Bond Strength between CAD/CAM PMMA Denture Base Resins and Characterisation Composites
Abstract
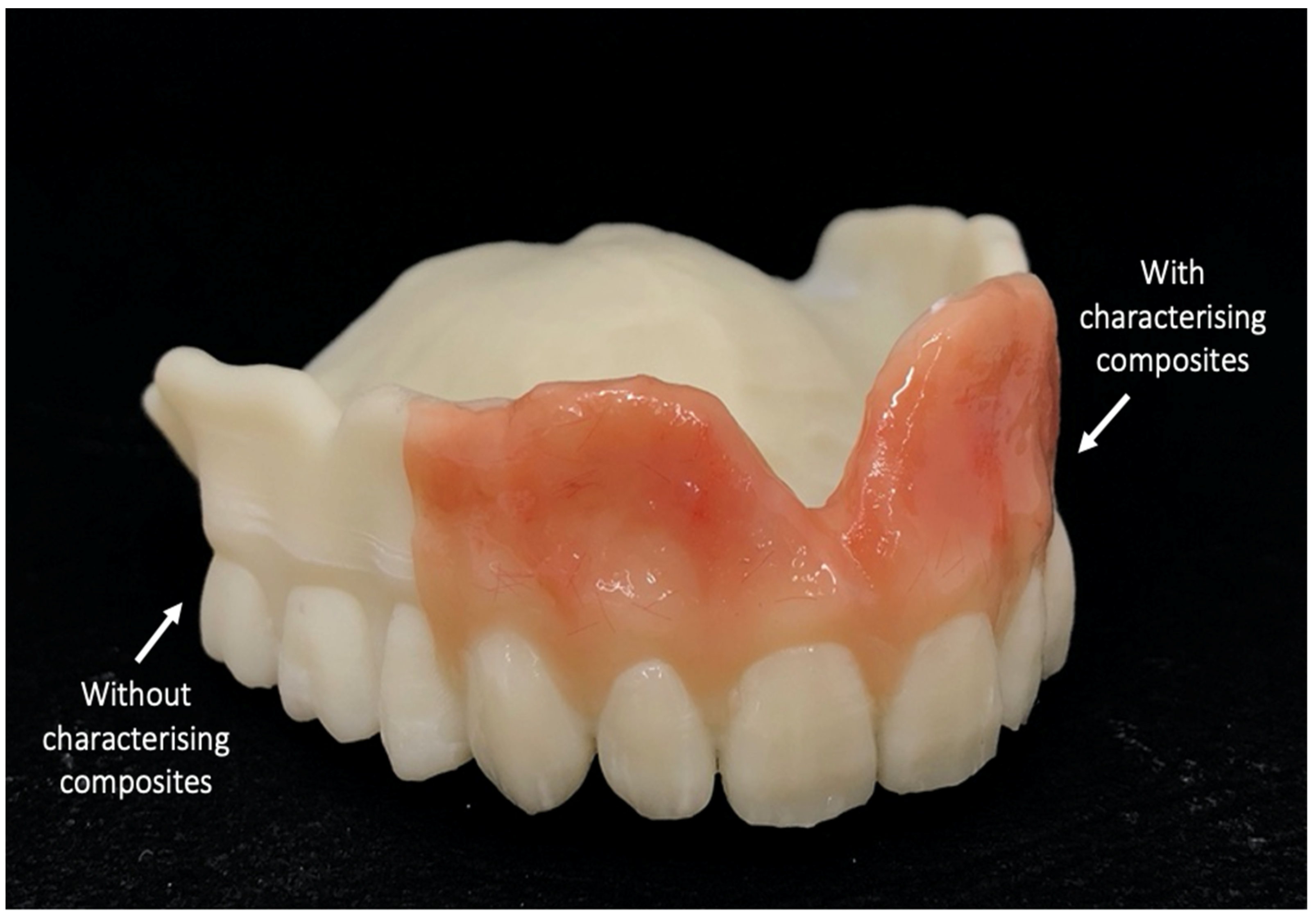
:1. Introduction
2. Materials and Methods
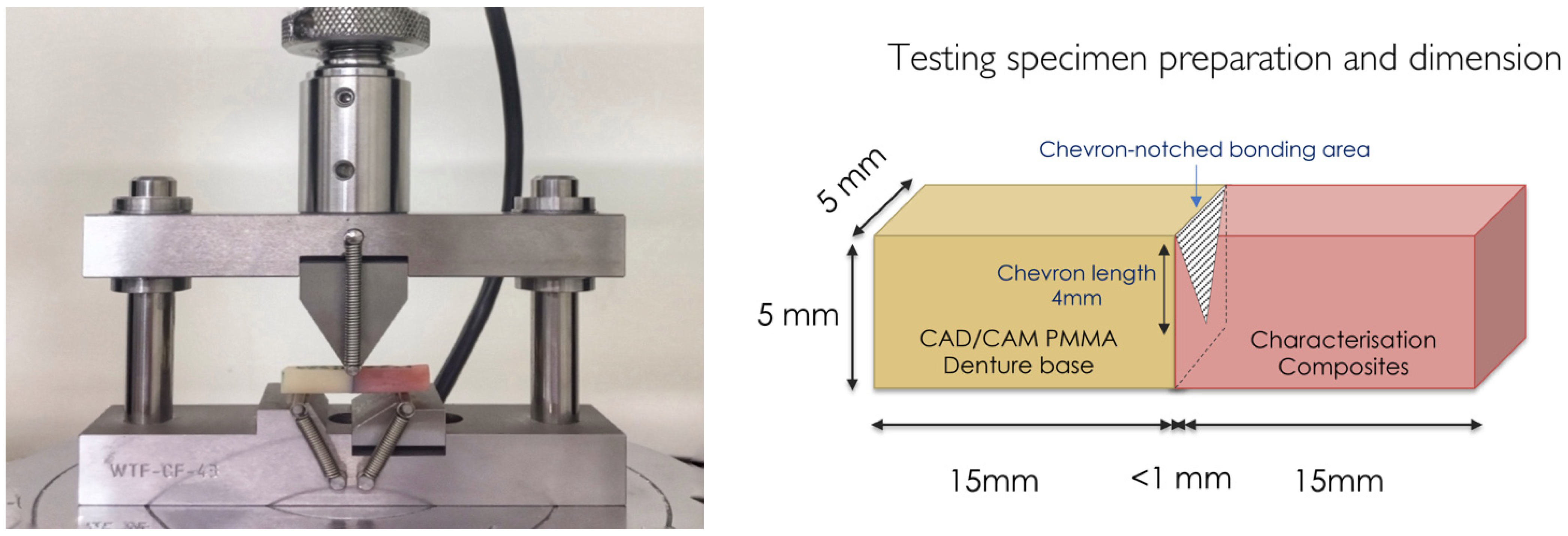
2.1. Specimen Fabrication
2.2. Surface Treatment and Characterisation of the Composite–Resin Bonding
2.3. Mechanical Testing of the Bonded Specimens
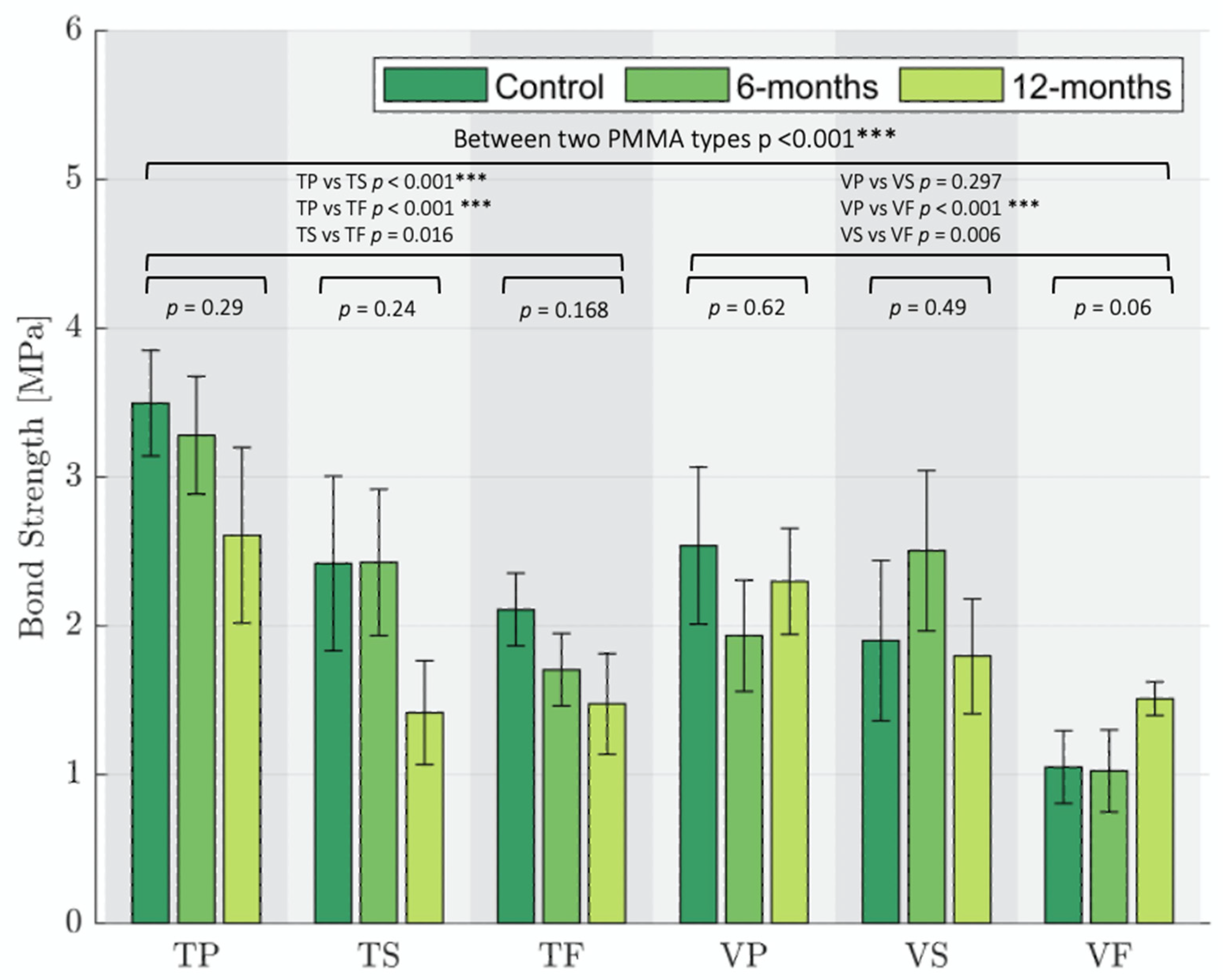
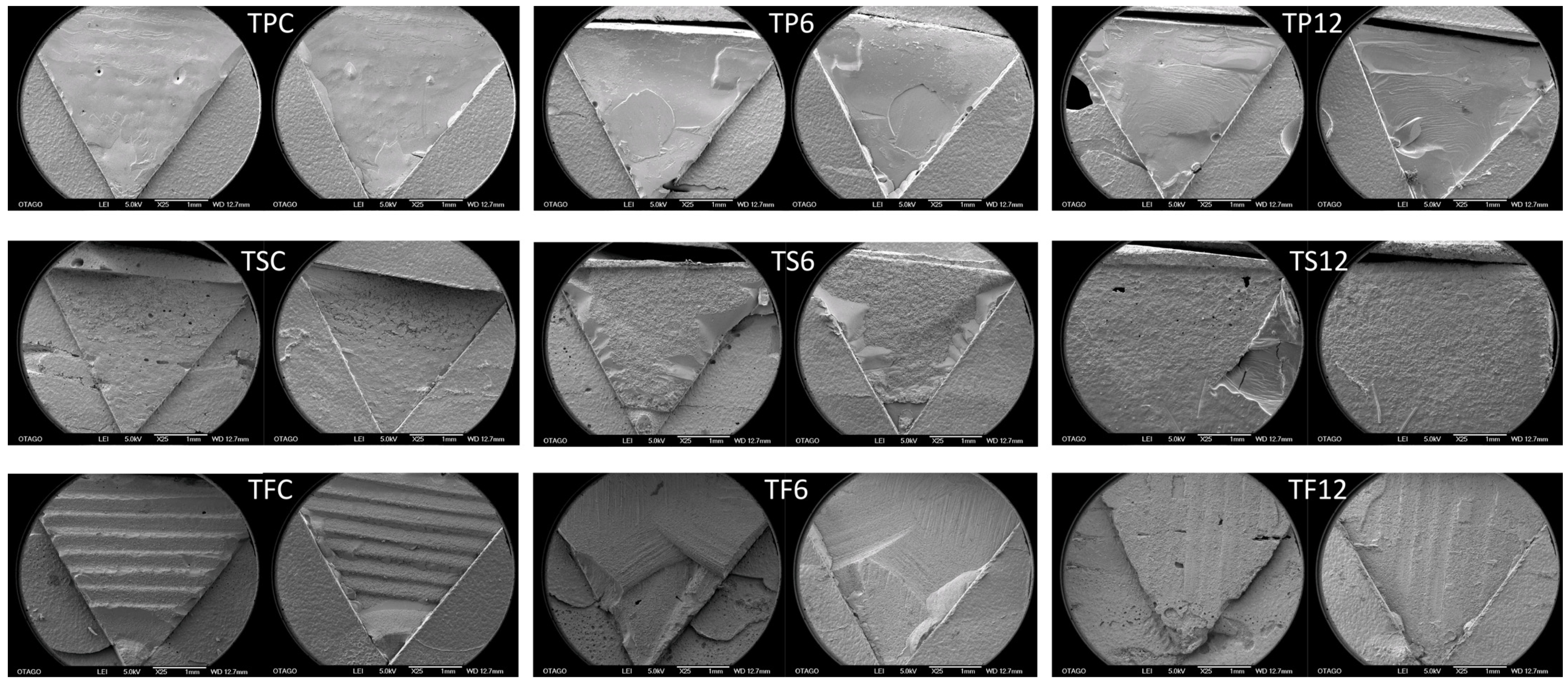
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Davidowitz, G.; Kotick, P.G. The Use of CAD/CAM in Dentistry. Dent. Clin. N. Am. 2011, 55, 559–570. [Google Scholar] [CrossRef] [PubMed]
- Mörmann, W.H. The evolution of the CEREC system. J. Am. Dent. Assoc. 2006, 137, 7S–13S. [Google Scholar] [CrossRef]
- Janeva, N.M.; Kovacevska, G.; Elencevski, S.; Panchevska, S.; Mijoska, A.; Lazarevska, B. Advantages of CAD/CAM versus Conventional Complete Dentures—A Review. Open Access Maced. J. Med Sci. 2018, 6, 1498–1502. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Srivastava, R.; Choukse, V. Characterization of complete denture. Int. J. Dent. Clin. 2011, 3, 56–59. [Google Scholar]
- Proctor, H.H. Characterization of dentures. J. Prosthet. Dent. 1953, 3, 339–349. [Google Scholar] [CrossRef]
- Shenoy, P.B. A Survey on the Denture Esthetics and the Denture Base Characteriztion-Questionnaire Based Study. J. Pharm. Sci. Res. 2018, 10, 956–957. [Google Scholar]
