Factors Determining the Willingness of Nigerian Clinicians to Recommend Protected Oral Sex: An Online Exploratory Study
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Participants
2.3. Study Instrument
2.4. Measures
2.5. Sample Size
2.6. Data Collection
2.7. Data Analysis
2.8. Ethical Considerations
3. Results
3.1. Total Number of Participants
3.2. Respondents’ Background Characteristics
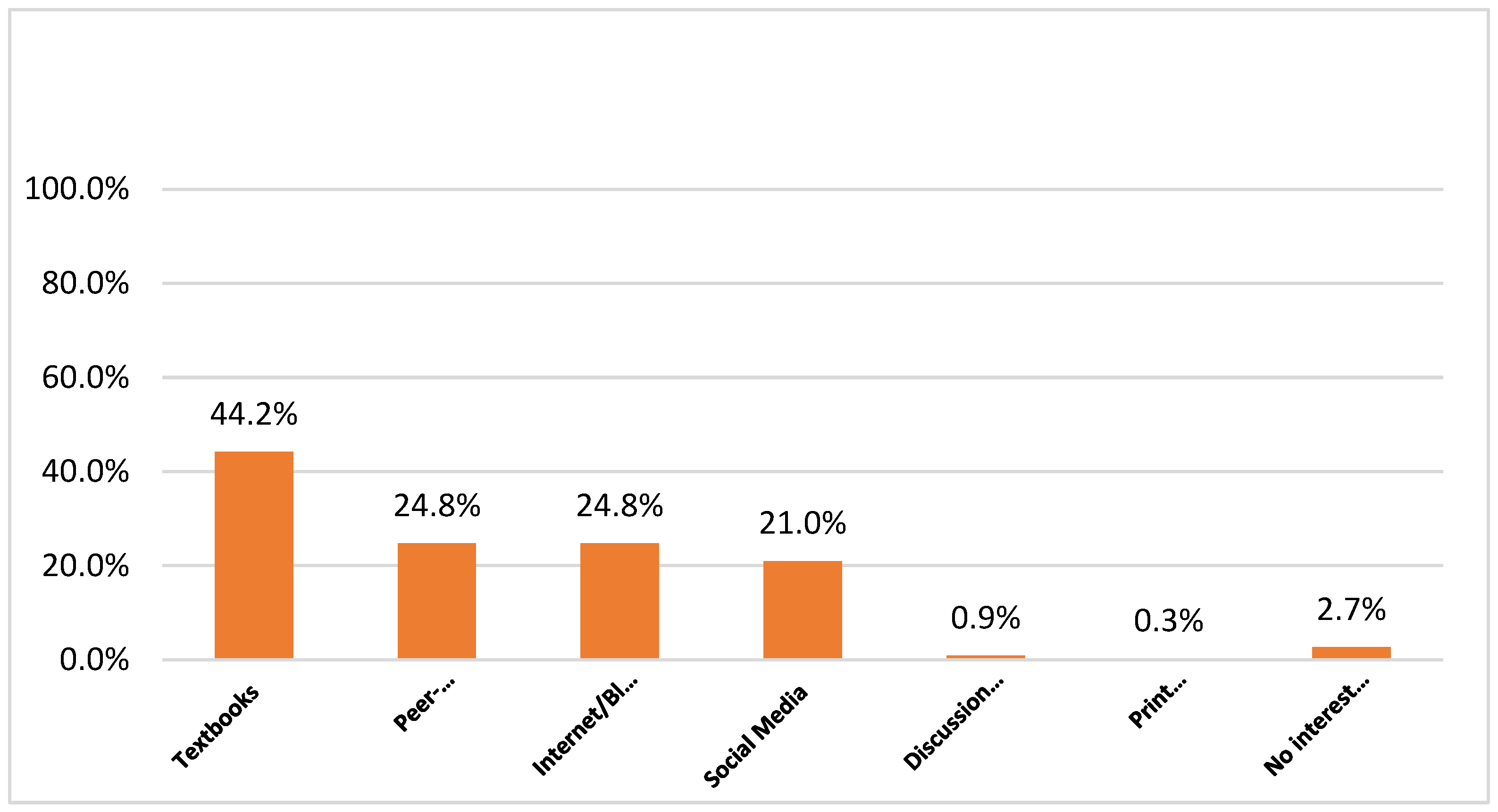
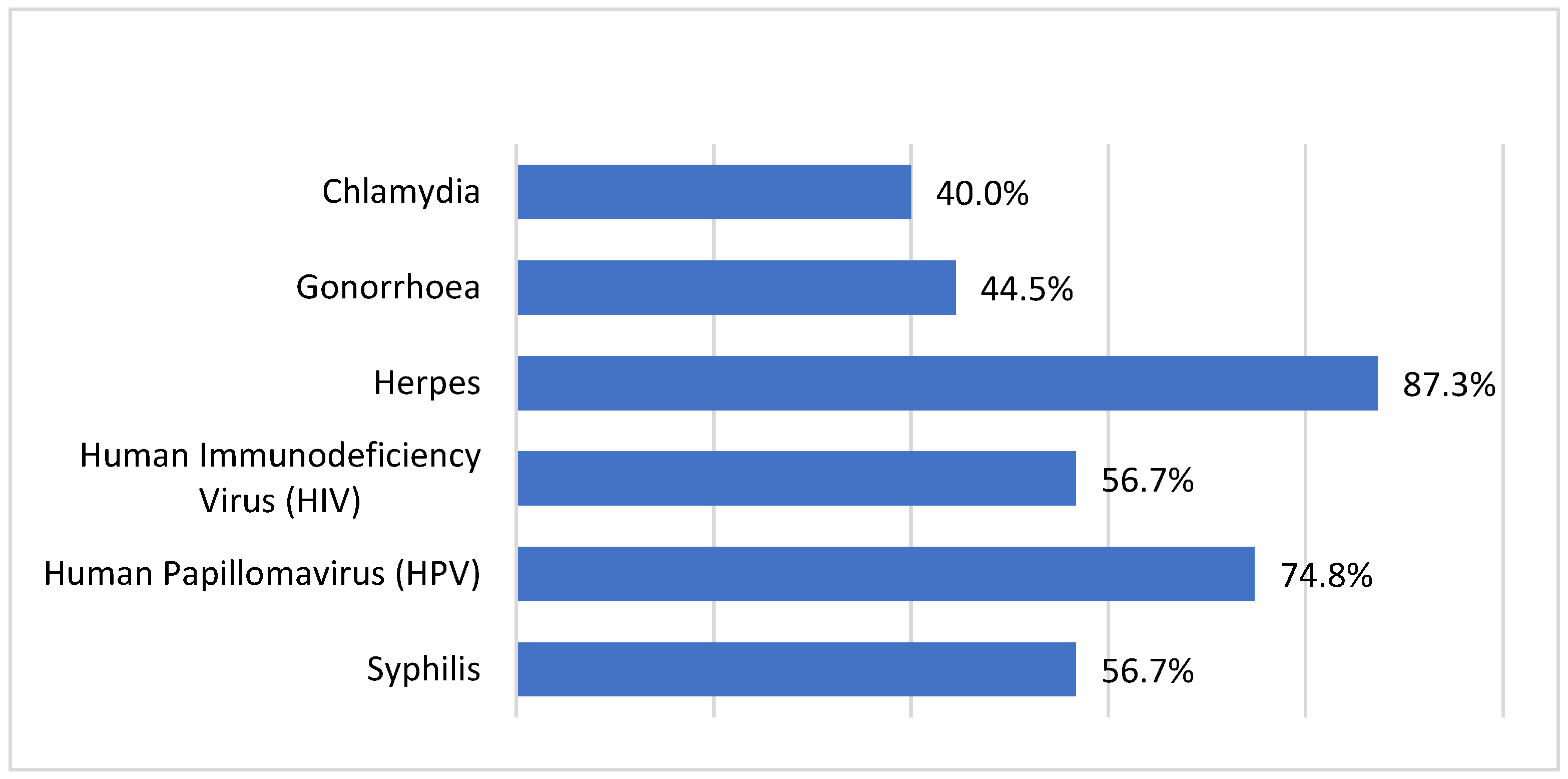
3.3. Respondents’ Knowledge on Oral Sex
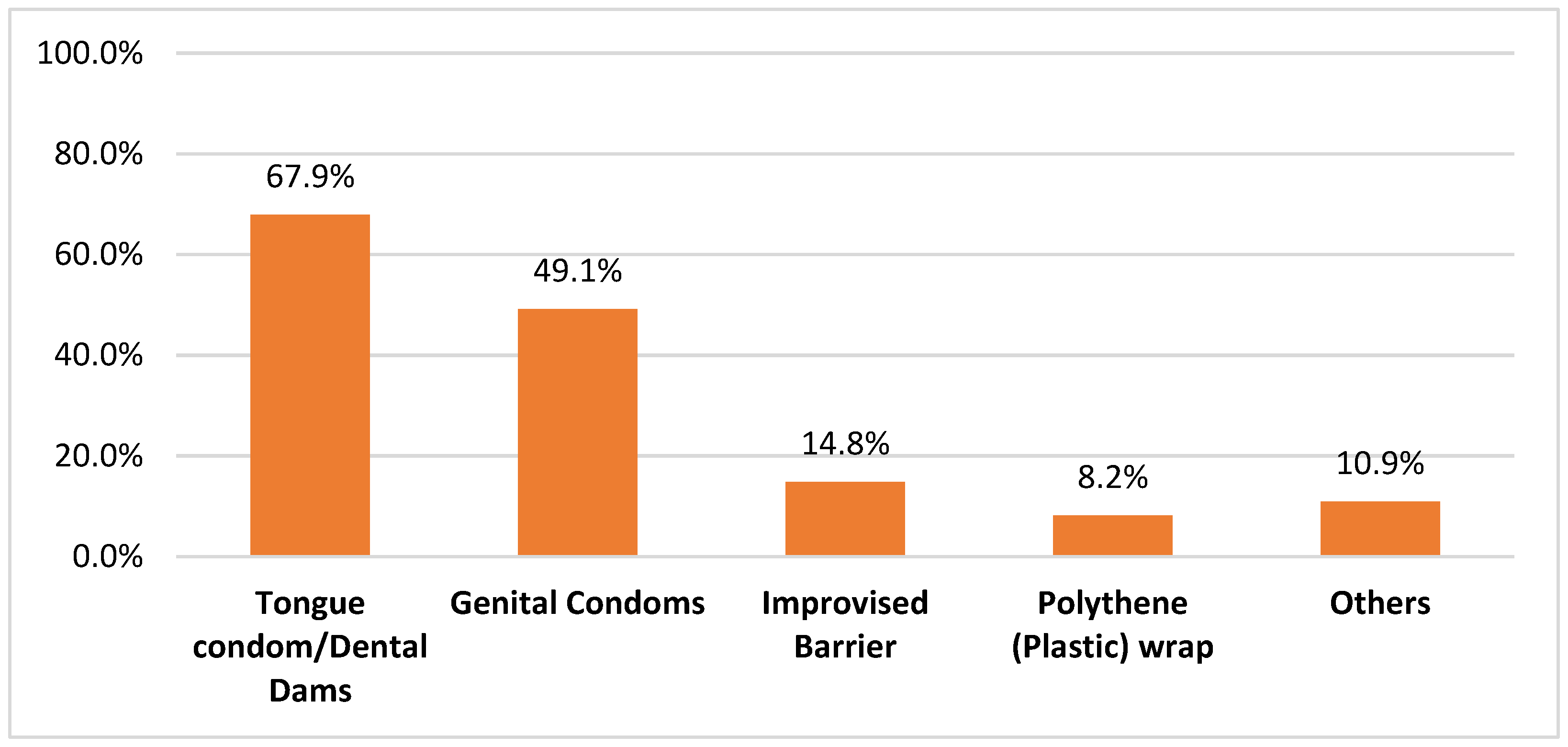
3.4. Respondents’ Experience and Attitudes concerning Safer Oral Sex
3.5. Respondents’ Experiences and Attitudes concerning Professional Discussions on Oral Sex
- (A)
- With Patients
- (B)
- With Clinicians/Academics/Others
3.6. Factors Determining the Respondents’ Willingness to Recommend Oral Sex Protective Measures to Patients
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Liu, H.; Shen, S.; Hsieh, N. A National Dyadic Study of Oral Sex, Relationship Quality, and Well-Being among Older Couples. J. Gerontol. Ser. B 2019, 74, 298–308. [Google Scholar] [CrossRef]
- Fritz, N.; Bowling, J. Sexual Behaviors and Aggression in Gay Pornography. J. Homosex 2022, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Pakpahan, C.; Darmadi, D.; Agustinus, A.; Rezano, A. Framing and understanding the whole aspect of oral sex from social and health perspective: A narrative review. F1000Research 2022, 11, 177. [Google Scholar] [CrossRef] [PubMed]
