Abstract
Tumors of the spine are rare, with an incidence of 1.0 and 1.5 per 100,000 individuals. A 44-year-old female patient underwent emergency surgery for posterior decompression and tumor resection. A 3-level laminectomy was performed from T6 to T8 using the Medtronic Midas Rex drill and a 5 mm diamond drill, with microsurgical resection of the lesion. A new resection was performed one week later to address a residual tumor located towards the rostral and cephalic levels. A sample of the extradural lesion was obtained and was sent to the Pathology Department of the Hospital Regional de Alta Especialidad de Ixtapaluca (HRAEI) for histopathological diagnosis, reporting Grade 1 psammomatous meningioma according to the WHO’s criteria. Our patient’s rehabilitation treatment consisted of two parts. The first part occurred during her hospital stay, before and after surgery, and upon her discharge. At the first outpatient consultation three weeks after surgery, the patient showed improved strength in the lower extremities, scoring 4/5 on the Daniel’s scale muscle strength test. After one year of follow-up, our patient has recovered muscle strength. This allows her to move freely, scoring 5/5 on the Daniel’s scale muscle strength test.
1. Introduction
Tumors of the spine are rare, with an incidence of 1.0 and 1.5 per 100,000 individuals. They can be classified as extradural, intradural extramedullary, and intradural intramedullary lesions [1,2,3].
As far as intradural tumors are concerned, they can be classified according to their location into intramedullary (if the injury affects the spinal cord) or extramedullary (if the lesion does not affect the spinal cord but is located within the dura mater) types [4,5,6,7]. The most common intradural extramedullary tumors are schwannomas [1,3,5,8], commonly located in the cervical and lumbar region; neurofibromas; and meningiomas, which are typically located in the thoracic region [3,9,10]. The latter are tumors originating from arachnoid cells found in the dural layers of the thecal sac [1,11,12].
Most meningiomas are benign, slow-growing, and do not invade the surrounding structures. However, the progressive growth and compression of the spinal cord can cause myelopathic symptoms of sensory or motor defects and, less frequently, pain. Among the main clinical presentations, the presence of masses, the loss of strength in the lower extremities, paraparesis, paraparesis in the lower extremities, paresthesia, hypoesthesia, neck pain associated with tingling, progressive spastic quadriparesis with bladder disturbances, and an inability to walk stand out [1,13].
On magnetic resonance imaging (MRI), meningiomas are usually isointense at T1 and hyperintense at T2 compared to the spinal cord. Complete surgical resection is the mainstay of the surgical treatment of symptomatic and asymptomatic spinal meningiomas, and the results depend on the size of the tumor, its location, and the patient’s preoperative neurological status [1,14,15].
The objective of this work is to report the case of an extradural meningioma with a rare location, identified in a patient with paraparesis. After two surgical interventions, total resection of the tumor was achieved, and with physical rehabilitation treatment she regained strength and moved freely. We also sought to review the cases that have been reported.
2. Case Presentation
A 44-year-old female patient without comorbidities started experiencing symptoms of acute urinary retention on 2 February 2023. Additionally, the muscle strength of the pelvic limbs (legs) progressively decreased until she could not stand up and move freely. The strength of the lower extremities scored 1 on the Daniel´s scale. Spastic hypotrophy, as well as loss of balance, incoordination, and hyperreflexia, required the use of a cane for approximately 4 months. Likewise, neuropathic pain increased during this period. The axial pain was diffuse, not well defined, not radicular, and without any specific root.
The course of the illness was insidious and progressive, requiring multiple visits to the emergency room, where the patient was treated with neuromodulators and NSAIDs without improvement. For this reason, an MRI of the lumbar spine was ordered during the first hospital stay (31 March 2023). However, degenerative changes were shown with no radicular compression, which did not explain the symptoms. Therefore, an assessment from the neurosurgery service was requested.
