Masticatory Functionality in Post-Acute-COVID-Syndrome (PACS) Patients with and without Sarcopenia
Abstract
1. Introduction
2. Materials and Methods
2.1. Short Medical History Interview
2.2. Anatomo-Functional Analysis
2.3. Intra-Oral Examination
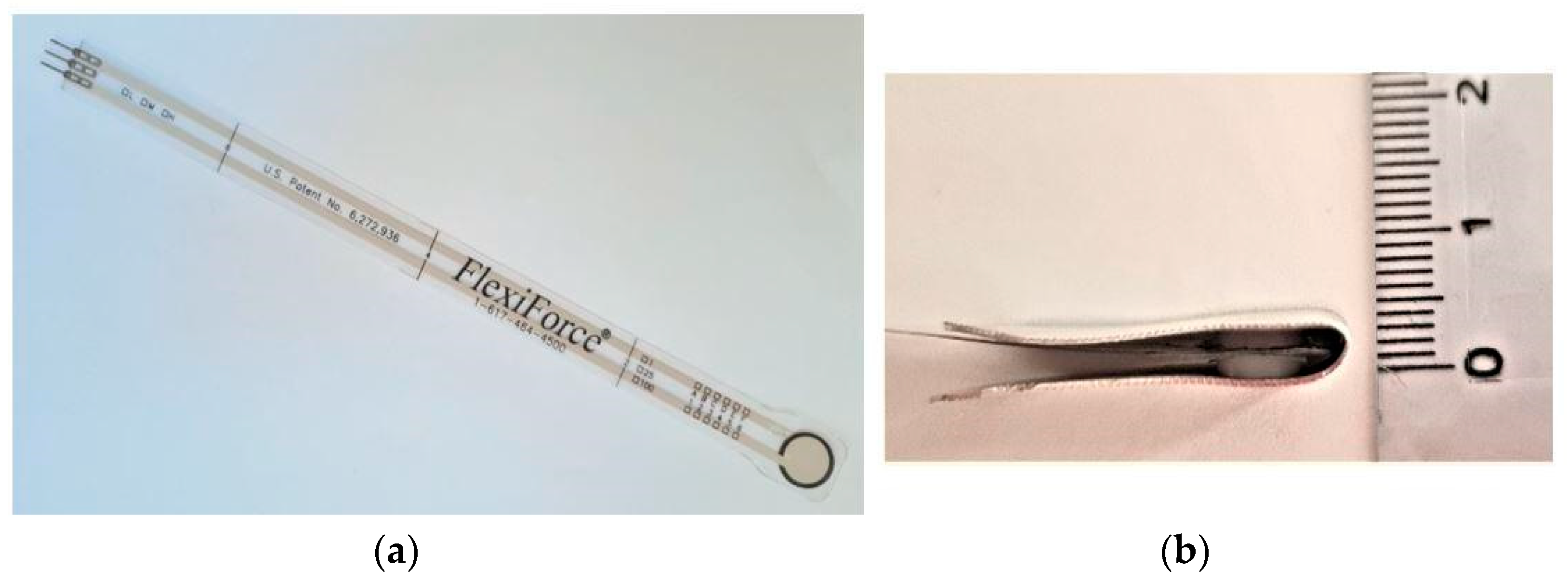
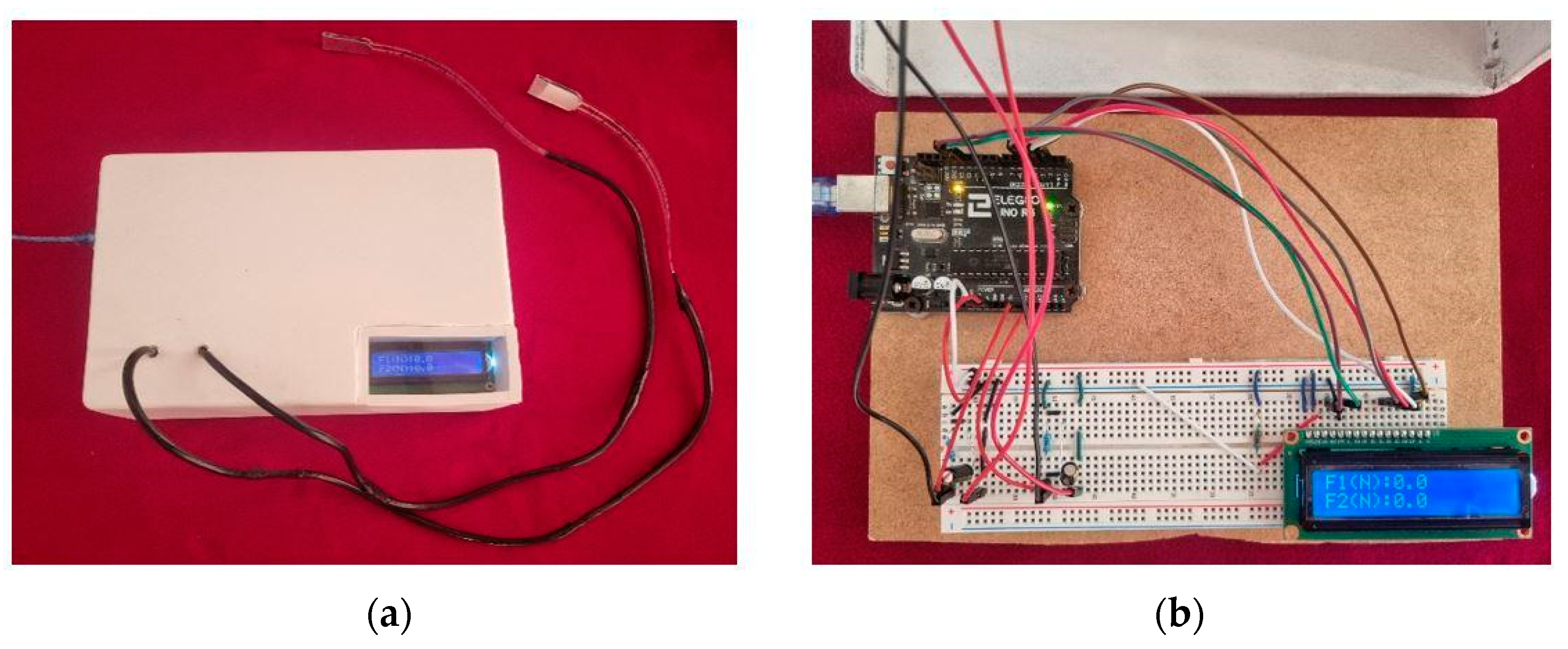
2.4. Bite Force Measurement
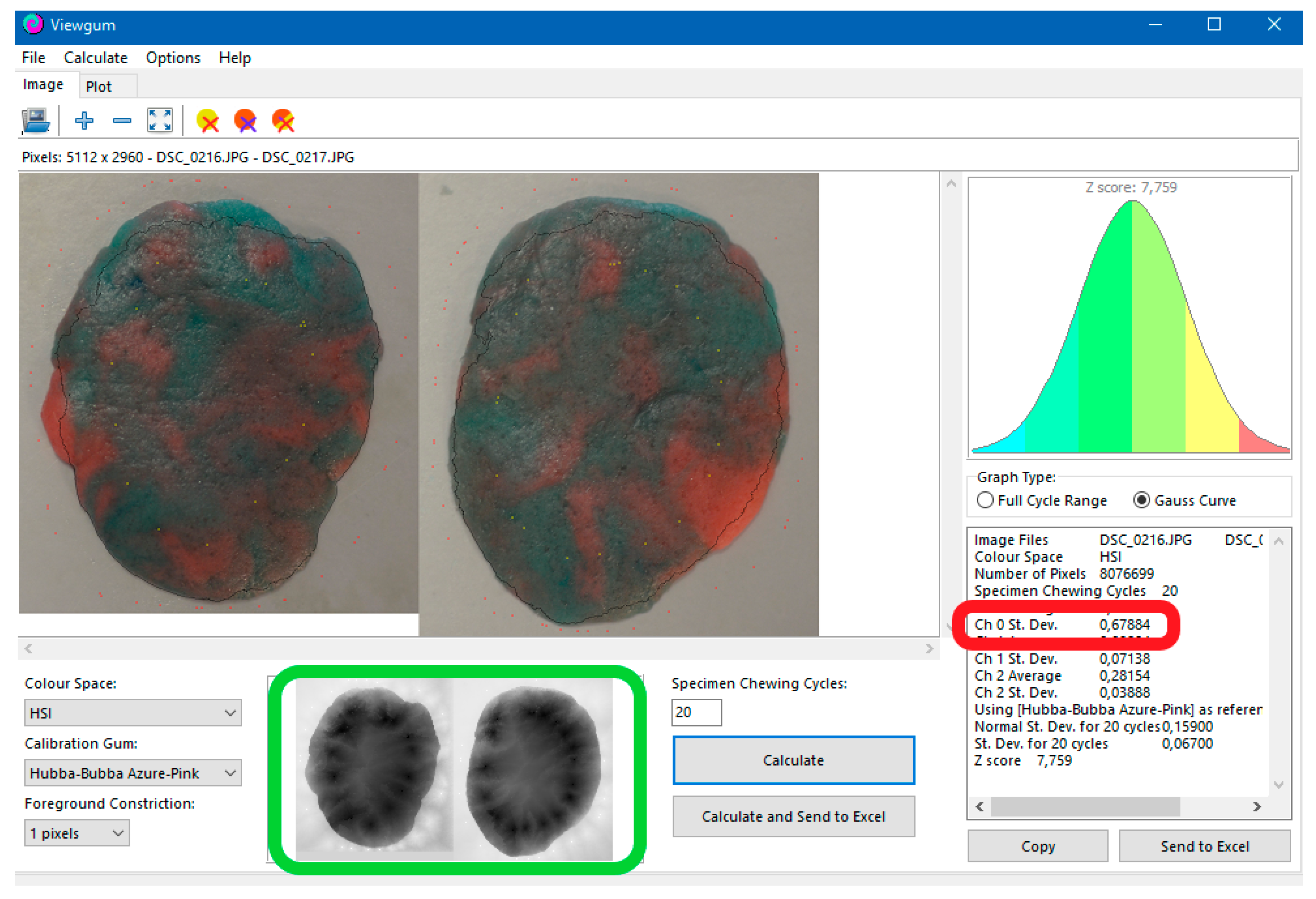
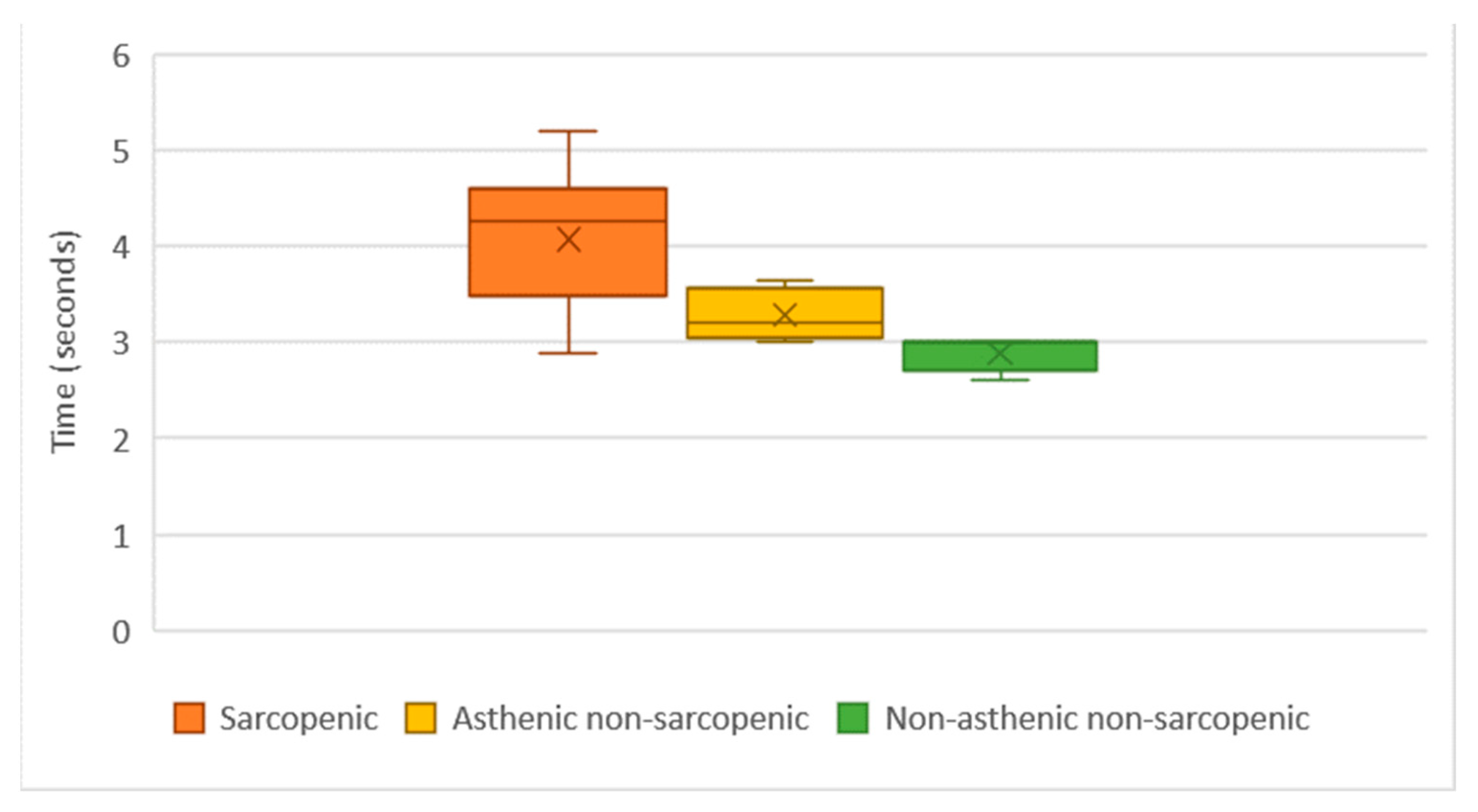
2.5. Chewing Gum Mixing Ability Test
2.6. Statistical Analysis
3. Results
3.1. Short Medical History Interview
3.2. Anatomo-Functional Analysis
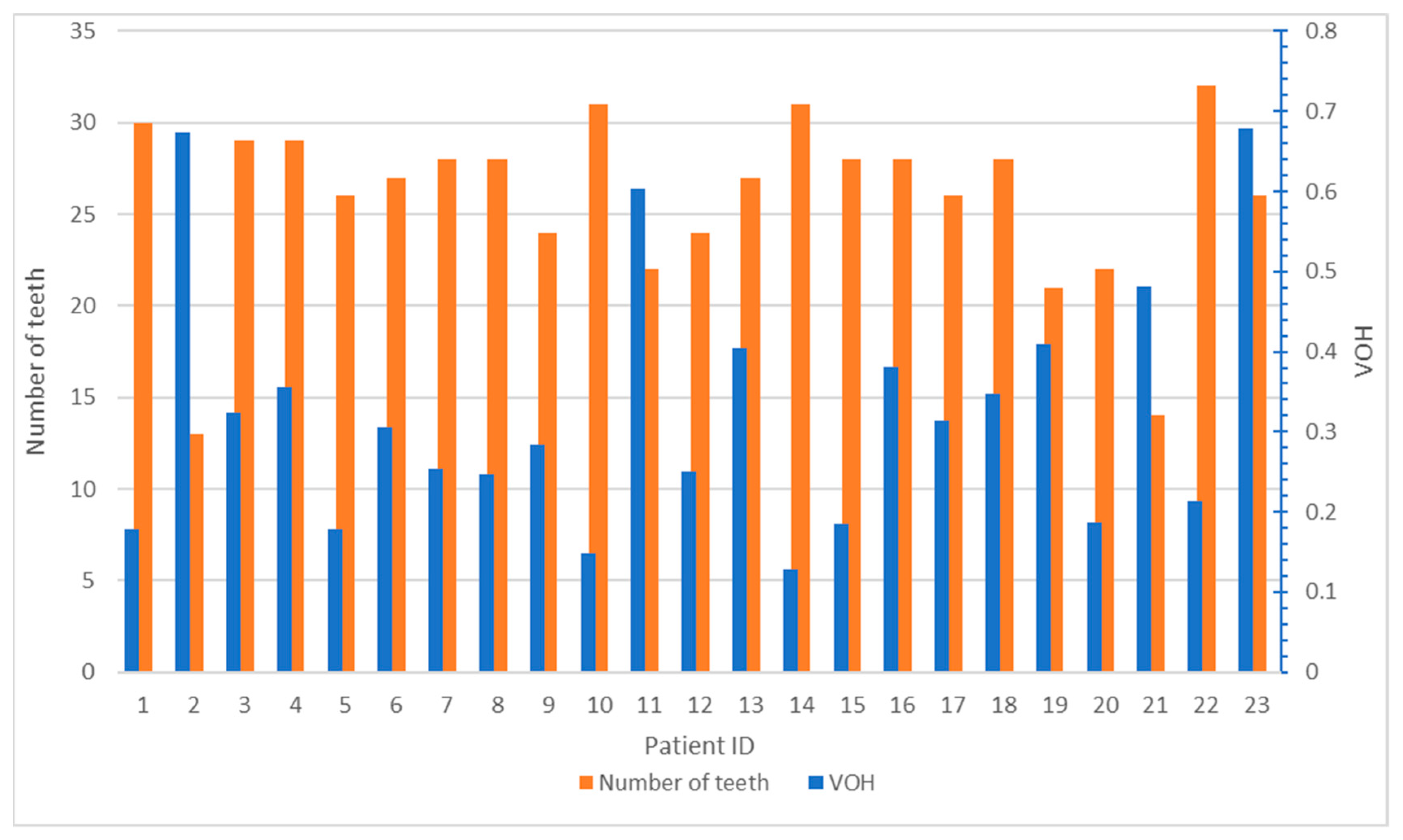
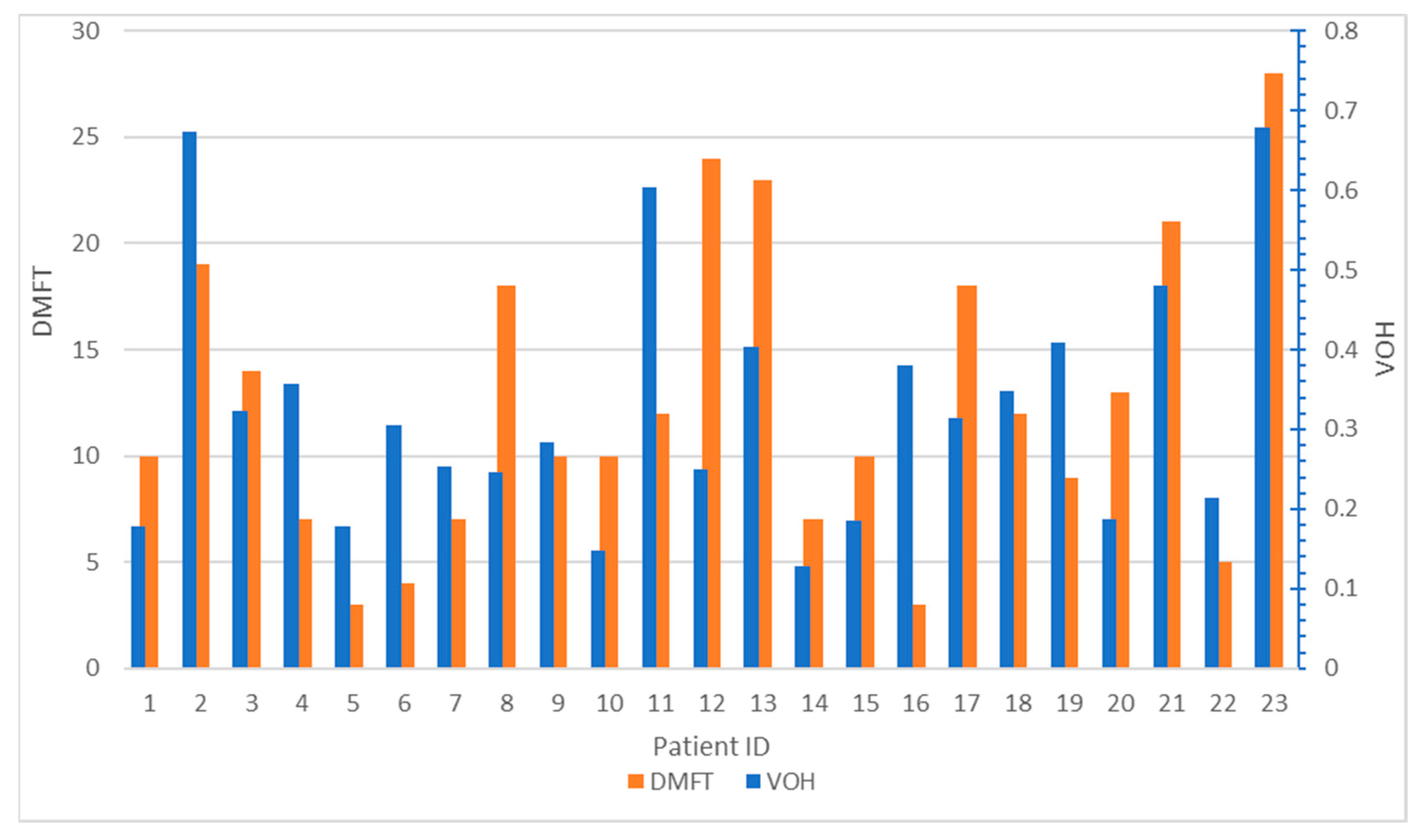
3.3. Intra-Oral Examination
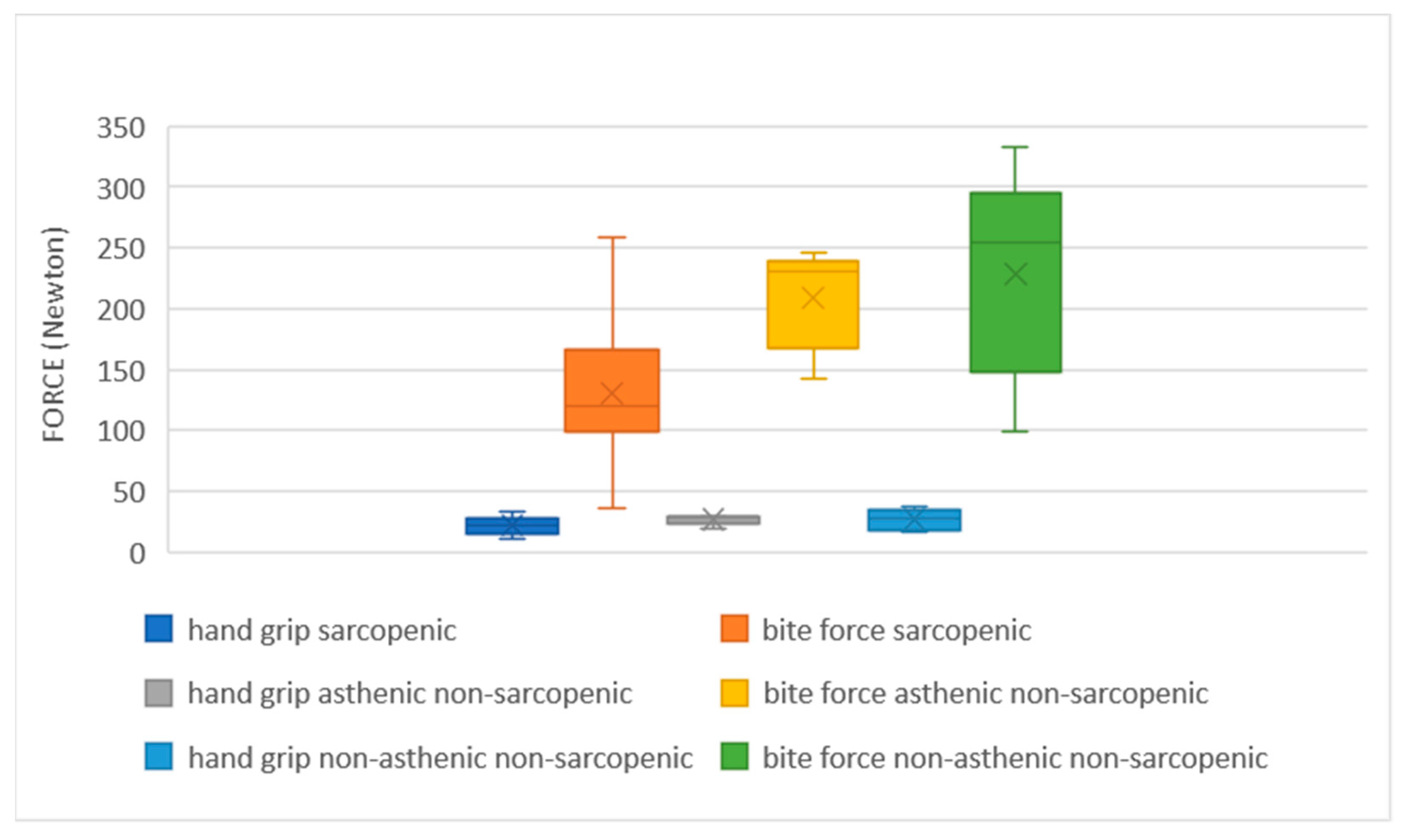
3.4. Bite Force Mesurament
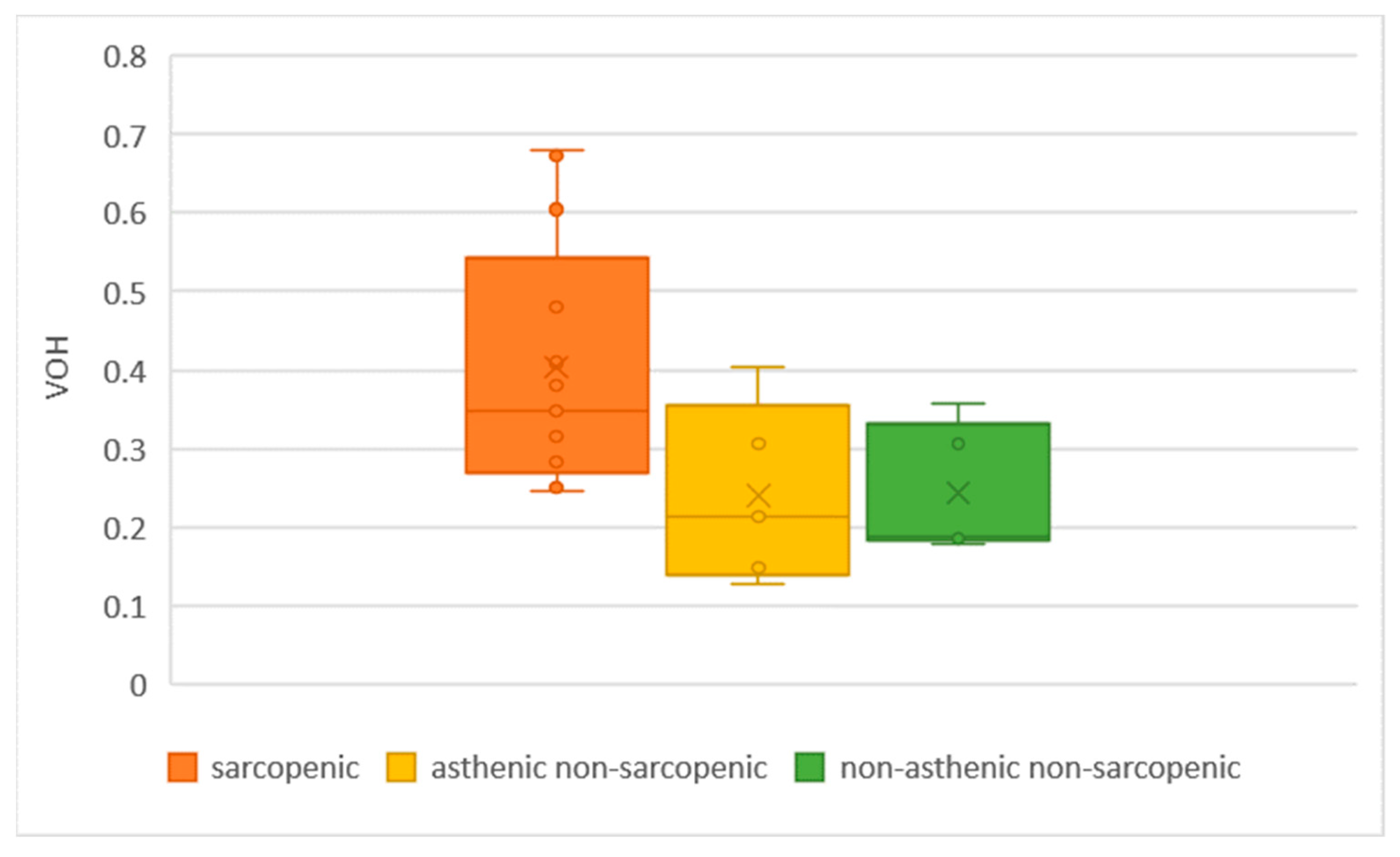
3.5. Chewing Gum Mixing Ability Test
4. Discussion
4.1. Short Medical History Interview
4.2. Anatomo-Functional Analysis