- Wylie, K. A Global Survey of Sexual Behaviours. J. Fam. Reproduc. Health 2009, 3, 39–49. [Google Scholar]
- Morhason-Bello, I.O.; Kabakama, S.; Baisley, K.; Francis, S.C.; Watson-Jones, D. Reported oral and anal sex among adolescents and adults reporting heterosexual sex in sub-Saharan Africa: A systematic review. Reprod. Health 2019, 16, 48. [Google Scholar] [CrossRef] [PubMed]
- Lewis, R.; Tanton, C.; Mercer, C.H.; Mitchell, K.R.; Palmer, M.; Macdowall, W.; Wellings, K. Heterosexual Practices Among Young People in Britain: Evidence from Three National Surveys of Sexual Attitudes and Lifestyles. J. Adolesc. Health 2017, 61, 694–702. [Google Scholar] [CrossRef] [PubMed]
- Lefkowitz, E.S.; Vasilenko, S.A.; Leavitt, C.E. Oral vs. Vaginal Sex Experiences and Consequences Among First-Year College Students. Arch. Sex Behav. 2016, 45, 329–337. [Google Scholar] [CrossRef]
- Saini, R.; Saini, S.; Sharma, S. Oral sex, oral health and orogenital infections. J. Glob. Infect. Dis 2010, 2, 57–62. [Google Scholar] [CrossRef]
- Koelman, C.A.; Coumans, A.B.; Nijman, H.W.; Doxiadis, I.I.; Dekker, G.A.; Claas, F.H. Correlation between oral sex and a low incidence of preeclampsia: A role for soluble HLA in seminal fluid? J. Reprod. Immunol. 2000, 46, 155–166. [Google Scholar] [CrossRef]