The physical examination and evaluation performed by the neurosurgery service included an imaging study, MRI (5 June 2023), and electrodiagnostic testing (somatosensory evoked potentials and electromyography). The assessments showed the following findings: 1. neuroconduction can be used to study pelvic limbs in normal ranges; 2. somatosensory evoked potential-based study of the pelvic limbs via tibial and peroneal nerves revealed no response on the left side and a slight delay in central conduction time via posterior cords; and 3. electromyography can be carried out without data regarding membrane instability. The magnetic resonance imaging of the thoracic and cervical region revealed an extradural hyperdense lesion at the T6–T8 level, compressing the medullary cord, and myelopathic changes in the spinal cord at the same level; likewise, sensory alteration was identified, with a loss of sensitivity from T10 (Figure 1).
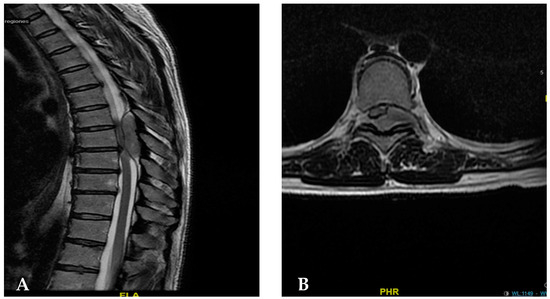
Figure 1.
(A) Sagittal section magnetic resonance imaging performed to identify an epidural lesion causing the compression of the dural sac (blue arrow). (B) Magnetic resonance imaging in the axial section at the T7 level, showing an extradural image that displaces the medullary sac to the right side, and a lesion that invades part of the framen on the left side without apparent extraspinal invasion.
Thus, the patient was admitted to the Hospital Regional de Alta Especialidad de Ixtapaluca (HRAEI), State of Mexico, Mexico, to undergo an emergency surgical procedure. Upon identifying the cause of symptoms and observing paresis, it was decided to intervene urgently for subsequent decompression and tumor resection.
A 3-level laminectomy was performed from T6 to T8 using the Medtronic Midas Rex drill and a 5 mm diamond drill with microsurgical resection of the lesion (5 June 2023). During the procedure, there was a failure of the microscope light, and so the total resection of the tumor was not performed. However, there was a partial improvement in symptoms, with an increased strengthening of both limbs. A new MRI was ordered three days after the first surgical intervention performed on 8 June 2023, showing a residual tumor towards the rostral and cephalic levels (Figure 2).
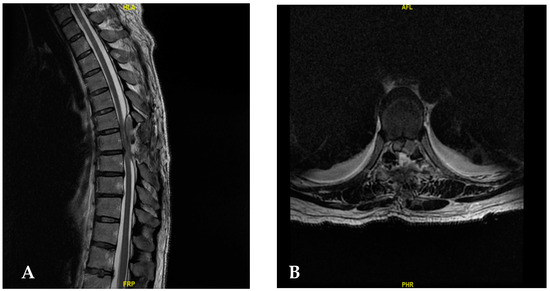
Figure 2.
(A) The MRI results after the first surgical intervention. It shows the distal part of the tumor that was resected, with the proximal part missing, which still causes the compression on the dural sac. (B) Magnetic resonance image of the axial section after the first surgery.
Therefore, a new resection was performed one week later. In this procedure, the cephalic and rostral parts were monitored to observe the limits, laminectomy was completed, and it was possible to see healthy dura mater. The resection was completed, and we observed nerve exit holes and resected the lesion in its entirety (Figure 3).
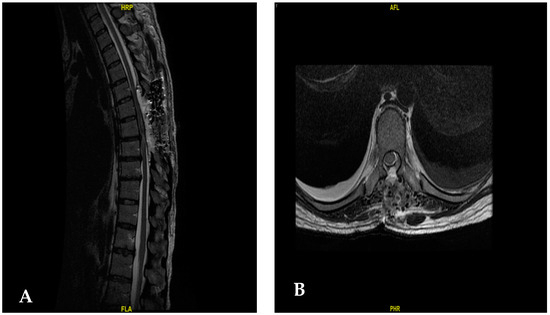
Figure 3.
