Plan, Track, and Live Mindfully: Insights from the Eat Smart, Move More, Prevent Diabetes Program
Abstract
1. Introduction
2. Materials and Methods
2.1. Development
Theory of Planned Behavior
2.2. Delivery
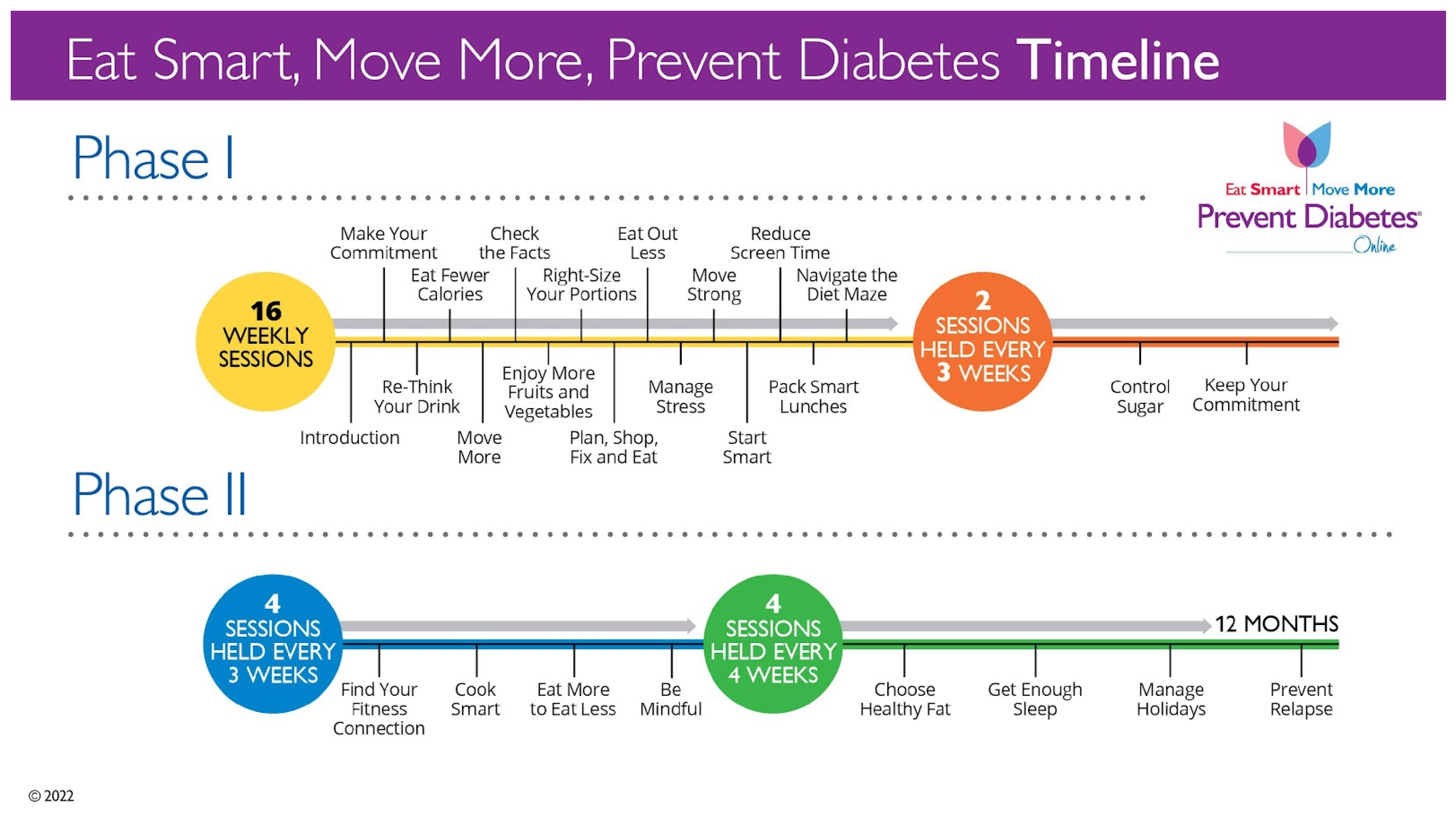
2.2.1. Curriculum Timeline and Lessons
2.2.2. Participant Resources
2.3. Core Components
2.3.1. Planning
2.3.2. Tracking
2.3.3. Living Mindfully
3. Results
4. Discussion
4.1. Limitations
4.2. Future Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- NIDDK. Type 2 Diabetes. Available online: https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/type-2-diabetes (accessed on 4 February 2025).
