Oxi-HA/ADH Hydrogels: A Novel Approach in Tissue Engineering and Regenerative Medicine
Abstract
:1. Introduction
2. Hyaluronic Acid Hydrogels
2.1. Molecular and Structural Domains
2.2. HA Hydrogels
2.3. HA Hydrogels in Tissue Engineering and Regenerative Medicine
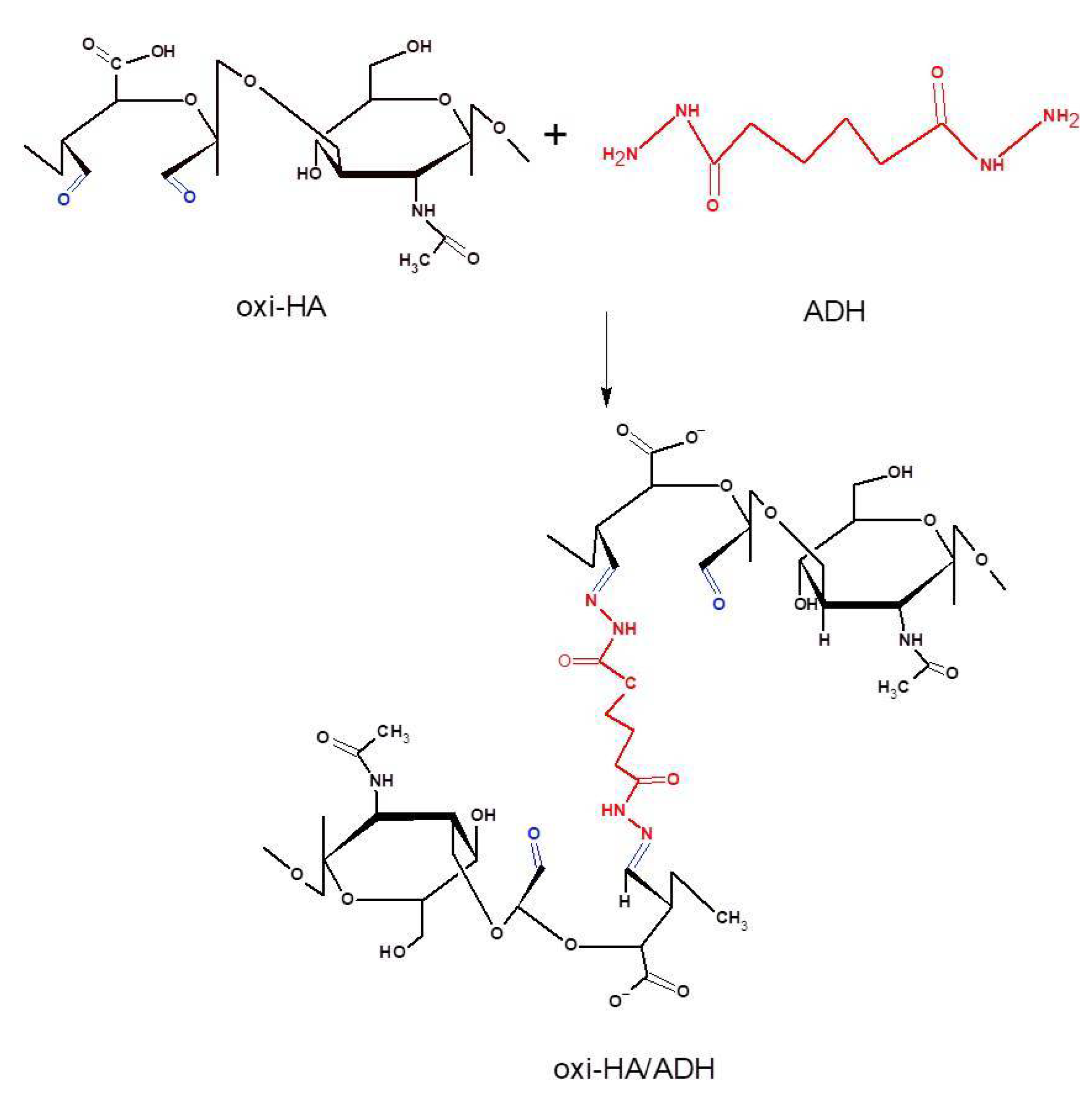
2.4. HA/ADH Hydrogels
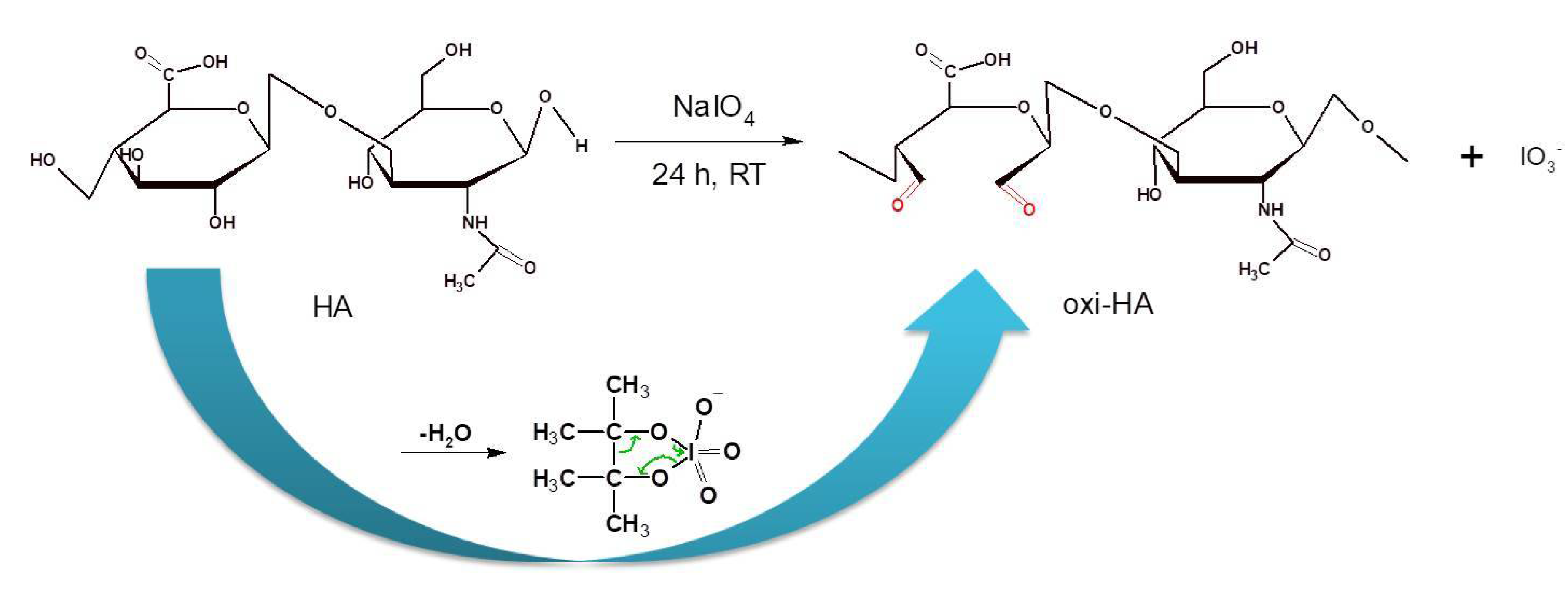
3. Partial Oxidation of Hyaluronic Acid (Oxi-HA)
4. Oxi-HA Cross-linkings and Conjugations
5. Oxi-HA/ADH Hydrogels
5.1. Partial Oxidation and Cross-linking Reactions
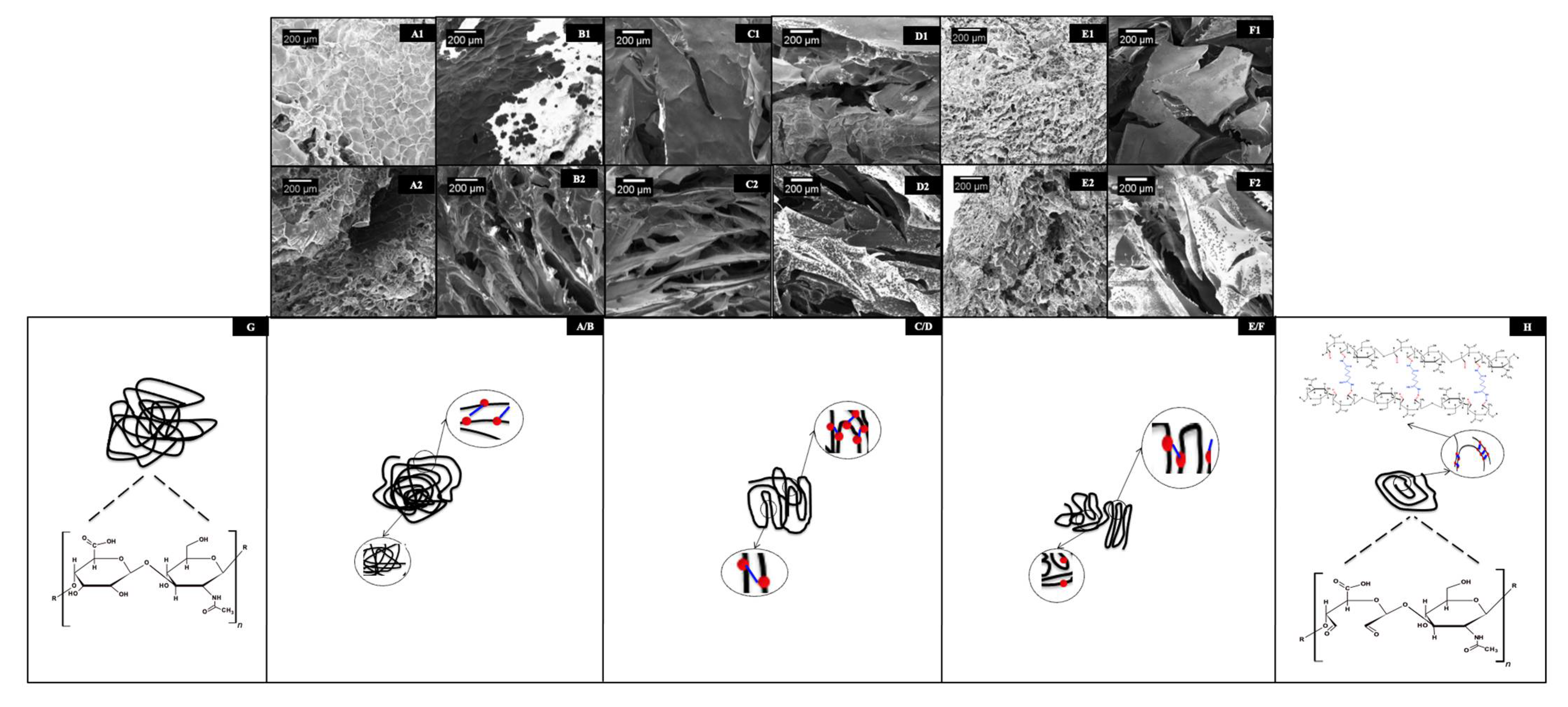
5.2. Structural, Physicochemical, and Mechanical Characterizations of oxi-HA/ADH
5.2.1. Click Reactions
5.2.2. Thermosensitivity
5.2.3. Thermogelling Mechanisms
5.2.4. Injectable Thermosensitive Hydrogels
6. Oxi-HA/ADH Hydrogels in Tissue Engineering and Regenerative Medicine
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Spicer, A.P.; Tien, J.Y. Hyaluronan and morphogenesis. Birth defects research. Embryo Today 2004, 72, 89–108. [Google Scholar]
- Meyer, K.; Palmer, J.W. The polysaccharide of vitreous humor. J. Biol. Chem. 1934, 107, 629–634. [Google Scholar] [CrossRef]
- Laurent, T.G. Glycoforun The Tree: Hyaluronan Research in the 20th Century. Available online: https://www.glycoforum.gr.jp/article/06A1.html (accessed on 20 May 2020).
- Balazs, E.A.; Leschiner, A.; Leschiner, A.; Band, P. Chemically modified hyaluronic acid preparation and method of recovery thereof from animal tissues. U.S. Patent No. 4,713,448, 15 December 1987. [Google Scholar]
- Berthiaume, F.; Maguire, T.J.; Yarmush, M.L. Tissue engineering and regenerative medicine: History, progress, and challenges. Annu. Rev. Chem. Biomol. Eng. 2011, 2, 403–443. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.Y.; Mooney, D.J. Hydrogels for tissue engineering. Chem. Rev. 2001, 101, 1869–1879. [Google Scholar] [CrossRef]
- Spiller, K.L.; Maher, S.A.; Lowman, A.M. Hydrogels for the repair of articular cartilage defects. Tissue Eng. Part B Rev. 2011, 17, 288–299. [Google Scholar] [CrossRef] [Green Version]
- Van Der Linden, H.J.; Herber, S.; Olthuis, W.; Bergveld, P. Stimulus-sensitive hydrogels and their applications in chemical (micro)analysis. Analyst 2003, 128, 325–331. [Google Scholar] [CrossRef]
- Jen, A.C.; Wake, M.C.; Mikos, A.G. Review: Hydrogels for cell immobilization. Biotechnol. Bioeng. 1996, 50, 357–364. [Google Scholar] [CrossRef]
- Wang, K.L.; Burban, J.H.; Cussler, E.L. Hydrogels as separation agents. Adv. Polym. Sci. 1993, 110, 67–79. [Google Scholar]
- Bennett, S.L.; Melanson, D.A.; Torchiana, D.F.; Wiseman, D.M.; Sawhney, A.S. Next-generation hydrogel films as tissue sealants and adhesion barriers. J. Card. Surg. 2003, 18, 494–499. [Google Scholar] [CrossRef] [PubMed]
- Radhakrishnan, J.; Subramanian, A.; Krishnan, U.M.; Sethuraman, S. Injectable and 3D bioprinted polysaccharide hydrogels: From cartilage to osteochondral tissue engineering. Biomacromolecules 2017, 18, 1–26. [Google Scholar] [CrossRef]
- Zhu, W.B.; Mow, V.C.; Rosenberg, L.C.; Tang, L.H. Determination of kinetic changes of aggrecan-hyaluronan interactions in solution from its rheological properties. J. Biomech. 1994, 27, 571–579. [Google Scholar] [CrossRef]
- Walimbe, T.; Panitch, A.; Sivasankar, P.M. A review of hyaluronic acid and hyaluronic acid-based hydrogels for vocal fold tissue engineering. J. Voice 2017, 31, 416–423. [Google Scholar] [CrossRef]
- Burdick, J.A.; Prestwich, G.D. Hyaluronic acid hydrogels for biomedical applications. Adv. Mater. 2011, 23, 41–56. [Google Scholar] [CrossRef]
- Ahadian, S.; Savoji, H.; Khademhosseini, A. Recent advances in hydrogels for tissue engineering. Chem. Eng. Prog. 2018, 114, 56–63. [Google Scholar]
- Hoare, T.R.; Kohane, D.S. Hydrogels in drug delivery: Progress and challenges. Polymer 2008, 49, 1993–2007. [Google Scholar] [CrossRef] [Green Version]