(A) Post-operative image after the second surgical intervention, showing complete tumor resection with a hyperintense image showing hemostatic material. (B) Axial post-operative image after the second surgery.
Our patient’s rehabilitation treatment consisted of two parts. The first part was during her hospital stay, both before and after surgery. In the pre-surgical and immediate post-surgical rehabilitation (two days after the second surgery), active movements of the upper limbs and passive mobilization of the lower limbs were carried out until the limit was reached in terms of tolerance. In addition, hamstring and triceps surae muscles were stretched, and lower limb muscle re-education was carried out.
In the second stage, she received an out-of-hospital physical treatment plan of two sessions per week for two months that included static and dynamic balance exercises, and visuospatial coordination exercises for the lower limbs. In addition, it included proprioception exercises for the lower limbs, which were performed in a standing position. This plan also included strengthening exercises for the tibialis anterior and calf muscles bilaterally. This included walking re-education with a single-point cane on uneven terrain with obstacles. She subsequently continued with exercises based on a home program for three more months, with periodic reviews by our hospital rehabilitation staff, until her discharge due to improvement. Three weeks later, at the first outpatient consultation, the patient showed strengthening of the lower extremities, scoring 4/5 on the Daniel’s scale muscle strength test. The patient continued rehabilitation and began assisted ambulation, with significant improvement of symptoms: neuropathic pain decreased and sphincter control was regained.
A sample of the extradural lesion obtained from the patient was sent to the Pathology Department of the HRAEI, which determined the histopathological diagnosis according to the WHO’s criteria, namely, Grade 1 psammomatous meningioma.
After one year of follow-up, the patient has improved favorably since she has a muscle strength of 5/5 on the Daniel’s scale, as well as urinary function and sensitivity, which allows her to walk freely (Figure 4).
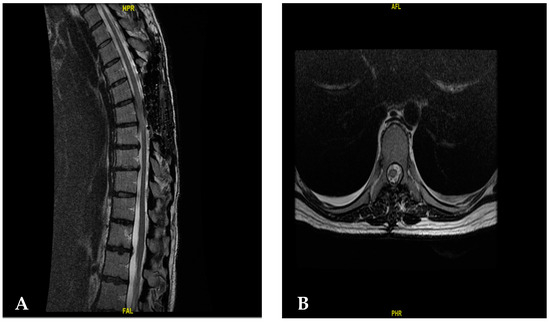
Figure 4.
(A) An image showing the follow-up of the patient 6 months after the first surgery in the sagittal section. (B) Am image showing the follow-up of the patient 6 months after the second surgery in the axial section.
It is worth mentioning that a presumptive diagnosis of meningioma was considered at first. However, the extradural location and characteristics of this cancer did not coincide with what was being reported.
3. Discussion
Exclusively extradural meningiomas are very rare, accounting for 2.5 to 3.5% of spinal meningiomas. However, it is difficult to obtain an accurate frequency as many reports used different criteria to differentiate between partial and complete extradural injuries [16,17,18,19,20,21,22,23,24] (Table 1).

Table 1.
Cases reports of extradural meningiomas.
Several theories have been proposed to explain the pathogenesis of purely extradural meningiomas. On the one hand, they are thought to originate from the ectopic arachnoid cells around the periradicular nerve root cuffs, where the spinal meninge fuses directly with the dura mater, as seen with other extracranial meningiomas, such as the nose or skin [1,2,17,19]. Other authors have suggested that because the periradicular dura mater is thin, it may contain vestigial remains of the superficial layers of the embryonic arachnoid and villi, which explains the extradural location and proximity of the root to some meningiomas [1,3,4,5,19]. It has also been suggested that arachnoid tissue might migrate into the extradural space, as seen in intraorbital meningiomas unrelated to the optic nerve sheath.
