Curing through Ceramics: Influence of Different Light-Curing Units and Curing Modes on Bond Strength
Abstract
:1. Introduction
2. Material and Methods
2.1. Specimen Preparation
2.2. Light Curing
2.3. Interfacial Bond Strength Test
- F = load at failure (N)
- L = distance from bonded interface to loading point
- E = elastic modulus of 3D-printed beam (4.16 GPa)
- D = cross sectional area of 3D-printed beam
2.4. Degree of Conversion (DC)
2.5. Mode of Failure and Surface Analysis
2.6. Statistical Analysis
3. Results
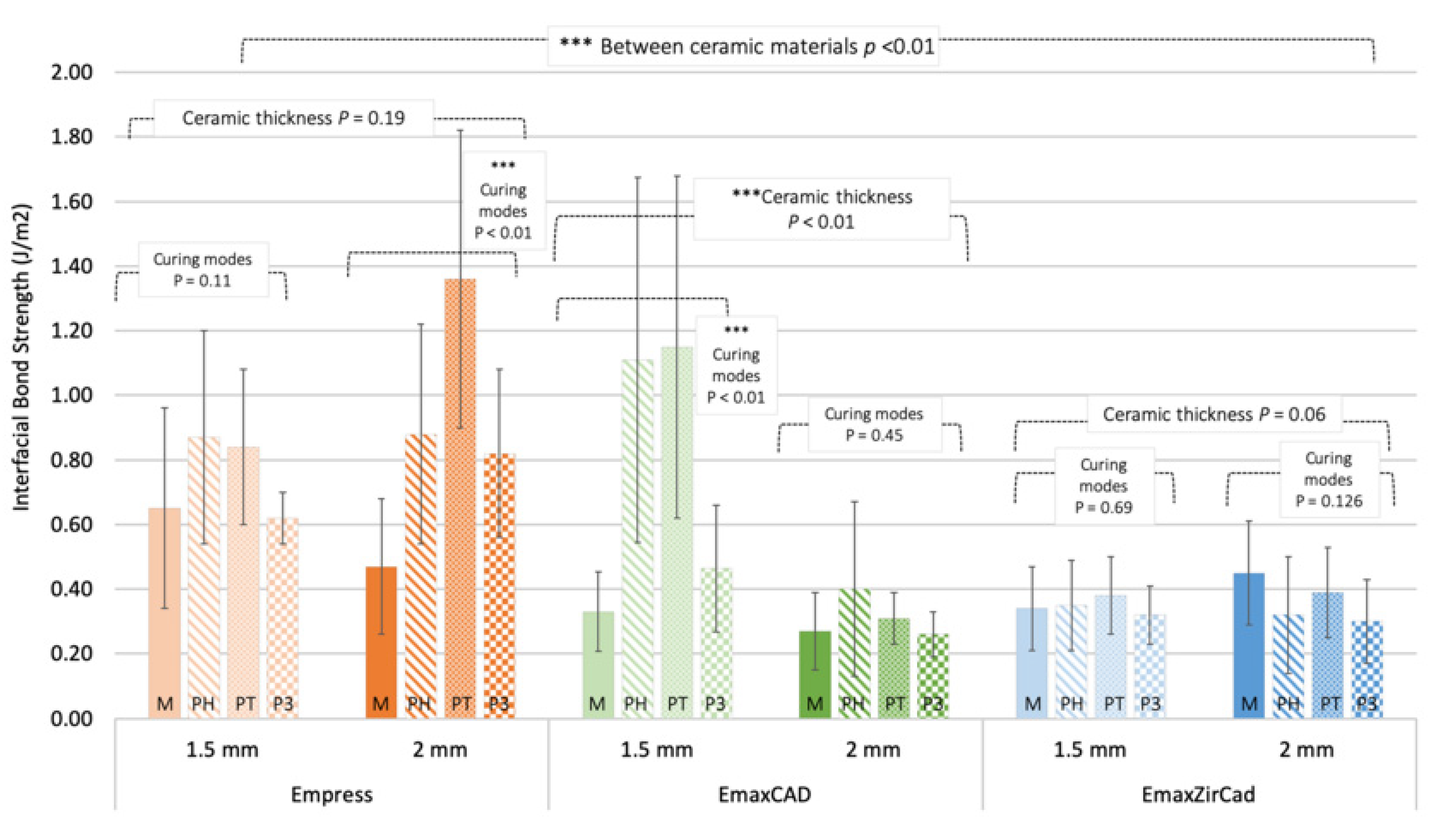
3.1. Interfacial Bond Strength
3.2. Degree of Cure
3.3. Mode of Failure and Surface Analysis
4. Discussion
5. Conclusions
- Increasing translucency of ceramics results in higher bond strength, as evidenced by Leucite-reinforced (Empress) > Lithium disilicate (Emax CAD) > Zirconia (Emax ZirCAD) ceramics.