- Schanté, C.E.; Zuber, G.; Herlin, C.; Vandamme, T.F. Chemical modifications of hyaluronic acid for the synthesis of derivatives for a broad range of biomedical applications. Carbohydr. Polym. 2011, 85, 469–489. [Google Scholar] [CrossRef]
- Painter, T.; Larsen, B. Further illustration of nearest-neighbor autoinhibitory effects in oxidation of alginate by periodate ion. Acta Chem. Scand. 1973, 27, 1957–1962. [Google Scholar] [CrossRef]
- Jeanloz, R.W.; Forchielli, E. Studies on hyaluronic acid and related substances: 4-Periodate oxidation. J. Biol. Chem. 1951, 190, 537–546. [Google Scholar] [CrossRef]
- Kristiansen, K.A.; Dalheim, M.; Christensen, B.E. Periodate oxidation and macromolecular compaction of hyaluronan. Pure Appl. Chem. 2013, 85, 1893–1900. [Google Scholar] [CrossRef] [Green Version]
- Wong, S.S. Chemistry of Protein Conjugation and Cross-Linking; CRC Press: Boca Raton, FL, USA, 1991. [Google Scholar]
- Solomons, G.; Fryhle, C. Organic Chemistry, 7 ed.; John Wiley & Sons: Hoboken, NJ, USA, 1999; p. 1344. [Google Scholar]
- Su, W.Y.; Chen, Y.C.; Lin, F.H. Injectable oxidized hyaluronic acid/adipic acid dihydrazide hydrogel for nucleus pulposus regeneration. Acta Biomater. 2010, 6, 3044–3055. [Google Scholar] [CrossRef]
- Chen, Y.C.; Su, W.Y.; Yang, S.H.; Gefen, A.; Lin, F.H. In situ forming hydrogels composed of oxidized high molecular weight hyaluronic acid and gelatin for nucleus pulposus regeneration. Acta Biomater. 2013, 9, 5181–5193. [Google Scholar] [CrossRef] [PubMed]
- Collin, E.C.; Grad, S.; Zeugolis, D.I.; Vinatier, C.S.; Clouet, J.R.; Guicheux, J.J.; Weiss, P.; Alini, M.; Pandit, A.S. An injectable vehicle for nucleus pulposus cell-based therapy. Biomaterials 2011, 32, 2862–2870. [Google Scholar] [CrossRef]
- Khunmanee, S.; Jeong, Y.; Park, H. Crosslinking method of hyaluronic-based hydrogel for biomedical applications. J. Tissue Eng. 2017, 8. [Google Scholar] [CrossRef] [Green Version]
- França, C.G.; Sacomani, D.P.; Villalva, D.G.; Nascimento, V.F.; Dávila, J.L.; Santana, M.H.A. Structural changes and crosslinking modulated functional properties of oxi-HA/ADH hydrogels useful for regenerative purposes. Eur. Polym. J. 2019, 121, 109288. [Google Scholar] [CrossRef]
- Fallacara, A.; Baldini, E.; Manfredini, S.; Vertuani, S. Hyaluronic acid in the third millennium. Polymers 2018, 10, 701. [Google Scholar] [CrossRef] [Green Version]
- Buwalda, S.J.; Boere, K.W.M.; Dijkstra, P.J.; Feijen, J.; Vermonden, T.; Hennink, W.E. Hydrogels in a historical perspective: From simple networks to smart materials. J. Control. Release 2014, 190, 254–273. [Google Scholar] [CrossRef] [PubMed]
- Deng, Y.; Ren, J.; Chen, G.; Li, G.; Wu, X.; Wang, G.; Gu, G.; Li, J. Injectable in situ cross-linking chitosan-hyaluronic acid based hydrogels for abdominal tissue regeneration. Sci. Rep. 2017, 7, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Bulpitt, P.; Aeschlimann, D. New strategy for chemical modification of hyaluronic acid: Preparation of functionalized derivatives and their use in the formation of novel biocompatible hydrogels. J. Biomed. Mater. Res. 1999, 47, 152–169. [Google Scholar] [CrossRef]
- Kolb, H.C.; Finn, M.G.; Sharpless, K.B. Click chemistry: Diverse chemical function from a few good reactions. Angew. Chem. Int. 2001, 40, 2004–2021. [Google Scholar] [CrossRef]
- Crescenzi, V.; Cornelio, L.; Di Meo, C.; Nardecchia, S.; Lamanna, R. Novel hydrogels via click chemistry: Synthesis and potential biomedical applications. Biomacromolecules 2007, 8, 1844–1850. [Google Scholar] [CrossRef]
- Kim, J.; Kim, I.S.; Cho, T.H.; Lee, K.B.; Hwang, S.J.; Tae, G.; Noh, I.; Lee, S.H.; Park, Y.; Sun, K. Bone regeneration using hyaluronic acid-based hydrogel with bone morphogenic protein-2 and human mesenchymal stem cells. Biomaterials 2007, 28, 1830–1837. [Google Scholar] [CrossRef]