Among the diagnostic tools, magnetic resonance imaging is essential for diagnosis, as the sequence shows hypointense responses on T1, hyperintense responses on T2 with contrast media, and homogeneous enhancement after contrast administration [5,8,15,17]. In this case report, simple and contrast-enhanced magnetic resonance imaging were very useful for evaluating the success of the surgical intervention. In this sense, two surgeries were performed due to the residual presence of the meningioma, the second intervention being the one that allowed the total removal of the tumor.
The mainstay of the surgical treatment of symptomatic spinal meningiomas is complete surgical resection. The gross total resection of the tumor is recommended, along with the resection of the part that infiltrates the bone or paraspinal space. Spine stabilization is necessary if the posterolateral approach involves facet joints. In addition, differential diagnosis with hemangioblastoma, plasmacytoma, lymphoma, neuroblastic tumor, leukemia, and epidural abscesses should be considered. Whereas, when conditions originate in the bone, multiple myeloma, aneurysmal bone cyst, osteoblastoma, metastasis, osteosarcoma should be considered, these being the most frequent form of relevant tumor [36]. The resection results depend on the tumor size and location and the patient’s preoperative neurological status [1,5,10,13,15]. As the pathogenesis suggests that extradural meningiomas arise from the dural root sheath and not from its outer surface, removing the dura mater is unnecessary.
In our case, a complete resection was performed next to the paraspinal part since there was no bone invasion. However, a 3-level laminectomy was conducted without opening the dura mater as intradural infiltration was not visible. This is the intervention most reported for cases of meningiomas, followed by thoracotomy and hemilaminectomy, and only one case requiring adjuvant treatment was reported [3,9,12,13,14,16,17,18,19,20,21,22,23,24].
In the case of extradural and intradural meningiomas, there is an increased risk of the recurrence of the lesion if total resection is not performed [34,35]. Whereas, when subtotal resection occurs, radiotherapy should be considered as an adjuvant treatment. In this regard, the recommended conditions for the implementation of radiotherapy are (1) after the total or subtotal resection of an early recurrence; (2) when total resection is not possible due to the location of the tumor or the medical condition of the patient; and (3) when the medical risks of surgical treatment are high. Reoperation should be performed in the case of early recurrence, followed by radiotherapy [34]. Wang et al. [33] reported that the recurrence-free rates after total resection at 5, 10, and 15 years were 93%, 80%, and 68%, respectively, while the progression-free rates during the same periods after subtotal resection were 63%, 45%, and 9%.
It is important to mention that, in the case we present, the patient did not receive adjuvant treatment (chemotherapy or radiotherapy). The case we presented highlights the benefit of pre-surgical and post-operative physical rehabilitation in terms of contributing to the patient’s improvement, with a reduction in evolution times. It is worth mentioning cases of success without adjuvant therapy, such as that reported by Yang et al. [30] regarding meningioma on T6–T8, where laminectomy resolved the lesion and improvement in motor weakness was identified; it was an angiomatous meningioma. Instrumentation was not considered then because the facet joints were unaffected, and the rib cage provided some protection as the lesion occurred at the thoracic level. The patient continued to be monitored for possible deformities in the future, such as increased kyphosis or instability, and to determine whether the use of instrumentation was needed.
After spinal cord injury, most of the determinant factors for walking relate to the severity of the injury, particularly the degree of motor function of the lower extremities. Other common impairments include spasticity, balance, proprioception, and trunk control; cognition also plays a role in walking. Therefore, rehabilitation is essential to improve the patient’s quality of life. According to the good prognostic factors established by Chay and Kirshblum [37], our patient benefited from pre-surgical and post-operative early surgery and rehabilitation.
It is worth mentioning that the prognosis was uncertain due to the data on myelopathy in magnetic resonance imaging; nonetheless, noticeable improvement was observed.
