1. Introduction
Class II malocclusion is a common occlusal disorder in the Caucasian population, characterized by a convex facial profile and caused by a combination of skeletal and dental components, each of which contributes to its characteristics and severity. Only a small percentage of cases exhibit maxillary skeletal protrusion. On the average, the maxilla is in a neutral position or even retruded, while the mandible is mostly retruded [
1].
So, the correction of dento-skeletal Class II malocclusion requires a comprehensive evaluation that includes both qualitative and quantitative analysis of the deviated elements. In addition to general diagnostic records such as photograph and radiograph, Fränkel’s maneuver [
2] is a crucial tool in this process, as it provides a clinical assessment of the subject and helps to identify the deviated elements.
The Fränkel maneuver involves protracting the mandible with half-closed lips until a proper canine Class I is achieved. The patient is then asked to close their lips, and the change in profile is evaluated to determine the most appropriate treatment strategy which may involve advancing the mandible, retracting the upper jaw, or a combination of both. However, this maneuver is based on occlusion, with the main focus on achieving a proper dental relation and only later evaluating the patient’s esthetics. This might be so because traditional therapies have limitations as they primarily affect the dentoalveolar component (70%) and only partially the skeletal component (30%) [
3,
4]. These limitations are due to anchorage loss with sagittal and vertical tooth movements, which are common with most of orthodontic appliances (proclination of lower incisors, lingual inclination of upper incisors, and clockwise rotation of the occlusal plane).
Indeed, a conventional functional treatment include a Pogonion advancement of at best 2 mm, a maxillary retraction of 1 mm, and a clockwise rotation of the mandibular plane (1° on average) [
5]. However, this might result in some cases in an aesthetically unacceptable correction, especially when a greater mandibular advancement is required, and maxillary retraction is undesirable.
Another critical factor in treating Class II malocclusions in growing patients is the overjet. In an ideal occlusion, the overjet is defined as the distance between the buccal surface of the lower central incisor and the palatal surface of the upper one. However, in the presence of a Class II malocclusion, the overjet might be considered as the minimum distance between the buccal surface of the lower six front teeth and the palatal surface of the upper ones, which is usable for mandibular advancement.
In fact, the extent of mandibular advancement will depend mainly on the initial overjet and the ability to maintain or increase it during the treatment [
6]. Therapies involving a large initial overjet or having the potential to create one (such as proclination of the incisors for correction of Class II Division II) are likely to achieve a significant mandibular advancement, with a high probability of success [
7].
2. Compliance
The success of Class II correction therapy also depends on patient cooperation. While numerous therapies have been proposed, including fixed and removable functional appliances and Class II elastics, patient compliance is known to be a challenge (in many cases, compliance is estimated to be between 27 and 37% for treatments that rely on the patient) [
8,
9,
10,
11]. Considering this, fixed functional appliances, such as the Herbst appliance, are particularly valuable in achieving a successful outcome.
3. Notes on Skeletal and Dentolaveolar Effects
Despite its original design [
12] being limited to severe Class II malocclusions and uncooperative patients, the clinical management of Herbst appliance has been modified in recent years and now boasts a higher success rate.
The traditional Herbst appliance, like other functional devices including Class II elastics, has both dentoalveolar and skeletal effects related to direction of the applied forces [
13]. The distalization of the upper arch and a slowdown in the forward growth of the maxilla (by approximately −0.4 to 1 mm due to the extraoral traction effect) [
14,
15] are combined with mesialization of the lower arch and mandibular advancement, resulting in a statistically significant but clinically insignificant Pog advancement of 1.45 to 1.91 mm [
16]. Alveolodental movements, caused by a reciprocal loss of anchorage, are more prevalent (70–80%) compared to skeletal movements (20–30%), with variations depending on the treatment period (pre-peak, peak, post-peak) and the extent of the original malocclusion.