- Tan, H.P.; Chu, C.R.; Payne, K.A.; Marra, K.G. Injectable in situ forming biodegradable chitosan-hyaluronic-acid based hydrogels for cartilage tissue engineering. Biomaterials 2009, 30, 2499–2506. [Google Scholar] [CrossRef] [Green Version]
- Hu, M.H.; Yang, K.C.; Sun, Y.H.; Chen, Y.C.; Yang, S.H.; Lin, F.H. In situ forming oxidized hyaluronic acid/adipic acid dihidrazide hydrogel for prevention of epidural fibrosis after laminectomy. Eur. Cells Mater. 2017, 34, 307–320. [Google Scholar] [CrossRef] [PubMed]
- Schiraldi, C.; La Gatta, A.; De Rosa, M. Biotechnological production and application of hyaluronan. Biopolymers 2010, 20, 387–412. [Google Scholar]
- Trombino, S.; Servidio, C.; Curcio, F.; Cassano, R. Strategies for hyaluronic acid-based hydrogel design in drug delivery. Pharmaceutics 2019, 11, 407. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matsiko, A.; Levingstone, T.J.; O’Brien, F.J.; Gleeson, J.P. Addition of hyaluronic acid improves cellular infiltration and promotes early-stage chondrogenesis in a collagen-based scaffold for cartilage tissue engineering. J. Mech. Behav. Biomed. Mater. 2012, 11, 41–52. [Google Scholar] [CrossRef]
- Park, S.N.; Lee, H.J.; Lee, K.H.; Suh, H. Biological characterization of EDC-crosslinked collagen-hyaluronic acid matrix in dermal tissue restoration. Biomaterials 2003, 24, 1631–1641. [Google Scholar] [CrossRef]
- Vaca-González, J.J.; Clara-Trujillo, S.; Guillot-Ferriols, M.; Ródenas-Rochina, J.; Sanchis, M.J.; Ribelles, L.G.; Garzón-Alvarado, D.A.; Ferrer, G.G. Effect of electrical stimulation on chondrogenic differentiation of mesenchymal stem cells cultured in hyaluronic acid-Gelatin injectable hydrogels. Bioelectrochemistry 2020, 134, 107536. [Google Scholar] [CrossRef]
- Park, S.N.; Kim, J.K.; Suh, H. Evaluation of antibiotic-loaded collagen-hyaluronic acid matrix as a skin substitute. Biomaterials 2004, 25, 3689–3698. [Google Scholar] [CrossRef]
- Hou, K.T.; Liu, T.Y.; Chiang, M.Y.; Chen, C.Y.; Chang, S.J.; Chen, S.Y. Cartilage tissue-mimetic pellets with multifunctional magnetic hyaluronic acid-graft-amphiphilic gelatin microcapsules for chondrogenic stimulation. Polymers 2020, 12, 785. [Google Scholar] [CrossRef] [Green Version]
- Thi, P.L.; Son, J.Y.; Lee, Y.; Ryu, S.B.; Park, K.M.; Park, K.D. Enzymatically crosslinkable hyaluronic acid-gelatin hybrid hydrogels as potential bioinks for tissue regeneration. Macromol. Res. 2020, 28, 400–406. [Google Scholar] [CrossRef]
- Lu, K.Y.; Lin, Y.C.; Lu, H.T.; Ho, Y.C.; Weng, S.C.; Tsai, M.L.; Mi, F.L. A novel injectable in situ forming gel based on carboxymethyl hexanoyl chitosan/hyaluronic acid polymer blending for sustained release of berberine. Carbohydr. Polym. 2019, 206, 664–673. [Google Scholar] [CrossRef]
- Park, H.; Choi, B.; Hu, J.L.; Lee, M. Injectable chitosan hyaluronic acid hydrogels for cartilage tissue engineering. Acta Biomater. 2013, 9, 4779–4786. [Google Scholar] [CrossRef] [PubMed]
- Sheu, S.Y.; Chen, W.S.; Sun, J.S.; Lin, F.H.; Wu, T. Biological characterization of oxidized hyaluronic acid/resveratrol hydrogel for cartilage tissue engineering. J. Biomed. Mater. Res. Part A 2013, 101, 3457–3466. [Google Scholar] [CrossRef]
- Li, H.R.; Qi, Z.P.; Zheng, S.; Chang, Y.X.; Kong, W.J.; Fu, C.; Yu, Z.Y.; Yang, X.Y.; Pan, S. The application of hyaluronic acid-based hydrogel in bone and cartilage tissue engineering. Adv. Mater. Sci. Eng. 2019, 2019, 3027303. [Google Scholar] [CrossRef] [Green Version]
- Eslami, M.; Vrana, N.E.; Zorlutuna, P.; Sant, S.; Jung, S.; Masoumi, N.; Khavari-Nejad, R.A.; Javadi, G.; Khademhosseini, A. Fiber-reinforced hydrogel scaffolds for heart valve tissue engineering. J. Biomater. Appl. 2014, 29, 399–410. [Google Scholar] [CrossRef] [PubMed]
- Dahlmann, J.; Krause, A.; Möller, L.; Kensah, G.; Möwes, M.; Diekmann, A.; Martin, U.; Kirschning, A.; Gruh, I.; Dräger, G. Fully defined in situ cross-linkable alginate and hyaluronic acid hydrogels for myocardial tissue engineering. Biomaterials 2013, 34, 940–951. [Google Scholar] [CrossRef] [PubMed]