4. Conclusions
Extradural meningiomas are very rare, and so it is essential to perform a differential diagnosis from the presumptive diagnosis of meningioma using specific techniques such as magnetic resonance imaging. The methodological approach for this pathology has yet to be established, and the difficulty in differentiating between partial and complete extradural lesions represents a limitation in the neurosurgical approach. However, tumor resection is an alternative method to treat extradural meningiomas; it is important to consider whether surgical reoperation is necessary to completely resect the tumor. Furthermore, magnetic resonance imaging as well as contrast-enhanced imaging studies are key tools in the management of patients with extradural thoracic meningioma. In addition, pre-surgical and post-surgical rehabilitation treatment are important, allowing for a prompt improvement of the patient.
Author Contributions
A.E.-R. and R.R.A.-G.; methodology, A.E.-R., R.R.A.-G., J.M.S.-C., L.B.M. and E.N.N.; investigation, A.E.-R., C.A.C.-F., A.K.A.M. and O.E.V.-L., writing—original draft preparation, A.E.-R., C.A.C.-F., A.K.A.M. and O.E.V.-L., writing—review and editing, A.E.-R., C.A.C.-F., A.K.A.M. and O.E.V.-L.; supervision, A.E.-R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Hospital Regional de Alta Especialidad de Ixtapaluca (HRAEI) (NR-122-2023; 20 March 2023).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study and written informed consent has been obtained from the patient to publish this paper.
Data Availability Statement
Data are contained within the article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Ledbetter, L.N.; Leever, J.D. Imaging of Intraspinal Tumors. Radiol. Clin. N. Am. 2019, 57, 341–357. [Google Scholar] [CrossRef] [PubMed]
- Schwake, M.; Adeli, A.; Sporns, P.; Ewelt, C.; Schmitz, T.; Sicking, J.; Hess, K.; Spille, D.C.; Paulus, W.; Stummer, W.; et al. Spinal meningiomas–Risks and potential of an increasing age at the time of surgery. J. Clin. Neurosci. 2018, 57, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Kumar, N.; Tan, W.L.B.; Wei, W.; Vellayappan, B.A. An overview of the tumors affecting the spine-Inside to out. Neurooncol. Pract. 2020, 7, i10–i17. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, A.; Nunez, L.; Timaran-Montenegro, D.; Riascos, R. Imaging of Common and Infrequent Extradural Tumors. Neuroimaging Clin. N. Am. 2023, 33, 443–457. [Google Scholar] [CrossRef]
- Bezu, M.T.; Nour, A.S.; Tefera, T.G.; Shumbash, K.Z.; Woldemariam, M.A. Preliminary Review of Spine Tumor Radiologic, Intra-Operative and Histopathology Findings, Addis Ababa, Ethiopia. Ethiop. J. Health Sci. 2022, 32, 41–46. [Google Scholar] [CrossRef]
- Guo, L.; Holdefer, R.N.; Kothbauer, K.F. Monitoring spinal surgery for extramedullary tumors and fractures. Handb. Clin. Neurol. 2022, 186, 245–255. [Google Scholar] [CrossRef]
- Bettaswamy, G.; Ambesh, P.; Das, K.K.; Sahu, R.; Srivastava, A.; Mehrotra, A.; Jaiswal, A.; Jaiswal, S.; Behari, S. Extradural spinal meningioma: Revisiting a rare entity. J. Craniovertebral Junction Spine 2016, 7, 65–68. [Google Scholar] [CrossRef]
