Large Submandibular Duct Sialolith Removal Using a Diode Laser: Description of the Technique Based on Two Cases and Narrative Review of the Literature
Abstract
1. Introduction
2. Materials and Methods
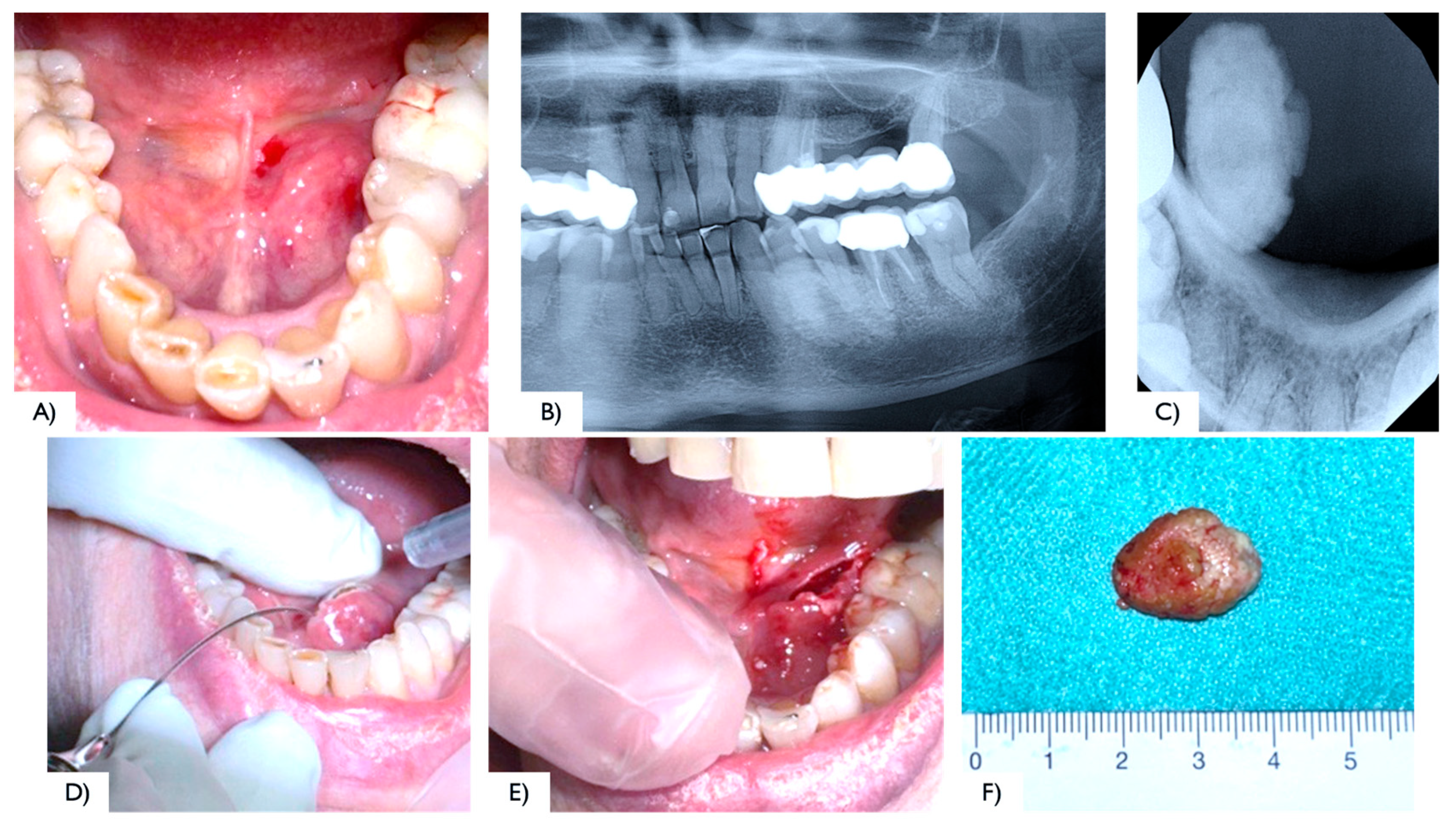
2.1. Case Report 1
2.2. Case Report 2
2.3. Literature Review
3. Results
- Full text not available (n = 10);
- Clinical study on animals (n = 4).