So, the skeletal effects of the Herbst appliance are limited by the alveolodental movements in both the vertical and sagittal planes [
16,
17,
18]. In the upper arch, the molars intrude and distalize, while the incisors extrude and lingualize (by approximately 1.5 to 3.5 mm on average) [
14,
15]; in the lower arch, the molars extrude and mesialize and the incisors intrude and buccally flare (with an average proclination of 7.5 to 10.5°) [
5,
7]. This results in a rapid overjet reduction and a clockwise rotation of the occlusal plane and of the mandible, losing some of the mandibular advancement.
This effect can be controlled with the use of a full-coverage resin splint, making Herbst therapy possible even for patients with increased vertical dimension and improving the anchorage, although the results are partial.
4. The Skeletal Anchorage
If the movement of teeth interfere with the sagittal advancement of the mandible, reducing these movements with skeletal anchorage could result in a better Class II aesthetic correction.
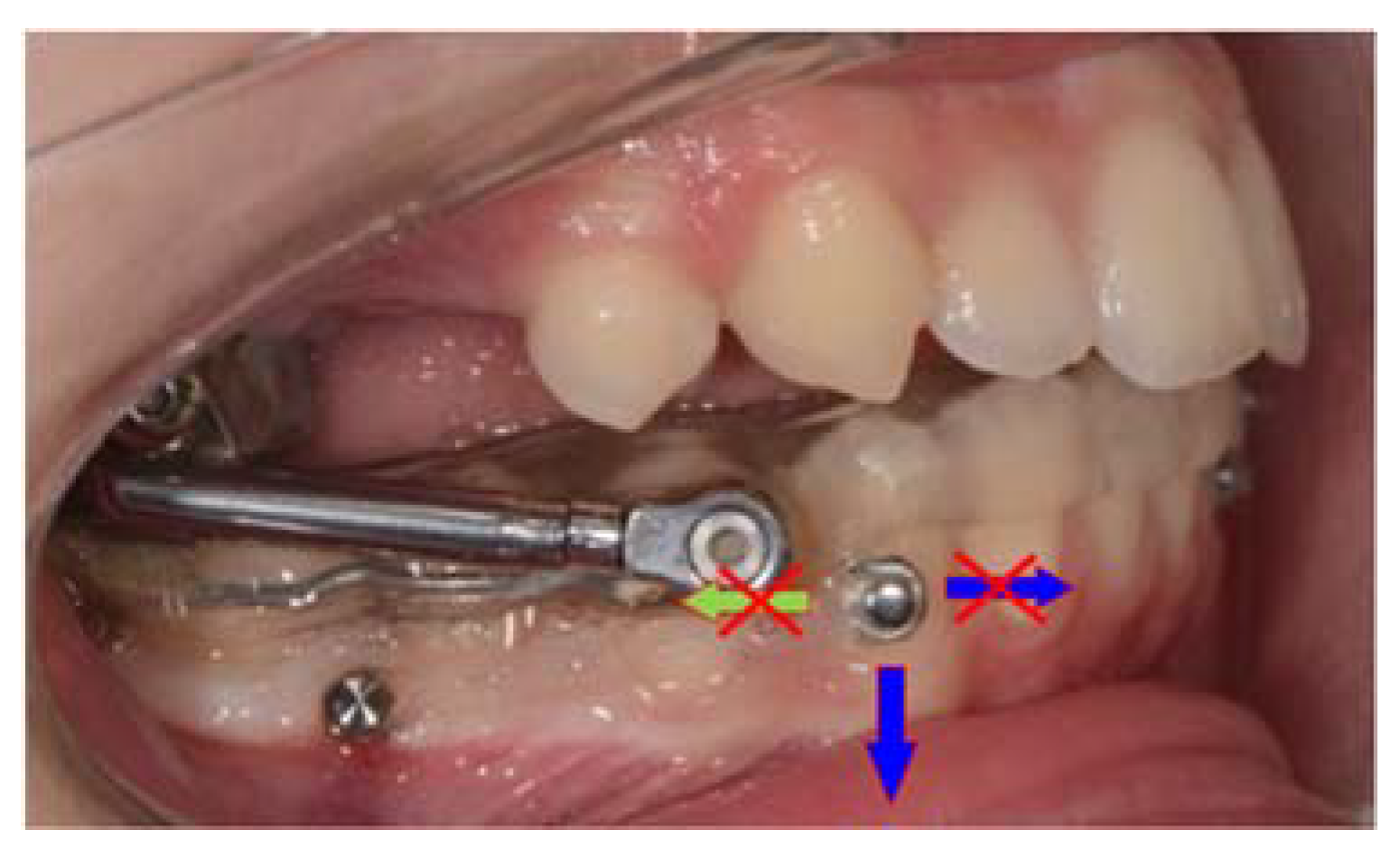
Anchorage in the lower arch involves the use of a resin splint, buccal miniscrews, and elastic ligatures (
Figure 1 and
Figure 2). The miniscrews are placed bilaterally between the first molar and second lower premolar, with the head positioned in the attached gingiva or on the mucogingival line. Two bondable buttons are placed on the buccal surface of the canines and connected to the miniscrews through elastic ligatures of 150–200 g. This configuration, combined with the splint, prevents molar mesialization and proclination of the incisors and enables effective control of the entire arch. The elastic ligatures should be parallel to the occlusal plane and replaced every 4 weeks. In addition, splinting the lower six frontal elements can prevent rotation, distalization, and intrusion of the canines caused by elastic traction.
This technique results in a greater skeletal effect, an average reduction in the gonial angle by 1.3–1.5°, a counterclockwise rotation of the mandible, and greater advancement of the Pog of 3.8–4.0 mm [
19,
20].
Moreover, when distalization of the upper arch with opening of Nasolabial angle is undesired, a similar anchorage reinforcement is required also in the upper arch (
Figure 3 and
