOM files were processed using the Horos Medical Imaging 64-bit software (Horos Project, Geneva, Switzerland). The Horos is a free DICOM viewer for Mac OS X based on OsiriX 5.8, the latest open-source version of OsiriX. The following procedure was used to obtain sections for an analysis of the amount of cortical bone and total bone in the area defined as the buccal step. The three colored reference lines offered by the software interface that correspond to the three conventional scan planes were considered: the yellow line identifies the sagittal plane; the purple line identifies the axial plane; and the blue line identifies the coronal plane. The scanning planes were then reoriented according to the following method: in the coronal view, the purple line was positioned to pass through the puncture point of the right and left first molar; in the axial view, the yellow line was positioned to pass through the alveolar process of first and second molars; and, in the sagittal view, the point of insertion of the scanning planes was positioned at the level of the distal CEJ of the permanent second molar (
Figure 1).
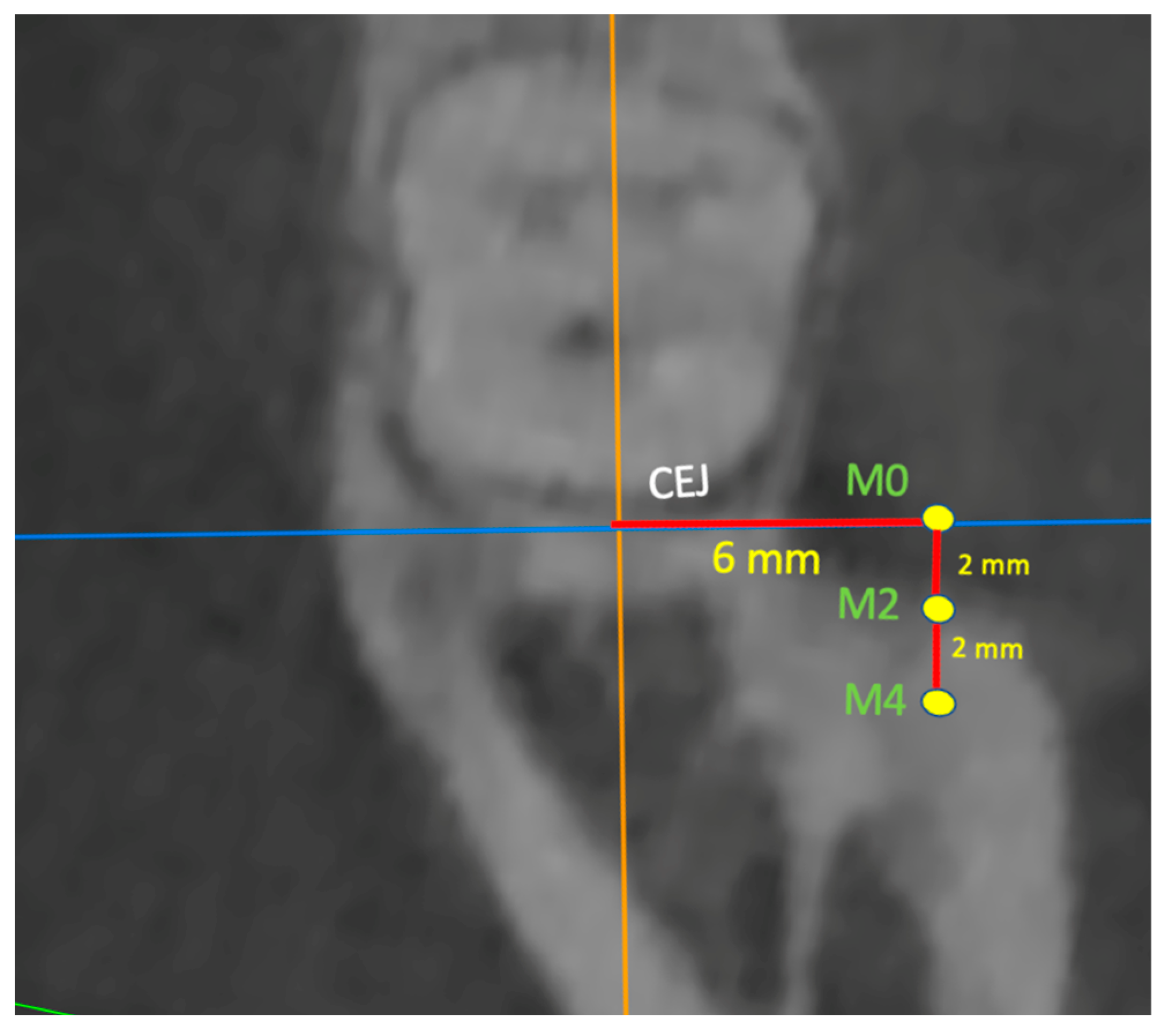
In the axial view, the point resulting from the reorientation of the planes was named as CEJc (cementoenamel junction crest), and a line was then traced from the CEJc in the lingual-vestibular direction of 6 mm in length and the first point of the measurements called M0 was identified here (
Figure 2 and
Figure 3).
