Abstract
Background: The long-term success of dental implants largely depends on achieving primary stability, previously described as crucial to obtaining osseointegration and immediate loading protocol requirements. Implant thread depths seem to be one of the key factors influencing primary stability, particularly in low-density bone. Insertion torque (IT) and resonance frequency analysis (RFA) are considered the most reliable tests to assess primary stability. The aim of this work was to evaluate how different thread depths of commercially available dental implants affect primary stability in low-density D3 bone. Materials and Methods: An in vitro study was carried out between February 2024 and March 2024. Twenty-four dental implants were divided into four groups (six implants each) according to their thread depths (Group A: 4 mm, Group B: 4.5 mm, Group C: 5 mm, Group D: 5.5 mm) and were inserted in D3-type artificial bone blocks. The main outcome variables were the IT and the Implant Stability Quotient (ISQ) measured in four different areas of the implant (buccal, lingual, mesial, and distal) with an Osstel® ISQ reader. Descriptive and inferential analyses of the data were performed, and the significance value was set at 5%. Results: A total of 24 implants were analyzed. The highest IT values were obtained in Group D, with a mean of 54.03 Ncm (standard deviation (SD) = 8.99), while the lowest measurements were observed in Group A (mean = 25.12; SD: 2.96 N.cm). The mean ISQ values were consistently higher in Group D for each analyzed area, with a mean of 70.13 N.cm (SD = 1.12). Conclusions: Taking into consideration the limitations of this in vitro study, greater thread depths seem to increase the primary stability of dental implants placed in soft bone. Furthermore, a positive correlation was observed between all IT and ISQ values, regardless of the thread depth.
1. Introduction
Implant rehabilitation stands as a treatment of choice for edentulous patients, renowned for its consistent predictability and high rates of survival [1,2,3,4,5].
Adequate primary stability of dental implants is essential to achieve osseointegration and meet the requirements for immediate loading protocols [5,6,7,8]. Bone-to-implant contact (BIC) is regarded as a measure of bone integration and, consequently, is associated to the long-term success of a prosthesis. The micro- and macro-geometry of dental implants are determinant to improve BIC [9,10].
Primary stability is influenced by a combination of factors and holds paramount importance during the initial week following surgery, subsequently exhibiting a substantial decrease to minimal levels around two weeks postoperatively. Such factors include the surgical protocol and implant- and patient-specific variables [1,7,8,10,11,12,13,14]. Recent studies suggest that the macro-geometry of the dental implant used and the bone characteristics of the surgical site play a crucial role in the long-term success of the treatment [10,13,14]. In this regard, the dental implant length, diameter, shape, thread depth, and pitch are important variables to consider [13]. Thread depth represents the measurement of how far the coils extend outward from the core of an implant [13]. Several authors state that implants with deeper threads provide benefits in regions with softer bone and more intense chewing forces because of the expanded BIC area [3,6].
Currently, implant insertion torque (IT) and the implant stability quotient (ISQ) measured through Resonance Frequency Analysis (RFA) are regarded as benchmarks for assessing implant primary stability [1,6,7,11,12,15,16]. The surgical technique, implant design, and bone quality have an impact on this mechanical interlocking. The IT force required, expressed in Ncm, offers information to clinicians regarding the primary stability, density, and quality of the bone [1,7]. According to some authors, an IT of at least 30 Ncm is considered necessary to achieve an ideal level of primary stability [7].
RFA offers non-invasive data and allows for documenting changes during the bone healing period with the aim of assessing when the final restoration or loading, should be performed [1,7,11,17]. The ISQ ranges from 1 to 100, where 100 represents the maximum primary stability [1,11,17]. The literature uniformly acknowledges that ISQ values below 45 indicate low primary stability, while values exceeding 65 indicate high primary stability [16].
Successful primary stability enables a proper process of bone healing and remodeling, leading to implant osseointegration and consequently achieving the so-called secondary stability [7].
The extent of secondary stability progressively rises over time, experiencing a more accelerated increase approximately 2.5 weeks post-implantation, ultimately reaching a plateau around 5–6 weeks post-implantation. The entire transitional period, shifting from the initially predominant primary stability phase to the ultimately dominant secondary stability phase, spans approximately 5–8 weeks [15].
The long-term success of implant treatment is directly proportional to the quality and quantity of bone [18]. Several features should be considered while defining maxillary bone quality—such as metabolic processes, blood flow, mineral deposition, cell turnover, and maturation. Bone density appears to significantly influence the planning and long-term success of implant treatment [19]. Clinical investigations have highlighted higher survival rates for dental implants in the mandible compared with the posterior maxilla, suggesting that bone density differences play a crucial role. Bone with lower densities, often referred to as “soft bone”, clinically exhibits a poor degree of mineralization, increased bone resorption, hindered healing processes, and limited resistance [18].
The aim of the present study was to determine if the thread depth of dental implants affects the primary stability, assessed through IT and ISQ, of implants placed in a low-density D3 bone in an in vitro setting. Secondarily, the authors evaluated if the IT and ISQ values are correlated.