- Park, B.J.; Dougherty, M.C.; Noeller, J.; Nourski, K.V.; Gold, C.J.; Menezes, A.H.; Hitchon, C.A.; Bathla, G.; Yamaguchi, S.; Hitchon, P.W. Spinal Meningioma in Adults: Imaging Characteristics, Surgical Outcomes, and Risk Factors for Recurrence. World Neurosurg. 2022, 164, e852–e860. [Google Scholar] [CrossRef]
- Matsuda, S.; Kajihara, Y.; Abiko, M.; Mitsuhara, T.; Takeda, M.; Karlowee, V.; Yamaguchi, S.; Amatya, V.J.; Kurisu, K. Concurrent Schwannoma and Meningioma Arising in the Same Spinal Level: A Report of Two Cases. NMC Case Rep. J. 2018, 5, 105–109. [Google Scholar] [CrossRef]
- Garaud, S.; Boto, J.; Egervari, K.; Vargas, M.I. Extradural Spinal Meningioma Mimicking a Schwannoma: Magnetic Resonance Imaging Findings. Can. J. Neurol. Sci. 2022, 49, 467–469. [Google Scholar] [CrossRef]
- Ho, U.C.; Chang, K.; Lin, Y.H.; Huang, Y.C.; Tsuang, F.Y. Primary intraosseous meningioma of the vertebra: Illustrative case. J. Neurosurg. Case Lessons 2021, 2, CASE213621. [Google Scholar] [CrossRef] [PubMed]
- Utsunomiya, Y.; Mori, N.; Matsui, Y.; Katsushima, H.; Hashimoto, K.; Furuta, A. Intraosseous metaplastic meningioma: A case report. Radiol. Case Rep. 2021, 16, 3300–3303. [Google Scholar] [CrossRef]
- Sivaraju, L.; Thakar, S.; Ghosal, N.; Hegde, A.S. Cervical En-Plaque Extradural Meningioma Involving Brachial Plexus. World Neurosurg. 2017, 108, 994.e7–994.e10. [Google Scholar] [CrossRef] [PubMed]
- Tulloch, I.; Georges, H.; Phadke, R.; Hardwidge, C. A thoracic extradural chordoid meningioma: A unique case report and literature review. Br. J. Neurosurg. 2020, 34, 112–114. [Google Scholar] [CrossRef]
- Lois, L.A.; Ratnakar, S.P.; Leong, C.K.; Yian, S.Y. Radiology Case. Radiol. Cases 2018, 12, 1–10. [Google Scholar]
- Yaldiz, C.; Asil, K.; Ceylan, D.; Erdem, S.A. A Dumbbell-shaped Meningioma in the Thoracic Spine: A Case Report. J. Spine 2014, 3, 168. [Google Scholar] [CrossRef]
- Hersh, E.H.; Sarkiss, C.A.; Ladner, T.R.; Lee, N.; Kothari, P.; Lakomkin, N.; Caridi, J.M. Perioperative Risk Factors for Thirty-Day Morbidity and Mortality in the Resection of Extradural Thoracic Spine Tumors. World Neurosurg. 2018, 114, e950–e956. [Google Scholar] [CrossRef] [PubMed]
- Tuli, J.; Drzymalski, D.M.; Lidov, H.; Tuli, S. Extradural in plaque spinal meningioma with intraneural invasion. World Neurosurg. 2012, 77, 202.e5–202.e13. [Google Scholar] [CrossRef]
- Koeller, K.K.; Shih, R.Y. Intradural extramedullary spinal neoplasms: Radiologic-pathologic correlation. Radiographics 2019, 39, 468–490. [Google Scholar] [CrossRef]
- Ghanchi, H.; Hariri, O.R.; Takayanagi, A.; Li, G. Multiple Extradural Spinal Meningiomas in a Patient with Acquired Immunodeficiency Syndrome: Case Report and Literature Review. World Neurosurg. 2018, 117, 366–370. [Google Scholar] [CrossRef]
- Yokoya, S.; Hisaoka, S.; Fujiwara, G.; Oka, H.; Hino, A. Posttraumatic rapid growing extradural meningioma: A case report on the effectiveness of echosonography. Surg. Neurol. Int. 2022, 13, 61. [Google Scholar] [CrossRef] [PubMed]
- Seo, E.H.; Cha, J.G.; Yoon, Y.S.; Moon, A.R. Extradural Spinal Lymphoplasmacyte-Rich Meningioma in the Thoracic Spine: A Case Report and Literature Review. J. Korean Soc. Radiol. 2022, 83, 924–930. [Google Scholar] [CrossRef] [PubMed]