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sánchez Barrueco, A.; Alcalá Rueda, I.; Ordoñez González, C.; Sobrino Guijarro, B.; Santillán Coello, J.; Tapia, G.D.; Guerra Gutiérrez, F.; Campos González, A.; Brenna, A.; Cenjor Españo, C.; et al. Transoral removal of submandibular hilar lithiasis: Results on the salivary duct system, glandular parenchyma, and quality-of-life recovery. Eur. Arch. Oto-Rhino-Laryngol. 2023, 280, 5031–5037. [Google Scholar] [CrossRef]
- Togni, L.; Mascitti, M.; Santarelli, A.; Contaldo, M.; Romano, A.; Serpico, R.; Rubini, C. Unusual Conditions Impairing Saliva Secretion: Developmental Anomalies of Salivary Glands. Front. Physiol. 2019, 10, 855. [Google Scholar] [CrossRef] [PubMed]
- Ungari, C.; Cicconetti, A.; Cerbelli, E.; Sulpasso, A.; Filiaci, F. Giant submandibular sialolith: A case report. Clin. Ter. 2022, 173, 217–221. [Google Scholar]
- Romero, N.J.; Fuson, A.; Kieliszak, C.R.; Joshi, A.S. Sonolocation during submandibular sialolithotomy. Laryngoscope 2019, 129, 2716–2720. [Google Scholar] [CrossRef] [PubMed]
- Dabirmoghaddam, P.; Hosseinzadehnik, R. Interventional sialendoscopy with endoscopic sialolith removal without fragmentation. Indian J. Otolaryngol. Head Neck Surg. 2013, 65, 111–115. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Soriano-Martín, D.; García-Consuegra, L.; Junquera, L.; Rodríguez-Santamarta, T.; Olay, S.; Junquera-Olay, S. Sialendoscopy approach in treating juvenile recurrent parotitis: A systematic review. J. Otolaryngol. Head Neck Surg. 2023, 52, 53. [Google Scholar] [CrossRef]
- Nofal, A.; El-Anwar, M.W.; Al Shawadfy, M.A.; Fouad, Y.A. Drain-Less Submandibular Gland Excision With Preserved Facial Artery. Ear Nose Throat J. 2022; OnlineFirst. [Google Scholar] [CrossRef]
- Witt, R.L.; Iro, H.; Koch, M.; McGurk, M.; Nahlieli, O.; Zenk, J. Minimally invasive options for salivary calculi. Laryngoscope 2012, 122, 1306–1311. [Google Scholar] [CrossRef]
- Capodiferro, S.; Maiorano, E.; Loiudice, A.M.; Scarpelli, F.; Favia, G. Oral laser surgical pathology: A preliminary study on the clinical advantages of diode laser and on the histopathological features of specimens evaluated by conventional and confocal laser scanning microscopy. Minerva Stomatol. 2008, 57, 1–7. [Google Scholar]
- Capodiferro, S.; Maiorano, E.; Scarpelli, F.; Favia, G. Fibrolipoma of the lip treated by diode laser surgery: A case report. J. Med. Case Rep. 2008, 2, 301. [Google Scholar] [CrossRef]
- Dell’Olio, F.; Baldassarre, M.E.; Russo, F.G.; Schettini, F.; Siciliani, R.A.; Mezzapesa, P.P.; Tempesta, A.; Laforgia, N.; Favia, G.; Li-mongelli, L. Lingual laser frenotomy in newborns with ankyloglossia: A prospective cohort study. Ital. J. Pediatr. 2022, 48, 163. [Google Scholar] [CrossRef] [PubMed]
- Capodiferro, S.; Limongelli, L.; D’Agostino, S.; Tempesta, A.; Dolci, M.; Maiorano, E.; Favia, G. Diode Laser Management of Primary Extranasopharyngeal Angiofibroma Presenting as Maxillary Epulis: Report of a Case and Literature Review. Healthcare 2021, 9, 33. [Google Scholar] [CrossRef]