- Andreescu, C.F.; Ghergic, D.L.; Botoaca, O.; Hancu, V.; Banateanu, A.M.; Patroi, D.N. Evaluation of Different Materials Used for Fabrication of Complete Digital Denture. Mater. Plast. 2018, 55, 124–128. [Google Scholar] [CrossRef]
- Bonfante, E.A.; Suzuki, M.; Hirata, R.; Bonfante, G.; Fardin, V.P.; Coelho, P.G. Resin composite repair for implant-supported crowns. J. Biomed. Mater. Res. Part B Appl. Biomater. 2017, 105, 1481–1489. [Google Scholar] [CrossRef]
- Arpa, C.; Ceballos, L.; Fuentes, M.V.; Perdigão, J. Repair bond strength and nanoleakage of artificially aged CAD-CAM composite resin. J. Prosthet. Dent. 2019, 121, 523–530. [Google Scholar] [CrossRef]
- Shimizu, H.; Dds, T.K.; Yoshida, K.; Tsue, F.; Takahashi, Y. Effect of Surface Preparation on the Failure Load of a Highly Filled Composite Resin Bonded to a Denture Base Resin. J. Prosthodont. 2009, 18, 684–687. [Google Scholar] [CrossRef]
- Scherrer, S.S.; Cesar, P.; Swain, M. Direct comparison of the bond strength results of the different test methods: A critical literature review. Dent. Mater. 2010, 26, e78–e93. [Google Scholar] [CrossRef] [PubMed]
- Maurin, J.-C.; Lagneau, C.; Durand, M.; Lissac, M.; Seux, D. Tensile and shear bond strength evaluation of a total-etch three-step and two self-etching one-step dentin bonding systems. J Adhes Dent 2006, 8, 27–30. [Google Scholar] [PubMed]