Figure 4). The arch is stabilized by the fixed appliances, with the transverse dimension blocked by the palatal arch of the Herbst appliance. The miniscrews are placed bilaterally between the first premolar and canine or, in some cases, between the second and first premolar. Elastic ligatures are stretched from the miniscrews to first molar bands, in a horizontal direction. This configuration reduces distalization of the molars and lingualization of the upper incisors, preserving the overjet, limiting the opening of nasolabial angle, and improving the aesthetic outcome also in biretruded Class II patients.
To date, a pilot study showed an average Pog advancement of 5.7 mm with the use of Herbst MTH, 4 buccal miniscrews, and elastic ligatures [
20].
Moreover, anchorage in the upper arch can be similarly managed using palatal miniscrews instead of buccal ones, increasing the potential of the technique.
5. A New Diagnostic Approach
Skeletal anchorage has increased the percentage of skeletal correction from 30 to 70%, with the ability to selectively modify individual components of the Class II malocclusion [
19,
20]. Traditional techniques facilitate the retraction of the maxilla or simultaneous retraction of the maxilla and advancement of the mandible, but not separately and not in a clinically significant manner. With the addition of skeletal anchorage, it is now possible to selectively (a) retract the maxilla; (b) advance the maxilla; (c) retract the maxilla and advance the mandible in a clinically significant manner; and (d) advance the mandible in a clinically significant manner.
This has led to a new diagnostic approach, considering more facial aesthetics rather than occlusal relation. As a result, Fränkel’s maneuver has been modified with a new maneuver known as Manni’s Aesthetic maneuver, which places most importance on aesthetics: basically, the patient is asked to bring the mandible forward until an aesthetically optimal position is achieved with closed lips (not open as in traditional Fränkel’s maneuver). Only after he is asked to open the lips to evaluate the occlusal relation. So, the decision of the optimal skeletal position is based on aesthetic0073 rather than occlusion, with much emphasis placed on the nasolabial angle, lips, maxillary, and mandibular sagittal position, evaluated through clinical and photographic analysis.
