Lifestyle Interventions for the Treatment of Obesity in Workers: An Integrative Review
Abstract
1. Introduction
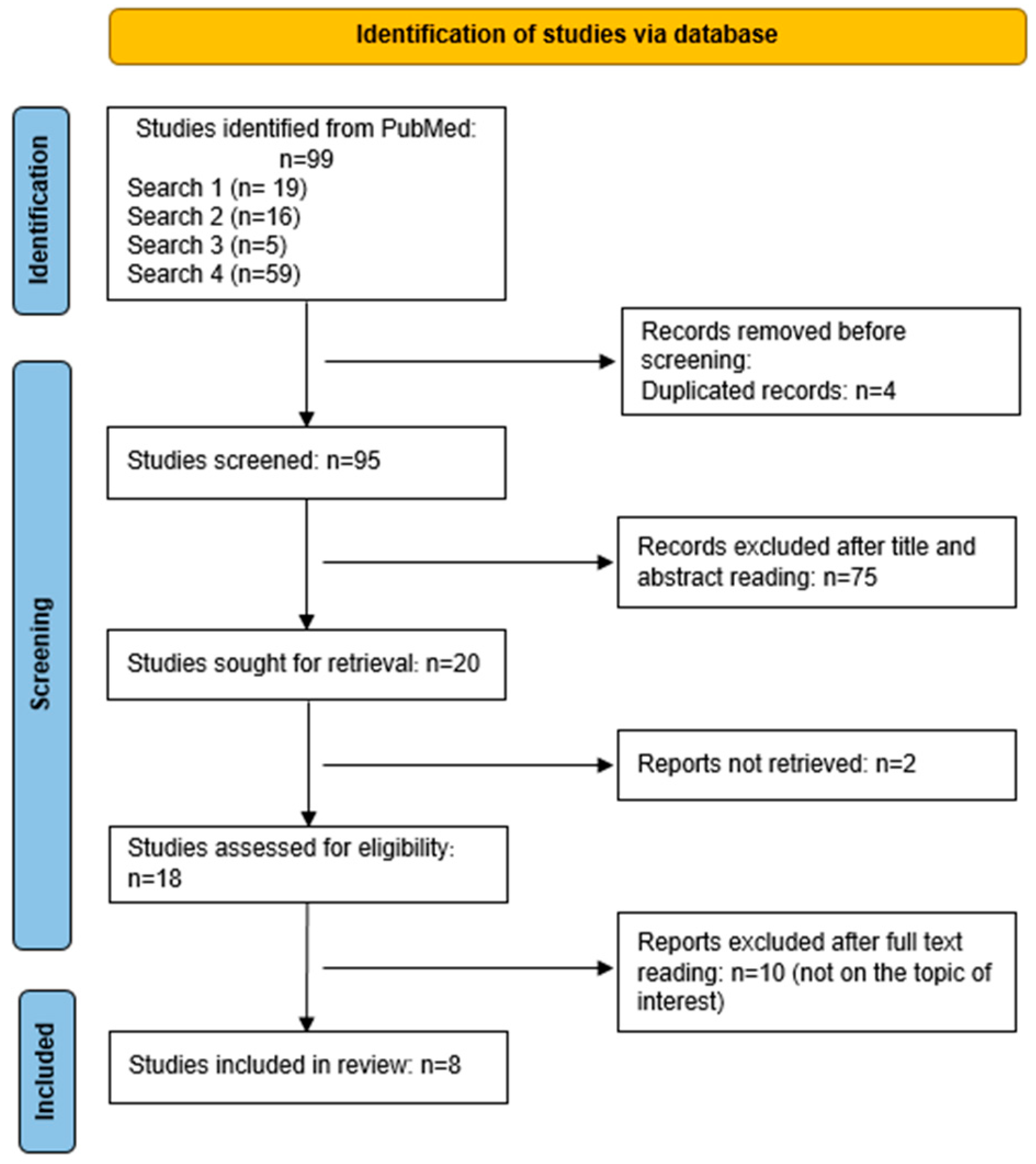
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria
2.3. Selection and Extraction Process
2.4. Methodological Quality Assessment
3. Results
| Reference | Population | Intervention | Comparison | Remarks |
|---|---|---|---|---|
| Viester et al. (2017) [16] | Construction workers in the Netherlands with overweight or obesity. EG (n = 162) CG (n = 152) | Single-blind randomized trial with workplace intervention conducted during working hours. D—Calorie guide, recipes, individual plan. PA—Pedometer and individualized exercise prescription. C—Stages of change; knowledge tests. | EG vs. CG (general health guidance) after 6 and 12 months. | The EG showed positive changes in vigorous physical activity and in the consumption of sugar-sweetened beverages compared with the CG, although the effects on body weight were modest. A significant reduction in BMI was observed after 6 months. |
| Olson et al. (2016) [11] | Transport company workers in the United States, BMI ≥ 27. EG (n = 247) CG (n = 225) | Randomized controlled trial with internet-based instructions. D (Diet): Guidance for reducing the consumption of high-calorie foods, reducing portion sizes, increasing fruit and vegetable intake, and an individualized meal plan. PA (Physical Activity): Pedometer, guidance to increase walking, and self-monitoring. C (Counseling/Behavioral): Motivational guidance, informational booklet, goal setting, prize-based competition, sleep recommendations, and follow-up with coaches. | EG vs. CG (general information and rewards for participation in assessments) after 6 months. | The EG showed significant reductions in BMI and body weight, in addition to increased fruit and vegetable consumption and a higher number of days per week of physical activity. |
| Atlantis et al. (2006) [18] | Casino workers in Australia, sedentary, with no BMI restriction. EG (n = 19) CG (n = 23) | Randomized controlled trial. D (Diet): Monthly individual consultations with a nutritionist, guidance on reducing fast food and sweets. PA (Physical Activity): Individualized prescription of moderate-to-high intensity aerobic exercises and resistance training, 3 times per week. C (Counseling/Behavioral): Health education, participation in seminars, individual counseling, and adherence-based rewards. | EG vs. CG (general information) after 24 weeks. | The EG showed a reduction in waist circumference and improvement in aerobic fitness compared with the CG; however, there was no statistically significant change in BMI. |
| Verweij et al. (2012) [17] | Workers from medium- and large-sized companies in the Netherlands with increased health risk (overweight or obesity, and/or elevated waist circumference, and/or sedentary lifestyle, and/or inadequate eating behavior). EG (n = 274) CG (n = 249) | Single-blind randomized controlled trial. D (Diet): Reduced price of healthy foods, strategies to promote healthy options in the cafeteria, guidance to reduce fast-food intake, encouragement to increase fruit consumption, and completion of a food diary. PA (Physical Activity): Installation of bicycle racks, promotion of physical activity, pedometer, and informational leaflets. C (Counseling/Behavioral): Guidance and sessions on behavior change, individual cognitive-behavioral therapy sessions. | EG vs. CG (general information) after 6 months. | After 6 months, the EG showed a significant reduction in workplace sedentary behavior and an increase in fruit consumption. However, no changes were observed in overall physical activity level, snack consumption, or BMI. |