- Diabetes Complications. Available online: https://www.cdc.gov/diabetes/complications/index.html (accessed on 4 February 2025).
- Parker, E.D.; Lin, J.; Mahoney, T.; Ume, N.; Yang, G.; Gabbay, R.A.; ElSayed, N.A.; Bannuru, R.R. Economic costs of diabetes in the U.S. in 2022. Diabetes Care 2023, 47, 26–43. [Google Scholar] [CrossRef] [PubMed]
- Bullard, K.M.; Cowie, C.C.; Lessem, S.E.; Saydah, S.H.; Menke, A.; Geiss, L.S.; Orchard, T.J.; Rolka, D.B.; Imperatore, G. Prevalence of diagnosed diabetes in adults by diabetes type—United States, 2016. MMWR. Morb. Mortal. Wkly. Rep. 2018, 67, 359–361. [Google Scholar] [CrossRef] [PubMed]
- Knowler, W.; Nathan, D.; Walker, E.; Lochin, J.; Hamman, R.; Fowler, S.; Barrett-Connor, E. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N. Engl. J. Med. 2002, 346, 393–403. [Google Scholar] [PubMed]
- A1C Test for Diabetes and Prediabetes. Available online: https://www.cdc.gov/diabetes/diabetes-testing/prediabetes-a1c-test.html (accessed on 4 February 2025).
- 1 in 3 Americans Have Prediabetes. Available online: https://www.cdc.gov/diabetes/communication-resources/1-in-3-americans.html (accessed on 4 February 2025).
- Preventing Type 2 Diabetes. Available online: https://www.cdc.gov/diabetes/prevention-type-2/index.html (accessed on 4 February 2025).
- Prakoso, D.A.; Mahendradhata, Y.; Istiono, W. Family involvement to stop the conversion of prediabetes to diabetes. Korean J. Fam. Med. 2023, 44, 303–310. [Google Scholar] [CrossRef] [PubMed]
- NIDDK. Diabetes Prevention Program (DPP). Available online: https://www.niddk.nih.gov/about-niddk/research-areas/diabetes/diabetes-prevention-program-dpp (accessed on 4 February 2025).
- What is the National DPP? Available online: https://www.cdc.gov/diabetes-prevention/programs/what-is-the-national-dpp.html (accessed on 4 February 2025).
- PreventT2 Curriculum and Handouts. Available online: https://www.cdc.gov/diabetes-prevention/php/lifestyle-change-resources/t2-curriculum.html (accessed on 18 March 2025).
- CDC Diabetes Prevention Recognition Program. Centers for Disease Control and Prevention Diabetes Prevention Recognition Program Standards and Operating Procedures. Updated 2021. Available online: https://nationaldppcsc.cdc.gov/s/article/DPRP-Standards-and-Operating-Procedures (accessed on 18 March 2025).
- Collins, C.; McCallum, E.; Nordby, K.; Aggarwal, S.; Griffith, E.; Thomas, C.; Dunn, C. Enrollment, Engagement, and Effectiveness of a Large-Scale Diabetes Prevention Program Using Synchronous Distance Technology. Diabetology 2023, 4, 574–585. [Google Scholar] [CrossRef]
- Dunn, C.; Olabode-Dada, O.; Whetstone, L.; Thomas, C.; Aggarwal, S.; Nordby, K.; Thompson, S.; Johnson, M.; Allison, C. Using synchronous distance education to deliver a weight loss intervention: A randomized trial. Obesity 2015, 24, 44–50. [Google Scholar] [CrossRef] [PubMed]
- Etheridge, J.C.; Sinyard, R.D.; Brindle, M.E. Implementation research. In Translational Surgery; Academic Press: Cambridge, MA, USA, 2023; pp. 563–573. [Google Scholar]
- Hayes, J.F.; Balantekin, K.N.; Fitzsimmons-Craft, E.E.; Jackson, J.J.; Ridolfi, D.R.; Boeger, H.S.; Welch, R.R.; Wilfley, D.E. Greater average meal planning frequency predicts greater weight loss outcomes in a worksite-based Behavioral Weight Loss Program. Ann. Behav. Med. 2021, 55, 14–23. [Google Scholar] [CrossRef] [PubMed]
- Peng, S.; Othman, A.T.; Yuan, F.; Liang, J. The effectiveness of planning interventions for improving physical activity in the general population: A systematic review and meta-analysis of randomized controlled trials. Int. J. Environ. Res. Public Health 2022, 19, 7337. [Google Scholar] [CrossRef] [PubMed]