4.3. Intra-Oral Examination
4.4. Bite Force Measurement
4.5. Chewing Gum Mixing Ability Test
4.6. Limits of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Imai, K.; Tanaka, H. SARS-CoV-2 Infection and Significance of Oral Health Management in the Era of “the New Normal with COVID-19”. Int. J. Mol. Sci. 2021, 22, 6527. [Google Scholar] [CrossRef]
- Huang, N.; Pérez, P.; Kato, T.; Mikami, Y.; Okuda, K.; Gilmore, R.C.; Conde, C.D.; Gasmi, B.; Stein, S.; Beach, M.; et al. SARS-CoV-2 infection of the oral cavity and saliva. Nat. Med. 2021, 27, 892–903. [Google Scholar] [CrossRef] [PubMed]
- Mulchandani, R.; Lyngdoh, T.; Kakkar, A.K. Deciphering the COVID-19 cytokine storm: Systematic review and meta-analysis. Eur. J. Clin. Investig. 2021, 51, e13429. [Google Scholar] [CrossRef] [PubMed]
- Sakaguchi, W.; Kubota, N.; Shimizu, T.; Saruta, J.; Fuchida, S.; Kawata, A.; Yamamoto, Y.; Sugimoto, M.; Yakeishi, M.; Tsukinoki, K. Existence of SARS-CoV-2 Entry Molecules in the Oral Cavity. Int. J. Mol. Sci. 2020, 21, 6000. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Zhong, L.; Deng, J.; Peng, J.; Dan, H.; Zeng, X.; Li, T.; Chen, Q. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int. J. Oral Sci. 2020, 12, 8. [Google Scholar] [CrossRef] [PubMed]
- Mason, R.J. Pathogenesis of COVID-19 from a cell biology perspective. Eur. Respir. J. 2020, 55, 2000607. [Google Scholar] [CrossRef] [PubMed]
- Gu, S.X.; Tyagi, T.; Jain, K.; Gu, V.W.; Lee, S.H.; Hwa, J.M.; Kwan, J.M.; Krause, D.S.; Lee, A.I.; Halene, S.; et al. Thrombocytopathy and endotheliopathy: Crucial contributors to COVID-19 thromboinflammation. Nat. Rev. Cardiol. 2020, 18, 194–209. [Google Scholar] [CrossRef]
- Fabrizi, F.; Alfieri, C.M.; Cerutti, R.; Lunghi, G.; Messa, P. COVID-19 and Acute Kidney Injury: A Systematic Review and Meta-Analysis. Pathogens 2020, 9, 1052. [Google Scholar] [CrossRef]
- Sultan, S.; Altayar, O.; Siddique, S.M.; Davitkov, P.; Feuerstein, J.D.; Lim, J.K.; Falck-Ytter, Y.; El-Serag, H.B. AGA Institute Rapid Review of the Gastrointestinal and Liver Manifestations of COVID-19, Meta-Analysis of International Data, and Recommendations for the Consultative Management of Patients with COVID-19. Gastroenterology 2020, 159, 320–334.e27. [Google Scholar] [CrossRef]
- Herridge, M.S.; Tansey, C.; Matté, A.; Tomlinson, G.; Diaz-Granados, N.; Cooper, A.; Guest, C.; Mazer, D.; Mehta, S.; Stewart, T.; et al. Functional Disability 5 Years after Acute Respiratory Distress Syndrome. N. Engl. J. Med. 2011, 364, 1293–1304. [Google Scholar] [CrossRef]
- Fernández-De-Las-Peñas, C.; Palacios-Ceña, D.; Gómez-Mayordomo, V.; Cuadrado, M.L.; Florencio, L.L. Defining Post-COVID Symptoms (Post-Acute COVID, Long COVID, Persistent Post-COVID): An Integrative Classification. Int. J. Environ. Res. Public Health 2021, 18, 2621. [Google Scholar] [CrossRef]
- Taquet, M.; Dercon, Q.; Luciano, S.; Geddes, J.R.; Husain, M.; Harrison, P.J. Incidence, co-occurrence, and evolution of long-COVID features: A 6-month retrospective cohort study of 273,618 survivors of COVID-19. PLoS Med. 2021, 18, e1003773. [Google Scholar] [CrossRef] [PubMed]
- Cohen, A.A. Complex systems dynamics in aging: New evidence, continuing questions. Biogerontology 2016, 17, 205–220. [Google Scholar] [CrossRef] [PubMed]
- 2021 Alzheimer’s Disease Facts and Figures. Available online: https://alz-journals.onlinelibrary.wiley.com/doi/10.1002/alz.12328#:~:text=An%20estimated%206.2%20million%20Americans,prevent%2C%20slow%20or%20cure%20AD (accessed on 17 December 2022).
- COVID-19 Associated with Long-Term Cognitive Dysfunction, Acceleration of Alzheimer’s Symptoms. Available online: https://aaic.alz.org/releases_2021/covid-19-cognitive-impact.asp (accessed on 19 January 2023).