| Wilson et al. (2014) [12] | Railway maintenance workers in the United States, with participation encouraged for those with BMI ≥ 27. EG (n = 227) CG (n = 135) | Randomized trial. D (Diet): Self-monitoring of food intake, consultation with a nutritionist, goal of reducing 7% of initial body weight, posters, and healthy menus. PA (Physical Activity): Self-monitoring of physical activity, recommendation of 150 min of physical activity per week. C (Counseling/Behavioral): Manual with simplified language, awareness of health behaviors, individual counseling, educational material for families, and a website with family support strategies. | EG vs. CG (general health information provided as part of the company’s usual operations) after 12 months. | The EG showed better weight and BMI outcomes compared to the CG, mainly because CG participants gained weight, while EG participants lost a small amount of weight (not reaching the target goal). Nevertheless, the EG developed strategies for weight control and engagement in physical activity. |
| Almeida et al. (2015) [13] | Workers from medium- and large-sized companies in the United States, with BMI ≥ 25. EG (n = 789) CG (n = 1001) | Randomized controlled trial, internet-based instructions. D (Diet): Low-fat, high-fiber diet with emphasis on fruits and vegetables, replacement of sugar-sweetened beverages with water, individualized meal plan. PA (Physical Activity): Guidance to perform 150 min per week, electronic coach. C (Counseling/Behavioral): Behavioral strategies via email, website support, financial incentives. | EG vs. CG (general information on healthy eating and physical activity) after 6 months. | Both groups showed a small reduction in BMI after 6 months. Participants also increased fruit and fiber intake and physical activity levels, while reducing saturated fat and cholesterol consumption. However, no statistically significant differences were observed between EG and CG. |
| LaCaille et al. (2016) [14] | Employees of a medium-sized healthcare system in the United States, with BMI ≥ 25. EG (n = 361) CG (n = 81) | Quasi-experimental study with a non-equivalent, non-randomized control group. Duration: 12 months. D (Diet): Food labeling with calorie information, number of steps required to burn them, and “traffic light” symbols based on energy density; changes in utensil size; increased availability of low-energy-density foods; reduced portion sizes of high-calorie foods; information on energy balance; health messages in the workplace. PA (Physical Activity): Pedometers to monitor steps, encourage walking, and promote self-monitoring. C (Counseling/Behavioral): Health-related behavior change strategies, “influential” employees trained to reinforce healthy messages, influence positive attitudes, and increase colleagues’ self-efficacy, financial incentives. | EG (hospital employees) vs. CG (clinic employees from the same administration, who received the same guidance and financial incentives but no pedometers), assessed at 6 and 12 months. | No statistically significant differences were observed between groups regarding BMI, body weight, or waist circumference over 12 months. The EG increased walking time compared with the CG, although overall physical activity levels were not altered. Moreover, fruit and vegetable consumption decreased, and fat intake remained unchanged. |