Next, two lines were drawn from M0, parallel to the yellow line, one at 2 mm (M2) and one at 4 mm (M4) in the postero-anterior direction.
In the axial view, planes were dragged at each point to obtain the precise cut-off in the coronal view, where measurements were made at a 90° angle to the occlusal plane of cortical thickness and total bone depth. A set of six measurements was taken for each scan root plane assessing the total and cortical bone depth in the apical direction: cortical bone thickness M0 (CrtM0), total bone depth M0 (TotM0), cortical bone thickness M2 (CrtM2), total bone depth M2 (TotM2), cortical bone thickness M4 (CrtM4), and total bone depth M4 (TotM4). All measurements were taken for both the left and right sides.
All measurements were taken while maintaining a safety distance of at least 2 mm from the lower alveolar nerve canal.
Statistics
Power analysis was performed with a power of 80% and a significance of 0.05. Power analysis was performed preliminarily on a group of 10 patients; the mean total bone depth in M2 was 17 mm, and the standard deviation (SD) was 16.1 mm. The analysis showed a sample size of 78 cases. Enrollment was set at 85 patients to minimize the risk of false negatives. The total bone depth and cortical bone thickness in the buccal step area were measured via M0 point, M2 point, and M4 point in an apical direction with a 90° inclination to the occlusal plane. A preliminary analysis of the data was performed to evaluate the normal distribution with the Shapiro–Wilk test and to assess the homogeneity of variance with Levene’s test. Descriptive and inferential statistics were performed using SPSS statistical software (version 25.0; IBM Corporation, Armonk, NY, USA). The paired
t-test and the intraclass correlation coefficient (ICC) were used to assess intra-operator reliability, as well as the inter-operator agreement between two independent operators. The magnitude of the random error was assessed using Dahlberg’s formula; no differences (
p < 0.05) were found between the two readings. Descriptive statistics were performed and reported the mean, SD, and maximum and minimum values for each considered parameter; these are reported in
Table 1. The greater total bone thickness was found at M4 (17.2 mm), and the greater cortical bone thickness was found at M0 (3.69 mm). For the inferential statistics, if the data showed a normal distribution, the following parametric tests were performed: unpaired
t-test, analysis of variance (ANOVA), and Tukey’s post hoc test. If the data showed a non-normal distribution, the following non-parametric tests were used: Kruskal–Wallis test and Dunn–Bonferroni post hoc test. The significance levels for all tests were set at
p < 0.05.
3. Results
In this study, descriptive statistics of the general sample and descriptive statistics within each subgroup (group with third molars, group without third molars, hyper-divergent, hypo-divergent, normo-divergent) were completed (
Table 1).
Both the descriptive statistics of the overall sample and in the different subgroups showed in the mesial-distal direction an increase in total bone and a decrease in cortical thickness; furthermore, the patients with hypo-divergency showed on average at least 0.4 mm greater cortical bone thicknesses.
Patients without a third molar showed, on average, total bone thicknesses greater than at least 1 mm and cortical bone thicknesses greater than 0.1 mm.
