Trends in the Prevalence of Overweight and Obesity and Associated Socioeconomic and Household Environmental Factors among Women in Nepal: Findings from the Nepal Demographic and Health Surveys
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Data Sources
2.3. Sampling Design
2.4. Data Collection
2.5. Sample Size
2.6. Outcome Variables
2.7. Explanatory Variables
2.7.1. Socioeconomic Factors
2.7.2. Household Environmental Factors
2.8. Statistical Analysis
2.9. Ethical Considerations
3. Results
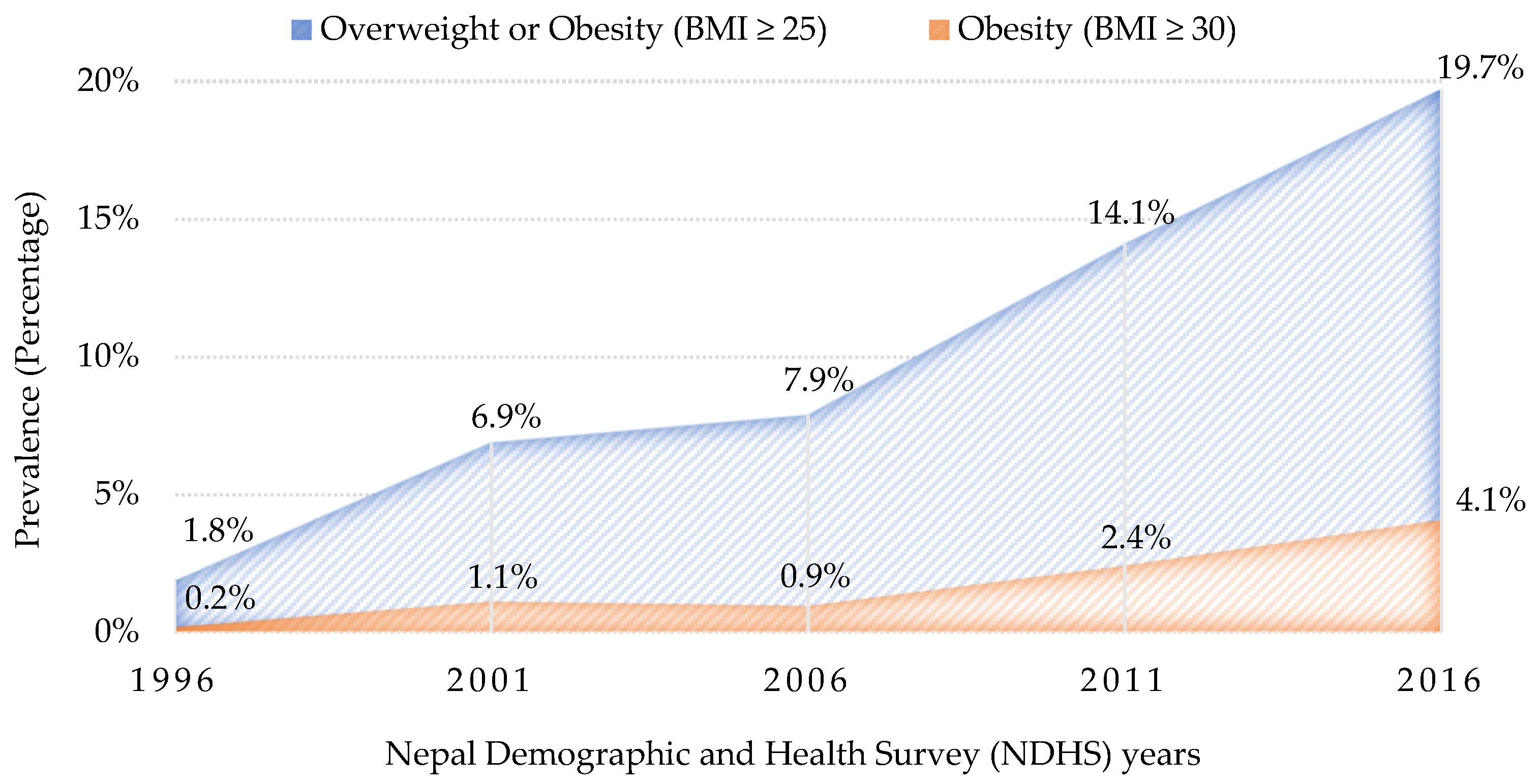
3.1. Trends in the Prevalence of Overweight and Obesity
3.2. Characteristics of the Study Participants from NDHS 2016
3.2.1. Socioeconomic Factors
3.2.2. Household Environmental Factors
3.3. Socioeconomic and Household Environmental Factors Associated with Overweight–Obesity (BMI ≥ 25) and Obesity (BMI ≥ 30)
4. Discussion
4.1. Summary of Key Findings
4.2. Trends in the Prevalence of Overweight and Obesity
4.3. Socioeconomic Factors Associated with Overweight and Obesity
4.4. Household Environmental Factors Associated with Overweight and Obesity
4.5. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Blüher, M. Obesity: Global epidemiology and pathogenesis. Nat. Rev. Endocrinol. 2019, 15, 288–298. [Google Scholar] [CrossRef]
- World Health Organization. Obesity and Overweight; WHO: Geneva, Switzerland, 2020; Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 13 October 2020).