- Young, J.L.; Tuler, J.; Braden, R.; Schup-Magoffin, P.; Schaefer, J.; Kretchmer, K.; Christman, K.L.; Engler, A.J. In vivo response to dynamic hyaluronic acid hydrogels. Acta Biomater. 2013, 9, 7151–7157. [Google Scholar] [CrossRef] [Green Version]
- Asim, M.H.; Silberhumer, S.; Shahzadi, I.; Jalil, A.; Matuszczak, B.; Bernkop-Schnurch, A. S-protected thiolated hyaluronic acid: In situ crosslinking hydrogels for 3D cell culture scaffold. Carbohydr. Polym. 2020, 237, 116092. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.X.; Li, W.Y.; Yang, L.; Tang, S.; Hu, Q.L.; Wang, Y.X. Construction of biomimetic cross-linking polyplexes with thiolated-HA shielding. Chem. J. Chin. Univ. Chin. 2012, 33, 404–408. [Google Scholar]
- Surini, S.; Akiyama, H.; Morishita, M.; Takayama, K.; Nagai, T. Polyion complex of chitosan and sodium hyaluronate as an implant device for insulin delivery. STP Pharma Sci. 2003, 13, 265–268. [Google Scholar]
- Weng, L.; Ivanova, N.D.; Zakhaleva, J.; Chen, W.L. In vitro and in vivo suppression of cellular activity by guanidinoethyl disulfide released from hydrogel microspheres composed of partially oxidized hyaluronan and gelatin. Biomaterials 2008, 29, 4149–4156. [Google Scholar] [CrossRef] [Green Version]
- Radhakumary, C.; Nandkumar, A.M.; Nair, P.D. Hyaluronic acid-g-poly(HEMA) copolymer with potential implications for lung tissue engineering. Carbohydr. Polym. 2011, 85, 439–445. [Google Scholar] [CrossRef]
- Bicudo, R.C.S.; Santana, M.H.A. Production of hyaluronic acid (HA) nanoparticles by a continuous process inside microchannels: Effects of nonsolvents, organic phase flow rate, and HA concentration. Chem. Eng. Sci. 2012, 84, 134–141. [Google Scholar] [CrossRef]
- Schramm, C.; Spitzer, M.S.; Henke-Fahle, S.; Steinmetz, G.; Januschowski, K.; Heiduschka, P.; Geis-Gerstorfer, J.; Biedermann, T.; Bartz-Schmidt, K.U.; Szurman, P. The crosslinked biopolymer hyaluronic acid as an artificial vitreous substitute. Investig. Ophthalmol. Vis. Sci. 2012, 53, 613–621. [Google Scholar] [CrossRef] [PubMed]
- Shimojo, A.A.M.; Pires, A.M.B.; Lichy, R.; Santana, M.H.A. The performance of crosslinking with divinyl sulfone as controlled by the interplay between the chemical modification and conformation of hyaluronic acid. J. Braz. Chem. Soc. 2015, 26, 506–512. [Google Scholar] [CrossRef]
- Borzacchiello, A.; Russo, L.; Malle, B.M.; Schwach-Abdellaoui, K.; Ambrosio, L. Hyaluronic-acid based hydrogels for regenerative medicine applications. BioMed Res. Int. 2015, 2015, 871218. [Google Scholar] [CrossRef]
- Shimojo, A.A.M.; Pires, A.M.B.; Lichy, R.; Rodrigues, A.A.; Santana, M.H.A. The crosslinking degree controls the mechanical, rheological, and swelling properties of hyaluronic acid microparticles. J. Biom. Mater. Res. Part A 2015, 103, 730–737. [Google Scholar] [CrossRef]
- Lee, D.Y.; Cheon, C.; Son, S.; Kim, Y.Z.; Kim, J.T.; Jang, J.W.; Kim, S.S. Influence of molecular weight on swelling and elastic modulus of hyaluronic acid dermal fillers. Polym. Korea 2015, 39, 976–980. [Google Scholar] [CrossRef]
- Xue, Y.; Chen, H.Y.; Xu, C.; Yu, D.H.; Xu, H.J.; Hu, Y. Synthesis of hyaluronic acid hydrogels by crosslinking the mixture of high-molecular-weight hyaluronic acid and low-molecular-weight hyaluronic acid with 1,4-butanediol diglycidyl ether. RSC Adv. 2020, 10, 7206–7213. [Google Scholar] [CrossRef]
- de Melo, B.A.G.; Franca, C.G.; Davila, J.L.; Batista, N.A.; Caliari-Oliveira, C.; d’Avila, M.A.; Luzo, A.C.M.; Lana, J.; Santana, M.H.A. Hyaluronic acid and fibrin from L-PRP form semi-IPNs with tunable properties suitable for use in regenerative medicine. Mater. Sci. Eng. C Mater. Biol. Appl. 2020, 109, 110547. [Google Scholar] [CrossRef]