Inferential statistics were conducted among the sites considered (M0, M2, M4) with both third molars and without third molars (
Table 2). In addition, comparisons were made between sites in subgroups created according to patients’ facial biotypes (normo-divergence, hypo-divergence, hyper-divergence) with and without third molars (
Table 2).
4. Discussion
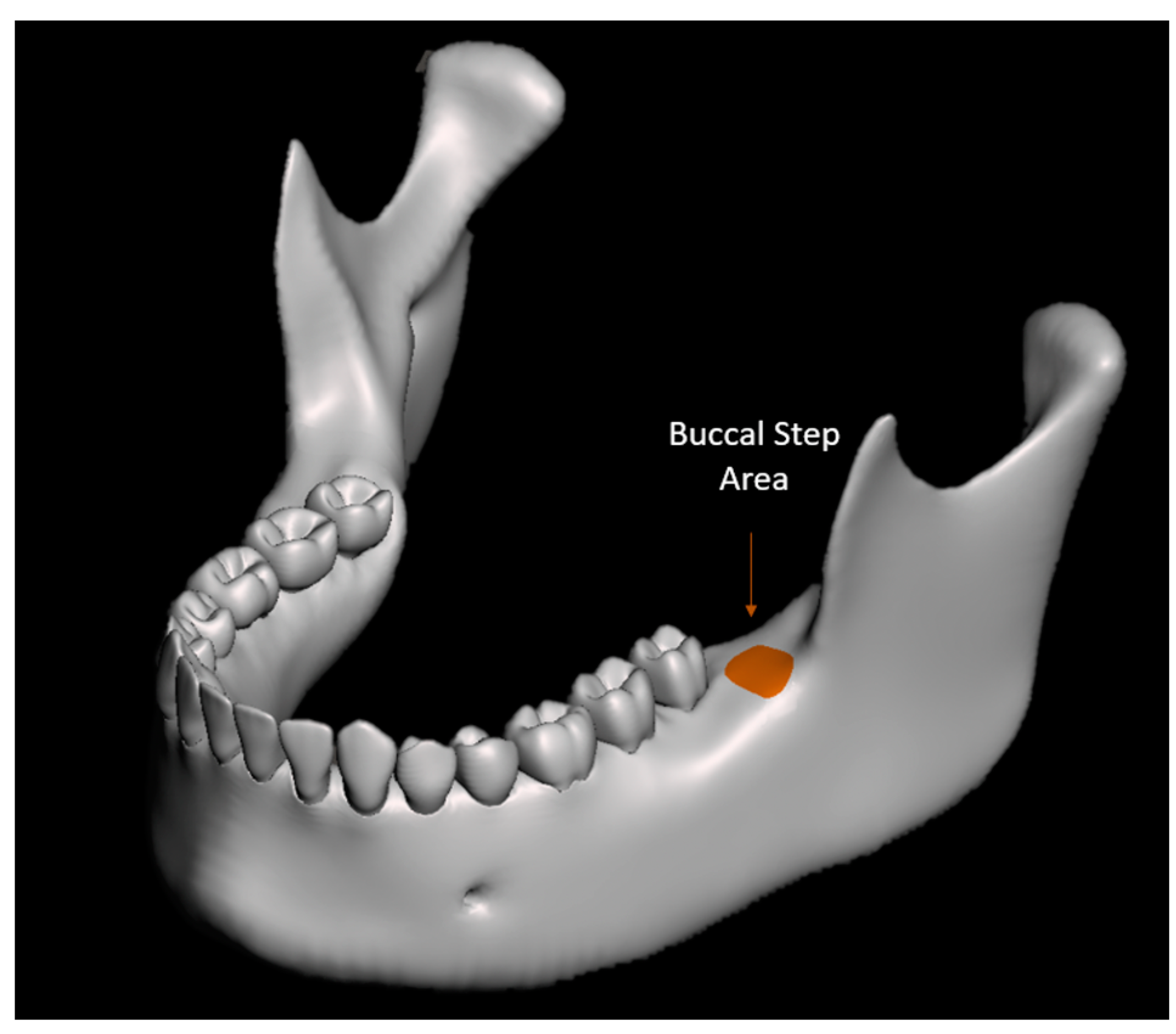
To the best of our knowledge, this is the first study in the literature that evaluates the bone quantity in a region posteriorly located compared to the buccal shelf, which was named the buccal step insertion site (
Figure 4).