- Dai, H.; Alsalhe, T.A.; Chalghaf, N.; Riccò, M.; Bragazzi, N.L.; Wu, J. The global burden of disease attributable to high body mass index in 195 countries and territories, 1990–2017: An analysis of the Global Burden of Disease Study. PLoS Med. 2020, 17, e1003198. [Google Scholar] [CrossRef] [PubMed]
- NCD Risk Factor Collaboration. Trends in adult body-mass index in 200 countries from 1975 to 2014: A pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet 2016, 387, 1377–1396. [Google Scholar] [CrossRef]
- Stanaway, J.D.; Afshin, A.; Gakidou, E.; Lim, S.S.; Abate, D.; Abate, K.H.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1923–1994. [Google Scholar] [CrossRef]
- Kanter, R.; Caballero, B. Global Gender Disparities in Obesity: A Review. Adv. Nutr. 2012, 3, 491–498. [Google Scholar] [CrossRef]
- Power, M.L.; Schulkin, J. Sex differences in fat storage, fat metabolism, and the health risks from obesity: Possible evolutionary origins. Br. J. Nutr. 2008, 99, 931–940. [Google Scholar] [CrossRef] [PubMed]
- Tuoyire, D.A.; Kumi-Kyereme, A.; Doku, D.T. Socio-demographic trends in overweight and obesity among parous and nulliparous women in Ghana. BMC Obes. 2016, 3, 44. [Google Scholar] [CrossRef]
- Kulie, T.; Slattengren, A.; Redmer, J.; Counts, H.; Eglash, A.; Schrager, S. Obesity and Women’s Health: An Evidence-Based Review. J. Am. Board Fam. Med. 2011, 24, 75–85. [Google Scholar] [CrossRef]
- Cardozo, E.R.; Dune, T.J.; Neff, L.M.; Brocks, M.E.; Ekpo, G.E.; Barnes, R.B.; Marsh, E.E. Knowledge of Obesity and Its Impact on Reproductive Health Outcomes Among Urban Women. J. Community Health 2012, 38, 261–267. [Google Scholar] [CrossRef]
- Swinburn, B.A.; Sacks, G.; Hall, K.D.; McPherson, K.; Finegood, D.T.; Moodie, M.; Gortmaker, S.L. The global obesity pandemic: Shaped by global drivers and local environments. Lancet 2011, 378, 804–814. [Google Scholar] [CrossRef]
- World Health Organization. Noncommunicable Diseases; WHO: Geneva, Switzerland, 2021; Available online: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed on 12 May 2021).
- Abarca-Gómez, L.; Abdeen, Z.A.; Hamid, Z.A.; Abu-Rmeileh, N.M.; Acosta-Cazares, B.; Acuin, C.; Adams, R.J.; Aekplakorn, W.; Afsana, K.; Aguilar-Salinas, C.A.; et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef]
- Ford, N.D.; Patel, S.A.; Narayan, K.V. Obesity in Low- and Middle-Income Countries: Burden, Drivers, and Emerging Challenges. Annu. Rev. Public Health 2017, 38, 145–164. [Google Scholar] [CrossRef]
- World Health Organization. Global Status Report on Noncommunicable Diseases; WHO: Geneva, Switzerland, 2014; Available online: https://apps.who.int/iris/bitstream/handle/10665/148114/9789241564854_eng.pdf (accessed on 14 May 2021).
- United Nations. Transforming Our World: The 2030 Agenda for Sustainable Development; United Nations: New York, NY, USA, 2015; Available online: https://sdgs.un.org/sites/default/files/publications/21252030%20Agenda%20for%20Sustainable%20Development%20web.pdf (accessed on 14 May 2021).
- Central Bureau of Statistics Nepal. National Population and Housing Census 2011: Population Projection 2011–2031; National Planning Commission Secretariat; CBS: Kathmandu, Nepal, 2014. Available online: https://cbs.gov.np/wp-content/upLoads/2018/12/PopulationProjection2011-2031.pdf (accessed on 13 April 2021).
- Central Bureau of Statistics Nepal. Population Monograph of Nepal; National Planning Commission Secretariat; CBS: Kathmandu, Nepal, 2014; Available online: https://nepal.unfpa.org/sites/default/files/pub-pdf/PopulationMonograph2014Volume1.pdf (accessed on 13 April 2021).
- Ministry of Health Nepal; New ERA; ICF. Nepal Demographic and Health Survey 2016; ICF: Kathmandu, Nepal, 2017.
- Al Kibria, G.M. Prevalence and factors affecting underweight, overweight and obesity using Asian and World Health Organization cutoffs among adults in Nepal: Analysis of the Demographic and Health Survey 2016. Obes. Res. Clin. Pract. 2019, 13, 129–136. [Google Scholar] [CrossRef]
- Das Gupta, R.; Haider, S.S.; Hashan, M.R.; Hasan, M.; Sutradhar, I.; Sajal, I.H.; Joshi, H.; Haider, M.R.; Sarker, M. Association between the frequency of television watching and overweight and obesity among women of reproductive age in Nepal: Analysis of data from the Nepal Demographic and Health Survey 2016. PLoS ONE 2020, 15, e0228862. [Google Scholar] [CrossRef]
- Rawal, L.B.; Kanda, K.; Mahumud, R.; Joshi, D.; Mehata, S.; Shrestha, N.; Poudel, P.; Karki, S.; Renzaho, A. Prevalence of underweight, overweight and obesity and their associated risk factors in Nepalese adults: Data from a Nationwide Survey, 2016. PLoS ONE 2018, 13, e0205912. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, N.; Mishra, S.R.; Ghimire, S.; Gyawali, B.; Pradhan, P.M.S.; Schwarz, D. Application of single-level and multi-level modeling approach to examine geographic and socioeconomic variation in underweight, overweight and obesity in Nepal: Findings from NDHS 2016. Sci. Rep. 2020, 10, 2406. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Physical status: The use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ. Tech. Rep. Ser. 1995, 854, 1–452. [Google Scholar]
- Lee, A.; Cardel, M.; Donahoo, W.T. Social and Environmental Factors Influencing Obesity. In Endotext; Feingold, K.R., Anawalt, B., Boyce, A., Chrousos, G., de Herder, W.W., Dhatariya, K., Dungan, K., Grossman, A., Hershman, J.M., Hofland, J., et al., Eds.; MDText.com, Inc.: South Dartmouth, MA, USA, 2000. [Google Scholar]
- Bhurosy, T.; Jeewon, R. Overweight and Obesity Epidemic in Developing Countries: A Problem with Diet, Physical Activity, or Socioeconomic Status? Sci. World J. 2014, 2014, 964236. [Google Scholar] [CrossRef] [PubMed]
- Amarasinghe, A.; D’Souza, G. Individual, Social, Economic, and Environmental Model: A Paradigm Shift for Obesity Prevention. ISRN Public Health 2012, 2012, 571803. [Google Scholar] [CrossRef][Green Version]
- DHS Program. The Demographic and Health Surveys (DHS) Program; ICF: Rockville, MD, USA, 2020; Available online: https://dhsprogram.com/data/available-datasets.cfm (accessed on 28 September 2020).
