Effects of Ceramic Translucency and Thickness on Polymerization of a Photosensitive Resin Cement
Abstract
1. Introduction
2. Materials and Methods
2.1. Specimen Preparation
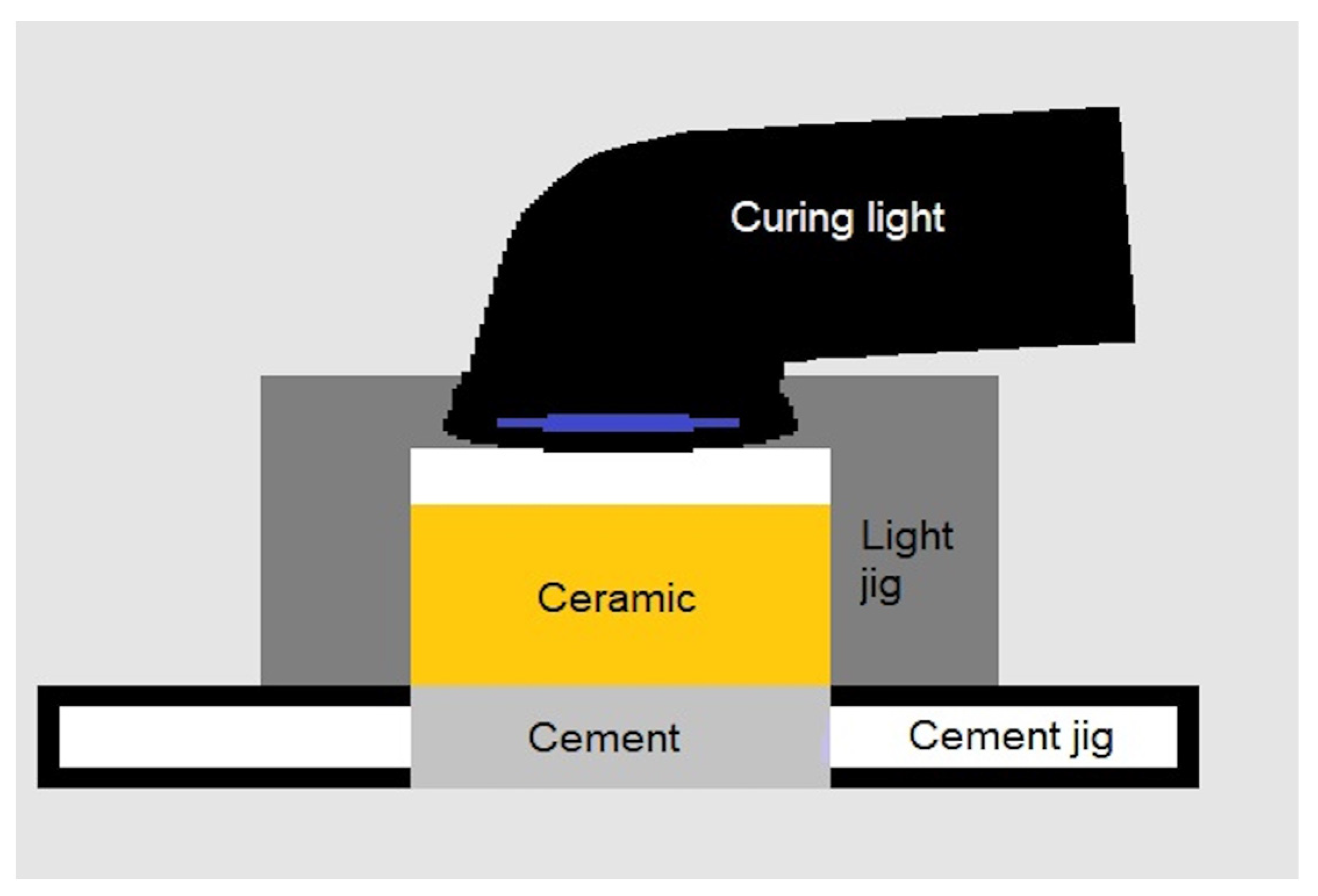
2.2. Curing Jigs
2.3. Light-Curing Protocol