- Meuleman, T.; Baden, N.; Haasnoot, G.W.; Wagner, M.M.; Dekkers, O.M.; le Cessie, S.; Picavet, C.; van Lith, J.M.M.; Claas, F.H.J.; Bloemenkamp, K.W.M. Oral sex is associated with reduced incidence of recurrent miscarriage. J. Reprod. Immunol. 2019, 133, 1–6. [Google Scholar] [CrossRef]
- Pittrof, R.; Sully, E.; Bass, D.C.; Kelsey, S.F.; Ness, R.B.; Haggerty, C.L. Stimulating an immune response? Oral sex is associated with less endometritis. Int. J. STD AIDS 2012, 23, 775–780. [Google Scholar] [CrossRef] [PubMed]
- Kumar, T.; Puri, G.; Aravinda, K.; Arora, N.; Patil, D.; Gupta, R. Oral sex and oral health: An enigma in itself. Indian J. Sex Transm. Dis AIDS 2015, 36, 129–132. [Google Scholar] [CrossRef] [PubMed]
- Queirós, C.; Costa, J.B.D. Oral Transmission of Sexually Transmissable Infections: A Narrative Review. Acta Med. Port. 2019, 32, 776–781. [Google Scholar] [CrossRef] [PubMed]
- Kanmodi, K.K.; Nwafor, J.N.; Amoo, B.A.; Nnyanzi, L.A.; Ogbeide, M.E.; Hundeji, A.A. Knowledge of the health implications of oral sex among registered nurses in Nigeria: An online pilot study. J. Health Allied Sci. 2022. [Google Scholar] [CrossRef]
- Deutsche Well. Nigerian ‘Aphrodisiac’ Potions for a Happy Marriage. Available online: https://www.dw.com/en/nigerian-aphrodisiac-potions-for-a-happy-marriage/a-49280968 (accessed on 16 August 2022).