- Increasing ceramic thickness lowers bond strength, which was especially significant in lithium disilicate ceramics.
- The use of polywave LCU in curing through ceramics generally resulted in greater bond strength compared to monowave LCU.
- The use of different curing modes had a significant effect on the degree of cure of resin cement.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Christensen, G.J. Is the rush to all-ceramic crowns justified? J. Am. Dent. Assoc. 2014, 145, 192–194. [Google Scholar] [CrossRef] [PubMed]
- Warreth, A.; Elkareimi, Y. All-ceramic restorations: A review of the literature. Saudi Dent. J. 2020, 32, 365–372. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Kelly, J.R. Dental ceramics for restoration and metal veneering. Dent. Clin. N. Am. 2017, 61, 797–819. [Google Scholar] [CrossRef] [PubMed]
- Brunton, P.A.; Sharif, M.O.; Creanor, S.; Burke, F.J.T.; Wilson, N.H.F. Contemporary dental practice in the UK in 2008: Indirect restorations and fixed prosthodontics. Br. Dent. J. 2012, 212, 115–119. [Google Scholar] [CrossRef] [PubMed]
- Brunton, P.A.; Ratnayake, J.; Loch, C.; Veerasamy, A.; Cathro, P.; Lee, R. Indirect restorations and fixed prosthodontics: Materials and techniques used by general dentists of New Zealand. Int. Dent. J. 2019, 2019, 5210162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zafar, M.S.; Amin, F.; Fareed, M.A.; Ghabbani, H.; Riaz, S.; Khurshid, Z. Biomimetic aspects of restorative dentistry biomaterials. Biomimetics 2020, 5, 34. [Google Scholar] [CrossRef]
- Bajraktarova-Valjakova, E.; Korunoska-Stevkovska, V.; Kapusevska, B.; Gigovski, N.; Bajraktarova-Misevska, C.; Grozdanov, A. Contemporary dental ceramic materials, A review: Chemical composition, physical and mechanical properties, indications for use. Maced. J. Med. Sci. 2018, 6, 1742–1755. [Google Scholar] [CrossRef] [Green Version]
- Lawson, N.C.; Frazier, K.; Bedran-Russo, A.K.; Khajotia, S.; Park, J.; Urquhart, O. Zirconia restorations: An american dental association clinical evaluators panel survey. J. Am. Dent. Assoc. 2021, 152, 80–81.e2. [Google Scholar] [CrossRef]
- Cadenaro, M.; Maravic, T.; Comba, A.; Mazzoni, A.; Fanfoni, L.; Hilton, T. The role of polymerization in adhesive dentistry. Dent. Mater. 2019, 35, e1–e22. [Google Scholar] [CrossRef]
- Zhang, L.; Luo, X.P.; Tan, R.X. Effect of Light-cured resin cement application on translucency of ceramic veneers and light transmission of LED polymerization units. J. Prosthodont. 2019, 28, e376–e382. [Google Scholar] [CrossRef] [Green Version]
- Passos, S.P.; Kimpara, E.T.; Bottino, M.A.; Júnior, G.C.S.; Rizkalla, A.S. Bond strength of different resin cement and ceramic shades bonded to dentin. J. Adhes. Dent. 2013, 15, 461–466. [Google Scholar] [PubMed]