- Visuttiwattanakorn, P.; Suputtamongkol, K.; Angkoonsit, D.; Kaewthong, S.; Charoonanan, P. Microtensile bond strength of repaired indirect resin composite. J. Adv. Prosthodont. 2017, 9, 38–44. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Choi, J.J.E.; Uy, C.E.; Plaksina, P.; Ramani, R.S.; Ganjigatti, R.; Waddell, J.N. Bond Strength of Denture Teeth to Heat-Cured, CAD/CAM and 3D Printed Denture Acrylics. J. Prosthodont. 2020, 29, 415–421. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.J.E.; Ramani, R.S.; Ganjigatti, R.; Uy, C.E.; Plaksina, P.; Waddell, J.N. Adhesion of Denture Characterizing Composites to Heat-Cured, CAD/CAM and 3D Printed Denture Base Resins. J. Prosthodont. 2021, 30, 83–90. [Google Scholar] [CrossRef]
- Katsoulis, J.; Müller, P.; Mericske-Stern, R.; Blatz, M.B. CAD/CAM fabrication accuracy of long-vs. short-span implant-supported FDP s. Clin. Oral Implant. Res. 2015, 26, 245–249. [Google Scholar] [CrossRef] [Green Version]
- Perea-Lowery, L.; Gibreel, M.; Vallittu, P.K.; Lassila, L. Characterization of the mechanical properties of CAD/CAM polymers for interim fixed restorations. Dent. Mater. J. 2020, 39, 319–325. [Google Scholar] [CrossRef] [Green Version]
- Soderholm, K.-J. Review of the fracture toughness approach. Dent. Mater. 2010, 26, e63–e77. [Google Scholar] [CrossRef]
- Gale, M.; Darvell, B. Thermal cycling procedures for laboratory testing of dental restorations. J. Dent. 1999, 27, 89–99. [Google Scholar] [CrossRef]