| Fernandez et al. (2015) [15] | Employees of a manufacturing, research, and development company in the United States, with BMI ≥ 25. EG (n = 1547) CG (n = 1068) | Randomized study with a qualitative phase (Phase 1) and a quantitative phase (Phase 2). D (Diet): Phase 1: exploration of the social and cultural role of food. Phase 2: actions to reduce energy intake and control portion sizes, sessions with nutritionists. PA (Physical Activity): Phase 1: exploration of the social and cultural role of physical activity. Phase 2: actions to increase energy expenditure, pedometers, and partnerships with gyms. C (Counseling/Behavioral): Actions to raise awareness and build capacities, workplace health promotion interventions, workshops, and financial incentives. | EG vs. CG (no intervention) after 2 years. | After 2 years of intervention, a favorable trend toward BMI reduction was observed among EG participants. Environmental changes implemented in the workplace increased employees’ exposure to an adequate energy balance. |
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ahirwar, R.; Mondal, P.R. Prevalence of obesity in India: A systematic review. Diabetes Metab. Syndr. Clin. Res. Rev. 2019, 13, 318–321. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Obesity and Overweight (1 March 2024). Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 24 July 2024).
- Beltrán-Carrillo, V.J.; Megías, Á.; González-Cutre, D.; Jiménez-Loaisa, A. Elements behind sedentary lifestyles and unhealthy eating habits in individuals with severe obesity. Int. J. Qual. Stud. Health Well-Being 2022, 17, 2056967. [Google Scholar] [CrossRef]
- Blüher, M. Obesity: Global epidemiology and pathogenesis. Nat. Rev. Endocrinol. 2019, 15, 288–298. [Google Scholar] [CrossRef] [PubMed]
- Atakan, M.M.; Koşar, Ş.N.; Güzel, Y.; Tin, H.T.; Yan, X. The role of exercise, diet, and cytokines in preventing obesity and improving adipose tissue. Nutrients 2021, 13, 1459. [Google Scholar] [CrossRef]
- Chopra, S.; Malhotra, A.; Ranjan, P.; Vikram, N.K.; Sarkar, S.; Siddhu, A.; Kumari, A.; Kaloiya, G.S.; Kumar, A. Predictors of successful weight loss outcomes amongst individuals with obesity undergoing lifestyle interventions: A systematic review. Obes. Rev. 2022, 22, e13148. [Google Scholar] [CrossRef] [PubMed]
- Cercato, C.; Fonseca, F.A. Cardiovascular risk and obesity. Diabetol. Metab. Syndr. 2019, 11, 74. [Google Scholar] [CrossRef]
- Goettler, A.; Grosse, A.; Sonntag, D. Productivity loss due to overweight and obesity: A systematic review of indirect costs. BMJ Open 2017, 7, e014632. [Google Scholar] [CrossRef]
- Trogdon, J.G.; Finkelstein, E.A.; Hylands, T.; Dellea, P.S.; Kamal-Bahl, S.J. Indirect costs of obesity: A review of the current literature. Obes. Rev. 2008, 9, 489–500. [Google Scholar] [CrossRef]