- Fulop, T.; Larbi, A.; Dupuis, G.; Le Page, A.; Frost, E.H.; Cohen, A.A.; Witkowski, J.M.; Franceschi, C. Immunosenescence and Inflamm-Aging as Two Sides of the Same Coin: Friends or Foes? Front. Immunol. 2018, 8, 1960. [Google Scholar] [CrossRef] [PubMed]
- Coppé, J.-P.; Patil, C.K.; Rodier, F.; Sun, Y.; Muñoz, D.P.; Goldstein, J.; Nelson, P.S.; Desprez, P.-Y.; Campisi, J. Senescence-Associated Secretory Phenotypes Reveal Cell-Nonautonomous Functions of Oncogenic RAS and the p53 Tumor Suppressor. PLoS Biol. 2008, 6, e301. [Google Scholar] [CrossRef]
- Salehi, S.; Reddy, S.; Gholamrezanezhad, A. Long-term Pulmonary Consequences of Coronavirus Disease 2019 (COVID-19): What we know and what to expect. J. Thorac. Imaging 2020, 35, W87–W89. [Google Scholar] [CrossRef]
- Puntmann, V.O.; Carerj, M.L.; Wieters, I.; Fahim, M.; Arendt, C.; Hoffmann, J.; Shchendrygina, A.; Escher, F.; Vasa-Nicotera, M.; Zeiher, A.M.; et al. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered from Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020, 5, 1265–1273. [Google Scholar] [CrossRef]
- Sathish, T.; Anton, M.C.; Sivakumar, T. New-onset diabetes in ‘long COVID’. J. Diabetes 2021, 13, 693–694. [Google Scholar] [CrossRef]
- Wang, F.; Kream, R.M.; Stefano, G.B. Long-term respiratory and neurological sequelae of COVID-19. Med. Sci. Monit. 2020, 26, e928996. [Google Scholar] [CrossRef]
- Phipps, M.M.; Barraza, L.H.; Lasota, E.D.; Sobieszczyk, M.E.; Pereira, M.R.; Zheng, E.X.; Fox, A.N.; Zucker, J.; Verna, E.C. Acute Liver Injury in COVID-19: Prevalence and Association with Clinical Outcomes in a Large U.S. Cohort. Hepatology 2020, 72, 807–817. [Google Scholar] [CrossRef]
- Troyer, E.A.; Kohn, J.N.; Hong, S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain. Behav. Immun. 2020, 87, 34–39. [Google Scholar] [CrossRef]
- Karaarslan, F.; Demircioğlu Güneri, F.; Kardeş, S. Postdischarge rheumatic and musculoskeletal symptoms following hospitalization for COVID-19: Prospective follow-up by phone interviews. Rheumatol. Int. 2021, 41, 1263–1271. [Google Scholar] [CrossRef]
- Bektas, A.; Schurman, S.H.; Franceschi, C.; Ferrucci, L. A public health perspective of aging: Do hyper-inflammatory syndromes such as COVID-19, SARS, ARDS, cytokine storm syndrome, and post-ICU syndrome accelerate short- and long-term inflammaging? Immun. Ageing 2020, 17, 23. [Google Scholar] [CrossRef]
- Delgado-Alonso, C.; Valles-Salgado, M.; Delgado-Álvarez, A.; Yus, M.; Gómez-Ruiz, N.; Jorquera, M.; Polidura, C.; Gil, M.J.; Marcos, A.; Matías-Guiu, J.; et al. Cognitive dysfunction associated with COVID-19: A comprehensive neuropsychological study. J. Psychiatr. Res. 2022, 150, 40–46. [Google Scholar] [CrossRef] [PubMed]
- van den Borst, B.; Peters, J.B.; Brink, M.; Schoon, Y.; Bleeker-Rovers, C.P.; Schers, H.; van Hees, H.W.H.; van Helvoort, H.; van den Boogaard, M.; van der Hoeven, H.; et al. Comprehensive Health Assessment 3 Months After Recovery from Acute Coronavirus Disease 2019 (COVID-19). Clin. Infect. Dis. 2021, 73, e1089. [Google Scholar] [CrossRef] [PubMed]
- Bloch, S.; Polkey, M.I.; Griffiths, M.; Kemp, P. Molecular mechanisms of intensive care unit-acquired weakness. Eur. Respir. J. 2012, 39, 1000–1011. [Google Scholar] [CrossRef]
- Wåhlin-Larsson, B.; Wilkinson, D.J.; Strandberg, E.; Hosford-Donovan, A.; Atherton, P.J.; Kadi, F. Mechanistic Links Underlying the Impact of C-Reactive Protein on Muscle Mass in Elderly. Cell. Physiol. Biochem. 2017, 44, 267–278. [Google Scholar] [CrossRef] [PubMed]
- Aschman, T.; Schneider, J.; Greuel, S.; Meinhardt, J.; Streit, S.; Goebel, H.-H.; Büttnerova, I.; Elezkurtaj, S.; Scheibe, F.; Radke, J.; et al. Association Between SARS-CoV-2 Infection and Immune-Mediated Myopathy in Patients Who Have Died. JAMA Neurol. 2021, 78, 948–960. [Google Scholar] [CrossRef]
- de Andrade-Junior, M.C.; de Salles, I.C.D.; de Brito, C.M.M.; Pastore-Junior, L.; Righetti, R.F.; Yamaguti, W.P. Skeletal Muscle Wasting and Function Impairment in Intensive Care Patients with Severe COVID-19. Front. Physiol. 2021, 12, 640973. [Google Scholar] [CrossRef]
- McKenna, H.T.; Murray, A.J.; Martin, D.S. Human adaptation to hypoxia in critical illness. J. Appl. Physiol. 2020, 129, 656–663. [Google Scholar] [CrossRef]
- Wierdsma, N.J.; Kruizenga, H.M.; Konings, L.A.; Krebbers, D.; Jorissen, J.R.; Joosten, M.-H.I.; van Aken, L.H.; Tan, F.M.; van Bodegraven, A.A.; Soeters, M.R.; et al. Poor nutritional status, risk of sarcopenia and nutrition related complaints are prevalent in COVID-19 patients during and after hospital admission. Clin. Nutr. Espen. 2021, 43, 369. [Google Scholar] [CrossRef] [PubMed]
- Soares, M.N.; Eggelbusch, M.; Naddaf, E.; Gerrits, K.H.L.; van der Schaaf, M.; van den Borst, B.; Wiersinga, W.J.; van Vugt, M.; Weijs, P.J.M.; Murray, A.J.; et al. Skeletal muscle alterations in patients with acute COVID-19 and post-acute sequelae of COVID-19. J. Cachexia Sarcopenia Muscle 2022, 13, 11–22. [Google Scholar] [CrossRef] [PubMed]
- Shepherd, S.; Batra, A.; Lerner, D.P. Review of Critical Illness Myopathy and Neuropathy. Neurohospitalist 2017, 7, 41–48. [Google Scholar] [CrossRef]
- Yoshida, M.; Hiraoka, A.; Takeda, C.; Mori, T.; Maruyama, M.; Yoshikawa, M.; Tsuga, K. Oral hypofunction and its relation to frailty and sarcopenia in community-dwelling older people. Gerodontology 2022, 39, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Kugimiya, Y.; Iwasaki, M.; Ohara, Y.; Motokawa, K.; Edahiro, A.; Shirobe, M.; Watanabe, Y.; Obuchi, S.; Kawai, H.; Fujiwara, Y.; et al. Relationship between Oral Hypofunction and Sarcopenia in Community-Dwelling Older Adults: The Otassha Study. Int. J. Environ. Res. Public Health 2021, 18, 6666. [Google Scholar] [CrossRef]
- Višnjić, A.; Veličković, V.; Sokolović, D.; Stanković, M.; Mijatović, K.; Milošević, Z.; Radulović, O. Relationship between the manner of mobile phone use and depression, anxiety, and stress in university students. Int. J. Environ. Res. Public Health 2018, 15, 697. [Google Scholar] [CrossRef]
- Calcolo Indice Massa Corporea—IMC (BMI—Body Mass Index). Available online: https://www.salute.gov.it/portale/nutrizione/dettaglioIMCNutrizione.jsp?lingua=italiano&id=5479&area=nutrizione&menu=vuoto (accessed on 17 December 2022).