- Wiegand, A.; Stucki, L.; Hoffmann, R.; Attin, T.; Stawarczyk, B. Repairability of CAD/CAM high-density PMMA- and composite-based polymers. Clin. Oral Investig. 2015, 19, 2007–2013. [Google Scholar] [CrossRef]
- Rosca, B.; Ramalho, S.; Sampaio-Fernandes, J.C.; Portugal, J. Reparability of two different CAD/CAM polymer materials using a light-cured composite and universal adhesives. Rev. Port. Estomatol. Med. Dentária E Cir. Maxilofac. 2016, 57, 189–196. [Google Scholar] [CrossRef] [Green Version]
- Van Meerbeek, B.; Peumans, M.; Poitevin, A.; Mine, A.; Van Ende, A.; Neves, A.; De Munck, J. Relationship between bond-strength tests and clinical outcomes. Dent. Mater. 2010, 26, e100–e121. [Google Scholar] [CrossRef] [PubMed]
- Sirisha, K.; Ravishankar, Y.; Ravikumar, P.; Rambabu, T. Validity of bond strength tests: A critical review-Part II. J. Conserv. Dent. 2014, 17, 420–426. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dogan, A.; Korkmaz, T.; Dogan, O.M.; Keskin, S.; Demir, H. Tensile Bond Strength of a Highly Cross-Linked Denture Tooth to the Compression-Molded and Injection-Molded Denture Base Polymers. J. Adhes. 2009, 85, 953–970. [Google Scholar] [CrossRef]
- Grzebiuluch, W.; Mikulewicz, M.; Kaczmarek, U. Resin composite materials for chairside CAD/CAM restorations: A comparison of selected mechanical properties. J. Healthc. Eng. 2021, 8828954. [Google Scholar] [CrossRef]