- da Costa Santos, C.M.; de Mattos Pimenta, C.A.; Nobre, M.R. The PICO strategy for the research question construction and evidence search. Rev. Lat. Am. Enferm. 2007, 15, 508–511. [Google Scholar] [CrossRef] [PubMed]
- Haas OLJr Scolari, N.; da Silva Meirelles, L.; Favoretto, A.X.; de Oliveira, R.B. Sialolith removal in the submandibular region using surgical diode laser: Report of two cases and literature review. Oral Maxillofac. Surg. 2018, 22, 105–111. [Google Scholar] [CrossRef]
- Mathew, J.; Pothanikat, J.J.K.; Vinod Kumar, R.B.; Padikadan, N.O.; Arakkal, N.J. Extremely Large Submandibular Sialolith Removal-A Case Report. Ann. Maxillofac. Surg. 2022, 12, 237–239. [Google Scholar] [CrossRef]
- Kılınç, Y.; Çetiner, S. Surgical Removal of a Giant Sialolith by Diode Laser. Open J. Stomatol. 2014, 4, 484–488. [Google Scholar] [CrossRef]
- Angiero, F.; Benedicenti, S.; Romanos, G.E.; Crippa, R. Sialolithiasis of the submandibular salivary gland treated with the 810- to 830-nm diode laser. Photomed. Laser Surg. 2008, 26, 517–521. [Google Scholar] [CrossRef]
- Azaz, B.; Regev, E.; Casap, N.; Chicin, R. Sialolithectomy done with a CO2 laser: Clinical and scintigraphic results. J. Oral Maxillofac. Surg. 1996, 54, 685–688. [Google Scholar] [CrossRef]
- Barak, S.; Horowitz, I.; Katz, J.; Kaplan, I. Experiences of the CO2 laser in the surgical treatment of intraoral salivary gland pathology. J. Clin. Laser Med. Surg. 1991, 9, 295–299. [Google Scholar] [CrossRef]
- Barak, S.; Katz, J.; Mintz, S. Use of the carbon dioxide laser to locate small sialoliths. J. Oral Maxillofac. Surg. 1993, 51, 379–381. [Google Scholar] [CrossRef]
- Yang, S.W.; Chen, T.A. Transoral carbon dioxide laser sialolithectomy with topical anaesthesia. A simple, effective, and minimally invasive method. Int. J. Oral Maxillofac. Surg. 2011, 40, 169–172. [Google Scholar] [CrossRef]
- Williams, M.F. Sialolithiasis. Otolaryngol. Clin. N. Am. 1999, 32, 819–834. [Google Scholar] [CrossRef]
- Favia, G.; Capodiferro, S.; Turco, M.; Cortelazzi, R. Lithiasis of minor salivary glands of the upper lip. Clinico-pathological report of a case with unusual presentation. Minerva Stomatol. 2004, 53, 179–183. [Google Scholar]
- Iro, H.; Dlugaiczyk, J.; Zenk, J. Current concepts in diagnosis and treatment of sialolithiasis. Br. J. Hosp. Med. 2006, 67, 24–28. [Google Scholar] [CrossRef]
- Hald, J.; Andreassen, U.K. Submandibular gland excision: Short- and long-term complications. ORL J. Otorhinolaryngol. Relat. Spec. 1994, 56, 87–91. [Google Scholar] [CrossRef] [PubMed]
- Sutter, E.; Giacomelli-Hiestand, B.; Rücker, M.; Valdec, S. Der CO2-Laser und seine Anwendung in der Stomatologie [CO2 laser application in stomatology]. Swiss. Dent. J. 2019, 129, 214–215. (In German) [Google Scholar] [CrossRef] [PubMed]
- Boj, J.R.; Poirier, C.; Hernandez, M.; Espassa, E.; Espanya, A. Case series: Laser treatments for soft tissue problems in children. Eur. Arch. Paediatr. Dent. 2011, 12, 113–117. [Google Scholar] [CrossRef]
- Tenore, G.; Palaia, G.; Mohsen, A.; Ambrogiano, S.; Gioia, C.R.T.D.; Dominiak, M.; Romeo, U. Could the super-pulsed CO2 laser be used for oral excisional biopsies? Adv. Clin. Exp. Med. 2019, 28, 1513–1517. [Google Scholar] [CrossRef] [PubMed]