- Tawfik, G.M.; Dila, K.A.S.; Mohamed, M.Y.F.; Tam, D.N.H.; Kien, N.D.; Ahmed, A.M.; Huy, N.T. A step by step guide for conducting a systematic review and meta-analysis with simulation data. Trop. Med. Health 2019, 47, 46. [Google Scholar] [CrossRef]
- Olson, R.; Wipfli, B.; Thompson, S.V.; Elliot, D.L.; Anger, W.K.; Bodner, T.; Hammer, L.B.; Perrin, N.A. Weight control intervention for truck drivers: The SHIFT randomized controlled trial, United States. Am. J. Public Health 2016, 106, 1698–1706. [Google Scholar] [CrossRef]
- Wilson, M.G.; DeJoy, D.M.; Vandenberg, R.; Padilla, H.; Davis, M. FUEL your life: A translation of the diabetes prevention program to worksites. Am. J. Health Promot. 2016, 30, 188–197. [Google Scholar] [CrossRef] [PubMed]
- Almeida, F.A.; You, W.; Harden, S.M.; Blackman, K.C.; Davy, B.M.; Glasgow, R.E.; Hill, J.L.; Linnan, L.A.; Wall, S.S.; Yenerall, J.; et al. Effectiveness of a worksite—Based weight loss randomized controlled trial: The worksite study. Obesity 2015, 23, 737–745. [Google Scholar] [PubMed]
- LaCaille, L.J.; Schultz, J.F.; Goei, R.; LaCaille, R.A.; Dauner, K.N.; de Souza, R.; Nowak, A.V.; Regal, R. Go!: Results from a quasi-experimental obesity prevention trial with hospital employees. BMC Public Health 2016, 16, 171. [Google Scholar] [CrossRef]
- Fernandez, I.D.; Chin, N.P.; Devine, C.M.; Dozier, A.M.; Martina, C.A.; McIntosh, S.; Thevenet-Morrison, K.; Yang, H. Images of a healthy worksite: A group-randomized trial for worksite weight gain prevention with employee participation in intervention design. Am. J. Public Health 2015, 105, 2167–2174. [Google Scholar]
- Viester, L.; Verhagen, E.A.; Bongers, P.M.; van der Beek, A.J. Effectiveness of a worksite intervention for male construction workers on dietary and physical activity behaviors, body mass index, and health outcomes: Results of a randomized controlled trial. Am. J. Health Promot. 2018, 32, 795–805. [Google Scholar] [CrossRef] [PubMed]
- Verweij, L.M.; Proper, K.I.; Weel, A.N.; Hulshof, C.T.; van Mechelen, W. The application of an occupational health guideline reduces sedentary behaviour and increases fruit intake at work: Results from an RCT. Occup. Environ. Med. 2012, 69, 500–507. [Google Scholar] [CrossRef]
- Atlantis, E.; Chow, C.M.; Kirby, A.; Fiatarone Singh, M.A. Worksite intervention effects on physical health: A randomized controlled trial. Health Promot. Int. 2006, 21, 191–200. [Google Scholar] [CrossRef]
- Burgess, E.; Hassmén, P.; Pumpa, K.L. Determinants of adherence to lifestyle intervention in adults with obesity: A systematic review. Clin. Obes. 2017, 7, 123–135. [Google Scholar] [CrossRef]
- Moroshko, I.; Brennan, L.; O’Brien, P. Predictors of dropout in weight loss interventions: A systematic review of the literature. Obes. Rev. 2011, 6, 912–934. [Google Scholar] [CrossRef]
- Liberali, R.; Kupek, E.; Assis, M.A. Dietary patterns and childhood obesity risk: A systematic review. Child. Obes. 2020, 16, 70–85. [Google Scholar] [CrossRef]
- Wu, E.; Ni, J.; Zhou, W.; You, L.; Tao, L.; Xie, T. Consumption of fruits, vegetables, and legumes are associated with overweight/obesity in the middle-and old-aged Chongqing residents: A casecontrol study. Medicine 2022, 101, e29749. [Google Scholar] [CrossRef]
- Mazur, M.; Przytuła, A.; Szymańska, M.; Popiołek-Kalisz, J. Dietary Strategies for Cardiovascular Disease Risk Factors Prevention. Curr. Probl. Cardiol. 2024, 49, 102746. [Google Scholar] [CrossRef]