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in Older AdultsEvidence for a Phenotype. J. Gerontol. Ser. A 2001, 56, M146–M157. [Google Scholar] [CrossRef]
- Giornale di Cardiologia. Available online: https://www.giornaledicardiologia.it/archivio/1261/articoli/13935/#:~:text=Inparticolare%2Cunavelocità%3E1.0,instabilieridottaautonomia24 (accessed on 17 December 2022).
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Aihie Sayer, A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef]
- Sondaggio Parodontale. Available online: https://www.gengive.org/glossario/sondaggio-parodontale/ (accessed on 17 December 2022).
- Testa, M.; Di Marco, A.; Pertusio, R.; Van Roy, P.; Cattrysse, E.; Roatta, S. A validation study of a new instrument for low cost bite force measurement. J. Electromyogr. Kinesiol. 2016, 30, 243–248. [Google Scholar] [CrossRef]
- FlexiForce User Manual | Tekscan. Available online: https://www.tekscan.com/support/faqs/flexiforce-user-manual (accessed on 16 May 2022).
- Manns, A.; Miralles, R.; Palazzi, C. EMG, bite force, and elongation of the masseter muscle under isometric voluntary contractions and variations of vertical dimension. J. Prosthet. Dent. 1979, 42, 674–682. [Google Scholar] [CrossRef]
- Âudio, C.; Fernandes, P.; Glantz, J.; Svensson, S.A.; Bergmark, A. A Novel Sensor for Bite Force Determinations. Available online: http://www.elsevier.com/locate/dental (accessed on 17 December 2022).
- Anastassiadou, V.; Heath, M.R.; Bartholomew, S. The development of a simple objective test of mastication suitable for older people, using chewing gums. Gerodontology 2001, 18, 79–86. [Google Scholar] [CrossRef]
- Prinz, J.F. Quantitative evaluation of the effect of bolus size and number of chewing strokes on the intra-oral mixing of a two-colour chewing gum. J. Oral Rehabil. 1999, 26, 243–247. [Google Scholar] [CrossRef] [PubMed]
- Schimmel, M.; Leemann, B.; Herrmann, F.R.; Kiliaridis, S.; Schnider, A.; Müller, F. Masticatory function and bite force in stroke patients. J. Dent. Res. 2011, 90, 230–234. [Google Scholar] [CrossRef]
- Buser, R.; Ziltener, V.; Samietz, S.; Fontolliet, M.; Nef, T.; Schimmel, M. Validation of a purpose-built chewing gum and smartphone application to evaluate chewing efficiency. J. Oral Rehabil. 2018, 45, 845–853. [Google Scholar] [CrossRef] [PubMed]
- Fankhauser, N.; Kalberer, N.; Müller, F.; Leles, C.R.; Schimmel, M.; Srinivasan, M. Comparison of smartphone-camera and conventional flatbed scanner images for analytical evaluation of chewing function. J. Oral Rehabil. 2020, 47, 1496–1502. [Google Scholar] [CrossRef]
- ViewGum. Available online: http://www.dhal.com/viewgum.html (accessed on 17 December 2022).
- Chippa, V.; Aleem, A.; Anjum, F. Post Acute Coronavirus (COVID-19) Syndrome. StatPearls. 2022. Available online: https://www.ncbi.nlm.nih.gov/books/NBK570608/ (accessed on 17 December 2022).
- PICS. Available online: https://postintensiva.it/la-pics-post-intensive-care-syndrome/ (accessed on 17 December 2022).
- Kuhn, M.; Türp, J.C.; Türp, J.C.; Myoarthropathien, M.A.A. Risk factors for bruxism. SWISS Dent. J. SSO 2018, 128, 118–124. [Google Scholar]
- Ohrbach, R.; Michelotti, A. The Role of Stress in the Etiology of Oral Parafunction and Myofascial Pain. Oral Maxillofac. Surg. Clin. N. Am. 2018, 30, 369–379. [Google Scholar] [CrossRef]
- Kit, A.; Tamrakar, M.; Jiang, C.M.; Man Lo, E.C.; Man Leung, K.C.; Chu, C.H. A Systematic Review on Caries Status of Older Adults. Int. J. Environ. Res. Public Health 2021, 18, 10662. [Google Scholar] [CrossRef]
- Mańka-Malara, K.; Gawlak, D.; Hovhannisyan, A.; Klikowska, M.; Kostrzewa-Janicka, J. Dental trauma prevention during endotracheal intubation—Review of literature. Anaesthesiol. Intensive Ther. 2015, 47, 425–429. [Google Scholar] [CrossRef]
- Teixeira, D.N.R.; Thomas, R.Z.; Soares, P.V.; Cune, M.S.; Gresnigt, M.M.M.; Slot, D.E. Prevalence of noncarious cervical lesions among adults: A systematic review. J. Dent. 2020, 95, 103285. [Google Scholar] [CrossRef]
- Nascimento, M.M.; Dilbone, D.A.; Pereira, P.N.; Duarte, R.; Geraldeli, S.; Delgado, A.J. Clinical, Cosmetic and Investigational Dentistry Abfraction lesions: Etiology, diagnosis, and treatment options. Clin. Cosmet. Investig. Dent. 2016, 8, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Testa, M.; Rolando, M. Control of jaw-clenching forces in dentate subjects. J. Orofac. Pain 2011, 25, 250–260. [Google Scholar] [PubMed]