- DHS Program. Demographic and Health Survey (DHS); ICF: Rockville, MD, USA, 2020; Available online: https://dhsprogram.com/Methodology/Survey-Types/DHS.cfm (accessed on 13 September 2020).
- DHS Program. Team and Partners; ICF: Rockville, MD, USA, 2020; Available online: https://dhsprogram.com/Who-We-Are/About-Us.cfm (accessed on 13 October 2020).
- Ministry of Health and Population Nepal; New ERA; ICF International. Nepal Demographic and Health Survey 2011; ICF International: Kathmandu, Nepal, 2012.
- Ministry of Health and Population Nepal; New ERA; Macro International. Nepal Demographic and Health Survey 2006; Macro International: Kathmandu, Nepal, 2007.
- Ministry of Health Nepal; New ERA; ORC Macro. Nepal Demographic and Health Survey 2001; ORC Macro: Calverton, MD, USA, 2002.
- Pradhan, A.; Aryal, R.H.; Regmi, G.; Ban, B.; Govindasamy, P. Nepal Family Health Survey 1996; Macro International: Kathmandu, Nepal, 1997. [Google Scholar]
- Hosmer, D.W., Jr.; Lemeshow, S.; Sturdivant, R.X. Applied Logistic Regression, 3rd ed.; John Wiley & Sons: Hoboken, NJ, USA, 2013. [Google Scholar]
- Asif, M.; Aslam, M.; Altaf, S.; Atif, S.; Majid, A. Prevalence and Sociodemographic Factors of Overweight and Obesity among Pakistani Adults. J. Obes. Metab. Syndr. 2020, 29, 58–66. [Google Scholar] [CrossRef]
- Chowdhury, M.A.B.; Adnan, M.; Hassan, Z. Trends, prevalence and risk factors of overweight and obesity among women of reproductive age in Bangladesh: A pooled analysis of five national cross-sectional surveys. BMJ Open 2018, 8, e018468. [Google Scholar] [CrossRef]
- Harding, K.L.; Aguayo, V.M.; Webb, P. Trends and Correlates of Overweight among Pre-School Age Children, Adolescent Girls, and Adult Women in South Asia: An Analysis of Data from Twelve National Surveys in Six Countries over Twenty Years. Nutrients 2019, 11, 1899. [Google Scholar] [CrossRef]
- Misra, A.; Jayawardena, R.; Anoop, S. Obesity in South Asia: Phenotype, Morbidities, and Mitigation. Curr. Obes. Rep. 2019, 8, 43–52. [Google Scholar] [CrossRef]
- Misra, A.; Soares, M.J.; Mohan, V.; Anoop, S.; Abhishek, V.; Vaidya, R.; Pradeepa, R. Body fat, metabolic syndrome and hyperglycemia in South Asians. J. Diabetes Complicat. 2018, 32, 1068–1075. [Google Scholar] [CrossRef]
- Ntuk, U.E.; Celis-Morales, C.A.; Mackay, D.F.; Sattar, N.; Pell, J.P.; Gill, J.M.R. Association between grip strength and diabetes prevalence in black, South-Asian, and white European ethnic groups: A cross-sectional analysis of 418 656 participants in the UK Biobank study. Diabet. Med. 2017, 34, 1120–1128. [Google Scholar] [CrossRef] [PubMed]
- Misra, A.; Khurana, L. Obesity-related non-communicable diseases: South Asians vs. White Caucasians. Int. J. Obes. 2010, 35, 167–187. [Google Scholar] [CrossRef] [PubMed]
- Mishra, S.R.; Kallestrup, P.; Neupane, D. Country in Focus: Confronting the challenge of NCDs in Nepal. Lancet Diabetes Endocrinol. 2016, 4, 979–980. [Google Scholar] [CrossRef]
- Luhar, S.; Mallinson, P.A.C.; Clarke, L.; Kinra, S. Trends in the socioeconomic patterning of overweight/obesity in India: A repeated cross-sectional study using nationally representative data. BMJ Open 2018, 8, e023935. [Google Scholar] [CrossRef]
- Amugsi, D.A.; Dimbuene, Z.T.; Mberu, B.; Muthuri, S.; Ezeh, A.C. Prevalence and time trends in overweight and obesity among urban women: An analysis of demographic and health surveys data from 24 African countries, 1991–2014. BMJ Open 2017, 7, e017344. [Google Scholar] [CrossRef]
- Ng, M.; Fleming, T.; Robinson, M.; Thomson, B.; Graetz, N.; Margono, C.; Mullany, E.C.; Biryukov, S.; Abbafati, C.; Abera, S.F.; et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014, 384, 766–781. [Google Scholar] [CrossRef]
- Jayawardena, R.; Byrne, N.; Soares, M.; Katulanda, P.; Hills, A.P. Prevalence, Trends and Associated Socio-Economic Factors of Obesity in South Asia. Obes. Facts 2013, 6, 405–414. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Thapa, G.; Mishra, A.K.; Joshi, P.K. Assessing food and nutrition security in Nepal: Evidence from diet diversity and food expenditure patterns. Food Secur. 2020, 12, 327–354. [Google Scholar] [CrossRef]
- Agrawal, S.; Agrawal, P.; Gupta, K.; Mishra, V. Awareness on causes, consequences and preventive measures of obesity among urban married women in India. Int. J. Med. Public Health 2013, 3, 293–302. [Google Scholar] [CrossRef] [PubMed]
- Popkin, B.M. Technology, transport, globalization and the nutrition transition food policy. Food Policy 2006, 31, 554–569. [Google Scholar] [CrossRef]