- Raszewski, Z.; Nowakowska-Toporowska, A.; Weżgowiec, J.; Nowakowska, D.; Więckiewicz, W. Influence of silanized silica and silanized feldspar addition on the mechanical behaviour of polymethyl methacrylate resin denture teeth. J. Prosthet. Dent. 2020, 123, 647. [Google Scholar] [CrossRef]
- Albeladi, H.; Al-Romaizan, A.; Hussein, M. Role of cross-linking process on the performance of PMMA. Int. J. Biosens. Bioelectron. 2017, 3, 279–284. [Google Scholar]
- Choi, J.E.; Ng, T.E.; Leong, C.K.; Kim, H.; Li, P.; Waddell, J.N. Adhesive evaluation of three types of resilient denture liners bonded to heat-polymerized, autopolymerized, or CAD-CAM acrylic resin denture bases. J. Prosthet. Dent. 2018, 120, 699–705. [Google Scholar] [CrossRef]
- Amaral, R.; Özcan, M.; Bottino, M.A.; Valandro, L.F. Microtensile bond strength of a resin cement to glass infiltrated zirconia-reinforced ceramic: The effect of surface conditioning. Dent. Mater. 2006, 22, 283–290. [Google Scholar] [CrossRef]
- Grzebieluch, W.; Kowalewski, P.; Grygier, D.; Rutkowska-Gorczyca, M.; Kozakiewicz, M.; Jurczyszyn, K. Printable and machinable dental restorative composites for CAD/CAM application-comparison of mechanical properites, fractographic, texture and fractal dimension analysis. Materials 2021, 14, 4919. [Google Scholar] [CrossRef]
- Araújo, P.; Sayer, C.; Giudici, R.; Poco, J.G. Techniques for reducing residual monomer content in polymers: A review. Polym. Eng. Sci. 2002, 42, 1442–1468. [Google Scholar] [CrossRef]