- De Angelis, B.; D’Autilio, M.; Orlandi, F.; Pepe, G.; Garcovich, S.; Scioli, M.G.; Orlandi, A.; Cervelli, V.; Gentile, P. Wound healing: In vitro and in vivo evaluation of a biofunctionalized scaffold based on hyaluronic acid and platelet-rich plasma in Chronic Ulcers. J. Clin. Med. 2019, 8, 1486. [Google Scholar] [CrossRef] [Green Version]
- Gilat, R.; Haunschild, E.D.; Knapik, D.M.; Evuarherhe, A., Jr.; Parvaresh, K.C.; Cole, B.J. Hyaluronic acid and platelet-rich plasma for the management of knee osteoarthritis. Int. Orthop. 2021, 45, 345–354. [Google Scholar] [CrossRef]
- Yun, Y.H.; Goetz, D.J.; Yellen, P.; Chen, W.L. Hyaluronan microspheres for sustained gene delivery and site-specific targeting. Biomaterials 2004, 25, 147–157. [Google Scholar] [CrossRef]
- Prestwich, G.D.; Marecak, D.M.; Marecek, J.F.; Vercruysse, K.P.; Ziebell, M.R. Controlled chemical modification of hyaluronic acid: Synthesis, applications, and biodegradation of hydrazide derivatives. J. Control. Release 1998, 53, 93–103. [Google Scholar] [CrossRef]
- Pouyani, T.; Harbison, G.S.; Prestwich, G.D. Novel hydrogels of hyaluronic acid synthesis, surface-morphology and solid-state NMR. J. Am. Chem. Soc. 1994, 116, 7515–7522. [Google Scholar] [CrossRef]
- Wang, W. A novel hydrogel crosslinked hyaluronan with glycol chitosan. J. Mater. Sci. Mater. Med. 2006, 17, 1259–1265. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Xiao, Y.M.; Jiang, B.; Fan, H.S.; Zhang, X.D. Effect of adipic dihydrazide modification on the performance of collagen/hyaluronic acid scaffold. J. Biomed. Mater. Res. Part B Appl. Biomater. 2010, 92, 307–316. [Google Scholar] [CrossRef] [PubMed]
- Jia, X.Q.; Yeo, Y.; Clifton, R.J.; Jiao, T.; Kohane, D.S.; Kobler, J.B.; Zeitels, S.M.; Langer, R. Hyaluronic acid-based microgels and microgel networks for vocal fold regeneration. Biomacromolecules 2006, 7, 3336–3344. [Google Scholar] [CrossRef] [PubMed]
- Hemshekhar, M.; Thushara, R.M.; Chandranayaka, S.; Sherman, L.S.; Kemparaju, K.; Girish, K.S. Emerging roles of hyaluronic acid bioscaffolds in tissue engineering and regenerative medicine. Int. J. Biol. Macromol. 2016, 86, 917–928. [Google Scholar] [CrossRef]
- Pereira, I.; Simoes, J.; Evtyugin, D.V.; Rouif, S.; Coimbra, M.A.; Domingues, M.R.M.; Gama, M. Effects of gamma irradiation and periodate oxidation on the structure of dextrin assessed by mass spectrometry. Eur. Polym. J. 2018, 103, 158–169. [Google Scholar] [CrossRef] [Green Version]
- Takei, T.; Sato, M.; Ijima, H.; Kawakami, K. In situ gellable oxidized citrus pectin for localized delivery of anticancer drugs and prevention of homotypic cancer cell aggregation. Biomacromolecules 2010, 11, 3525–3530. [Google Scholar] [CrossRef] [PubMed]
- Ragothaman, M.; Palanisamy, T.; Kalirajan, C. Collagen-poly(dialdehyde) guar gum based porous 3D scaffolds immobilized with growth factor for tissue engineering applications. Carbohydr. Polym. 2014, 114, 399–406. [Google Scholar] [CrossRef]
- Su, W.Y.; Chen, K.H.; Chen, Y.C.; Lee, Y.H.; Tseng, C.L.; Lin, F.H. An injectable oxidated hyaluronic acid/adipic acid dihydrazide hydrogel as a vitreous substitute. J. Biomater. Sci. Polym. 2011, 22, 1777–1797. [Google Scholar] [CrossRef]
- Gomez, C.G.; Rinaudo, M.; Villar, M.A. Oxidation of sodium alginate and characterization of the oxidized derivatives. Carbohydr. Polym. 2007, 67, 296–304. [Google Scholar] [CrossRef]
- Jia, X.Q.; Colombo, G.; Padera, R.; Langer, R.; Kohane, D.S. Prolongation of sciatic nerve blockade by in situ crosslinked hyaluronic acid. Biomaterials 2004, 25, 4797–4804. [Google Scholar] [CrossRef]
- Agerup, B.; Wik, O. Nasha TM, The Monograph: 2008, 28, Q-Med AB, Uppsala, Sweden. Available online: https://docplayer.net/20739410-Nasha-the-monograph-1.html. (accessed on 3 April 2020).
- Scott, J.E. Glycoforum Secondary and Tertiary Structures of Hyaluronan in Aqueous Solution Some Biological Consequences (2020). Available online: https://www.glycoforum.gr.jp/article/02A1.html (accessed on 20 May 2020).