- Vaidya, A.; Shakya, S.; Krettek, A. Obesity Prevalence in Nepal: Public Health Challenges in a Low-Income Nation during an Alarming Worldwide Trend. Int. J. Environ. Res. Public Health 2010, 7, 2726–2744. [Google Scholar] [CrossRef]
- Jayawardena, R.; Byrne, N.M.; Soares, M.J.; Katulanda, P.; Hills, A.P. Body weight perception and weight loss practices among Sri Lankan adults. Obes. Res. Clin. Pract. 2014, 8, e192–e200. [Google Scholar] [CrossRef]
- Al Kibria, G.M.; Swasey, K.; Hasan, Z.; Sharmeen, A.; Day, B. Prevalence and factors associated with underweight, overweight and obesity among women of reproductive age in India. Glob. Health Res. Policy 2019, 4, 24. [Google Scholar] [CrossRef]
- Sutradhar, I.; Akter, T.; Hasan, M.; Das Gupta, R.; Joshi, H.; Haider, M.R.; Sarker, M. Nationally representative surveys show gradual shifting of overweight and obesity towards poor and less-educated women of reproductive age in Nepal. J. Biosoc. Sci. 2020, 53, 214–232. [Google Scholar] [CrossRef]
- Tanwi, T.S.; Chakrabarty, S.; Hasanuzzaman, S.; Saltmarsh, S.; Winn, S. Socioeconomic correlates of overweight and obesity among ever-married urban women in Bangladesh. BMC Public Health 2019, 19, 842. [Google Scholar] [CrossRef]
- Kominiarek, M.A.; Peaceman, A.M. Gestational weight gain. Am. J. Obstet. Gynecol. 2017, 217, 642–651. [Google Scholar] [CrossRef]
- Marston, C.; Arjyal, A.; Maskey, S.; Regmi, S.; Baral, S. Using qualitative evaluation components to help understand context: Case study of a family planning intervention with female community health volunteers (FCHVs) in Nepal. BMC Health Serv. Res. 2020, 20, 685. [Google Scholar] [CrossRef]
- Bilger, M.; Kruger, E.J.; Finkelstein, E.A. Measuring Socioeconomic Inequality in Obesity: Looking Beyond the Obesity Threshold. Health Econ. 2016, 26, 1052–1066. [Google Scholar] [CrossRef] [PubMed]
- Villareal, D.T.; Apovian, C.; Kushner, R.F.; Klein, S. Obesity in Older Adults: Technical Review and Position Statement of the American Society for Nutrition and NAASO, The Obesity Society. Obes. Res. 2005, 13, 1849–1863. [Google Scholar] [CrossRef] [PubMed]
- Cohen, A.K.; Rai, M.; Rehkopf, D.H.; Abrams, B. Educational attainment and obesity: A systematic review. Obes. Rev. 2013, 14, 989–1005. [Google Scholar] [CrossRef] [PubMed]
- Gouda, J.; Prusty, R.K. Overweight and Obesity among Women by Economic Stratum in Urban India. J. Health Popul. Nutr. 2014, 32, 79–88. [Google Scholar] [PubMed]
- Sarma, H.; Saquib, N.; Hasan, M.; Saquib, J.; Rahman, A.S.; Khan, J.R.; Uddin, J.; Cullen, M.R.; Ahmed, T. Determinants of overweight or obesity among ever-married adult women in Bangladesh. BMC Obes. 2016, 3, 13. [Google Scholar] [CrossRef] [PubMed]
- Kain, J.; Vio, F.; Albala, C. Obesity trends and determinant factors in Latin America. Cad. Saude Publica 2003, 19, S77–S86. [Google Scholar] [CrossRef]
- Bishwajit, G. Household wealth status and overweight and obesity among adult women in Bangladesh and Nepal. Obes. Sci. Pract. 2017, 3, 185–192. [Google Scholar] [CrossRef]
- Mangemba, N.T.; Sebastian, M.S. Societal risk factors for overweight and obesity in women in Zimbabwe: A cross-sectional study. BMC Public Health 2020, 20, 103. [Google Scholar] [CrossRef] [PubMed]
- Popkin, B.M.; Gordon-Larsen, P. The nutrition transition: Worldwide obesity dynamics and their determinants. Int. J. Obes. 2004, 28, S2–S9. [Google Scholar] [CrossRef] [PubMed]
- Bharmal, N.H.; McCarthy, W.J.; Gadgil, M.D.; Kandula, N.R.; Kanaya, A.M. The Association of Religious Affiliation with Overweight/Obesity Among South Asians: The Mediators of Atherosclerosis in South Asians Living in America (MASALA) Study. J. Relig. Health 2016, 57, 33–46. [Google Scholar] [CrossRef] [PubMed]
- Cline, K.M.C.; Ferraro, K.F. Does Religion Increase the Prevalence and Incidence of Obesity in Adulthood? J. Sci. Study Relig. 2006, 45, 269–281. [Google Scholar] [CrossRef]
- Tan, M.-M.; Chan, C.K.Y.; Reidpath, D.D. Religiosity and Spirituality and the Intake of Fruit, Vegetable, and Fat: A Systematic Review. Evid. Based Complement. Altern. Med. 2013, 2013, 146214. [Google Scholar] [CrossRef] [PubMed]
- Dave, S.S.; Craft, L.L.; Mehta, P.; Naval, S.; Kumar, S.; Kandula, N.R. Life Stage Influences on U.S. South Asian Women’s Physical Activity. Am. J. Health Promot. 2015, 29, e100–e108. [Google Scholar] [CrossRef] [PubMed]
- Biswas, T.; Garnett, S.P.; Pervin, S.; Rawal, L.B. The prevalence of underweight, overweight and obesity in Bangladeshi adults: Data from a national survey. PLoS ONE 2017, 12, e0177395. [Google Scholar] [CrossRef]