The buccal step area has several biomechanical advantages. Being an extra-radicular site, it reduces the risk of screw-to-root impact during a mini-screw insertion procedure, which has been considered the primary cause of mini-screw failure [
20]. Several authors have documented cases in the literature using the buccal step as an insertion site in class 3 malocclusions [
19,
21], in cases of medially impacted mandibular molars [
22,
23], and in cases of enforcement molar uprighting [
24]. To ensure successful mini-screw insertion in the buccal step area, it is crucial to have a good understanding of the anatomical bone characteristics at this site its various relationships with regard to the alveolar nerve. A minimum buccal bone thickness of 5 mm (considering 1.7 mm for root safety distance, 1.6 mm for screw diameter, and 1.7 mm for cortical buccal bone safety distance) was considered as a safe threshold for mini-screw insertion [
1,
7].
A study by Nucera et al. evaluated the total and cortical bone thicknesses of the mandibular buccal shelf at a site near the buccal step but located anteriorly compared to the buccal step [
1]. The authors found that the buccal shelf consistently had bone thicknesses of at least 7 mm, making it an ideal site for mini-screw placement. However, cortical bone thicknesses in this region varied, underscoring the need for pre-drilling during insertion [
1]. In this investigation, total bone measurements were taken at 90 degrees to the occlusal plane because it is considered easier and more reproducible for the clinician to insert the mini-screw perpendicular to the occlusal plane. Instead, measurement points were chosen at 0 mm (M0), 2 mm (M2), and 4 mm (M4), moving in the buccal direction to allow the clinician using a periodontal millimeter probe to identify the insertion site by starting the millimeter measurement from the amelo-cemental junction of the second molar. The findings of this study indicate that total bone thickness increases in the mesio-distal direction for all sites considered. However, there were no significant differences observed when comparing the total bone thickness values among the evaluated outcomes. This result suggests that the overall increase in bone thickness occurs consistently across all sites, without any specific site showing a significantly different outcome. The cortical bone thickness was also assessed to determine the necessity of pre-drilling. Descriptive statistics showed that the cortical bone thickness decreased in the mesial-distal and that the average cortical bone thickness was consistently at least 3 mm; therefore, a pre-drilling procedure in this site is always recommended to avoid high insertion torque and potential bone resorption around mini-screw neck or mini-screw fracture [
25,
26,
27].
However, similar to total bone depth, no significant differences were found when comparing the cortical bone thicknesses among the evaluated sites, except for the M0 vs. M4 comparison. This result suggests that the decrease in cortical bone thickness is consistent across all sites except for the specific comparison between M0 and M4.
To account for the heterogeneity of subjects’ facial features, subgroup comparisons were created to test the influence of facial vertical skeletal patterns (normo-divergence, hypo-divergence, hyper-divergence) on the results. Within each subgroup, the comparison of the total bone thicknesses between different sites did not yield statistically significant differences. Similarly, the comparison of the cortical bone thicknesses between different sites within the subgroups did not show statistically significant differences, except for the comparison within the hypo-subgroup at the M0 vs. M4 sites. Interestingly, descriptive statistics in the subgroups revealed greater cortical bone thicknesses in subjects with hypo-divergency, which aligns with the previous literature [
4,
23,
28,
29,
30]. This indicates the influence of facial morphology on mandibular cortical bone thickness [
31]. To further explore this, statistical analysis was performed to assess if there were significant differences between subjects with different facial divergences within each site (M0, M2, M4). The results showed no significant differences in cortical bone thickness at site M0, except for the comparison between subjects with hypo-divergency and meso-divergency, which demonstrated greater cortical bone thicknesses than subjects with hypo-divergency. Similar results were obtained for the other two sites (M2, M4). One limitation of this study is the evaluation of Caucasian subjects only, which may limit the generalizability of the findings to other ethnic populations. Another theoretical limitation could be the high standard deviation of the detected bone thicknesses. However, despite the high standard deviation, the total bone depth at each site investigated was sufficient for the insertion of mini-screws, as the minimum value observed was 7.75 mm. This study provides valuable insights into bone thickness variations at different sites and directions of the buccal step, considering the consistent increase in total bone thicknesses in the mesial-distal direction. It also suggests that cortical bone thickness decreases in this direction as subjects with hypo-divergency exhibited greater cortical bone thicknesses. These findings contribute to defining the influence of facial skeletal patterns on the mandibular cortical bone thickness and implications for orthodontic treatment planning and mini-screw insertion strategies. However, future studies evaluating different ethnic groups are necessary to obtain results with greater external validity.