2. Materials and Methods
An in vitro study comprising a total of 24 dental implants with a 3.3 mm inner core and a 10 mm length (Anyridge®, MegaGen® Implant, Daegu, Republic of Korea) was performed. The implants were randomly allocated to 4 groups according to their total widths (Group A (4 mm), Group B (4.5 mm), Group C (5 mm), and Group D (5.5 mm)) (Figure 1). Figure 2 shows the employed implants and the progressive increase in the thread depth determining the final diameters. The implants were tested on three blocks of D3-type artificial bone (Bone Models™, Castellon, Spain) (Figure 3). The study protocol was performed at the CIIS (Center for Interdisciplinary Research in Health), Precision Dental Medicine Platform, Universidade Católica Portuguesa School of Dentistry, Viseu, Portugal.
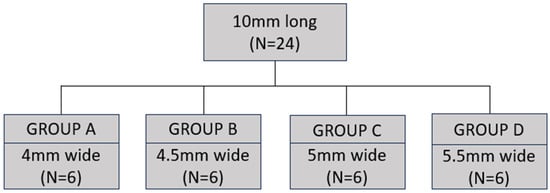
Figure 1.
Implant groups under study.

Figure 2.
From left to right: implants measuring 4 mm (Group A), 4.5 mm (Group B), 5 mm (Group C), and 5.5 mm (Group D) wide × 10 mm long.
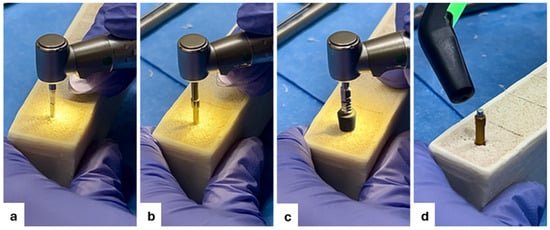
Figure 3.
Implant bed preparation sequence. (a) Initial bur perforation; (b) 2 mm diameter bur perforation; (c) implant insertion; and (d) implant stability quotient measurement.
2.1. In Vitro Implant Placement Procedure
The bone blocks were divided into 24 equal spaces, and the center of the ridge was marked with a pencil. Then, keeping the drills perpendicular to the bone plane of the block, the implant beds were prepared according to the manufacturer’s instructions for placement in low-density bone (i.e., final drill of the same width as the implant core).
2.2. Implant Bed Preparation Sequence
Using a surgical hand piece (Micro-Series CA 20 handpiece, Bien-air Dental® SA, Biel, Switzerland), and the Anyridge® surgical kit (Anyridge®, MegaGen® Implant, Daegu, Republic of Korea), the initial perforation was performed with the lance drill bur, positioned at the central point of one of the 24 designated perforation sites (Figure 3a). The surgical unit (iChiropro Surgery Set, Bien-Air Dental® SA, Biel, Switzerland) was set at 1200 rpm and 20 N/cm. Subsequently, the osteotomy site was progressively enlarged with 2 mm, 2.8 mm, and 3.3 mm diameter drill burs with a vertical stop at 10 mm (Figure 3b). The same perpendicular position relative to the bone was maintained for the insertion of all three drill burs. Once the osteotomy site preparation was completed, the implant was placed (Figure 3c) with the surgical unit set at 35 rpm and 75 N/cm. Applying slight pressure, the implant was inserted up to 1 mm below the bone level. The insertion torque value displayed on the surgical unit screen was recorded. Subsequently, the SmartPeg® (SmartPeg® Osstell®, Gothenburg, Sweden) was manually screwed onto the implant until it was firmly attached. Using the ISQ reader (Osstell®, Sweden), four ISQ measurements simulating buccal, lingual, mesial, and distal were recorded (Figure 3d) by a calibrated investigator (CC). Calibration was performed ahead of the protocol by using a 4 × 10 mm sample placed in the same bone blocks, performing SmartPeg® manual placement and ISQ measurement 5 times a day for 3 days in all V, P, M, and D positions. The non-parametric Friedman test was used, and no significant difference was observed among the measurements. For each inserted implant, IT and ISQ values were recorded.
2.3. Statistical Analysis
An initial descriptive analysis was performed. For the inferential analysis, non-parametric Kruskal–Wallis and Mann–Whitney test with Bonferroni correction (in order to reduce the risk of false positives) were used for group and multiple comparisons. The Spearman correlation test was used to assess correlation between IT and ISQ. The significance value was set at 5%. A convenience sample comprising 24 implants was used.
3. Results
3.1. IT Results
Considering mean values, the highest IT value is observed in Group D (54.03 ± 8.99 N/cm), and the lowest is observed in Group A (25.12 ± 2.96 N/cm). The non-parametric Kruskal–Wallis test indicates that at least one group significantly differs from the others (H = 17.901; p < 0.01). The Mann–Whitney test with Bonferroni correction shows that Group A differs significantly from the other groups, as does Group B, while Groups C and D yield statistically similar results.