- Van Minh, H.; Hung, N.V. Economic Aspects of Sanitation in Developing Countries. Environ. Health Insights 2011, 5, EHI.S8199. [Google Scholar] [CrossRef] [PubMed]
- Morakinyo, O.M.; Adebowale, A.S.; Obembe, T.A.; Oloruntoba, E.O. Association between household environmental conditions and nutritional status of women of childbearing age in Nigeria. PLoS ONE 2020, 15, e0243356. [Google Scholar] [CrossRef]
- Rana, K.; Shrestha, V.; Chimoriya, R. The Effect of Housing on Health and Challenges of Demographic Changes. Glob. J. Sci. Front. Res. 2020, 20, 75–82. [Google Scholar]
- Ghimire, S.; Mishra, S.R.; Sharma, A.; Siweya, A.; Shrestha, N.; Adhikari, B. Geographic and socio-economic variation in markers of indoor air pollution in Nepal: Evidence from nationally-representative data. BMC Public Health 2019, 19, 195. [Google Scholar] [CrossRef]
- Harrison, R.M.; Thornton, C.A.; Lawrence, R.G.; Mark, D.; Kinnersley, R.P.; Ayres, J.G. Personal exposure monitoring of particulate matter, nitrogen dioxide, and carbon monoxide, including susceptible groups. Occup. Environ. Med. 2002, 59, 671–679. [Google Scholar] [CrossRef]
- Li, J.; Xu, X.; Li, D.; Liu, Q.; Xue, H. Association between household fuel types and undernutrition status of adults and children under 5 years in 14 low and middle income countries. Environ. Res. Lett. 2021, 16, 054079. [Google Scholar] [CrossRef]
- Neupane, M.; Basnyat, B.; Fischer, R.; Froeschl, G.; Wolbers, M.; Rehfuess, E.A. Sustained use of biogas fuel and blood pressure among women in rural Nepal. Environ. Res. 2014, 136, 343–351. [Google Scholar] [CrossRef]
- Banks, E.; Lim, L.; Seubsman, S.-A.; Bain, C.; Sleigh, A. Relationship of obesity to physical activity, domestic activities, and sedentary behaviours: Cross-Sectional findings from a national cohort of over 70,000 Thai adults. BMC Public Health 2011, 11, 762. [Google Scholar] [CrossRef] [PubMed]
- Eknoyan, G. A History of Obesity, or How What Was Good Became Ugly and Then Bad. Adv. Chronic Kidney Dis. 2006, 13, 421–427. [Google Scholar] [CrossRef]
- Chen, X.; Zhang, Z.; Yang, H.; Qiu, P.; Wang, H.; Wang, F.; Zhao, Q.; Fang, J.; Nie, J. Consumption of ultra-processed foods and health outcomes: A systematic review of epidemiological studies. Nutr. J. 2020, 19, 86. [Google Scholar] [CrossRef] [PubMed]
- Emery, C.F.; Olson, K.L.; Lee, V.S.; Habash, D.L.; Nasar, J.L.; Bodine, A. Home environment and psychosocial predictors of obesity status among community-residing men and women. Int. J. Obes. 2015, 39, 1401–1407. [Google Scholar] [CrossRef] [PubMed]
- Adhikari, S.; Sigdel, D. Prevalence of Overweight and Obesity and Its Associated Factors among Adult People at Chitwan, Nepal. IOSR J. Nurs. Health Sci. 2020, 9, 30–41. [Google Scholar] [CrossRef]
- Chen, C.-Y.; Pereira, M.A.; Kim, K.H.; Erickson, D.; Jacobs, D.R., Jr.; Zgibor, J.C.; Chung, T.; Sidney, S.; Iribarren, C.; Fabio, A. Fifteen-Year prospective analysis of television viewing and adiposity in african American and caucasian men and women: The CARDIA study. Sage Open 2015, 5, 2158244015600480. [Google Scholar] [CrossRef]
- Lajunen, H.-R.; Keski-Rahkonen, A.; Pulkkinen, L.; Rose, R.J.; Rissanen, A.; Kaprio, J. Are computer and cell phone use associated with body mass index and overweight? A population study among twin adolescents. BMC Public Health 2007, 7, 24. [Google Scholar] [CrossRef] [PubMed]
- Al-Agha, A.E.; Nizar, F.S.; Nahhas, A. The association between body mass index and duration spent on electronic devices in children and adolescents in Western Saudi Arabia. Saudi Med. J. 2016, 37, 436–439. [Google Scholar] [CrossRef]
- Kenney, E.L.; Gortmaker, S.L. United States Adolescents’ Television, Computer, Videogame, Smartphone, and Tablet Use: Associations with Sugary Drinks, Sleep, Physical Activity, and Obesity. J. Pediatr. 2017, 182, 144–149. [Google Scholar] [CrossRef] [PubMed]
- Wang, E.; Abrahamson, K.; Liu, P.J.; Ahmed, A. Can Mobile Technology Improve Weight Loss in Overweight Adults? A Systematic Review. West. J. Nurs. Res. 2019, 42, 747–759. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; Kong, X.; Cao, J.; Chen, S.; Li, C.; Huang, J.; Gu, D.; Kelly, T.N. Mobile Phone Intervention and Weight Loss Among Overweight and Obese Adults: A Meta-Analysis of Randomized Controlled Trials. Am. J. Epidemiol. 2015, 181, 337–348. [Google Scholar] [CrossRef]
| Categories | Sub-Categories | Available DHS Categories |
|---|---|---|
| Source of drinking water | Unimproved | unprotected dug well/spring; tanker truck/cart with small tank; surface water; other |