5. Conclusions
The buccal step insertion site offers biomechanical advantages and reduces the risk of screw-to-root impact during mini-screw insertions compared to the buccal shelf. Total bone thickness consistently increases in the mesial-distal direction at all evaluated sites (M0, M2, M4), making it suitable for mini-screw placement. Cortical bone thickness decreases in this direction, with no significant differences among sites except for the M0 vs. M4 comparison. Subjects with hypo-divergency showed greater cortical bone thickness, suggesting that facial skeletal patterns influence mandibular cortical bone thickness. Subgroup comparisons based on facial vertical skeletal patterns did not reveal significant differences in total bone and cortical bone thicknesses between different sites, except for the M0 vs. M4 comparison within the hypo-subgroup. Limitations include this study’s exclusive focus on Caucasian subjects, potentially limiting generalizability to other ethnic populations. However, the total bone depth at each investigated site was sufficient for mini-screw insertion, with the minimum observed value being 7.75 mm. These findings provide insights into the influence of facial skeletal patterns on mandibular cortical bone thickness, informing orthodontic treatment planning and mini-screw insertion strategies. Future research should consider diverse ethnic populations to enhance this study’s external validity.
Author Contributions
Conceptualization, A.M.B., E.C., S.B. and A.C.; data curation, A.M.B., E.C., S.B. and A.C.; formal analysis, A.M.B., E.C., S.B. and A.C.; funding acquisition, A.M.B., E.C., S.B. and A.C.; investigation, A.M.B., E.C., S.B. and A.C; methodology, A.M.B., E.C., S.B. and A.C.; project administration, N.D., N.A. and R.N.; resources, A.M.B., E.C., S.B., A.C., N.D., N.A. and R.N.; software, N.D., N.A. and R.N.; supervision, N.D., N.A. and R.N.; validation, N.D., N.A. and R.N.; visualization, N.D., N.A. and R.N.; roles/writing—original draft preparation, A.M.B., N.D., N.A. and R.N.; writing—review and editing, A.M.B., N.D., N.A. and R.N. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the principles of the Declaration of Helsinki. The research protocol was approved by the ethical committee of the University of Messina (Prot. 33-2020) on 29 June 2020.
Informed Consent Statement
Informed consent was obtained from all subjects involved in this study.