- Gerbase, A.C.; Mertens, T.E. Sexually transmitted diseases in Africa: Time for action. Afr. Health 1998, 20, 10–12. [Google Scholar] [PubMed]
- Stewart, J.; Bukusi, E.; Celum, C.; Delany-Moretlwe, S.; Baeten, J.M. Sexually transmitted infections among African women: An opportunity for combination sexually transmitted infection/HIV prevention. AIDS 2020, 34, 651–658. [Google Scholar] [CrossRef] [PubMed]
- Badawi, M.M.; SalahEldin, M.A.; Idris, A.B.; Hasabo, E.A.; Osman, Z.H.; Osman, W.M. Knowledge gaps of STIs in Africa; Systematic review. PLoS ONE 2019, 14, e0213224. [Google Scholar] [CrossRef]
- UNAIDS; NACA; FMOH (Nigeria). New Survey Results Indicate That Nigeria Has a HIV Prevalence of 1.4%. Available online: https://www.unaids.org/sites/default/files/20190314_PR_Nigeria_en.pdf (accessed on 16 August 2022).
- Bruni, L.; Albero, G.; Serrano, B.; Mena, M.; Collado, J.J.; Gómez, D.; Muñoz, J.; Bosch, F.X.; de Sanjosé, S.; ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre). Human Papillomavirus and Related Diseases in Nigeria. Available online: https://hpvcentre.net/statistics/reports/NPL.pdf (accessed on 22 October 2021).
- Morhason-Bello, I.O.; Baisley, K.; Pavon, M.A.; Adewole, I.F.; Bakare, R.A.; de Sanjosé, S.; Francis, S.C.; Watson-Jones, D. Oral, genital and anal human papillomavirus infections among female sex workers in Ibadan, Nigeria. PLoS ONE 2022, 17, e0265269. [Google Scholar] [CrossRef]
- Esere, M.O. Effect of Sex Education Programme on at-risk sexual behaviour of school-going adolescents in Ilorin, Nigeria. Afr. Health Sci. 2008, 8, 120–125. [Google Scholar] [CrossRef]
- Ogunfowokan, A.A.; Fajemilehin, R.B. Impact of a school-based sexual abuse prevention education program on the knowledge and attitude of high school girls. J. Sch. Nurs. 2012, 28, 459–468. [Google Scholar] [CrossRef] [PubMed]
- Osadolor, U.E.; Amoo, E.O.; Azuh, D.E.; Mfonido-Abasi, I.; Washington, C.P.; Ugbenu, O. Exposure to Sex Education and Its Effects on Adolescent Sexual Behavior in Nigeria. J. Environ. Public Health 2022, 2022, 3962011. [Google Scholar] [CrossRef] [PubMed]
- Amu, E.O.; Adegun, P.T. Awareness and Knowledge of Sexually Transmitted Infections among Secondary School Adolescents in Ado Ekiti, South Western Nigeria. J. Sex. Transm. Dis. 2015, 2015, 260126. [Google Scholar] [CrossRef]
- Morhason-Bello, I.O.; Fagbamigbe, A.F. Association between Knowledge of Sexually Transmitted Infections and Sources of the Previous Point of Care among Nigerians: Findings from Three National HIV and AIDS Reproductive Health Surveys. Int. J. Reprod. Med. 2020, 2020, 6481479. [Google Scholar] [CrossRef] [PubMed]
- Akokuwebe, M.E.; Daini, B.; Falayi, E.O.; Oyebade, O. Knowledge and attitude of sexually transmitted diseases among adolescents in Ikeji-Arakeji, Osun State, in South-Western Nigeria. Afr. J. Med. Med. Sci. 2016, 45, 281–289. [Google Scholar] [PubMed]
- Orji, E.O.; Esimai, O.A. Introduction of sex education into Nigerian schools: The parents’, teachers’ and students’ perspectives. J. Obstet. Gynaecol. 2003, 23, 185–188. [Google Scholar] [CrossRef]
- Odeyemi, K.A.; Onajole, A.T.; Ogunowo, B.E.; Olufunlayo, T.; Segun, B. The effect of a sexuality education programme among out- of- school adolescents in Lagos, Nigeria. Niger. Postgrad. Med. J. 2014, 21, 122–127. [Google Scholar]
- Ahanonu, E.L. Attitudes of Healthcare Providers towards Providing Contraceptives for Unmarried Adolescents in Ibadan, Nigeria. J. Fam. Reprod. Health 2014, 8, 33–40. [Google Scholar]
- Nnyanzi, L.; Kanmodi, K.; Nwafor, J.; Salami, A.; Obute, P.; Eze, U.; Almu, B.; Amoo, B.; Adebayo, O.; Obute, G.; et al. Establishing the “International Head and Neck Cancer Working Group”. South Asian J. Cancer, 2022; accepted. [Google Scholar]
- Kapoor, D.A.; Latino, K.; Hodes, G.; Anderson, A.E.; Anderson, J.; Cognetti, M.; Patel, C. The Impact of Systematic Safety Precautions on COVID-19 Risk Exposure and Transmission Rates in Outpatient Healthcare Workers. Rev. Urol. 2020, 22, 93–101. [Google Scholar]
