Abstract
This study presents the development of an ultraviolet-C (UVC)-enabled smart bandage embedded with a temperature sensor, designed for the treatment and management of chronic wounds. The bandage also incorporates an RGB light-emitting diode (LED) and a microcontroller. It features a high-precision temperature sensor with an accuracy of ±0.1 °C for real-time wound temperature monitoring. The UVC LED is employed to eliminate bacteria on wound surfaces, while an RGB LED, controlled by a microcontroller, signals the need for treatment and any changes in wound temperature. The strip is etched on a 25 µm thick Kapton film to offer flexibility and comfort for wearing on the body and is seamlessly integrated into a cotton crepe bandage, forming a smart bandage. The embedded electronics are protected from wound exudates with a conformal polyurethane encapsulant film. Initial results indicate that the sensor achieves an accuracy of 97% in free space, inside a bandage, and on the human body.
1. Introduction
Chronic wounds, unlike acute injuries, require continuous monitoring and specialized treatment for effective healing. UVC LEDs, emitting within the 265 to 285 nm range, exhibit antibacterial properties, offering an efficient means of disinfecting wound surfaces. The integration of UVC-based treatment technology and the real-time monitoring of wound parameters in smart bandages holds great promise for enhancing the treatment and management of chronic wounds [1,2,3].
A previous study proposed a battery-free smart bandage incorporating UVC LEDs, powered by wireless power transfer (WPT), for disinfecting chronic wound surfaces [4]. However, the proposed design lacks the real-time monitoring of crucial wound-related parameters, such as temperature, moisture, and pH levels, essential for assessing the healing process [5]. Localized wound temperatures may surpass 37 °C due to congestion and inflammation; nevertheless, abrupt increases in wound temperatures serve as indicators of infection [5]. Consequently, temperature measurements during clinical assessments may provide vital insights into the wound’s condition.
To address this limitation, this study introduces a UVC LED strip embedded with a temperature sensor, TMP117 from Texas Instruments (Dallas, TX, USA), and encapsulated within a fabric crepe bandage specifically designed for the treatment of chronic wounds. The embedded temperature sensor has a resolution of ±0.1 °C and shows an accuracy of over 97% when compared to those of a commercial thermocouple, Kane-May, KM330 from Comark InstrumentS (Norwich, Norfolk, UK). The performance of the temperature sensor in the presence of wound exudate is preliminarily simulated by enclosing the sensor in a wet bandage, and the results indicate that the embedded sensor still maintains its accuracy.
2. UVC-Enabled Smart Bandage Design
The proposed smart bandage comprises a flexible PCB strip integrated into a cotton fabric bandage housing several key components, as depicted in Figure 1: (i) a Vishay (Malvern, Pennsylvania, USA) UVC LED, VLMU35CL2-275-120; (ii) a high-accuracy temperature sensor, TMP117, from Texas Instruments (Dallas, TX, USA); (iii) an RGB LED; (iv) an Attiny84 microcontroller from Microchip Technology (Chandler, Arizona, USA); and (v) a boost converter. The UVC LED functions to disinfect wound surfaces, while the temperature sensor continuously monitors the real-time temperature of chronic wounds. Controlled by the microcontroller, the RGB LED indicates the necessity for treatment and any fluctuations in temperature. Additionally, the microcontroller manages the system’s operation, and the boost converter ensures a stable DC voltage output for the UVC LED.
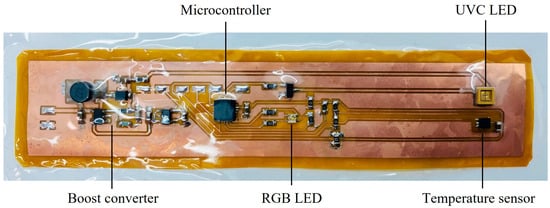
Figure 1.
Flexible UVC LED strip embedded with a temperature sensor for smart bandages.
The circuit design was etched using a 25 µm thick Kapton film, making the design fully flexible, as shown in Figure 2 and therefore well suited for wearable applications. The design incorporates six pads for the SPI interface, facilitating microcontroller programming. The temperature sensor is linked with the microcontroller using the I2C protocol. Given the UVC LED’s high voltage requirement (>5 V), a transistor is employed to regulate the UVC LED with a pulse width modulation (PWM) signal from the microcontroller. Furthermore, the embedded electronics are shielded from wound exudates using a conformal polyurethane encapsulant film applied by vacuum forming. The smart bandage is powered by 3.3 V coin batteries.
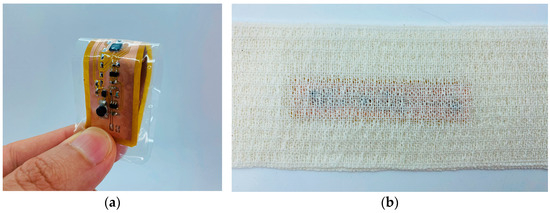
Figure 2.
(a) Incorporating a flexible design that allows for versatile healthcare applications, (b) integrated into a fabric crepe bandage, forming a smart bandage for chronic wounds’ care and management.
3. Measurements and Results
3.1. Temperature Measurement Setup
The temperature measurement setup is illustrated in Figure 3. A Thermo Scientific hotplate was used to generate various temperature ranges. Both the TMP117 sensor and the thermocouple (Kane-May, KM330) were placed at the center of the hotplate. The measurements were carried out at room temperature, ranging from 26 °C to 40 °C. Temperature readings were recorded for both the TMP117 sensor and the thermocouple.