2.4. Measurement of Resin Polymerization
2.5. Statistical Analysis
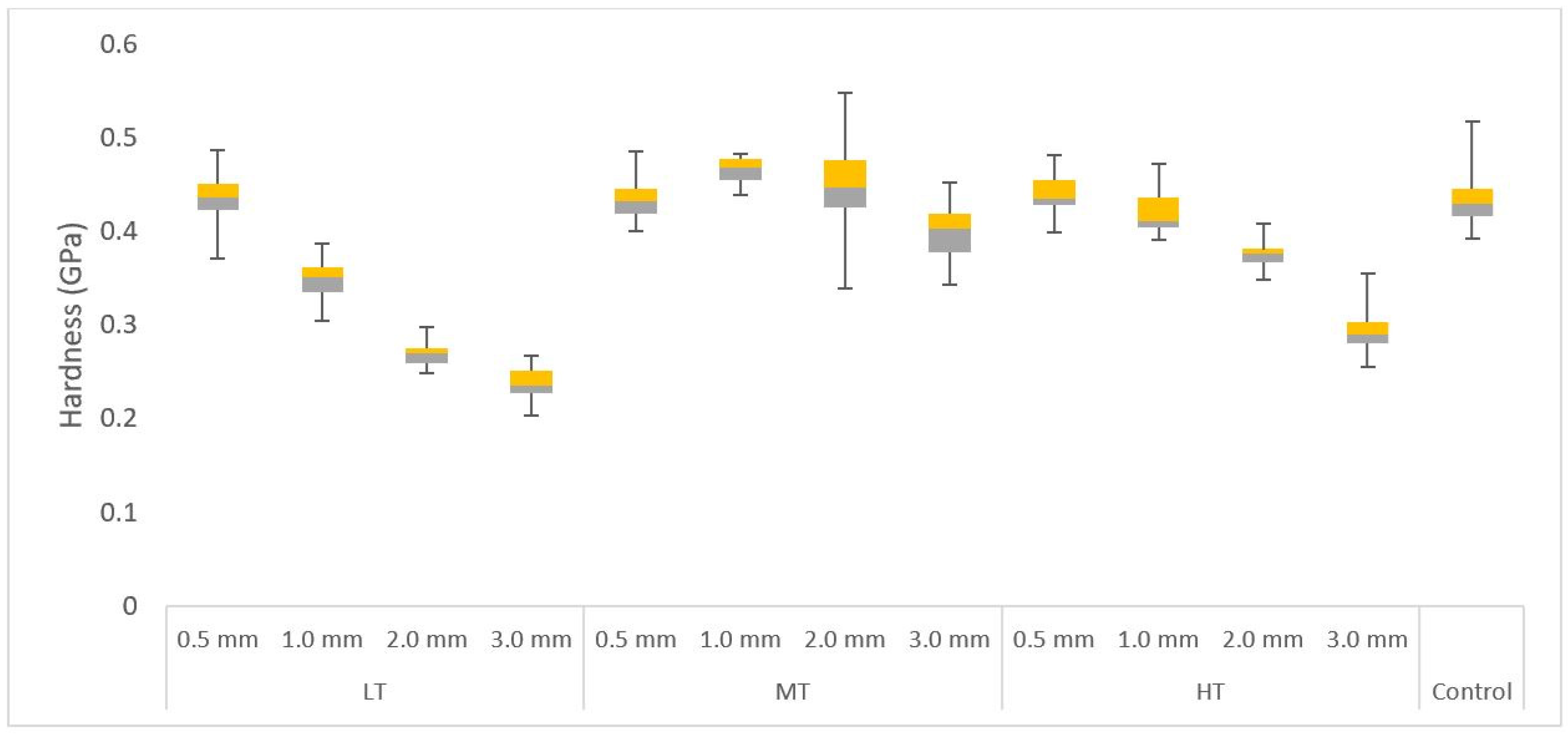
3. Results
4. Discussion
5. Conclusions
- The thickness of low- and high-translucency lithium disilicate ceramics negatively affects the polymerization of light-cured resin cement.