6. Conclusions
A proper Skeletal Class II treatment requires specific focus on patient aesthetics.
Skeletal anchorage facilitates a reduction in dental compensations and increased skeletal effects of orthopedic therapy [
21,
22].
The combination of the Herbst MTH appliance with elastic ligatures and skeletal anchorage in the lower, or both lower and upper arch, represent an effective and efficient therapy in the management of Class II malocclusion, with the possibility of modulating the effects on the maxilla and mandible.
The presence of a mandibular splint provides increased control of verticality and limits post-rotation of the occlusal and mandibular plane, with significant effects on Pogonion projection [
23].
Achieving and maintaining a functional overjet to the mandibular advancement is the key to a successful treatment.
However, these conclusions should be interpreted with caution, as currently available research is not enough appropriate to determine the long-term effects of such a treatment, and further well-designed randomized clinical trials are needed to confirm these results.
Author Contributions
Conceptualization, A.M. and A.B.; methodology, A.M. and A.B.; software, S.P.; validation, A.M., M.C. and G.G.; formal analysis, A.B. and S.P.; investigation, A.M.; resources, A.M.; writing—original draft preparation, S.P.; writing—review and editing, A.B.; visualization, S.P.; supervision, M.C. and G.G.; project administration, G.G. and M.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study since it turns out to be an opinion.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- McNamara, J.A., Jr. Components of Class II malocclusion in children 8–10 years of age. Angle Orthod. 1981, 51, 177–202. [Google Scholar] [CrossRef] [PubMed]
- Fränkel, R.; Fränkel, C. Orofacial Orthopedics with the Function Regulator; Karger Publishers: Basel, Switzerland, 1989. [Google Scholar]
- Bock, N.C.; Gnandt, E.; Ruf, S. Occlusal stability after Herbst treatment of patients with retrognathic and prognathic facial types: A pilot study. J. Orofac. Orthop. 2016, 77, 160–167. [Google Scholar] [CrossRef] [PubMed]
- VanLaecken, R.; Martin, C.A.; Dischinger, T.; Razmus, T.; Ngan, P. Treatment effects of the edgewise Herbst appliance: A cephalometric and tomographic investigation. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 582–593. [Google Scholar] [CrossRef] [PubMed]
- Valant, J.R.; Sinclair, P.M. Treatment effects of the Herbst appliance. Am. J. Orthod. Dentofac. Orthop. 1989, 95, 138–147. [Google Scholar] [CrossRef] [PubMed]
- Pancherz, H. The Herbst appliance—Its biologic effects and clinical use. Am. J. Orthod. 1985, 87, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Casutt, C.; Pancherz, H.; Gawora, M.; Ruf, S. Success rate and efficiency of activator treatment. Eur. J. Orthod. 2007, 29, 614–621. [Google Scholar] [CrossRef] [PubMed]
- Čirgić, E.; Kjellberg, H.; Hansen, K. Treatment of large overjet in Angle Class II: Division 1 malocclusion with Andresen activators versus prefabricated functional appliances—A multicenter, randomized, controlled trial. Eur. J. Orthod. 2016, 38, 516–524. [Google Scholar] [CrossRef]
- Arreghini, A.; Trigila, S.; Lombardo, L.; Siciliani, G. Objective assessment of compliance with intra- and extraoral removable appliances. Angle Orthod. 2017, 87, 88–95. [Google Scholar] [CrossRef]
- Veeroo, H.J.; Cunningham, S.J.; Newton, J.T.; Travess, H.C. Motivation and compliance with intraoral elastics. Am. J. Orthod. Dentofac. Orthop. 2014, 146, 33–39. [Google Scholar] [CrossRef]