- Cai, Y.; López-Ruiz, E.; Wengel, J.; Creemers, L.B.; Howard, K.A. A hyaluronic acid-based hydrogel enabling CD44-mediated chondrocyte binding and gapmer oligonucleotide release for modulation of gene expression in osteoarthritis. J. Control. Release 2017, 253, 153–159. [Google Scholar] [CrossRef] [Green Version]
- Liu, C.; Liu, D.; Wang, Y.; Li, Y.; Li, T.; Zhou, Z.; Yang, Z.; Wang, J.; Zhang, Q. Glycol chitosan/oxidized hyaluronic acid hydrogels functionalized with cartilage extracellular matrix particles and incorporating BMSCs for cartilage repair. Artif. Cells Nanomed. Biotechnol. 2018, 46, 721–732. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, S.; Pei, M.; Wan, T.; Yang, H.; Gu, S.; Tao, Y.; Liu, X.; Zhou, Y.; Xu, W.; Xiao, P. Self-healing hyaluronic acid hydrogels based on dynamic Schiff base linkages as biomaterials. Carbohydr. Polym. 2020, 250, 116922. [Google Scholar] [CrossRef] [PubMed]
- Bao, Z.; Yu, A.; Shi, H.; Hu, Y.; Jin, B.; Lin, D.; Dai, M.; Lei, L.; Li, X.; Wang, Y. Glycol chitosan/oxidized hyaluronic acid hydrogel film for topical ocular delivery of dexamethasone and levofloxacin. Int. J. Biol. Macromol. 2021, 167, 659–666. [Google Scholar] [CrossRef]
- Lee, S.J.; Nah, H.; Heo, D.N.; Kim, K.H.; Seok, J.M.; Heo, M.; Moon, H.J.; Lee, D.; Lee, J.S.; An, S.Y. Induction of osteogenic differentiation in a rat calvarial bone defect model using an in situ forming graphene oxide incorporated glycol chitosan/oxidized hyaluronic acid injectable hydrogel. Carbon 2020, 168, 264–277. [Google Scholar] [CrossRef]
- Han, C.; Zhang, H.; Wu, Y.; He, X.; Chen, X. Dual-crosslinked hyaluronan hydrogels with rapid gelation and high injectability for stem cell protection. Sci. Rep. 2020, 10, 1–7. [Google Scholar]
- Kim, D.Y.; Park, H.; Kim, S.W.; Lee, J.W.; Lee, K.Y. Injectable hydrogels prepared from partially oxidized hyaluronate and glycol chitosan for chondrocyte encapsulation. Carbohydr. Polym. 2017, 157, 1281–1287. [Google Scholar] [CrossRef]
- Nair, S.; Remya, N.S.; Remya, S.; Nair, P.D. A biodegradable in situ injectable hydrogel based on chitosan and oxidized hyaluronic acid for tissue engineering applications. Carbohydr. Polym. 2011, 85, 838–844. [Google Scholar] [CrossRef]
- Sun, J.; Xiao, C.; Tan, H.; Hu, X. Covalently crosslinked hyaluronic acid-chitosan hydrogel containing dexamethasone as an injectable scaffold for soft tissue engineering. J. Appl. Polym. Sci. 2013, 129, 682–688. [Google Scholar] [CrossRef]
- Zhu, J.; Jiang, G.; Hong, W.; Zhang, Y.; Xu, B.; Song, G.; Liu, T.; Hong, C.; Ruan, L. Rapid gelation of oxidized hyaluronic acid and succinyl chitosan for integration with insulin-loaded micelles and epidermal growth factor on diabetic wound healing. Mater. Sci. Eng. 2020, 117, 111273. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Sanz, E.; Ossipov, D.A.; Hilborn, J.; Larsson, S.; Jonsson, K.B.; Varghese, O.P. Bone reservoir: Injectable hyaluronic acid hydrogel for minimal invasive bone augmentation. J. Control. Release 2011, 152, 232–240. [Google Scholar] [CrossRef]
- Nimmo, C.M.; Owen, S.C.; Shoichet, M.S. Diels-Alder click crosslinked hyaluronic acid hydrogels for tissue engineering. Biomacromolecules 2011, 12, 824–830. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, Z.W.; Wei, X.C.; Gao, J.Z.; Zhao, Y.; Zhao, Y.M.; Guo, L.; Chen, C.W.; Duan, Z.Q.; Li, P.C.; Wei, L. Intra-articular injection of cross-linked hyaluronic acid-Dexamethasone hydrogel attenuates osteoarthritis: An experimental study in a rat model of osteoarthritis. Int. J. Mol. Sci. 2016, 17, 411. [Google Scholar] [CrossRef]
- Fu, S.L.; Dong, H.; Deng, X.Y.; Zhuo, R.X.; Zhong, Z.L. Injectable hyaluronic acid/poly(ethylene glycol) hydrogels crosslinked via strain-promoted azide-alkyne cycloaddition click reaction. Carbohydr. Polym. 2017, 169, 332–340. [Google Scholar] [CrossRef] [PubMed]
- Wei, Y.; Chang, Y.H.; Liu, C.J.; Chung, R.J. Integrated oxidized-hyaluronic acid/collagen hydrogel with β-TCP using proanthocyanidins as a crosslinker for drug delivery. Pharmaceutics 2018, 10, 37. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boehler, R.M.; Graham, J.G.; Shea, L.D. Tissue engineering tools for modulation of the immune response. Biotechniques 2011, 51, 239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- França, C.G.; Plaza, T.; Naveas, N.; Santana, M.H.A.; Manso-Silván, M.; Recio, G.; Hernandez-Montelongo, J. Nanoporous silicon microparticles embedded into oxidized hyaluronic acid/adipic acid dihydrazide hydrogel for enhanced controlled drug delivery. Microporous Mesoporous Mater. 2021, 310, 110634. [Google Scholar] [CrossRef]
- Ossipov, D.A.; Piskounova, S.; Varghese, O.P.; Hilborn, J. Functionalization of hyaluronic acid with chemoselective groups via a disulfide-based protection strategy for in situ formation of mechanically stable hydrogels. Biomacromolecules 2010, 11, 2247–2254. [Google Scholar] [CrossRef]
- Liu, H.N.; Guo, N.N.; Wang, T.T.; Guo, W.W.; Lin, M.T.; Huang-Fu, M.Y.; Vakili, M.R.; Xu, W.H.; Chen, J.J.; Wei, Q.C. Mitochondrial Targeted Doxorubicin-Triphenylphosphonium Delivered by Hyaluronic Acid Modified and pH Responsive Nanocarriers to Breast Tumor: In Vitro and in Vivo Studies. Mol. Pharm. 2018, 15, 882–891. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.; Chen, J.; Deng, C.; Suuronen, E.J.; Zhong, Z. Click hydrogels, microgels and nanogels: Emerging platforms for drug delivery and tissue engineering. Biomaterials 2014, 35, 4969–4985. [Google Scholar] [CrossRef] [PubMed]
- Deforest, C.A.; Polizzotti, B.D.; Anseth, K.S. Sequential click reactions for synthesizing and patterning three-dimensional cell microenvironments. Nat. Mater. 2009, 8, 659–664. [Google Scholar] [CrossRef] [Green Version]
- van Dijk, M.; Rijkers, D.T.S.; Liskamp, R.M.J.; van Nostrum, C.F.; Hennink, W.E. Synthesis and applications of biomedical and pharmaceutical polymers via click chemistry methodologies. Bioconjugate Chem. 2009, 20, 2001–2016. [Google Scholar] [CrossRef]