- Greene, R.E. The Complex Road Ahead for Preexposure Prophylaxis: A Primary Care Physician Perspective. Am. J. Public Health 2017, 107, 1580–1581. [Google Scholar] [CrossRef]
- Leslie, K. Survey Sampling; John Wiley and Sons: New York, NY, USA, 1965. [Google Scholar]
- Habel, M.A.; Leichliter, J.S.; Dittus, P.J.; Spicknall, I.H.; Aral, S.O. Heterosexual Anal and Oral Sex in Adolescents and Adults in the United States, 2011-2015. Sex Transm. Dis. 2018, 45, 775–782. [Google Scholar] [CrossRef] [PubMed]
- Onuwabuchi, E.; Omololu, A.; Grillo, E.; Ekundayo, O.; Adeniyi, M.A.; Ogunsuji, O.O.; Kpuduwei, S.P.K.; Egbuchulem, I.K.; Oduyemi, I.; Soneye, O.; et al. Letter to the editor: The demographic profile of the Nigeria early career doctors. Yen Med. J. 2020, 2, 1–4. [Google Scholar]
- Ebuehi, O.M.; Campbell, P.C. Attraction and retention of qualified health workers to rural areas in Nigeria: A case study of four LGAs in Ogun State, Nigeria. Rural Remote Health 2011, 11, 1515. [Google Scholar] [CrossRef] [PubMed]
- Nwankwo, O.N.O.; Ugwu, C.I.; Nwankwo, G.I.; Akpoke, M.A.; Anyigor, C.; Obi-Nwankwo, U.; Andrew, S., Jr.; Nwogu, K.; Spicer, N. A qualitative inquiry of rural-urban inequalities in the distribution and retention of healthcare workers in southern Nigeria. PLoS ONE 2022, 17, e0266159. [Google Scholar] [CrossRef] [PubMed]
- Umunna, J.I. The scope and challenges of rural surgical practice in Nigeria. Niger J. Surg. 2011, 17, 25–28. [Google Scholar] [CrossRef]
- Increasing Access to Health Workers in Remote and Rural Areas through Improved Retention: Global Policy Recommendations; World Health Organization: Geneva, Switzerland, 2010.
- Adebayo, O.; Igbokwe, M.; Kanmodi, K.; Amoo, A.; Olaopa, O.; Oiwoh, S.; Kpuduwei, S.P.K.; Grillo, E.; Babalola, R.; Popoola, G.; et al. Practice, perception, and associations of peer learning among resident doctors in Nigeria: CHARTING Study. Med. Univ. 2020, 3, 100–109. [Google Scholar] [CrossRef]
- Sackin, P.; Barnett, M.; Eastaugh, A.; Paxton, P. Peer-supported learning. Br. J. Gen. Pract. 1997, 47, 67–68. [Google Scholar]
- Kanmodi, K.K.; Kanmodi, P.A. Rising prevalence of head and neck cancer risk factors among Nigerian adolescents: A call for school-based intervention programmes. Popul. Med. 2020, 2, 13. [Google Scholar] [CrossRef]
- Vannier, S.A.; Byers, E.S. A qualitative study of university students’ perceptions of oral sex, intercourse, and intimacy. Arch. Sex Behav. 2013, 42, 1573–1581. [Google Scholar] [CrossRef]
- Chambers, W.C. Oral sex: Varied behaviors and perceptions in a college population. J. Sex Res. 2007, 44, 28–42. [Google Scholar] [CrossRef]
- Prinstein, M.J.; Meade, C.S.; Cohen, G.L. Adolescent oral sex, peer popularity, and perceptions of best friends’ sexual behavior. J. Pediatr. Psychol. 2003, 28, 243–249. [Google Scholar] [CrossRef] [PubMed]
- Strome, A.; Moore-Petinak, N.; Waselewski, M.; Chang, T. Youths’ Knowledge and Perceptions of Health Risks Associated with Unprotected Oral Sex. Ann. Fam. Med. 2022, 20, 72–76. [Google Scholar] [CrossRef] [PubMed]
- Doull, M.; Wolowic, J.; Saewyc, E.; Rosario, M.; Prescott, T.; Ybarra, M.L. Why Girls Choose Not to Use Barriers to Prevent Sexually Transmitted Infection During Female-to-Female Sex. J. Adolesc. Health 2018, 62, 411–416. [Google Scholar] [CrossRef] [PubMed]
- Muzny, C.A.; Harbison, H.S.; Pembleton, E.S.; Hook, E.W.; Austin, E.L. Misperceptions regarding protective barrier method use for safer sex among African-American women who have sex with women. Sex Health 2013, 10, 138–141. [Google Scholar] [CrossRef] [PubMed]
- Kanmodi, K.K.; Amoo, B.A.; Sopeju, A.E.; Adeniyi, O.R. Oral cancer and oral sex: Awareness and practice among nursing students in Ibadan metropolis, Nigeria. Asian J. Med. Health 2017, 2, AJMAH.29935. [Google Scholar] [CrossRef]