- Jeong, S.K.; Seong, H.Y.; Roh, S.W. Extra-intradural Spinal Meningioma: A Case Report. Korean J. Spine 2014, 11, 202–204. [Google Scholar] [CrossRef]
- Frank, B.L.; Harrop, J.S.; Hanna, A.; Ratliff, J. Cervical Extradural Meningioma: Case Report and Literature Review. J. Spinal Cord Med. 2008, 31, 302–305. [Google Scholar] [CrossRef]
- Suzuki, A.; Nakamura, H.; Konishi, S.; Yamano, Y. Dumbbell-shaped meningioma with cystic degeneration in the thoracic spine: A case report. Spine 2002, 27, E193–E196. [Google Scholar] [CrossRef]
- Restrepo, C.S.; Herrera, D.A.; Lemos, J.A. Extraforaminal meningioma with extrapleural space extension. Am. J. Roentgenol. 2006, 186, 1314–1316. [Google Scholar] [CrossRef] [PubMed]
- Santiago, B.M.; Rodeia, P.; Cunha, E.; Sa, M. Extradural thoracic spinal meningioma. Neurol India 2009, 57, 98. [Google Scholar] [CrossRef] [PubMed]
- Buchfelder, M.; Nomikos, P.; Paulus, W.; Rupprecht, H. Spinal-thoracic dumbbell meningioma: A case report. Spine 2001, 26, 1500–1504. [Google Scholar] [CrossRef]
- Kim, M.S.; Eun, J.P.; Park, J.S. A dumbbell-shaped meningioma mimicking a schwannoma in the thoracic spine. J. Korean Neurosurg. Soc. 2011, 50, 264–267. [Google Scholar] [CrossRef]
- Yang, Y.; Li, D.; Cao, X.Y.; Hao, S.Y.; Wang, L.; Wu, Z.; Zhang, J.T. Clinical features, treatment, and prognostic factors of chordoid meningioma: Radiological and pathological features in 60 cases of chordoid meningioma. World Neurosurg. 2016, 93, 198–207. [Google Scholar] [CrossRef]
- Khayal, H.B.; Abograra, A.; Iashhab, M. Extradural spinal meningioma in a nine-year-old girl: A case report and review of the literature. Open Access J. Neurol. Neurosurg. 2017, 5, 555659. [Google Scholar]
- Hong, W.; Kim, E.S.; Lee, Y.; Lee, K.; Koh, S.H.; Song, H.; Kwon, M.J. Spinal Extradural Meningioma: A Case Report and Review of the Literature. J. Korean Soc. Radiol. 2018, 79, 11–17. [Google Scholar] [CrossRef]
- Wang, Z.L.; Mou, J.H.; Sun, D.; Liu, P. Case Report: Upper Thoracic Purely Extradural Spinal Meningioma with Nerve Root Attachment: A Case Report and Literature Review. Front. Surg. 2022, 16, 918094. [Google Scholar] [CrossRef]
- Gader, G.; Masmoudi, M.; Ghedira, K.; Krifa, M.I.; Chelly, I.; Zammel, I.; Badri, M. Lumbar spine epidural meningioma: Report of a rare case. Spinal Cord Ser. Cases 2023, 9, 53. [Google Scholar] [CrossRef] [PubMed]
- Redhu, R.; Pavithra, H.N. Spinal extradural meningioma: Report of two cases. J. Craniovertebral Junction Spine 2024, 15, 254–257. [Google Scholar] [CrossRef]
- Arvind, V.; Nevzati, E.; Ghaly, M.; Nasim, M.; Farshad, M.; Guggenberger, R.; Sciubba, D.; Spiessberger, A. Primary extradural tumors of the spinal column: A comprehensive treatment guide for the spine surgeon based on the 5th Edition of the World Health Organization bone and soft-tissue tumor classification. J. Craniovertebral Junction Spine 2021, 12, 336–360. [Google Scholar] [CrossRef]
- Chay, W.; Kirshblum, S. Predicting Outcomes After Spinal Cord Injury. Phys. Med. Rehabil. Clin. N. Am. 2020, 31, 331–343. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).