- Heller, D.A.; Levi, Y.; Pelet, J.M.; Doloff, J.C.; Wallas, J.; Pratt, G.W.; Jiang, S.; Sahay, G.; Schroeder, A.; Schroeder, J.E. Modular ‘click-in-emulsion’ bone-targeted nanogels. Adv. Mater. 2013, 25, 1449–1454. [Google Scholar] [CrossRef] [Green Version]
- Bajpai, A.K.; Shukla, S.K.; Bhanu, S.; Kankane, S. Responsive polymers in controlled drug delivery. Prog. Polym. Sci. 2008, 33, 1088–1118. [Google Scholar] [CrossRef]
- Jeong, B.; Kim, S.W.; Bae, Y.H. Thermosensitive sol-gel reversible hydrogels. Adv. Drug Deliv. Rev. 2012, 64, 154–162. [Google Scholar] [CrossRef]
- Peppas, N.A.; Bures, P.; Leobandung, W.; Ichikawa, H. Hydrogels in pharmaceutical formulations. Eur. J. Pharm. Biopharm. 2000, 50, 27–46. [Google Scholar] [CrossRef]
- Gil, E.S.; Hudson, S.M. Stimuli-reponsive polymers and their bioconjugates. Prog. Polym. Sci. 2004, 29, 1173–1222. [Google Scholar] [CrossRef]
- Niu, G.; Du, F.; Song, L.; Zhang, H.; Yang, J.; Cao, H.; Zheng, Y.; Yang, Z.; Wang, G.; Yang, H. Synthesis and characterization of reactive poloxamer 407 for biomedical applications. J. Control. Release 2009, 138, 49–56. [Google Scholar] [CrossRef]
- Chenite, A.; Chaput, C.; Wang, D.; Combes, C.; Buschmann, M.D.; Hoemann, C.D.; Leroux, J.C.; Atkinson, B.L.; Binette, F.; Selmani, A. Novel injectable neutral solutions of chitosan form biodegradable gels in situ. Biomaterials 2000, 21, 2155–2161. [Google Scholar] [CrossRef]
- Ruel-Gariepy, E.; Leclair, G.; Hildgen, P.; Gupta, A.; Leroux, J. Thermosensitive chitosan-based hydrogel containing liposomes for the delivery of hydrophilic molecules. J. Control. Release 2002, 82, 373–383. [Google Scholar] [CrossRef]
- Mishra, D.; Bhunia, B.; Banerjee, I.; Datta, P.; Dhara, S.; Maiti, T.K. Enzymatically crosslinked carboxymethyl-chitosan/gelatin/nanohydroxyapatite injectable gels for in situ bone tissue engineering application. Mater. Sci. Eng. C 2011, 31, 1295–1304. [Google Scholar] [CrossRef]
- Lee, S.C.; Cho, Y.W.; Park, K. Control of thermogelation properties of hydrophobically modified methylcellulose. J. Bioact. Compat. Polym. 2005, 20, 5–13. [Google Scholar] [CrossRef]
- Kondiah, P.J.; Choonara, Y.E.; Kondiah, P.P.D.; Marimuthu, T.; Kumar, P.; Du, T.; Lisa, C.; Pillay, V. A review of injectable polymeric hydrogel systems for application in bone tissue engineering. Molecules 2016, 21, 1580. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, H.; Qi, X.; Chen, Y.; Wu, Z. Thermosensitive hydrogels for delivering biotherapeutic molecules: A review. Saudi Pharm. J. 2019, 27, 990–999. [Google Scholar] [CrossRef]
- Ohya, S.; Nakayama, Y.; Matsuda, T. Thermoresponsive artificial extracellular matrix for tissue engineering: Hyaluronic acid bioconjugated with poly(N-isopropylacrylamide) grafts. Biomacromolecules 2001, 2, 856–863. [Google Scholar] [CrossRef] [PubMed]
- Mayol, L.; Quaglia, F.; Borzacchiello, A.; Ambrosio, L.; Rotonda, M.I.L. A novel poloxamers/hyaluronic acid in situ forming hydrogel for drug delivery: Rheological, mucoadhesive and in vitro release properties. Eur. J. Pharm. Biopharm. 2008, 70, 199–206. [Google Scholar] [CrossRef]
- Babo, P.S.; Santo, V.E.; Gomes, M.E.; Reis, R.L. Development of an injectable calcium phosphate/hyaluronic acid microparticles system for platelet lysate sustained delivery aiming bone regeneration. Macromol. Biosci. 2016, 16, 1662–1677. [Google Scholar] [CrossRef]
- Hou, Q.; De Bank, P.A.; Shakesheff, K.M. Injectable scaffolds for tissue regeneration. J. Mater. Chem. 2004, 14, 1915–1923. [Google Scholar] [CrossRef]
- Nuttelman, C.R.; Rice, M.A.; Rydholm, A.E.; Salinas, C.N.; Shah, D.N.; Anseth, K.S. Macromolecular monomers for the synthesis of hydrogel niches and their application in cell encapsulation and tissue engineering. Prog. Polym. Sci. 2008, 33, 167–179. [Google Scholar] [CrossRef] [Green Version]
- Klouda, L. Thermoresponsive hydrogels in biomedical applications a seven-year update. Eur. J. Pharm. Biopharm. 2015, 97, 338–349. [Google Scholar] [CrossRef]
- Vashi, A.V.; Keramidaris, E.; Abberton, K.M.; Morrison, W.A.; Wilson, J.L.; O’Connor, A.J.; Cooper-White, J.J.; Thompson, E.W. Adipose differentiation of bone marrow-derived mesenchymal stem cells using Pluronic F-127 hydrogel in vitro. Biomaterials 2008, 29, 573–579. [Google Scholar] [CrossRef] [PubMed]
- Klouda, L.; Mikos, A.G. Thermoresponsive hydrogels in biomedical applications. Eur. J. Pharm. Biopharm. 2008, 68, 34–45. [Google Scholar] [CrossRef] [Green Version]
- Southall, N.T.; Dill, K.A.; Haymet, A.D.J. A view of the hydrophobic effect. J. Phys. Chem. B 2002, 106, 521–533. [Google Scholar] [CrossRef]
- Hoffman, A.S. “Intelligent” Polymers in medicine and biotechnology. Macromol. Symp. 1995, 98, 645–664. [Google Scholar] [CrossRef]
- Ruel-Gariépy, E.; Leroux, J.C. In situ-forming hydrogels-review of temperature-sensitive systems. Eur. J. Pharm. Biopharm. 2004, 58, 409–426. [Google Scholar] [CrossRef]
- De las Heras Alarcón, C.; Pennadam, S.; Alexander, C. Stimuli responsive polymers for biomedical applications. Chem. Soc. Rev. 2005, 34, 276–285. [Google Scholar] [CrossRef]
- Tekin, H.; Sanchez, J.G.; Tsinman, T.; Langer, R.; Khademhosseini, A. Thermoresponsive platforms for tissue engineering and regenerative medicine. AIChE J. 2011, 57, 3249–3258. [Google Scholar] [CrossRef]
- Lee, J.H. Injectable hydrogels delivering therapeutic agents for disease treatment and tissue engineering. Biomater. Res. 2018, 22, 1–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mellati, A.; Akhtari, J. Injectable hydrogels: A review of injectability mechanisms and biomedical applications. Res. Mol. Med. 2018, 6, 1–20. [Google Scholar] [CrossRef]
- Gupta, K.C.; Jabrail, F.H. Glutaraldehyde and glyoxal cross-linked chitosan microspheres for controlled delivery of centchroman. Carbohydr. Res. 2006, 341, 744–756. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Liu, Z. A pH-responsive hydrogel based on a tumor-targeting mesoporous silica nanocomposite for sustained cancer labeling and therapy. Macromol. Rapid Commun. 2016, 37, 1533–1539. [Google Scholar] [CrossRef]