- Pal, M.; Saokar, A.; Gopalkrishna, P.; Rajeshwari, H.R.; Kumar, S. Diode laser-assisted management of intraoral soft tissue overgrowth: A case series. Gen. Dent. 2020, 68, 28–31. [Google Scholar]
- Romanos, G.E.; Gutknecht, N.; Dieter, S.; Schwarz, F.; Crespi, R.; Sculean, A. Laser wavelengths and oral implantology. Lasers Med. Sci. 2009, 24, 961–970. [Google Scholar] [CrossRef]
- Ortega-Concepción, D.; Cano-Durán, J.A.; Peña-Cardelles, J.F.; Paredes-Rodríguez, V.M.; González-Serrano, J.; López-Quiles, J. The application of diode laser in the treatment of oral soft tissues lesions. A literature review. J. Clin. Exp. Dent. 2017, 9, e925–e928. [Google Scholar] [CrossRef] [PubMed]
- Al-Mohaya, M.A.; Al-Malik, A.M. Excision of oral pyogenic granuloma in a diabetic patient with 940nm diode laser. Saudi Med. J. 2016, 37, 1395–1400. [Google Scholar] [CrossRef] [PubMed]




| First Author (Year) Country | Study Design | N° Cases, Gender, Age | Sialolith Locations | Laser Type | Laser Setting | Pharmacological Therapy | Complications | Follow-Up | Outcome or Conclusions |
|---|---|---|---|---|---|---|---|---|---|
| Haas OL H. et al. (2018) [14] | Case series | 2 cases, 1 M: 33 Y 1 F: 93 Y | Distal part of the submandibular duct and could be palpated intraorally | Diode laser | 400 μm optical fiber emitting at a wavelength of 980 nm (infrared), 2.5 W output power, and in continuous pulse mode | Amoxicillin (500 mg) every 8 h for 7 days and oral acetaminophen (750 mg) every 6 h for 3 days | No intraoperative complications were reported | Evaluated on days 7, 14, and 30 free surgery. | The diode laser is a safe, minimally invasive option for this procedure, offering enhanced coagulation, high-quality incisions, no bleeding, low nerve damage risk, and minimal comorbidities. |
| Mathew J et al. (2022) [15] | Case report | 1 case, 1 M: 50 Y | Behind the lower right second permanent molar | Diode laser | 810 μm | - | Asymptomatic with undisturbed salivary flow | One year. | Newer treatment modalities offer effective alternatives to conventional surgical methods for sialoliths. |
| Kılınç et al. (2014) [16] | Case report | 1 case, 1 F: 57 Y | In the anterior part of the left side of the floor in the mouth. | Diode laser | 810 nm of wavelength, 4.0 W of power, 0.5 ms continuous wave and 1000 Hz of frequency was selected | Antibiotic: amoxicillin clavulonate 1000 mg, every 12 h for 5 d. Rovamycine every 12 h for 5 d. Anti-inflammatory: 100 mgr flurbiprofen every 12 h for 3 d | No sign of infection was observed, and salivary flow was normal | 10th day. | An 810 nm diode laser is a safe and effective technique, offering excellent cutting and coagulation with a low complication rate, making it suitable for this surgical procedure. |
| Angiero et al. (2008) [17] | Case series | 25 cases | Wharton’s duct | Diode laser | Wavelength of 810–830 nm, 2.5 W CW with 5–10 s irradiation time (energy density 12,5–25 J, flexible fiber 300–320 em | None of the patients required analgesic therapy | Postoperatively, three patients experienced odynophagia, impaired mouth opening, and submandibular swelling, which subsided in 2–3 days | For up to 6 years. | It is a valid alternative to traditional surgery. |