| Improved | piped into dwelling/yard/plot; piped to neighbour; public tap/standpipe; tube well or borehole; protected dug well; protected spring; rainwater; bottled water | |
| Type of toilet facility | Unimproved | flush/pour flush not to sewer/septic tank/pit latrine; pit latrine without slab/open pit; other; no facility/bush/field |
| Improved | flush/pour flush to piped sewer system/septic tank/pit latrine; ventilated improved pit (VIP) latrine; pit latrine with slab; composting toilet | |
| Cooking fuel | Solid fuel | wood; straw/shrubs/grass; animal dung; agricultural crop; coal/ignite; charcoal; other |
| Clean fuel | electricity; LPG; natural gas; biogas; kerosene | |
| Main floor material | Unimproved | earth/sand; dung; wood planks; palm/bamboo; other |
| Improved | parquet or polished wood; vinyl or asphalt strips; ceramic tiles; cement; carpet | |
| Main wall material | Unimproved | no wall; cane/palm/trunks; mud/sand; bamboo with mud; stone with mud; plywood; cardboard; reused wood; metal/galvanized sheet; other |
| Improved | cement; stone with lime/cement; bricks; cement blocks; wood planks/shingles | |
| Main roof material | Unimproved | no roof; thatch/palm leaf; mud; rustic mat; palm/bamboo; wood planks; cardboard; other |
| Improved | galvanized sheet/metal; wood; calamine/cement fibre; ceramic tiles; cement; roofing shingles |
| Variable n (%) or Mean ± SD | All Participants (n = 6165) | Participants with Overweight–Obesity (BMI ≥ 25) (n = 1215) | Participants with Obesity (BMI ≥ 30) (n = 250) |
|---|---|---|---|
| Weight (kg) | 50.7 ± 9.6 | 64.9 ± 7.9 | 74.7 ± 8.3 |
| Height (cm) | 151.7 ± 5.6 | 151.6 ± 5.5 | 151.1 ± 6.0 |
| BMI (kg/m2) | 22.0 ± 3.9 | 28.2 ± 2.8 | 32.6 ± 2.6 |
| Socioeconomic factors | |||
| Individual-level factors | |||
| Age (years) | |||
| 15–24 | 2331 (37.8%) | 150 (12.3%) | 24 (9.6%) |
| 25–34 | 1834 (29.7%) | 456 (37.5%) | 77 (30.8%) |
| 35–49 | 2000 (32.4%) | 609 (50.1%) | 149 (59.6%) |
| Educational status | |||
| No formal education | 2126 (34.5%) | 375 (30.9%) | 65 (26.0%) |
| Primary | 965 (15.7%) | 244 (20.0%) | 57 (22.8%) |
| Secondary | 2223 (36.1%) | 404 (33.3%) | 88 (35.2%) |
| Higher | 851 (13.8%) | 192 (15.8%) | 40 (16.0%) |
| Employment status | |||
| Not currently employed | 2498 (40.5%) | 480 (39.5%) | 110 (44.0%) |
| Currently employed | 3667 (59.5%) | 735 (60.5%) | 140 (56.0%) |
| Household-level factors | |||
| Marital status | |||
| Never married | 1323 (21.5%) | 64 (5.3%) | 11 (4.4%) |
| Married/living with a partner | 4671 (75.7%) | 1111 (91.4%) | 230 (92.0%) |
| Widowed/divorced/separated | 171 (2.8%) | 40 (3.3%) | 9 (3.6%) |
| Number of household members | |||
| ≤5 | 3763 (61.0%) | 855 (70.4%) | 190 (76.0%) |
| >5 | 2402 (31.0%) | 360 (29.6%) | 60 (24.0%) |
| Wealth index | |||
| Poorest | 1310 (21.2%) | 109 (9.0%) | 9 (3.6%) |
| Poorer | 1250 (20.3%) | 187 (15.4%) | 24 (9.6%) |
| Middle | 1251 (20.3%) | 186 (15.3%) | 26 (10.4%) |
| Richer | 1276 (20.7%) | 283 (23.3%) | 55 (22.0%) |
| Richest | 1078 (17.5%) | 450 (37.0%) | 136 (54.4%) |
| Religion | |||
| Hindu | 5369 (87.1%) | 1022 (84.1%) | 207 (82.8%) |
| Buddhist | 296 (4.8%) | 90 (7.4%) | 21 (8.4%) |
| Muslim | 267 (4.3%) | 41 (3.4%) | 9 (3.6%) |
| Other | 233 (3.8%) | 62 (5.1%) | 13 (5.2%) |
| Household environmental factors | |||
| Environmental factors | |||
| Place of residence | |||
| Urban | 3984 (64.6%) | 893 (73.5%) | 206 (82.4%) |
| Rural | 2181 (35.4%) | 322 (26.5%) | 44 (17.6%) |
| Province of residence | |||
| Province 1 | 878 (14.2%) | 242 (19.9%) | 48 (19.2%) |
| Province 2 | 984 (16.0%) | 113 (9.3%) | 19 (7.6%) |
| Province 3 | 822 (13.3%) | 259 (21.3%) | 69 (27.6%) |
| Province 4 | 783 (12.7%) | 235 (19.3%) | 54 (21.6%) |
| Province 5 | 962 (15.6%) | 182 (15.0%) | 33 (13.2%) |
| Province 6 | 862 (14.0%) | 110 (9.1%) | 17 (6.8%) |
| Province 7 | 874 (14.2%) | 74 (6.1%) | 10 (4.0%) |
| Ecological zone | |||
| Mountain | 441 (7.2%) | 67 (5.5%) | 12 (4.8%) |
| Hill | 2823 (45.7%) | 625 (51.4%) | 136 (54.4%) |
| Terai | 2901 (47.1%) | 523 (43.0%) | 102 (40.8%) |
| Household facilities | |||
| Source of drinking water | |||
| Unimproved | 344 (5.6%) | 41 (3.4%) | 7 (2.8%) |
| Improved | 5549 (90%) | 1132 (93.2%) | 235 (94.0%) |
| Type of toilet facility | |||
| Unimproved | 747 (12.1%) | 67 (5.5%) | 7 (2.8%) |
| Improved | 5146 (83.5%) | 1106 (91.0%) | 235 (94.0%) |
| Cooking fuel | |||
| Solid fuel | 4201 (68.1%) | 557 (45.8%) | 74 (29.6%) |
| Clean fuel | 1690 (27.4%) | 616 (50.7%) | 168 (67.2%) |
| Access to electricity | |||
| No | 592 (9.6%) | 39 (3.2%) | 5 (2.0%) |