Data Availability Statement
The data presented in this study are available in the article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Nucera, R.; Lo Giudice, A.; Bellocchio, A.M.; Spinuzza, P.; Caprioglio, A.; Perillo, L.; Matarese, G.; Cordasco, G. Bone and cortical bone thickness of mandibular buccal shelf for mini-screw insertion in adults. Angle Orthod. 2017, 87, 745–751. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.P.; Tseng, Y.C. Miniscrew implant applications in contemporary orthodontics. Kaohsiung J. Med. Sci. 2014, 30, 111–115. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulos, M.A.; Tarawneh, F. The use of miniscrew implants for temporary skeletal anchorage in orthodontics: A comprehensive review. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2007, 103, e6–e15. [Google Scholar] [CrossRef]
- Nucera, R.; Bellocchio, A.M.; Oteri, G.; Farah, A.J.; Leonardi, R.; Cordasco, G.; Portelli, M. Bone and cortical bone characteristics of mandibular retromolar trigone and anterior ramus region for miniscrew insertion in adults. Am. J. Orthod. Dentofac. Orthop. 2019, 155, 330–338. [Google Scholar] [CrossRef] [PubMed]
- Araruna, R.d.C.; Vendrúscolo, D.M. [Nutrition of children with cleft lip and cleft palate, a bibliographic study]. Rev. Lat. Am. Enfermagem 2000, 8, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Nucera, R.; Costa, S.; Bellocchio, A.M.; Barbera, S.; Drago, S.; Silvestrini, A.; Migliorati, M. Evaluation of palatal bone depth, cortical bone, and mucosa thickness for optimal orthodontic miniscrew placement performed according to the third palatal ruga clinical reference. Eur. J. Orthod. 2022, 44, 530–536. [Google Scholar] [CrossRef] [PubMed]
- Nucera, R.; Ciancio, E.; Maino, G.; Barbera, S.; Imbesi, E.; Bellocchio, A.M. Evaluation of bone depth, cortical bone, and mucosa thickness of palatal posterior supra-alveolar insertion site for miniscrew placement. Prog. Orthod. 2022, 23, 18. [Google Scholar] [CrossRef] [PubMed]
- Ye, C.; Zhihe, Z.; Zhao, Q.; Ye, J. Treatment effects of distal movement of lower arch with miniscrews in the retromolar area compared with miniscrews in the posterior area of the maxillary. J. Craniofac. Surg. 2013, 24, 1974–1979. [Google Scholar] [CrossRef] [PubMed]
- Tepedino, M.; Cattaneo, P.M.; Niu, X.; Cornelis, M.A. Interradicular sites and cortical bone thickness for miniscrew insertion: A systematic review with meta-analysis. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 783–798.e20. [Google Scholar] [CrossRef]
- Papageorgiou, S.N.; Zogakis, I.P.; Papadopoulos, M.A. Failure rates and associated risk factors of orthodontic miniscrew implants: A meta-analysis. Am. J. Orthod. Dentofac. Orthop. 2012, 142, 577–595.e7. [Google Scholar] [CrossRef] [PubMed]
- Baumgaertel, S.; Hans, M.G. Assessment of infrazygomatic bone depth for mini-screw insertion. Clin. Oral Implant. Res. 2009, 20, 638–642. [Google Scholar] [CrossRef] [PubMed]
- Melo, A.C.; Andrighetto, A.R.; Hirt, S.D.; Bongiolo, A.L.; Silva, S.U.; Silva, M.A. Risk factors associated with the failure of miniscrews—A ten-year cross sectional study. Braz. Oral Res. 2016, 30, e124. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.W.; Park, J.H.; Bay, R.C.; Choi, S.K.; Chae, J.M. Cortical bone thickness and bone density effects on miniscrew success rates: A systematic review and meta-analysis. Orthod. Craniofac. Res. 2021, 24 (Suppl. S1), 92–102. [Google Scholar] [CrossRef] [PubMed]
- Janson, G.; Gigliotti, M.P.; Estelita, S.; Chiqueto, K. Influence of miniscrew dental root proximity on its degree of late stability. Int. J. Oral Maxillofac. Surg. 2013, 42, 527–534. [Google Scholar] [CrossRef] [PubMed]
- Ahn, H.W.; Kang, Y.G.; Jeong, H.J.; Park, Y.G. Palatal temporary skeletal anchorage devices (TSADs): What to know and how to do? Orthod. Craniofac. Res. 2021, 24 (Suppl. S1), 66–74. [Google Scholar] [CrossRef] [PubMed]