| Azaz et al. (1996) [18] | Case series |
49 cases, 26 M, 23 W: (15 Y–18 Y) | Wharton’s duct: 47; Stensen’s duct: 2 | CO2 laser | 1020 8 W CW | Four patients had antibiotics for 5 days | Four patients experienced discomfort | 7 days after for the follow-up. And after one year. | Excellent results with no bleeding, minimal scarring, and little discomfort. Sialadenectomy should be considered for patients who suffer from recurrent symptoms. |
| Barak et al. (1991) [19] | Case series | 21 cases, 14 M, 7 W. | Wharton’s duct: 10 patients. Submandibular/sublingual glands: 8 patients. Stensen’s duct: 3 patients | CO2 laser | 5 W/10 W in continuous mode | - | No complication | Three weeks. | Complete healing after three weeks. |
| Barak et al. (1993) [20] | Case series | 6 cases, 2 M (22–54 Y) 4 W (19–32 Y) |
Wharton’s duct: 4 patients. Submandibular gland: 2 patients | CO2 laser | 10 W in continuous mode | - | No complication. Postoperative Swelling in 2 patients (Hilus of submandibular gland) | 1 year. | Complete healing in 7 to 20 days. |
| Yang et al. (2011) [21] | Case series | 19 cases, 12 M, 7 FW (8- 54 Y) | In the posterior half of Wharton’s duct | CO2 laser | 4–6 W in continuous mode | - | One patient developed ranula formation after laser surgery | 1–3.5 years. | The results suggest that transoral CO2 laser sialolithectomy is a simple, safe, and low-complication procedure suitable for outpatient treatment. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
D’Albis, G.; Forte, M.; Manfuso, A.; Artin, A.; Fioriello, M.; Di Grigoli, A.; Limongelli, L.; Capodiferro, S. Large Submandibular Duct Sialolith Removal Using a Diode Laser: Description of the Technique Based on Two Cases and Narrative Review of the Literature. Surgeries 2025, 6, 53. https://doi.org/10.3390/surgeries6030053
D’Albis G, Forte M, Manfuso A, Artin A, Fioriello M, Di Grigoli A, Limongelli L, Capodiferro S. Large Submandibular Duct Sialolith Removal Using a Diode Laser: Description of the Technique Based on Two Cases and Narrative Review of the Literature. Surgeries. 2025; 6(3):53. https://doi.org/10.3390/surgeries6030053
Chicago/Turabian StyleD’Albis, Giuseppe, Marta Forte, Alfonso Manfuso, Alexandra Artin, Mariachiara Fioriello, Adriano Di Grigoli, Luisa Limongelli, and Saverio Capodiferro. 2025. "Large Submandibular Duct Sialolith Removal Using a Diode Laser: Description of the Technique Based on Two Cases and Narrative Review of the Literature" Surgeries 6, no. 3: 53. https://doi.org/10.3390/surgeries6030053
APA StyleD’Albis, G., Forte, M., Manfuso, A., Artin, A., Fioriello, M., Di Grigoli, A., Limongelli, L., & Capodiferro, S. (2025). Large Submandibular Duct Sialolith Removal Using a Diode Laser: Description of the Technique Based on Two Cases and Narrative Review of the Literature. Surgeries, 6(3), 53. https://doi.org/10.3390/surgeries6030053