- Novais, V.R.; Raposo, L.H.; Miranda, R.R.; Lopes, C.C.; Simamoto, P.C.J.; Soares, C.J. Degree of conversion and bond strength of resin-cements to feldspathic ceramic using different curing modes. J. Appl. Oral Sci. 2017, 25, 61–68. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wingo, K. A review of dental cements. J. Vet. Dent. 2018, 35, 18–27. [Google Scholar] [CrossRef] [Green Version]
- Price, R.B.; Ferracane, J.L.; Hickel, R.; Sullivan, B. The light-curing unit: An essential piece of dental equipment. Int. Dent. J. 2020, 70, 407–417. [Google Scholar] [CrossRef] [PubMed]
- Price, R.B.; Ferracane, J.L.; Shortall, A.C. Light-curing units: A review of what we need to know. J. Dent. Res. 2015, 94, 1179–1186. [Google Scholar] [CrossRef]
- Rueggeberg, F.A.; Giannini, M.; Arrais, C.A.G.; Price, R.B.T. Light curing in dentistry and clinical implications: A literature review. Braz. Oral Res. 2017, 31 (Suppl. 1), e61. [Google Scholar] [CrossRef] [Green Version]
- Gan, J.K.; Yap, A.U.; Cheong, J.W.; Arista, N.; Tan, C. Bulk-fill composites: Effectiveness of cure with poly- and monowave curing lights and modes. Oper. Dent. 2018, 43, 136–143. [Google Scholar] [CrossRef]
- AlShaafi, M.M.; AlQahtani, M.Q.; Price, R.B. Effect of exposure time on the polymerization of resin cement through ceramic. J. Adhes. Dent. 2014, 16, 129–135. [Google Scholar]
- Barutcigil, K.; Büyükkaplan, U. The effect of thickness and translucency of polymer-infiltrated ceramic-network material on degree of conversion of resin cements. J. Adv. Prosthodont. 2020, 12, 61–66. [Google Scholar] [CrossRef]
- Faria, E.S.A.L.; Pfeifer, C.S. Effectiveness of high-power LEDs to polymerize resin cements through ceramics: An in vitro study. J. Prosthet. Dent. 2017, 118, 631–636. [Google Scholar]
- Ilie, N.; Stawarczyk, B. Quantification of the amount of blue light passing through monolithic zirconia with respect to thickness and polymerization conditions. J. Prosthet. Dent. 2015, 113, 114–121. [Google Scholar] [CrossRef]
- Sulaiman, T.A.; Abdulmajeed, A.A.; Donovan, T.E.; Ritter, A.V.; Lassila, L.V.; Vallittu, P.K. Degree of conversion of dual-polymerizing cements light polymerized through monolithic zirconia of different thicknesses and types. J. Prosthet. Dent. 2015, 114, 103–108. [Google Scholar] [CrossRef] [PubMed]
- Turkoglu, P.; Sen, D. Evaluation of dual-cure resin cement polymerization under different types and thicknesses of monolithic zirconia. Biomed. Res. Int. 2019, 2019, 4567854. [Google Scholar] [CrossRef] [PubMed]
- Caprak, Y.O.; Turkoglu, P.; Akgungor, G. Does the translucency of novel monolithic CAD/CAM materials affect resin cement polymerization with different curing modes? J. Prosthodont. 2019, 28, e572–e579. [Google Scholar] [CrossRef]
- Oh, S.; Shin, S.-M.; Kim, H.-J.; Paek, J.; Kim, S.-J.; Yoon, T.H. Influence of glass-based dental ceramic type and thickness with identical shade on the light transmittance and the degree of conversion of resin cement. Int. J. Oral Sci. 2018, 10, 5. [Google Scholar] [CrossRef] [PubMed]