- Su, Y.; Sun, J.; Zhou, Y.; Sun, W. The Relationship of Waist Circumference with the Morbidity of Cardiovascular Diseases and All-Cause Mortality in Metabolically Healthy Individuals: A Population-Based Cohort Study. Rev. Cardiovasc. Med. 2024, 25, 212. [Google Scholar] [CrossRef]
- Alexander, L.; Christensen, S.M.; Richardson, L.; Ingersoll, A.B.; Burridge, K.; Golden, A.; Karjoo, S.; Cortez, D.; Shelver, M.; Bays, H.E. Nutrition and physical activity: An obesity medicine association (OMA) clinical practice statement 2022. Obes. Pillars 2022, 1, 100005. [Google Scholar] [CrossRef] [PubMed]
- Brusaca, L.A.; Gupta, N.; Hallman, D.M.; Holtermann, A.; Barbieri, D.F.; Oliveira, A.B. Does the intervention approach matter for improving 24-hour physical behaviours among overweight and obese Brazilian office workers? BMC Public Health 2025, 25, 2699. [Google Scholar] [CrossRef] [PubMed]
- Aldana, S.G.; Anderson, D.R.; Adams, T.B.; Whitmer, R.W.; Merrill, R.M.; George, V.; Noyce, J. A review of the knowledge base on healthy worksite culture. J. Occup. Environ. Med. 2012, 54, 414–419. [Google Scholar] [CrossRef] [PubMed]
- Finkelstein, E.A.; Linnan, L.A.; Tate, D.F.; Birken, B.E. A pilot study testing the effect of different levels of financial incentives on weight loss among overweight employees. J. Occup. Environ. Med. 2007, 49, 981–989. [Google Scholar] [CrossRef]
- Eisenmann, J.C.; Gentile, D.A.; Welk, G.J.; Callahan, R.; Strickland, S.; Walsh, M.; Walsh, D.A. SWITCH: Rationale, design, and implementation of a community, school, and family-based intervention to modify behaviors related to childhood obesity. BMC Public Health 2008, 8, 223. [Google Scholar] [CrossRef]
- Ruggiero, L.; Quinn, L.; Castillo, A.; Monahan, C.; Price, L.B.; Hernandez, W. Community Health Worker Diabetes Prevention Awareness Training in an Immersive Virtual World Environment: Mixed Methods Pilot Study. JMIR Form. Res. 2025, 9, e64051. [Google Scholar] [CrossRef]
- Barrington, W.E.; Beresford, S.A.; Koepsell, T.D.; Duncan, G.E.; Moudon, A.V. Worksite neighborhood and obesogenic behaviors: Findings among employees in the Promoting Activity and Changes in Eating (PACE) trial. Am. J. Prev. Med. 2015, 48, 31–41. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oliveira, M.C.A.M.; Viana, J.P.M.N.; Braga, S.d.Q.; Pimentel, M.M.W. Lifestyle Interventions for the Treatment of Obesity in Workers: An Integrative Review. Obesities 2025, 5, 79. https://doi.org/10.3390/obesities5040079
Oliveira MCAM, Viana JPMN, Braga SdQ, Pimentel MMW. Lifestyle Interventions for the Treatment of Obesity in Workers: An Integrative Review. Obesities. 2025; 5(4):79. https://doi.org/10.3390/obesities5040079
Chicago/Turabian StyleOliveira, Marcia Cristina Almeida Magalhães, Julia Passo Machado Neto Viana, Sergio de Queiroz Braga, and Magno Merces Weyll Pimentel. 2025. "Lifestyle Interventions for the Treatment of Obesity in Workers: An Integrative Review" Obesities 5, no. 4: 79. https://doi.org/10.3390/obesities5040079
APA StyleOliveira, M. C. A. M., Viana, J. P. M. N., Braga, S. d. Q., & Pimentel, M. M. W. (2025). Lifestyle Interventions for the Treatment of Obesity in Workers: An Integrative Review. Obesities, 5(4), 79. https://doi.org/10.3390/obesities5040079