- Kanmodi, K.; Fagbule, O.; Ogunniyi, K.; Ogbeide, M.; Samuel, V.; Aliemeke, E.; Olatunji, Y.; Isola, T.; Adewuyi, H.; Musa, S. Determinants of sexual practices among secondary school students in Nigeria: Focusing on socio-cultural and school-related factors. Rwanda Med. J. 2020, 77, 32–37. [Google Scholar]
- Salami, A.; Kanmodi, K.K.; Nnyanzi, L.A. Re-emphasizing the roles of general medical and dental practitioners regarding oral cancer eradication in Nigeria. Acta Med. Martiniana 2021, 21, 90–102. [Google Scholar] [CrossRef]
- Alpert, J.S. If You Are Not a Liberal When You Are Young, You Have No Heart, and If You Are Not a Conservative When Old, You Have No Brain. Am. J. Med. 2016, 129, 647–648. [Google Scholar] [CrossRef][Green Version]
- Kanmodi, K.K.; Evbuomwan, O.; Nwafor, N.J.; Omoruyi, E. Healthcare practitioners’ experience and perceptions on ICT-related training programs: An online survey. Egypt J. Med. Educ. 2020, 5, 2. [Google Scholar]
- Meiklejohn, J.; Connor, J.; Kypri, K. The effect of low survey response rates on estimates of alcohol consumption in a general population survey. PLoS ONE 2012, 7, e35527. [Google Scholar] [CrossRef]
- McKernan, S.C.; Reynolds, J.C.; McInroy, B.; Damiano, P.C. Randomized experiment on the effect of incentives and mailing strategy on response rates in a mail survey of dentists. J. Public Health Dent. 2022, 82, 484–490. [Google Scholar] [CrossRef] [PubMed]
| Variable | Frequency/Value | Percentage |
|---|---|---|
| Age (Years) | ||
| 20–29 | 74 | 22.4 |
| 30–39 | 176 | 53.3 |
| 40–49 | 66 | 20.0 |
| 50–59 | 10 | 3.0 |
| 60 & above | 4 | 1.2 |
| Mean (±SD) | 35.0 (±7.2) | Not applicable |
| Gender | ||
| Female | 122 | 37.0 |
| Male | 206 | 62.4 |
| Transgender | 1 | 0.3 |
| Prefer not to say | 1 | 0.3 |
| Marital Status | ||
| Married/With Partner | 215 | 65.2 |
| Single | 107 | 32.4 |
| Widowed | 4 | 1.2 |
| Divorced/Separated | 4 | 1.2 |
| Specialty | ||
| Medical Doctor | 217 | 65.8 |
| Dentist | 72 | 21.8 |
| Nurse/Midwife | 30 | 9.1 |
| Clinical Pharmacist | 11 | 3.3 |
| Place of Practice | ||
| Primary healthcare setting | 28 | 8.5 |
| Secondary healthcare setting | 70 | 21.2 |
| Tertiary healthcare setting | 232 | 70.3 |
| Ownership of the Place of Practice | ||
| Private | 55 | 16.7 |
| Public | 272 | 82.4 |
| No response | 3 | 0.9 |
| Years of Practice | ||
| <1 year | 2 | 0.6 |
| 1–10 years | 206 | 62.4 |
| 11–20 years | 109 | 33.0 |
| >20 years | 1 | 0.3 |
| No response | 12 | 3.6 |
| Mean (±SD) | 9 (±6.1) | Not applicable |
| Questions | Frequency | Percentage |
|---|---|---|
| Do you have adequate knowledge about oral sex? | ||
| Yes | 213 | 64.5 |
| No | 32 | 9.7 |
| Not sure | 85 | 25.8 |
| Have you read a peer reviewed journal on oral sex/STIs in the past 6 months? | ||
| Yes | 50 | 15.2 |
| No | 279 | 84.5 |
| Uncertain | 1 | 0.3 |
| Oral sex is a low-risk sexual activity | ||
| True | 55 | 16.7 |
| False | 230 | 69.7 |
| Do not know | 45 | 13.6 |
| Have you ever heard of a tongue condom before this interview? | ||
| Yes | 64 | 19.4 |
| No | 264 | 80.0 |
| Do not know | 2 | 0.6 |
| Have you ever seen a tongue condom (oral/mouth condom)? | ||
| Yes | 15 | 4.5 |
| No | 313 | 94.8 |
| Do not know | 2 | 0.6 |
| Have you heard of a dental dam before this interview? | ||
| Yes | 124 | 37.6 |
| No | 203 | 61.5 |
| Do not know | 3 | 0.9 |
| Have you ever seen a dental dam? | ||
| Yes | 78 | 23.6 |
| No | 251 | 76.1 |
| Do not know | 1 | 0.3 |
| Are you knowledgeable on how to make improvise barriers for safer oral sex? | ||
| Yes | 28 | 8.5 |
| No | 295 | 89.4 |
| Unsure | 7 | 2.1 |
| Factors that make oral sex unsafe * | ||
| incoming into contact with genital secretions | 259 | 78.5 |
| Not checking for cuts or lesions in the mouth or genitals before oral sex | 279 | 84.5 |
| Not knowing the sexually transmitted diseases status of oneself/partner | 302 | 91.5 |
| Not using barriers during oral sex | 197 | 59.7 |
| Poor oral hygiene | 207 | 62.7 |
| Presence of periodontal diseases while engaging in oral sex | 227 | 68.8 |