- Duran, İ.; Kaleli, N.; Ural, Ç.; Kavut, İ. Evaluation of the light transmission of chairside polymer infiltrated hybrid ceramics in different shades and thicknesses. J. Appl. Biomater. Funct. Mater. 2019, 17, 2280800018807109. [Google Scholar] [CrossRef] [Green Version]
- Cheng, Y.S.; Douglas, W.H.; Versluis, A.; Tantbirojn, D. Analytical study on a new bond test method for measuring adhesion. Eng. Fract. Mech. 1999, 64, 117–123. [Google Scholar] [CrossRef]
- Pacheco, R.R.; Carvalho, A.O.; Andre, C.B.; Ayres, A.P.A.; de Sa, R.B.C.; Dias, T.M. Effect of indirect restorative material and thickness on light transmission at different wavelengths. J. Prosthodont. Res. 2019, 63, 232–238. [Google Scholar] [CrossRef]
- Fu, L.; Engqvist, H.; Xia, W. Glass-ceramics in dentistry: A Review. Materials 2020, 13, 1049. [Google Scholar] [CrossRef] [Green Version]
- Mendonca, L.M.; Ramalho, I.S.; Lima, L.; Pires, L.A.; Pegoraro, T.A.; Pegoraro, L.F. Influence of the composition and shades of ceramics on light transmission and degree of conversion of dual-cured resin cements. J. Appl. Oral Sci. 2019, 27, e20180351. [Google Scholar] [CrossRef] [Green Version]
- Alkhudhairy, F.; AlKheraif, A.; Naseem, M.; Khan, R.; Vohra, F. Degree of conversion and depth of cure of Ivocerin containing photo-polymerized resin luting cement in comparison to conventional luting agents. Pak. J. Med. Sci. 2018, 34, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Delgado, A.J.; Castellanos, E.M.; Coelho Sinhoreti, M.A.; De Oliveira, D.C.R.S.; Abdulhameed, N.; Geraldeli, S. The use of different photoinitiator systems in photopolymerizing resin cements through ceramic veneers. Oper. Dent. 2019, 44, 396–404. [Google Scholar] [CrossRef]
- Chen, Y.; Yao, C.; Huang, C.; Wang, Y. The effect of monowave and polywave light-polymerization units on the adhesion of resin cements to zirconia. J. Prosthet. Dent. 2019, 121, 549.e1–549.e7. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Lin, H.L.; Zheng, M.; Ozcan, M.; Yu, H. Minimum radiant exposure and irradiance for triggering adequate polymerization of a photo-Polymerized resin cement. Materials 2021, 14, 2341. [Google Scholar] [CrossRef] [PubMed]
- Lanza, M.D.S.; Andreeta, M.R.B.; Pegoraro, T.A.; Pegoraro, L.F.; Carvalho, R.M. Influence of curing protocol and ceramic composition on the degree of conversion of resin cement. J. Appl. Oral Sci. 2017, 25, 700–707. [Google Scholar] [CrossRef] [PubMed]
- Von Fraunhofer, J.A. Adhesion and Cohesion. Int. J. Dent. 2012, 2012, 951324. [Google Scholar] [CrossRef]
- Li, R.; Ma, S.Q.; Zang, C.C.; Zhang, W.Y.; Liu, Z.H.; Sun, Y.C. Enhanced bonding strength between lithium disilicate ceramics and resin cement by multiple surface treatments after thermal cycling. PLoS ONE 2019, 14, e0220466. [Google Scholar] [CrossRef]