- Baumann, M.D.; Kang, C.E.; Stanwick, J.C.; Wang, Y.; Kim, H.; Lapitsky, Y.; Shoichet, M.S. An injectable drug delivery platform for sustained combination therapy. J. Control. Release 2009, 138, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Davoodi, P.; Ng, W.C.; Yan, W.C.; Srinivasan, M.P.; Wang, C.H. Double-walled microparticles-embedded self-cross-linked, injectable, and antibacterial hydrogel for controlled and sustained release of chemotherapeutic agents. ACS Appl. Mater. Interfaces 2016, 8, 22785–22800. [Google Scholar] [CrossRef]
- Allemann, I.B.; Baumann, L. Hyaluronic acid gel (JuvédermTM) preparations in the treatment of facial wrinkles and folds. Clin. Interv. Ag. 2008, 3, 629–634. [Google Scholar]
- Falcone, S.J.; Berg, R.A. Crosslinked hyaluronic acid dermal fillers: A comparison of rheological properties. J. Biomed. Mater. Res. Part A 2008, 87, 264–271. [Google Scholar] [CrossRef] [PubMed]
- Liang, H.; Kuang, T.; Lai, X.S.; Wei, M.F.; Lu, S.H.; Wen, W.F.; Kuo, S.H.; Chen, C.M.; Tseng, W.; Yih, I. Intratumoral injection of thermogelling and sustained-release carboplatin-loaded hydrogel simplifies the administration and remains the synergistic effect with radiotherapy for mice gliomas. Biomaterials 2018, 151, 38–52. [Google Scholar] [CrossRef]
- Kim, S.W.; Kim, D.Y.; Roh, H.H.; Kim, H.S.; Lee, J.W.; Lee, K.Y. Three-dimensional bioprinting of cell-laden constructs using polysaccharide-based self-healing hydrogels. Biomacromolecules 2019, 20, 1860–1866. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; Xu, T.; Chen, W.; Wang, R.; Xu, Z.; Ye, Z.; Chi, B. Improvement of toughness for the hyaluronic acid and adipic acid dihydrazide hydrogel by PEG. Fibers Polym. 2017, 18, 817–824. [Google Scholar] [CrossRef]
- Sargazi, A.; Kamali, N.; Shiri, F.; Heidari, M. Hyaluronic acid/polyethylene glycol nanoparticles for controlled delivery of mitoxantrone. Artif. Cells Nanomed. Biotechnol. 2018, 46, 500–509. [Google Scholar] [CrossRef]
- Pörtner, R.; Nagel-Heyer, S.; Goepfert, C.; Adamietz, P.; Meenen, N.M. Bioreactor design for tissue engineering. J. Biosci. Bioeng. 2005, 100, 235–245. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hsiao, M.Y.; Lin, A.-C.; Liao, W.-H.; Wang, T.-G.; Hsu, C.-H.; Chen, W.-S.; Lin, F.-H. Drug-loaded hyaluronic acid hydrogel as a sustained-release regimen with dual effects in early intervention of tendinopathy. Sci. Rep. 2019, 9, 1–9. [Google Scholar] [CrossRef]
- Hsiao, M.Y.; Lin, P.C.; Lin, A.C.; Wu, Y.W.; Chen, W.S.; Lin, F.H. Oxidized hyaluronic acid/adipic acid dihidrazide hydrogel as drug-carrier for cytoprotective medications-preliminary results. Biomed. Eng. Appl. Basis Commun. 2019, 31, 1–7. [Google Scholar] [CrossRef]
- Liang, Y.; Wang, Y.; Wang, L.; Liang, Z.; Li, D.; Xu, X.; Chen, Y.; Yang, X.; Zhang, H.; Niu, H. Self-crosslinkable chitosan-hyaluronic acid dialdehyde nanoparticles for CD44-targeted siRNA delivery to treat bladder cancer. Bioact. Mater. 2021, 6, 433–446. [Google Scholar] [CrossRef] [PubMed]
- Emoto, S.; Yamaguchi, H.; Kamei, T.; Ishigami, H.; Suhara, T.; Suzuki, Y.; Ito, T.; Kitayama, J.; Watanabe, T. Intraperitoneal administration of cisplatin via an in situ cross-linkable hyaluronic acid-based hydrogel for peritoneal dissemination of gastric cancer. Surg. Today 2014, 44, 919–926. [Google Scholar] [CrossRef]
- Liao, C.H.; Chen, C.S.; Chen, Y.C.; Jiang, N.E.; Farn, C.J.; Shen, Y.S.; Hsu, M.L.; Chang, C.H. Vancomycin-loaded oxidized hyaluronic acid and adipic acid dihydrazide hydrogel: Biocompatibility, drug release, antimicrobial activity, and biofilm model. J. Microbiol. Immunol. Infect. 2020, 53, 525–531. [Google Scholar] [CrossRef] [PubMed]
- Weis, M.; Shan, J.; Kuhlmann, M.; Jungst, T.; Tessmar, J.; Groll, J. Evaluation of hydrogels based on oxidized hyaluronic acid for bioprinting. Gels 2018, 4, 82. [Google Scholar] [CrossRef] [Green Version]





| Biomaterial | Application | Reference |
|---|---|---|
| HA 1-collagen matrix | cartilage tissue repair and neural regeneration | [40,41] |
| HA-gelatin hydrogels | bone regeneration and chondrogenic differentiation | [42,43,44,45] |
| HA-CHI 2 composite | cartilage TE | [36,46,47] |
| oxi-HA-resveratrol hydrogel | cell carrier for chondrocytes | [48,49] |
| PGS-PCL-Me-HA | heart valve TE | [50] |
| Alginate-HA | myocardial TE | [51] |
| thiolated-HA hydrogels | Adipose-substitutes TE | [52,53,54] |
| collagen-PEG-grafted-HA | intradermal drug delivery | [55] |
| oxi-HA-gelatin microspheres | drug delivery | [56] |
| HA-g-poly-(HEMA) | lung TE | [57] |
| HA-ADH 3-EDCI 4 | drug delivery | [58,59] |
| HA-DVS 5 | viscosupplement | [60,61] |
| HA-BDDE 6 | viscosupplement | [62,63,64] |
| HA-PRP 7 | regenerative medicine | [65,66,67] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
França, C.G.; Villalva, D.G.; Santana, M.H.A. Oxi-HA/ADH Hydrogels: A Novel Approach in Tissue Engineering and Regenerative Medicine. Polysaccharides 2021, 2, 477-496. https://doi.org/10.3390/polysaccharides2020029
França CG, Villalva DG, Santana MHA. Oxi-HA/ADH Hydrogels: A Novel Approach in Tissue Engineering and Regenerative Medicine. Polysaccharides. 2021; 2(2):477-496. https://doi.org/10.3390/polysaccharides2020029
Chicago/Turabian StyleFrança, Carla Giometti, Denise Gradella Villalva, and Maria Helena Andrade Santana. 2021. "Oxi-HA/ADH Hydrogels: A Novel Approach in Tissue Engineering and Regenerative Medicine" Polysaccharides 2, no. 2: 477-496. https://doi.org/10.3390/polysaccharides2020029
APA StyleFrança, C. G., Villalva, D. G., & Santana, M. H. A. (2021). Oxi-HA/ADH Hydrogels: A Novel Approach in Tissue Engineering and Regenerative Medicine. Polysaccharides, 2(2), 477-496. https://doi.org/10.3390/polysaccharides2020029