- Baumgaertel, S. Hard and soft tissue considerations at mini-implant insertion sites. J. Orthod. 2014, 41 (Suppl. S1), S3–S7. [Google Scholar] [CrossRef] [PubMed]
- Giudice, A.L.; Rustico, L.; Longo, M.; Oteri, G.; Papadopoulos, M.A.; Nucera, R. Complications reported with the use of orthodontic miniscrews: A systematic review. Korean J. Orthod. 2021, 51, 199–216. [Google Scholar] [CrossRef] [PubMed]
- Baumgaertel, S.; Tran, T.T. Buccal mini-implant site selection: The mucosal fallacy and zones of opportunity. J. Clin. Orthod. 2012, 46, 434–436. [Google Scholar] [PubMed]
- Poletti, L.; Silvera, A.A.; Ghislanzoni, L.T. Dentoalveolar class III treatment using retromolar miniscrew anchorage. Prog. Orthod. 2013, 14, 7. [Google Scholar] [CrossRef] [PubMed]
- Kuroda, S.; Yamada, K.; Deguchi, T.; Hashimoto, T.; Kyung, H.M.; Takano-Yamamoto, T. Root proximity is a major factor for screw failure in orthodontic anchorage. Am. J. Orthod. Dentofac. Orthop. 2007, 131, S68–S73. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.T.; Kim, Y.J.; Yang, K.S.; Lee, D.Y. Bone availability for mandibular molar distalization in adults with mandibular prognathism. Angle Orthod. 2018, 88, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.J.; Kim, J.W.; Choi, T.H.; Lee, K.J. Restoration of a vertical alveolar bone defect by orthodontic relocation of a mesially impacted mandibular first molar. Am. J. Orthod. Dentofac. Orthop. 2015, 147, S122–S132. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Zhang, H.; Smales, R.J.; Zhang, Y.; Ni, Y.; Ma, J.; Wang, L. Effect of 3 vertical facial patterns on alveolar bone quality at selected miniscrew implant sites. Implant Dent. 2014, 23, 92–97. [Google Scholar] [CrossRef] [PubMed]
- Musilli, M.; Marsico, M.; Romanucci, A.; Grampone, F. Molar uprighting with mini screws: Comparison among different systems and relative biomechanical analysis. Prog. Orthod. 2010, 11, 166–173. [Google Scholar] [CrossRef] [PubMed]
- Teekavanich, C.; Uezono, M.; Takakuda, K.; Ogasawara, T.; Techalertpaisarn, P.; Moriyama, K. Evaluation of Cortical Bone Microdamage and Primary Stability of Orthodontic Miniscrew Using a Human Bone Analogue. Materials 2021, 14, 1825. [Google Scholar] [CrossRef] [PubMed]
- Hung, E.; Oliver, D.; Kim, K.B.; Kyung, H.M.; Buschang, P.H. Effects of pilot hole size and bone density on miniscrew implants’ stability. Clin. Implant Dent. Relat. Res. 2012, 14, 454–460. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, M.; Deguchi, T.; Watanabe, H.; Seiryu, M.; Iikubo, M.; Sasano, T.; Fujiyama, K.; Takano-Yamamoto, T. Evaluation of optimal length and insertion torque for miniscrews. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 251–259. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Gao, J.; Sun, W.; Zhang, H.; Qin, W.; Jin, Z. Evaluation of alveolar bone morphology of incisors with different sagittal skeletal facial types by cone beam computed tomography: A retrospective study. Heliyon 2023, 9, e15369. [Google Scholar] [CrossRef] [PubMed]
- Nucera, R.; Lo Giudice, A.; Bellocchio, M.; Spinuzza, P.; Caprioglio, A.; Cordasco, G. Diagnostic concordance between skeletal cephalometrics, radiograph-based soft-tissue cephalometrics, and photograph-based soft-tissue cephalometrics. Eur. J. Orthod. 2017, 39, 352–357. [Google Scholar] [CrossRef] [PubMed]
- Fan, Z.; Zhang, Q.; Jiang, Y.; Qin, Q.; Huang, S.; Guo, J. Mandibular retromolar space in adults with different sagittal skeletal patterns. Angle Orthod. 2022, 92, 606–612. [Google Scholar] [CrossRef] [PubMed]
- Decaup, P.H.; Couture, C.; Garot, E. Is the distribution of cortical bone in the mandibular corpus and symphysis linked to loading environment in modern humans? A systematic review. Arch. Oral Biol. 2023, 152, 105718. [Google Scholar] [CrossRef]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).