- Ayman, A.-D. The residual monomer content and mechanical properties of CAD\CAM resins used in the fabrication of complete dentures as compared to heat cured resins. Electron. Physician 2017, 9, 4766–4772. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klziber, D.; Spintzyk, S.; Geis-Gerstorfer, J.; Klink, A.; Unkovskiy, A.; Huettig, F. Bonding behaviour of conventional PMMA towards industrial CAD/CAM PMMA and artificial resin teeth for complete denture manufacturing in a digital workflow. Materials 2021, 14, 3822. [Google Scholar] [CrossRef] [PubMed]
- Kuscu, E.; Klink, A.; Spintzyk, S.; Fernandez, P.K.; Huettig, F. Bonding Interface and Repairability of 3D-Printed Intraoral Splints: Shear Bond Strength to Current Polymers, with and without Ageing. Materials 2021, 14, 3935. [Google Scholar] [CrossRef]


| Material | Composition | Abbreviation | Manufacturer | |
|---|---|---|---|---|
| CAD/CAM Milled PMMA Base Materials | Telio CAD |
| T | Ivoclar Vivodent, Schaan, Liechtenstein |
| Vivodent CAD |
| V | Ivoclar Vivodent, Schaan, Liechtenstein | |
| Characterising Composite Resins | Pala Cre-ative |
| P | Kulzer, South Bend, Indiana, USA |
| SR Nexco |
| S | Ivoclar Vivodent, Schaan, Liechtenstein | |
| Ceramage |
| F | Shofu, Kyoto, Japan |
| Fracture Toughness (MPa√m ± SD) | Bond Strength (MPa ± SD) | |||||
|---|---|---|---|---|---|---|
| Groups | Control | 6-Months | 12-Months | Control | 6-Months | 12-Months |