| Yes | 5301 (86.0%) | 1134 (93.3%) | 237 (94.8%) |
| Housing characteristics | |||
| Main floor material | |||
| Unimproved | 3815 (61.9%) | 498 (41.0%) | 63 (25.2%) |
| Improved | 2078 (33.7%) | 675 (55.6%) | 179 (71.6%) |
| Main wall material | |||
| Unimproved | 3255 (52.8%) | 427 (35.1%) | 57 (22.8%) |
| Improved | 2638 (42.8%) | 746 (61.4%) | 185 (74.0%) |
| Main roof material | |||
| Unimproved | 635 (10.3%) | 63 (5.2%) | 7 (2.8%) |
| Improved | 5258 (85.3%) | 1110 (91.4%) | 235 (94.0%) |
| Household possessions | |||
| Refrigerator | |||
| No | 5013 (81.3%) | 817 (67.2%) | 134 (53.6%) |
| Yes | 880 (14.3%) | 356 (29.3%) | 108 (43.2%) |
| Television | |||
| No | 2793 (45.3%) | 313 (25.8%) | 46 (18.4%) |
| Yes | 3100 (50.3%) | 860 (70.8%) | 196 (78.4%) |
| Mobile phone | |||
| No | 1747 (28.3%) | 188 (15.5%) | 31 (12.4%) |
| Yes | 4418 (71.7%) | 1027 (84.5%) | 219 (87.6%) |
| Bicycle | |||
| No | 3522 (57.1%) | 731 (60.2%) | 155 (62.0%) |
| Yes | 2371 (38.5%) | 442 (36.4%) | 87 (34.8%) |
| Motorised vehicle | |||
| No | 4782 (77.6%) | 834 (68.6%) | 143 (57.2%) |
| Yes | 1111 (18.0%) | 339 (27.9%) | 99 (39.6%) |
| Variable | Overweight–Obesity (BMI ≥ 25) | Obesity (BMI ≥ 30) | ||
|---|---|---|---|---|
| COR (95% CI) | p-Value | COR (95% CI) | p-Value | |
| Socioeconomic factors | ||||
| Individual-level factors | ||||
| Age (years) | ||||
| 15–24 | ref | ref | ||
| 25–34 | 4.81 (3.95–5.86) | <0.001 | 4.21 (2.65–6.69) | <0.001 |
| 35–49 | 6.37 (5.26–7.07) | <0.001 | 7.73 (5.01–11.96) | <0.001 |
| Educational status | ||||
| No formal education | ref | ref | ||
| Primary | 1.58 (1.32–1.90) | <0.001 | 1.99 (1.38–2.87) | <0.001 |
| Secondary | 1.04 (0.89–1.21) | 0.646 | 1.30 (0.94–1.81) | 0.108 |
| Higher | 1.36 (1.12–1.65) | 0.002 | 1.56 (1.05–2.34) | 0.029 |
| Employment status | ||||
| Not currently employed | ref | ref | ||
| Currently employed | 1.05 (0.93–1.20) | 0.422 | 0.86 (0.67–1.11) | 0.253 |
| Household-level factors | ||||
| Marital status | ||||
| Never married | ref | ref | ||
| Married/living with a partner | 6.14 (4.73–7.96) | <0.001 | 6.17 (3.36–11.35) | <0.001 |
| Widowed/divorced/separated | 6.01 (3.89–9.27) | <0.001 | 6.62 (2.71–16.23) | <0.001 |
| Number of household members | ||||
| ≤5 | ref | ref | ||
| >5 | 1.67 (1.46–1.91) | <0.001 | 0.48 (0.36–0.64) | <0.001 |
| Wealth index | ||||
| Poorest | ref | ref | ||
| Poorer | 1.94 (1.51–2.49) | <0.001 | 2.83 (1.31–6.11) | 0.008 |
| Middle | 1.92 (1.50–2.47) | <0.001 | 3.07 (1.43–6.57) | 0.004 |
| Richer | 3.14 (2.48–3.98) | <0.001 | 6.51 (3.20–13.23) | <0.001 |
| Richest | 7.90 (6.27–9.94) | <0.001 | 20.87 (10.58–41.19) | <0.001 |
| Religion | ||||
| Hindu | ref | ref | ||
| Buddhist | 1.86 (1.44–2.40) | <0.001 | 1.90 (1.19–3.02) | 0.007 |
| Muslim | 0.77 (0.55–1.08) | 0.135 | 0.87 (0.44–1.71) | 0.687 |
| Other | 1.54 (1.14–2.08) | 0.004 | 1.47 (0.82–2.62) | 0.187 |
| Household environmental factors | ||||
| Environmental factors | ||||
| Place of residence | ||||
| Urban | ref | ref | ||
| Rural | 0.60 (0.52–0.69) | <0.001 | 0.38 (0.27–0.53) | <0.001 |
| Province of residence | ||||
| Province 1 | ref | ref | ||
| Province 2 | 0.34 (0.27–0.44) | <0.001 | 0.34 (0.20–0.58) | <0.001 |
| Province 3 | 1.21 (0.98–1.49) | 0.075 | 1.58 (1.08–2.32) | 0.018 |
| Province 4 | 1.13 (0.91–1.39) | 0.271 | 1.28 (0.86–1.91) | 0.227 |
| Province 5 | 0.61 (0.49–0.76) | <0.001 | 0.61 (0.39–0.97) | 0.035 |
| Province 6 | 0.38 (0.30–0.49) | <0.001 | 0.35 (0.20–0.61) | <0.001 |
| Province 7 | 0.24 (0.18–0.32) | <0.001 | 0.20 (0.10–0.40) | <0.001 |
| Ecological zone | ||||
| Mountain | ref | ref | ||
| Hill | 1.59 (1.21–2.09) | <0.001 | 1.81 (0.99–3.29) | 0.052 |
| Terai | 1.23 (0.93–1.62) | 0.146 | 1.30 (0.71–2.39) | 0.393 |
| Household facilities | ||||
| Source of drinking water | ||||
| Unimproved | ref | ref | ||
| Improved | 1.89 (1.36–2.64) | <0.001 | 2.12 (0.99–4.55) | 0.051 |
| Type of toilet facility | ||||
| Unimproved | ref | ref | ||
| Improved | 2.79 (2.14–3.60) | <0.001 | 5.06 (2.38–10.77) | <0.001 |
| Cooking fuel | ||||
| Solid fuel | ref | ref | ||
| Clean fuel | 3.57 (3.28–4.29) | <0.001 | 6.16 (4.65–8.14) | <0.001 |
| Access to electricity | ||||
| No | ref | ref | ||
| Yes | 3.86 (2.77–5.37) | <0.001 | 5.49 (2.26–13.38) | <0.001 |
| Housing characteristics | ||||
| Main floor material | ||||
| Unimproved | ref | ref | ||
| Improved | 3.21 (2.81–3.66) | <0.001 | 5.61 (4.19–7.52) | <0.001 |
| Main wall material | ||||
| Unimproved | ref | ref | ||
| Improved | 2.61 (2.29–2.98) | <0.001 | 4.23 (3.13–5.72) | <0.001 |
| Main roof material | ||||