| Protective measures that make oral sex safer * | ||
| Consistent and proper use of barriers while having oral sex | 195 | 59.1 |
| Ensuring a good oral health | 230 | 69.7 |
| Ensure there are no genital lesions before engaging in oral sex | 265 | 80.3 |
| Ensuring there are no cuts/lesions in the mouth before engaging in oral sex | 280 | 84.8 |
| Ensuring you/your partner(s) are free from STIs | 300 | 90.9 |
| Ensuring that you and or your partner(s) are vaccinated against preventable STIs | 255 | 77.3 |
| Good oral hygiene | 222 | 67.3 |
| Variable | Frequency | Percentage |
|---|---|---|
| Ever had oral sex (n = 330) | ||
| Yes | 183 | 55.5 |
| No | 141 | 42.7 |
| Not sure | 6 | 1.8 |
| Period of first oral sex (n = 183) | ||
| <1 week | 10 | 5.5 |
| about 1 month ago | 26 | 14.2 |
| <6 months | 28 | 15.3 |
| 2–5 years | 36 | 19.6 |
| 6–10 years | 35 | 19.1 |
| >10 years | 30 | 16.4 |
| Could not remember | 21 | 11.5 |
| Ever used any measure/precaution to prevent STIs while having oral sex (n = 183) | ||
| Yes | 19 | 10.4 |
| No | 164 | 89.6 |
| Measure/Precaution taken (n = 19) | ||
| Genital condom | 13 | 68.4 |
| Improvised barrier | 5 | 26.3 |
| Immediate rinsing of the mouth after every act | 1 | 5.3 |
| Tongue condom/Dental dam | 2 | 10.5 |
| Good oral hygiene e.g checking for cuts, rashes, ensuring good bath | 1 | 5.3 |
| Willingness to use protection for oral sex (n = 164) | ||
| Yes | 141 | 86.0 |
| No | 23 | 14.0 |
| Questions | Frequency | Percentage |
|---|---|---|
| Have you ever had patients ask you questions about safe oral sex? | ||
| Yes | 121 | 36.7 |
| No | 203 | 61.5 |
| No response | 6 | 1.8 |
| Do you ever discussed the risk of oral sex with patients? | ||
| Yes | 158 | 47.9 |
| No | 167 | 50.6 |
| No response | 5 | 1.5 |
| Have you had to recommend any form of protection for your patients having oral sex? | ||
| Yes | 72 | 21.8 |
| No | 249 | 75.5 |
| No response | 9 | 2.7 |
| Are you willing to recommend protection for your patients engaging in oral sex? | ||
| Yes | 294 | 89.1 |
| No | 25 | 7.6 |
| No response | 12 | 3.3 |
| How do you feel when you advise your patients to use protection during oral sex? | ||
| Great, that is in their best interest | 188 | 57.0 |
| Never had to advise any patient | 20 | 6.1 |
| Unsure of feeling | 1 | 0.3 |
| Too rigid for patients | 25 | 7.6 |
| Unbothered/Indifferent | 46 | 13.9 |
| No response | 47 | 14.2 |
| Questions | Frequency | Percentage |
|---|---|---|
| Have you ever had a discussion on oral sex in any clinical/academic meeting? | ||
| Yes | 105 | 31.8 |
| No | 221 | 67.0 |
| No response | 4 | 1.2 |
| Are you willing to discuss oral sex in clinical/academic meetings? | ||
| Yes | 291 | 88.2 |
| No | 36 | 10.9 |
| No response | 3 | 0.9 |
| Are you willing to discuss oral sex in community health engagement/advocacy meetings? | ||
| Yes | 280 | 84.8 |
| No | 44 | 13.3 |
| No response | 6 | 1.8 |
| Variable/Question | n | Willingness to Recommend Protection for Patients Engaging in Oral Sex | X2 (p-Value) | |
|---|---|---|---|---|
| Yes (%) | No (%) | |||
| Gender | ||||
| Female | 116 | 109 (94.0) | 7 (6.0) | 1.04 (0.792) |
| Male | 201 | 183 (91.0) | 18 (9.0) | |
| Prefer not to say | 1 | 1 (100.0) | 0 (0.0) | |
| Transgender | 1 | 1 (100.0) | 0 (0.0) | |
| Age (Years) | ||||
| 20–29 | 72 | 68 (94.4) | 4 (5.6) | 3.60 (0.463) |
| 30–39 | 172 | 159 (92.4) | 13 (7.6) | |
| 40–49 | 61 | 55 (90.2) | 6 (9.8) | |
| 50–59 | 11 | 10 (90.9) | 1 (9.1) | |
| 60 & above | 3 | 2 (66.7) | 1 (33.3) | |
| Marital Status | ||||
| Divorced/Separated | 4 | 4 (100.0) | 0 (0.0) | 1.81 (0.612) |
| Married/With Partner | 207 | 188 (90.8) | 19 (9.2) | |
| Single | 104 | 98 (94.2) | 6 (5.8) | |
| Widowed | 4 | 4 (100.0) | 0 (0.0) | |
| Specialty | ||||
| Dentist | 72 | 65 (90.3) | 7 (9.7) | 1.88 (0.597) |
| Medical doctor | 210 | 193 (91.9) | 17 (8.1) | |
| Nurse/midwife | 26 | 25 (96.2) | 1 (3.8) | |
| Clinical pharmacist | 11 | 11 (100.0) | 0 (0.0) | |