| TP | 1.59 ± 0.34 | 1.39 ± 0.32 | 1.12 ± 0.44 | 3.49 ± 0.86 | 3.28 ± 0.96 | 2.61 ± 1.43 |
| TS | 1.07 ± 0.55 | 0.87 ± 0.31 | 0.52 ± 0.0.3 | 2.42 ± 1.43 | 2.42 ± 1.19 | 1.42 ± 0.85 |
| TF | 0.98 ± 0.28 | 0.72 ± 0.24 | 0.6 ± 0.29 | 2.10 ± 0.59 | 1.67 ± 0.62 | 1.47 ± 0.82 |
| VP | 1.05 ± 0.42 | 0.86 ± 0.5 | 1.13 ± 0.44 | 2.53 ± 1.28 | 1.93 ± 0.91 | 2.29 ± 0.87 |
| VS | 0.8 ± 0.47 | 1.02 ± 0.57 | 0.71 ± 0.29 | 1.9 ± 1.32 | 2.50 ± 1.31 | 1.79 ± 0.94 |
| VF | 0.56 ± 0.27 | 0.47 ± 0.4 | 0.69 ± 0.12 | 1.05 ± 0.59 | 1.02 ± 0.67 | 1.51 ± 0.27 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pong, M.T.; Grymak, A.; Waddell, J.N.; Choi, J.J.E. Bond Strength between CAD/CAM PMMA Denture Base Resins and Characterisation Composites. Oral 2022, 2, 75-87. https://doi.org/10.3390/oral2010009
Pong MT, Grymak A, Waddell JN, Choi JJE. Bond Strength between CAD/CAM PMMA Denture Base Resins and Characterisation Composites. Oral. 2022; 2(1):75-87. https://doi.org/10.3390/oral2010009
Chicago/Turabian StylePong, Mei Ting, Anastasiia Grymak, John Neil Waddell, and Joanne Jung Eun Choi. 2022. "Bond Strength between CAD/CAM PMMA Denture Base Resins and Characterisation Composites" Oral 2, no. 1: 75-87. https://doi.org/10.3390/oral2010009
APA StylePong, M. T., Grymak, A., Waddell, J. N., & Choi, J. J. E. (2022). Bond Strength between CAD/CAM PMMA Denture Base Resins and Characterisation Composites. Oral, 2(1), 75-87. https://doi.org/10.3390/oral2010009