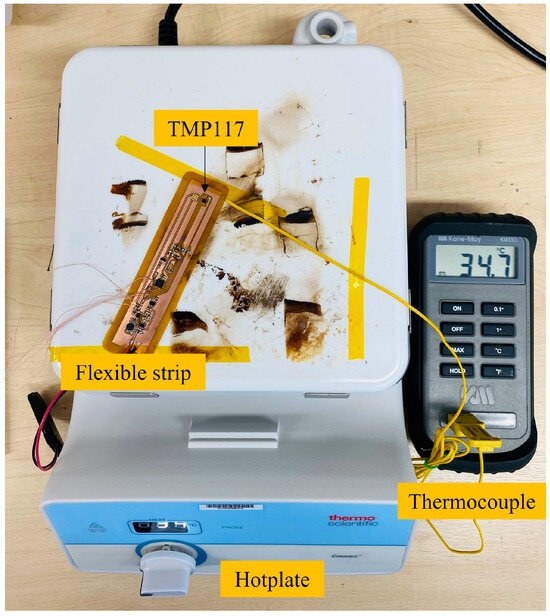
Figure 3.
Measurement setup for assessing the accuracy of the temperature sensor against the state-of-the-art thermocouple device.
3.2. Temperature Measurements
Measurements were conducted to evaluate the accuracy of the temperature sensor in four different scenarios: (i) free space, (ii) bandaged, (iii) wet bandaged, and (iv) mounted on the human arm without a bandage. The results demonstrate that the sensor achieves an accuracy exceeding 97% when compared to that of a commercial thermocouple (Kane-May, KM330), illustrated in Figure 4a. To measure the sensor’s performance in the presence of wound exudate, it was enclosed in a wet bandage. The results indicate that even in this scenario, the embedded sensor maintains its accuracy, as shown in Figure 4b.
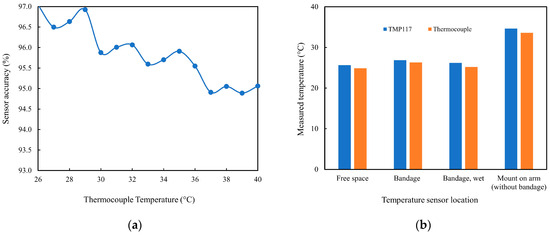
Figure 4.
(a) Accuracy of the embedded temperature sensor against a commercial thermocouple and (b) temperature sensor readings in four different scenarios.
4. Conclusions
We have developed a smart bandage for healthcare applications, incorporating a flexible UVC LED strip embedded with a temperature sensor and encapsulated within a fabric bandage. The strip seamlessly integrates into fabric bandages to treat chronic wounds and monitor wound-related parameters, such as temperature. The strip design is low profile and comfortable to the body, making it suitable for integration into fabric bandages for chronic wound applications. This smart bandage is programmable, enabling the customization of treatment duration and radiation dosage. Utilizing its RGB LED, it promptly indicates fluctuations in wound temperature, signaling the requirement for treatment. Our future focus involves integrating low-power Bluetooth technology into the smart bandage, enabling wireless data transmission and enhanced control capabilities.
Author Contributions
Conceptualization, I.U. and A.K.; methodology, I.U.; software, I.U.; validation, I.U., A.K., and S.P.B.; formal analysis, I.U.; investigation, I.U.; writing—original draft preparation, I.U.; writing—review and editing A.K.; supervision, S.P.B.; project administration, S.P.B.; funding acquisition, S.P.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by European Regional Development Fund (ERDF) via its Inter-reg V France (Channel) England programme: Smart Textile for Regional Industry and Smart Specialisation Sectors (SmartT). The work of Steve Beeby was supported by the Royal Academy of Engineering under the Chairs in Emerging Technologies Scheme.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are contained within the article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Tang, N.; Zheng, Y.; Jiang, X.; Zhou, C.; Jin, H.; Jin, K.; Wu, W.; Haick, H. Wearable Sensors and Systems for Wound Healing-Related pH and Temperature Detection. Micromachines 2021, 12, 430. [Google Scholar] [CrossRef] [PubMed]
- Farooqui, M.; Shamim, A. Low cost inkjet printed smart bandage for wireless monitoring of chronic wounds. Sci. Rep. 2016, 6, 28949. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Grabham, N.; Komolafe, A.; Tudor, J. Battery free smart bandage based on NFC RFID technology. In Proceedings of the IEEE International Conference on Flexible and Printable Sensors and Systems (FLEPS), Manchester, UK, 16–19 August 2020; pp. 1–4. [Google Scholar]
- Ullah, I.; Wagih, M.; Sun, Y.; Li, Y.; Hajdu, K.; Courson, R.; Dreanno, C.; Prado, E.; Komolafe, A.; Harris, N.R.; et al. Wirelessly powered drug-free and anti-infective smart bandage for chronic wound care. IEEE Trans. Biomed. Circuits Syst. 2023, 17, 900–915. [Google Scholar] [CrossRef] [PubMed]
- Darvishi, S.; Tavakoli, S.; Kharaziha, M.; Girault, H.H.; Kaminski, C.F.; Mela, I. Advances in the sensing and treatment of wound biofilms. Angew. Chem. Int. Ed. 2022, 134, e202112218. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).