- Sniehotta, F.F.; Schwarzer, R.; Scholz, U.; Schüz, B. Action planning and coping planning for long-term lifestyle change: Theory and assessment. Eur. J. Soc. Psychol. 2005, 35, 565–576. [Google Scholar] [CrossRef]
- The Diabetes Prevention Program (DPP) Research Group. The Diabetes Prevention Program (DPP): Description of lifestyle intervention. Diabetes Care 2002, 25, 2165–2171. [Google Scholar] [CrossRef] [PubMed]
- Tang, H.-B.; Jalil, N.I.; Tan, C.-S.; He, L.; Zhang, S.-J. Why more successful? an analysis of participants’ self-monitoring data in an online weight loss intervention. BMC Public Health 2024, 24, 1–13. [Google Scholar] [CrossRef]
- Ingels, J.S.; Misra, R.; Stewart, J.; Lucke-Wold, B.; Shawley-Brzoska, S. The effect of adherence to dietary tracking on weight loss: Using HLM to model weight loss over time. J. Diabetes Res. 2017, 2017, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Patel, M.L.; Hopkins, C.M.; Brooks, T.L.; Bennett, G.G. Comparing self-monitoring strategies for weight loss in a smartphone app: Randomized Controlled Trial. JMIR mHealth uHealth 2019, 7, e12209. [Google Scholar] [CrossRef] [PubMed]
- Linde, J.A.; Jeffery, R.W.; Crow, S.J.; Brelje, K.L.; Pacanowski, C.R.; Gavin, K.L.; Smolenski, D.J. The tracking study: Description of a randomized controlled trial of variations on weight tracking frequency in a behavioral weight loss program. Contemp. Clin. Trials 2015, 40, 199–211. [Google Scholar] [CrossRef] [PubMed]
- Woods-Giscombe, C.L.; Gaylord, S.A.; Li, Y.; Brintz, C.E.; Bangdiwala, S.I.; Buse, J.B.; Mann, J.D.; Lynch, C.; Phillips, P.; Smith, S.; et al. A mixed-methods, randomized clinical trial to examine feasibility of a mindfulness-based stress management and diabetes risk reduction intervention for African Americans with Prediabetes. Evid.-Based Complement. Altern. Med. 2019, 2019, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Muñoz-Mireles, G.; Mantzios, M.; Schellinger, J.N.; Messiah, S.E.; Marroquín, E. Mindful eating as a tool for diabetes prevention and management: A review of potential mechanisms of action. Mindfulness 2023, 14, 2831–2847. [Google Scholar] [CrossRef]
- Rosenzweig, S.; Reibel, D.K.; Greeson, J.M.; Edman, J.S.; Jasser, S.A.; McMearty, K.D.; Goldstein, B.J. Mindfulness-based stress reduction is associated with improved glycemic control in type 2 diabetes mellitus: A pilot study. Altern. Ther. Health Med. 2007, 13, 36–38. [Google Scholar] [PubMed]
- Audet, C.M.; Roller, L.J.; Aliyu, M.H.; Rolando, L.; Alva, M.; Ali, M.; Schildcrout, J.S.; Chakkalakal, R. Evaluation of a workplace diabetes prevention program delivered via Distance Learning: A qualitative study. Health Educ. Behav. 2024, 52, 156–165. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
McCallum, E.; Nordby, K.; Aggarwal, S.; Lavelle, C.; Thomas, C.; Dunn, C. Plan, Track, and Live Mindfully: Insights from the Eat Smart, Move More, Prevent Diabetes Program. Diabetology 2025, 6, 42. https://doi.org/10.3390/diabetology6050042
McCallum E, Nordby K, Aggarwal S, Lavelle C, Thomas C, Dunn C. Plan, Track, and Live Mindfully: Insights from the Eat Smart, Move More, Prevent Diabetes Program. Diabetology. 2025; 6(5):42. https://doi.org/10.3390/diabetology6050042
Chicago/Turabian StyleMcCallum, Erin, Kelly Nordby, Surabhi Aggarwal, Christine Lavelle, Cathy Thomas, and Carolyn Dunn. 2025. "Plan, Track, and Live Mindfully: Insights from the Eat Smart, Move More, Prevent Diabetes Program" Diabetology 6, no. 5: 42. https://doi.org/10.3390/diabetology6050042
APA StyleMcCallum, E., Nordby, K., Aggarwal, S., Lavelle, C., Thomas, C., & Dunn, C. (2025). Plan, Track, and Live Mindfully: Insights from the Eat Smart, Move More, Prevent Diabetes Program. Diabetology, 6(5), 42. https://doi.org/10.3390/diabetology6050042