- Flury, S.; Lussi, A.; Hickel, R.; Ilie, N. Light curing through glass ceramics with a second- and a third-generation LED curing unit: Effect of curing mode on the degree of conversion of dual-curing resin cements. Clin. Oral. Investig. 2013, 17, 2127–2137. [Google Scholar] [CrossRef] [Green Version]
- Flury, S.; Lussi, A.; Hickel, R.; Ilie, N. Light curing through glass ceramics: Effect of curing mode on micromechanical properties of dual-curing resin cements. Clin. Oral Investig. 2014, 18, 809–818. [Google Scholar] [CrossRef]







| Type of LCU | Monowave | Polywave | ||
|---|---|---|---|---|
| Curing Modes | - | High | Turbo | 3-s |
| Irradiance (W/cm2) | 1470 | 1200 | 2100 | 3000 |
| Curing time (s) | 10 | 10 | 5 | 3 |
| Ceramic Type | Empress | EmaxCAD | EmaxZirCAD | ||||
|---|---|---|---|---|---|---|---|
| Ceramic Thickness (mm) | 1.5 | 2 | 1.5 | 2 | 1.5 | 2 | |
| LCUs & Curing Modes | |||||||
| M | 0.65 ± 0.31 | 0.47 ± 0.21 | 0.33 ± 0.12 | 0.27 ± 0.12 | 0.34 ± 0.13 | 0.45 ± 0.16 | |
| PH | 0.87 ± 0.33 | 0.88 ± 0.34 | 1.11 ± 0.57 | 0.40 ± 0.27 | 0.35 ± 0.14 | 0.32 ± 0.18 | |
| PT | 0.84 ± 0.24 | 1.36 ± 0.46 | 1.15 ± 0.53 | 0.31 ± 0.08 | 0.38 ± 0.12 | 0.39 ± 0.14 | |
| P3 | 0.62 ± 0.08 | 0.82 ± 0.26 | 0.46 ± 0.20 | 0.26 ± 0.07 | 0.32 ± 0.09 | 0.30 ± 0.13 | |
| Ceramic Type | Empress | EmaxCAD | EmaxZirCAD | ||||
|---|---|---|---|---|---|---|---|
| Ceramic Thickness (mm) | 1.5 | 2 | 1.5 | 2 | 1.5 | 2 | |
| LCUs & Curing Modes | |||||||
| M | 55.71 ± 7.45 | 58.82 ± 8.44 | 58.82 ± 8.44 | 59.80 ± 15.15 | 59.56 ± 10.40 | 48.35 ± 10.75 | |
| PH | 57.70 ± 12.17 | 58.68 ± 5.59 | 48.94 ± 5.22 | 47.04 ± 6.79 | 44.16 ± 7.08 | 50.52 ± 10.36 | |
| PT | 50.66 ± 4.40 | 49.74 ± 4.40 | 51.66 ± 7.93 | 50.02 ± 5.38 | 44.66 ± 9.13 | 49.25 ± 6.86 | |
| P3 | 60.48 ± 5.19 | 54.73 ± 12.32 | 42.51 ± 9.95 | 51.01 ± 4.18 | 36.02 ± 8.46 | 47.74 ± 8.60 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Phua, E.M.J.; Waddell, J.N.; Choi, J.J.E. Curing through Ceramics: Influence of Different Light-Curing Units and Curing Modes on Bond Strength. Oral 2022, 2, 62-74. https://doi.org/10.3390/oral2010008
Phua EMJ, Waddell JN, Choi JJE. Curing through Ceramics: Influence of Different Light-Curing Units and Curing Modes on Bond Strength. Oral. 2022; 2(1):62-74. https://doi.org/10.3390/oral2010008
Chicago/Turabian StylePhua, Evonne Mei Jing, John Neil Waddell, and Joanne Jung Eun Choi. 2022. "Curing through Ceramics: Influence of Different Light-Curing Units and Curing Modes on Bond Strength" Oral 2, no. 1: 62-74. https://doi.org/10.3390/oral2010008
APA StylePhua, E. M. J., Waddell, J. N., & Choi, J. J. E. (2022). Curing through Ceramics: Influence of Different Light-Curing Units and Curing Modes on Bond Strength. Oral, 2(1), 62-74. https://doi.org/10.3390/oral2010008