- Testa, M.; Geri, T.; Signori, A.; Roatta, S. Visual Feedback of Bilateral Bite Force to Assess Motor Control of the Mandible in Isometric Condition. Mot. Control. 2015, 19, 312–324. [Google Scholar] [CrossRef]
- Ikebe, K.; Matsuda, K.-I.; Kagawa, R.; Enoki, K.; Yoshida, M.; Maeda, Y.; Nokubi, T. Association of masticatory performance with age, gender, number of teeth, occlusal force and salivary flow in Japanese older adults: Is ageing a risk factor for masticatory dysfunction? Arch. Oral Biol. 2011, 56, 991–996. [Google Scholar] [CrossRef]
- Yamada, A.; Kanazawa, M.; Komagamine, Y.; Minakuchi, S. Association between tongue and lip functions and masticatory performance in young dentate adults. J. Oral Rehabil. 2015, 42, 833–839. [Google Scholar] [CrossRef] [PubMed]
- Schimmel, M.; Christou, P.; Miyazaki, H.; Halazonetis, D.; Herrmann, F.R.; Müller, F. A novel colourimetric technique to assess chewing function using two-coloured specimens: Validation and application. J. Dent. 2015, 43, 955–964. [Google Scholar] [CrossRef] [PubMed]
- Silva, L.C.; Nogueira, T.E.; Rios, L.F.; Schimmel, M.; Leles, C.R. Reliability of a two-colour chewing gum test to assess masticatory performance in complete denture wearers. J. Oral Rehabil. 2018, 45, 301–307. [Google Scholar] [CrossRef]


| Total (n = 23) | Sarcopenic (n = 13, 56.5) | Asthenic Non-Sarcopenic (n = 5, 21.7) | Non Asthenic Non-Sarcopenic (n = 5, 21.7) | p-Value | |
|---|---|---|---|---|---|
| Missing teeth | 5.5 ± 6.8 (0–28) | 8.1 ± 7.9 (1–28) | 2.0 ± 2.9 (0–7) | 2.4 ± 2.7 (0–7) | 0.118 |
| Crown | 4.3 ± 6.7 (0–28) | 4.7 ± 8.1 (0–28) | 4.0 ± 6.3 (0–15) | 3.6 ± 3.5 (0–9) | 0.944 |
| Pontic elements or part of RPP | 2.0 ± 4.5 (0–18) | 3.0 ± 5.7 (0–18) | 1.2 ± 1.7 (0–4) | 0.4 ± 0.5 (0–1) | 0.507 |
| Teeth present (natural or prosthetic) | 25.8 ± 4.8 (13–32) | 23.9 ± 5.2 (13–29) | 29.6 ± 2.4 (27–32) | 27.0 ± 3.1 (22–30) | 0.063 |
| Decayed teeth | 1.4 ± 1.8 (0–8) | 2.0 ± 2.1 (0–8) | 0.8 ± 0.8 (0–2) | 0.6 ± 0.5 (0–1) | 0.235 |
| Filled teeth | 2.3 ± 2.6 (0–7) | 2.3 ± 2.9 (0–7) | 3.0 ± 1.6 (1–5) | 2.0 ± 2.8 (0–6) | 0.834 |
| Teeth with NCCL | 2.9 ± 4.1 (0–14) | 1.6 ± 3.8 (0–14) | 3.4 ± 3.4 (0–8) | 5.8 ± 4.6 (0–11) | 0.145 |
| DMFT | 12.5 ± 7.1 (3–28) | 15.0 ± 7.1 (3–28) | 9.8 ± 7.7 (4–23) | 8.6 ± 3.7 (3–13) | 0.143 |
| DASS-A | 4.6 ± 4.4 (0–14) | 5.3 ± 5.0 (0–14) | 6.0 ± 2.7 (4–9) | 1.5 ± 2.3 (0–5) | 0.293 |
| DASS-D | 4.9 ± 5.1 (0–18) | 5.6 ± 5.5 (0–18) | 6.3 ± 5.1 (2–12) | 2.0 ± 4.0 (0–8) | 0.441 |
| DASS-S | 6.6 ± 4.7 (0–17) | 8.0 ± 4.7 (3–17) | 7.7 ± 2.5 (5–10) | 2.0 ± 3.4 (0–7) | 0.078 |
| Total (n = 23) | Sarcopenic (n = 13, 56.5) | Asthenic Non-Sarcopenic (n = 5, 21.7) | Non-Asthenic Non-Sarcopenic (n = 5, 21.7) | p-Value | |
|---|---|---|---|---|---|
| DMFT | 12.5 ± 7.1 (3–28) | 15.0 ± 7.1 (3–28) | 9.8 ± 7.7 (4–23) | 8.6 ± 3.7 (3–13) | 0.143 |
| VOH | 0.33 ± 0.16 (0.13–0.68) | 0.40 ± 0.14 (0.25–0.68) | 0.24 ± 0.11 (0.12–0.4) | 0.22 ± 0.07 (0.18–0.35) | 0.02 |
| Hand grip test | 24.2 ± 7.0 (9.2–35.1) | 23.4 ± 6.5 (10.1–34.4) | 27.6 ± 4.9 (19.2–31.9) | 23.1 ± 10.1 (9.2–35.1) | 0.501 |
| Gait speed test * | 3.6 ± 0.7 (2.6–5.2) | 4.1 ± 0.7 (2.9–5.2) | 3.2 ± 0.2 (3.0–3.6) | 2.8 ± 0.2 (8.5–14.3) | 0.001 |
| Chair stand test | 12.7 ± 2.7 (8.5–18.7) | 13.2 ± 2.9 (9.5–18.7) | 13.5 ± 2.2 (10.4–16.3) | 10.7 ± 2.3 (8.5–14.3) | 0.189 |
| Bite force * | 168.5 ± 69.9 (35.5–332.8) | 122.4 ± 41.9 (35.5–173.5) | 208.5 ± 41.8 (142.3–246.1) | 248.2 ± 55.2 (197.5–332.8) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pugliese, B.D.; Garuti, G.; Bergamini, L.; Khamaisi, R.K.; Guaraldi, G.; Consolo, U.; Bellini, P. Masticatory Functionality in Post-Acute-COVID-Syndrome (PACS) Patients with and without Sarcopenia. Oral 2023, 3, 77-91. https://doi.org/10.3390/oral3010008
Pugliese BD, Garuti G, Bergamini L, Khamaisi RK, Guaraldi G, Consolo U, Bellini P. Masticatory Functionality in Post-Acute-COVID-Syndrome (PACS) Patients with and without Sarcopenia. Oral. 2023; 3(1):77-91. https://doi.org/10.3390/oral3010008
Chicago/Turabian StylePugliese, Bruno Davide, Giovanna Garuti, Lucia Bergamini, Riccardo Karim Khamaisi, Giovanni Guaraldi, Ugo Consolo, and Pierantonio Bellini. 2023. "Masticatory Functionality in Post-Acute-COVID-Syndrome (PACS) Patients with and without Sarcopenia" Oral 3, no. 1: 77-91. https://doi.org/10.3390/oral3010008
APA StylePugliese, B. D., Garuti, G., Bergamini, L., Khamaisi, R. K., Guaraldi, G., Consolo, U., & Bellini, P. (2023). Masticatory Functionality in Post-Acute-COVID-Syndrome (PACS) Patients with and without Sarcopenia. Oral, 3(1), 77-91. https://doi.org/10.3390/oral3010008