| Unimproved | ref | ref | ||
| Improved | 2.43 (1.86–3.18) | <0.001 | 4.19 (1.97–8.94) | <0.001 |
| Household possessions | ||||
| Refrigerator | ||||
| No | ref | ref | ||
| Yes | 3.49 (2.99–4.07) | <0.001 | 5.09 (3.91–6.64) | <0.001 |
| Television | ||||
| No | ref | ref | ||
| Yes | 3.04 (2.64–3.50) | <0.001 | 4.03 (2.91–5.58) | <0.001 |
| Mobile phone | ||||
| No | ref | ref | ||
| Yes | 2.51 (2.12–2.96) | <0.001 | 2.89 (1.97–4.22) | <0.001 |
| Bicycle | ||||
| No | ref | ref | ||
| Yes | 0.88 (0.77–1.00) | 0.046 | 0.83 (0.63–1.08) | 0.166 |
| Motorised vehicle | ||||
| No | ref | ref | ||
| Yes | 2.08 (1.79–2.41) | <0.001 | 3.17 (2.43–4.14) | <0.001 |
| Variable * | Overweight–Obesity (BMI ≥ 25) | Obesity (BMI ≥ 30) | ||
|---|---|---|---|---|
| AOR (95% CI) | p-Value | AOR (95% CI) | p-Value | |
| Socioeconomic factors | ||||
| Individual-level factors | ||||
| Age (years) | ||||
| 15–24 | ref | ref | ||
| 25–34 | 3.00 (2.37–3.82) | <0.001 | 2.21 (1.29–3.79) | 0.004 |
| 35–49 | 4.72 (3.67–6.10) | <0.001 | 4.41 (2.62–7.43) | <0.001 |
| Educational status | ||||
| No formal education | ref | |||
| Primary | 1.43 (1.15–1.77) | 0.001 | ||
| Secondary | 1.21 (0.97–1.50) | 0.096 | ||
| Higher | 1.08 (0.81–1.43) | 0.615 | ||
| Household-level factors | ||||
| Marital status | ||||
| Never married | ref | ref | ||
| Married/living with a partner | 3.48 (2.52–4.81) | <0.001 | 3.06 (1.50–6.24) | 0.002 |
| Widowed/divorced/separated | 2.76 (1.64–4.65) | <0.001 | 2.85 (1.04–7.79) | 0.042 |
| Wealth index | ||||
| Poorest | ref | ref | ||
| Poorer | 1.87 (1.41–2.47) | <0.001 | 2.83 (1.28–6.21) | 0.010 |
| Middle | 1.91 (1.40–2.62) | <0.001 | 3.59 (1.62–7.96) | 0.003 |
| Richer | 2.49 (1.76–3.52) | <0.001 | 5.78 (2.60–12.82) | <0.001 |
| Richest | 4.36 (2.83–6.71) | <0.001 | 10.52 (4.37–25.28) | <0.001 |
| Religion | ||||
| Hindu | ref | |||
| Buddhist | 1.41 (1.03–1.94) | 0.032 | ||
| Muslim | 1.10 (0.74–1.64) | 0.637 | ||
| Other | 1.33 (0.93–1.89) | 0.121 | ||
| Household environmental factors | ||||
| Environmental factors | ||||
| Province of residence | ||||
| Province 1 | ref | ref | ||
| Province 2 | 0.38 (0.28–0.51) | <0.001 | 0.40 (0.23–0.71) | 0.002 |
| Province 3 | 0.92 (0.71–1.13) | 0.533 | 1.00 (0.65–1.54) | 0.997 |
| Province 4 | 0.89 (0.69–1.16) | 0.394 | 1.00 (0.64–1.56) | 0.990 |
| Province 5 | 0.55 (0.43–0.71) | <0.001 | 0.60 (0.37–0.96) | 0.032 |
| Province 6 | 0.53 (0.39–0.71) | <0.001 | 0.57 (0.31–1.02) | 0.056 |
| Province 7 | 0.30 (0.22–0.41) | <0.001 | 0.25 (0.12–0.53) | <0.001 |
| Household facilities | ||||
| Type of toilet facility | ||||
| Unimproved | ref | |||
| Improved | 1.40 (1.04–1.87) | 0.026 | ||
| Cooking fuel | ||||
| Solid fuel | ref | ref | ||
| Clean fuel | 1.44 (1.15–1.81) | 0.002 | 1.66 (1.06–2.60) | 0.026 |
| Household possessions | ||||
| Refrigerator | ||||
| No | ref | ref | ||
| Yes | 1.27 (1.01–1.61) | 0.042 | 1.44 (1.01–2.07) | 0.047 |
| Television | ||||
| No | ref | |||
| Yes | 1.26 (1.04–1.54) | 0.021 | ||
| Mobile phone | ||||
| No | ref | |||
| Yes | 1.51 (1.24–1.84) | <0.001 | ||
| Bicycle | ||||
| No | ref | ref | ||
| Yes | 0.76 (0.63–0.91) | 0.004 | 0.66 (0.48–0.91) | 0.012 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rana, K.; Ghimire, P.; Chimoriya, R.; Chimoriya, R. Trends in the Prevalence of Overweight and Obesity and Associated Socioeconomic and Household Environmental Factors among Women in Nepal: Findings from the Nepal Demographic and Health Surveys. Obesities 2021, 1, 113-135. https://doi.org/10.3390/Obesities1020011
Rana K, Ghimire P, Chimoriya R, Chimoriya R. Trends in the Prevalence of Overweight and Obesity and Associated Socioeconomic and Household Environmental Factors among Women in Nepal: Findings from the Nepal Demographic and Health Surveys. Obesities. 2021; 1(2):113-135. https://doi.org/10.3390/Obesities1020011
Chicago/Turabian StyleRana, Kritika, Puspa Ghimire, Romila Chimoriya, and Ritesh Chimoriya. 2021. "Trends in the Prevalence of Overweight and Obesity and Associated Socioeconomic and Household Environmental Factors among Women in Nepal: Findings from the Nepal Demographic and Health Surveys" Obesities 1, no. 2: 113-135. https://doi.org/10.3390/Obesities1020011
APA StyleRana, K., Ghimire, P., Chimoriya, R., & Chimoriya, R. (2021). Trends in the Prevalence of Overweight and Obesity and Associated Socioeconomic and Household Environmental Factors among Women in Nepal: Findings from the Nepal Demographic and Health Surveys. Obesities, 1(2), 113-135. https://doi.org/10.3390/Obesities1020011