- The thickness of ceramic materials has a greater effect on the polymerization of light-cured resin cement than translucency.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jurado, C.A.; Villalobos-Tinoco, J.; Tsujimoto, A.; Castro, P.; Torrealba, Y. The art of minimal tooth reduction for veneer restorations. Eur. J. Gen. Dent. 2020, 9, 45–52. [Google Scholar] [CrossRef]
- Ritter, A.V.; Baratieri, L.N. Ceramic restorations for posterior teeth: Guidelines for the clinician. J. Esthet. Restor. Dent. 1999, 11, 72–86. [Google Scholar] [CrossRef] [PubMed]
- Brodbelt, R.H.W.; O’Brien, W.J.; Fan, P.L. Translucency of dental porcelains. J. Dent. Res. 1980, 59, 70–75. [Google Scholar] [CrossRef] [PubMed]
- Assaf, A.; Azer, S.S.; Sfeir, A.; Al-Haj Husain, N.; Özcan, M. Risk Factors with Porcelain Laminate Veneers Experienced during Cementation: A Review. Materials 2023, 16, 4932. [Google Scholar] [CrossRef] [PubMed]
- Bonna, A.B.; Kelly, J.R. The clinical success of all-ceramic restorations. J. Prosthodont. 2008, 139, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Aziz, A.; El-Mowafy, O. Six-year clinical performance of lithium disilicate glass-ceramic CAD-CAM versus metal-ceramic crowns. J. Adv. Prosthodont. 2023, 15, 44. [Google Scholar] [CrossRef] [PubMed]
- Gierthmuehlen, P.C.; Spitznagel, F.A.; Koschate, M.; Bonfante, E.A.; Prott, L.S. Influence of ceramic thickness and dental substrate on the survival rate and failure load of non-retentive occlusal veneers after fatigue. J. Esthet. Restor. Dent. 2023, 1–8. [Google Scholar] [CrossRef]
- Dapieve, K.S.; Pereira, G.K.; Venturini, A.B.; Daudt, N.; Valcanaia, A.; Bottino, M.C.; Valandro, L.F. Do resin cement viscosity and ceramic surface etching influence the fatigue performance of bonded lithium disilicate glass-ceramic crowns? Dent. Mater. 2022, 38, e59–e67. [Google Scholar] [CrossRef]
- Blatz, M.B.; Sadan, A.; Kern, M. Resin-ceramic bonding: A review of the literature. J. Prosthet. Dent. 2003, 89, 268–274. [Google Scholar] [CrossRef]
- Braga, R.R.; Cesar, P.F.; Gonzaga, C.C. Mechanical properties of resin cements with different activation modes. J. Oral Rehabil. 2002, 29, 257–262. [Google Scholar] [CrossRef]
- Sunico-Segarra, M.; Segarra, A. A Practical Clinical Guide to Resin Cements; Springer: Berlin, Germany, 2014. [Google Scholar]
- Anusavice, K.J.; Phillips, R.W.; Shen, C.; Rawls, H.R. Phillip’s Science of Dental Materials, 12th ed.; Elsevier/Saunders: St. Louis, MO, USA, 2013. [Google Scholar]
- Strang, R.; Macdonald, I.; O’Hagan, S.; Murray, J.; Stephen, K.W. Variations in performance of curing light units by determination of composite resin setting time. Br. Dent. J. 1987, 162, 63–65. [Google Scholar] [CrossRef]
- Flury, S.; Lussi, A.; Hickel, R.; Ilie, N. Light curing through glass ceramics with a second- and a third-generation LED curing unit: Effect of curing mode on the degree of conversion of dual-curing resin cements. Clin. Oral Investig. 2013, 17, 2127–2137. [Google Scholar] [CrossRef] [PubMed]
- El-Badrawy, W.A.; El-Mowafy, O.M. Chemical versus dual curing of resin inlay cements. J. Prosthet. Dent. 1995, 73, 515–524. [Google Scholar] [CrossRef]
- Pissaia, J.F.; Guanaes, B.K.; Kintopp, C.C.; Correr, G.M.; da Cunha, L.F.; Gonzaga, C.C. Color stability of ceramic veneers as a function of resin cement curing mode and shade: 3-year follow-up. PLoS ONE 2019, 14, e0219183. [Google Scholar] [CrossRef]