| Place of Practice | ||||
| Primary Healthcare setting | 28 | 27 (96.4) | 1 (3.6) | 2.58 (0.275) |
| Secondary Healthcare setting | 68 | 65 (95.6) | 3 (4.4) | |
| Tertiary Healthcare setting | 223 | 202 (90.6) | 21 (9.4) | |
| Ownership of the Place of Practice | ||||
| Private | 53 | 48 (90.6) | 5 (9.4) | 3.02 (0.220) |
| Public | 263 | 244 (92.8) | 19 (7.2) | |
| Oral sex is a low-risk sexual activity | ||||
| True | 55 | 52 (94.5) | 3 (5.5) | 9.23 (0.010) |
| False | 221 | 207 (93.7) | 14 (6.3) | |
| Not sure | 40 | 32 (80.0) | 8 (20.0) | |
| Have you ever heard of a tongue condom before this interview? | ||||
| Yes | 62 | 62 (100.0) | 0 (0.0) | 6.60 (0.010) |
| No | 255 | 230 (90.2) | 25 (9.8) | |
| Have you heard of a dental dam before this interview? | ||||
| Yes | 123 | 116 (94.3) | 7 (5.7) | 1.36 (0.243) |
| No | 193 | 175 (90.7) | 18 (9.3) | |
| Oral Sex History | ||||
| Yes | 181 | 171 (94.5) | 10 (5.5) | 2.65 (0.103) |
| No | 134 | 120 (89.6) | 14 (10.4) | |
| Ever used any measure/precaution to prevent STIs while having oral sex | ||||
| Yes | 16 | 15 (5.1) | 1 (4.0) | 0.01 (0.928) |
| No | 234 | 218 (74.1) | 16 (64.0) | |
| Knowledgeable on the improvised barriers for safer oral sex | ||||
| Yes | 28 | 26 (92.9) | 2 (7.1) | 0.02 (0.878) |
| No | 289 | 266 (92.0) | 23 (8.0) | |
| Have you ever had a discussion on oral sex in any clinical/academic meeting? | ||||
| Yes | 103 | 99 (96.1) | 4 (3.9) | 2.93 (0.087) |
| No | 215 | 195 (90.7) | 20 (9.3) | |
| Are you willing to discuss oral sex in clinical/academic meetings? | ||||
| Yes | 284 | 269 (94.7) | 15 (5.3) | 23.40 (<0.001) |
| No | 35 | 25 (71.4) | 10 (28.6) | |
| Are you willing to discuss oral sex in community health engagement/advocacy meetings? | ||||
| Yes | 273 | 260 (95.2) | 13 (4.8) | 22.94 (<0.001) |
| No | 43 | 32 (74.4) | 11 (25.6) | |
| Question | Response | Adjusted OR | 95% C.I. for Adjusted OR | p-Value | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Oral sex is a low-risk sexual activity | True (ref) | ||||
| False | 3.48 | 0.79 | 15.35 | 0.100 | |
| Not sure | 3.06 | 1.07 | 8.69 | 0.036 | |
| Are you willing to discuss oral sex in clinical/academic meetings? | No (ref) | ||||
| Yes | 0.30 | 0.08 | 1.06 | 0.061 | |
| Are you willing to discuss oral sex in community health engagement/advocacy meetings? | No (ref) | ||||
| Yes | 0.38 | 0.11 | 1.30 | 0.123 | |
| Have you ever heard of a tongue condom before this interview? | No (ref) | ||||
| Yes | 0.00 | 0.00 | 0.00 | 0.997 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kanmodi, K.K.; Nwafor, J.N.; Eze, U.A.; Amoo, B.A.; Salami, A.A.; Almu, B.; Ogbeide, M.E.; Obute, P.E.; Aladelusi, T.; Adebayo, O.; et al. Factors Determining the Willingness of Nigerian Clinicians to Recommend Protected Oral Sex: An Online Exploratory Study. Oral 2022, 2, 299-315. https://doi.org/10.3390/oral2040029
Kanmodi KK, Nwafor JN, Eze UA, Amoo BA, Salami AA, Almu B, Ogbeide ME, Obute PE, Aladelusi T, Adebayo O, et al. Factors Determining the Willingness of Nigerian Clinicians to Recommend Protected Oral Sex: An Online Exploratory Study. Oral. 2022; 2(4):299-315. https://doi.org/10.3390/oral2040029
Chicago/Turabian StyleKanmodi, Kehinde Kazeem, Jacob Njideka Nwafor, Ugochukwu Anthony Eze, Babatunde Abiodun Amoo, Afeez Abolarinwa Salami, Bello Almu, Mike Eghosa Ogbeide, Precious Ehi Obute, Timothy Aladelusi, Oladimeji Adebayo, and et al. 2022. "Factors Determining the Willingness of Nigerian Clinicians to Recommend Protected Oral Sex: An Online Exploratory Study" Oral 2, no. 4: 299-315. https://doi.org/10.3390/oral2040029
APA StyleKanmodi, K. K., Nwafor, J. N., Eze, U. A., Amoo, B. A., Salami, A. A., Almu, B., Ogbeide, M. E., Obute, P. E., Aladelusi, T., Adebayo, O., & Nnyanzi, L. A. (2022). Factors Determining the Willingness of Nigerian Clinicians to Recommend Protected Oral Sex: An Online Exploratory Study. Oral, 2(4), 299-315. https://doi.org/10.3390/oral2040029