- Schiöth, T.; Von Bremen, J.; Pancherz, H.; Ruf, S. Complications during Herbst Appliance Treatment with Reduced Mandibular Cast Splints: A prospective, clinical multicenter study. J. Orofac. Orthop. 2007, 68, 321–327. [Google Scholar] [CrossRef]
- Pancherz, H. The mechanism of Class II correction in Herbst appliance treatment: A cephalometric investigation. Am. J. Orthod. 1982, 82, 104–113. [Google Scholar] [CrossRef] [PubMed]
- LeCornu, M.; Cevidanes, L.H.; Zhu, H.; Wu, C.-D.; Larson, B.; Nguyen, T. Three-dimensional treatment outcomes in Class II patients treated with the Herbst appliance: A pilot study. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 818–830. [Google Scholar] [CrossRef] [PubMed]
- Pancherz, H.; Fackel, U. The skeletofacial growth pattern pre-and post-dentofacial orthopaedics. A long-term study of Class II malocclusions treated with the Herbst appliance. Eur. J. Orthod. 1990, 12, 209–218. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Zhu, Y.; Long, H.; Zhou, Y.; Jian, F.; Ye, N.; Gao, M.; Lai, W. The effectiveness of the Herbst appliance for patients with Class II malocclusion: A meta-analysis. Eur. J. Orthod. 2016, 38, 324–333. [Google Scholar] [CrossRef] [PubMed]
- Sangalli, K.L.; Dutra-Horstmann, K.L.; Correr, G.M.; Topolski, F.; Flores-Mir, C.; Lagravère, M.O.; Moro, A. Three-dimensional skeletal and dentoalveolar sagittal and vertical changes associated with cantilever Herbst appliance in prepubertal patients with Class II malocclusion. Am. J. Orthod. Dentofac. Orthop. 2022, 161, 638–651.e1. [Google Scholar] [CrossRef] [PubMed]
- Hägg, U.; Pancherz, H. Dentofacial orthopaedics in relation to chronological age, growth period and skeletal development. An analysis of 72 male patients with Class II division 1 malocclusion treated with the Herbst appliance. Eur. J. Orthod. 1988, 10, 169–176. [Google Scholar] [CrossRef]
- Manni, A.; Mutinelli, S.; Cerruto, C.; Cozzani, M. Influence of incisor position control on the mandibular response in growing patients with skeletal Class II malocclusion. Am. J. Orthod. Dentofac. Orthop. 2021, 159, 594–603. [Google Scholar] [CrossRef]
- Manni, A.; Mutinelli, S.; Pasini, M.; Mazzotta, L.; Cozzani, M. Herbst appliance anchored to miniscrews with 2 types of ligation: Effectiveness in skeletal Class II treatment. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 871–880. [Google Scholar] [CrossRef]
- Manni, A.; Migliorati, M.; Calzolari, C.; Silvestrini-Biavati, A. Herbst appliance anchored to miniscrews in the upper and lower arches vs standard Herbst: A pilot study. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 617–625. [Google Scholar] [CrossRef]
- Al-Dboush, R.; Soltan, R.; Rao, J.; El-Bialy, T. Skeletal and dental effects of Herbst appliance anchored with temporary anchorage devices: A systematic review with meta-analysis. Orthod. Craniofacial Res. 2021, 25, 31–48. [Google Scholar] [CrossRef]
- Huang, Y.; Sun, W.; Xiong, X.; Zhang, Z.; Liu, J.; Wang, J. Effects of fixed functional appliances with temporary anchorage devices on Class II malocclusion: A systematic review and meta-analysis. J. World Fed. Orthod. 2021, 10, 59–69. [Google Scholar] [CrossRef] [PubMed]
- Manni, A.; Pasini, M.; Mazzotta, L.; Mutinelli, S.; Nuzzo, C.; Grassi, F.R.; Cozzani, M. Comparison between an Acrylic Splint Herbst and an Acrylic Splint Miniscrew-Herbst for Mandibular Incisors Proclination Control. Int. J. Dent. 2014, 2014, 173187. [Google Scholar] [CrossRef] [PubMed]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).