- Ferracane, J.L. Correlation between hardness and degree of conversion during the setting reaction of unfilled dental restorative resins. Dent. Mater 1985, 1, 11–14. [Google Scholar] [CrossRef] [PubMed]
- Kilinc, E.; Antonson, S.A.; Hardigan, P.C.; Kesercioglu, A. The effect of ceramic restoration shade and thickness on the polymerization of light- and dual-cure resin cements. Oper. Dent. 2011, 36, 661–669. [Google Scholar] [CrossRef]
- Ilie, N.; Hickel, R. Correlation between ceramics translucency and polymerization efficiency through ceramics. Dent. Mater. 2008, 24, 908–914. [Google Scholar] [CrossRef] [PubMed]
- Aldryhim, H.; El-Mowafy, O.; McDermott, P.; Prakki, A. Hardness of resin cements polymerized through glass-ceramic veneers. Dent. J. 2021, 9, 92. [Google Scholar] [CrossRef]
- Wang, F.; Takahashi, H.; Iwasaki, N. Translucency of dental ceramics with different thicknesses. J. Prosthet. Dent. 2013, 110, 14–20. [Google Scholar] [CrossRef]
- Pilo, R.; Cardash, H.S. Post-irradiation polymerization of different anterior and posterior visible light-activated resin composites. Dent. Mater. 1992, 8, 299–304. [Google Scholar] [CrossRef]
- Shenoy, A.; Shenoy, N. Dental ceramics: An update. J. Conserv. Dent. 2010, 13, 195–203. [Google Scholar] [CrossRef]
- Al Ben Ali, B.; Kang, K.; Finkelman, M.D.; Zandparsa, R.; Hirayama, H. The effect of variations in translucency and background on colour differences in CAD/CAM lithium disilicate glass ceramics. J. Prosthodont. 2014, 23, 213–220. [Google Scholar] [CrossRef]
- Denry, I.; Holloway, J.A. Ceramics for dental applications: A review. Materials 2010, 3, 351–368. [Google Scholar] [CrossRef]
- Tsukuma, K.; Yamashita, I.; Kusunose, T. Transparent 8 mol% Y2O3-ZrO2 (8Y) ceramics. J. Am. Ceram. Soc. 2008, 91, 813–818. [Google Scholar] [CrossRef]
- O’Keefe, K.L.; Pease, P.L.; Herrin, H.K. Variables affecting the spectral transmittance of light through porcelain veneer samples. J. Prosthet. Dent. 1991, 66, 434–438. [Google Scholar] [CrossRef]
- Peixoto, R.T.; Paulinelli, V.M.; Sander, H.H.; Lanza, D.M.; Cury, L.A.; Poletto, L.T. Light transmission through porcelain. Dent. Mater. 2007, 23, 1363–1368. [Google Scholar] [CrossRef]
- Yuh, C.-S.; Kim, J.-H.; Kim, S.-J.; Lee, Y.-K.; Shim, J.-S. Comparison of the degree of conversion of light-cured resin cement in regard to porcelain laminate thickness, light source and curing time using FT-IR. J. Korean Acad. Prosthodont. 2009, 47, 416–423. [Google Scholar] [CrossRef]
- Furuse, A.Y.; Glir, D.H.; Rizzante, F.A.; Prochnow, R.; Borges, A.F.; Gonzaga, C.C. Degree of conversion of a flowable composite light-activated through ceramics of different shades and thicknesses. Br. J. Oral Sci. 2015, 14, 230–233. [Google Scholar] [CrossRef][Green Version]
- Donmez, M.B.; Yucel, M.T. Effect of monolithic CAD-CAM ceramic thickness on resin cement polymerization: An in-vitro study. Am. J. Dent. 2019, 32, 240–244. [Google Scholar] [PubMed]
- Liporoni, P.C.; Ponce, A.C.; de Freitas, M.R.; Zanatta, R.F.; Pereira, M.C.; Catelan, A. Influence of thickness and translucency of lithium disilicate ceramic on degree of conversion of resinous materials. J. Clin. Exp. Dent. 2020, 12, e745–e748. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, G.R.; Simamoto-Junior, P.C.; Da Mota, A.S.; Soares, C.J. Mechanical properties of light-curing composites polymerized with different laboratory photo-curing units. Dent. Mater. J. 2007, 26, 217–223. [Google Scholar] [CrossRef]
- Da Rocha Svizero, N.; Silva, M.S.; Alonso, R.C.; Rodrigues, F.P.; Di Hipólito, V.; Carvalho, R.M.; D’Alpino, P.H. Effects of curing protocols on fluid kinetics and hardness of resin cements. Dent. Mater. J. 2013, 32, 32–41. [Google Scholar] [CrossRef] [PubMed]
- Ortiz-Magdaleno, M.; Bogarin-Topete, E.R.; Cerda-Cristerna, B.I.; Gutiérrez-Sánchez, M. Effect of degree of conversion on the surface properties of polymerized resin cements used for luting glass fiber posts. J. Prosth Dent. 2023, 130, 256.e1–256.e12. [Google Scholar] [CrossRef]
- De Jesus, R.H.; Quirino, A.S.; Salgado, V.; Cavalcante, L.M.; Palin, W.M.; Schneider, L.F. Does ceramic translucency affect the degree of conversion of luting agents? Appl. Adhes. Sci. 2020, 8, 4. [Google Scholar] [CrossRef]
- Dewald, J.P.; Ferracane, J.L. A comparison of four modes of evaluating depth of cure of light-activated composites. J. Dent. Res. 1987, 66, 727–730. [Google Scholar] [CrossRef]
- Vohra, F.; Al-Rifaiy, M.; Al Qahtani, M. Factors affecting resin polymerization of bonded all ceramic restorations. Review of literature. J. Dow Univ. Health Sci. 2013, 7, 80–86. [Google Scholar]
- Cardash, H.S.; Baharav, H.; Pilo, R.; Ben-Amar, A. The effect of porcelain color on the hardness of luting composite resin cement. J. Prosthet. Dent. 1993, 69, 620–623. [Google Scholar] [CrossRef] [PubMed]
- Boitelle, P.; Mawussi, B.; Tapie, L.; Fromentin, O. A systematic review of CAD/CAM fit restoration evaluations. J. Oral Rehabil. 2014, 41, 853–874. [Google Scholar] [CrossRef]

| Content | |
|---|---|
| Filler Content | Zirconia and fumed silica |
| Monomer | TEGDMA/BisGMA |
| Thickness | |||||
|---|---|---|---|---|---|
| 0.5 mm | 1.0 mm | 2.0 mm | 3.0 mm | ||
| Translucency | LT | 0.44 (0.03) | 0.35 (0.02) | 0.27 (0.01) | 0.24 (0.02) |
| MT | 0.44 (0.02) | 0.47 (0.01) | 0.45 (0.06) | 0.40 (0.03) | |
| HT | 0.44 (0.02) | 0.42 (0.02) | 0.38 (0.01) | 0.29 (0.02) | |
| Control | 0.44 (0.03) | ||||
| Translucency | Thickness | p-Value |
|---|---|---|
| LT | 0.5 mm | 0.74 |
| 1.0 mm | <0.001 | |
| 2.0 mm | <0.001 | |
| 3.0 mm | <0.001 | |
| MT | 0.5 mm | 0.92 |
| 1.0 mm | <0.001 | |
| 2.0 mm | 0.40 | |
| 3.0 mm | <0.001 | |
| HT | 0.5 mm | 0.44 |
| 1.0 mm | 0.07 | |
| 2.0 mm | <0.001 | |
| 3.0 mm | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barazanchi, A.; Abduo, J.; Lee, Y.M.-J.; Lee, M.-S.; Li, K.C. Effects of Ceramic Translucency and Thickness on Polymerization of a Photosensitive Resin Cement. Oral 2023, 3, 490-498. https://doi.org/10.3390/oral3040040
Barazanchi A, Abduo J, Lee YM-J, Lee M-S, Li KC. Effects of Ceramic Translucency and Thickness on Polymerization of a Photosensitive Resin Cement. Oral. 2023; 3(4):490-498. https://doi.org/10.3390/oral3040040
Chicago/Turabian StyleBarazanchi, Abdullah, Jaafar Abduo, Yvonne Min-Joo Lee, Min-Suk Lee, and Kai Chun Li. 2023. "Effects of Ceramic Translucency and Thickness on Polymerization of a Photosensitive Resin Cement" Oral 3, no. 4: 490-498. https://doi.org/10.3390/oral3040040
APA StyleBarazanchi, A., Abduo, J., Lee, Y. M.-J., Lee, M.-S., & Li, K. C. (2023). Effects of Ceramic Translucency and Thickness on Polymerization of a Photosensitive Resin Cement. Oral, 3(4), 490-498. https://doi.org/10.3390/oral3040040