3.2. ISQ Results
The highest mean ISQ is observed in Group D (70.13 ± 1.12), and the lowest is observed in Group A (65.58 ± 1.37). However, the results obtained for Groups B and C are relatively close. The non-parametric Kruskal–Wallis test concludes that there is at least one group that has significantly different results from the others (H = 11.751; p < 0.01). Multiple comparisons were conducted using the Mann–Whitney test with Bonferroni correction, and it was found that Group A differs significantly from both Groups B and D. Individual results for the four ISQ measurements are available in Table 1.

Table 1.
Characterization and comparison of mean IT and ISQ measurements. Non-parametric Kruskal–Wallis test and results of multiple comparisons when statistically significant differences are detected.
3.3. IT and ISQ Correlation Results
Table 2 presents the Spearman correlation coefficients between IT and ISQ, and Figure 4 shows a scatter plot depicting the relation between IT and Mean ISQ. It is observed that all correlation coefficients show statistical significance and a positive direction, indicating that if there is an increase in IT, there will also be an increase in the ISQ measures. However, the strength of this increase, i.e., the correlation intensity, varies among the ISQ measures. Specifically, the correlation is weak between IT and ISQ V and ISQ P and moderate to strong with the remaining ISQ measures.

Table 2.
Spearman correlation between the IT and ISQ measures.
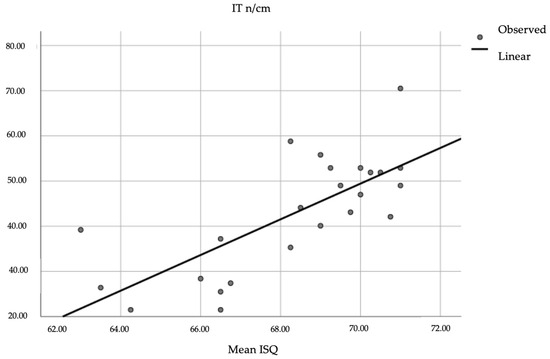
Figure 4.
Scatter plot representing the correlation between IT and mean ISQ.
4. Discussion
The presented results suggest that initial stability in soft bone (D3), evaluated through IT and ISQ, can be managed by correct implant selection, where deeper threads can play an important role. Also, a positive correlation between IT and ISQ is observed.
The use of dental implants with greater thread depth has been suggested to improve the achievement of primary stability and osseointegration in soft bone, where a larger anchoring surface at the bone–implant interface and better force distribution are needed. These implants seem to promote a pressure distribution along all the bone–implant surface and do not depend on the cortical anchorage that can lead to local bone remodeling [6,20]. On the other hand, the macro-geometry of deep-threaded dental implants can pose challenges in the case of perimplantitis and subsequent non-surgical/surgical treatment strategies because of more difficult access between threads [21].
4.1. Discussion of the IT Results
Our results revealed that considering mean values, the highest IT values were obtained in Group D (54.03 ± 8.99 N/cm), while the lowest values were obtained in Group A (25.12 ± 2.96 N/cm).
A comparable study conducted by Lee et al. [6] utilized the same model implants from the same company but with different dimensions. Tests were performed on polyurethane blocks of various densities and with multiple drilling protocols. Their report showed that progressively greater thread depths produced progressively higher IT values across all three block densities of 0.16 g/cm3, 0.24 g/cm3, and 0.32 g/cm3. However, density did not have a significant impact on the relationship between thread depth and IT values. Similarly, in our study, greater thread depths yielded higher IT results. Specifically, Group D, consisting of implants with a diameter of 5.5 mm, exhibited higher torque values compared with Group A, which consisted of implants with a diameter of 4 mm.
According to the studies by Sarfaraz et al., optimal primary stability corresponds to IT values between 30 and 60 N/cm. Therefore, implants with increasing thread depth, belonging to Groups B, C, and D and inserted into soft bone, seemed to have a better adaptation compared with Group A, which had the shallowest thread depth [7]. Furthermore, the threads of Group C (5 mm wide) and Group D (5.5 mm wide) yielded statistically equivalent and significant IT results.
Yet, a high IT value does not always imply implant osseointegration. Other studies suggest that values exceeding 50 N/cm may indeed be detrimental both to bone remodeling and to the implant structures and that osseointegration could be compromised if that threshold is surpassed [20].
4.2. Discussion of the ISQ Results
All the analyzed ISQ data yielded the same result, indicating that Group A (4 mm wide) consistently recorded the lowest values among the four groups, whether comparing the means of individual values (ISQ V, P, M, or D) or comparing the overall mean values among the groups. Notably, Group A, with the shallowest thread depth, always differed significantly from Group D, which had the deepest thread depth. The mean ISQ of Group A was found to be 65.58 ± 1.37, compared with that of Group D, which was 70.13 ± 1.12. Nearly similar results between the mean ISQ values of Groups B (69.04 ± 1.51) and C (68.42 ± 2.76) could be attributed to various factors. For example, there might be minimal variation in the data because of the limited sample size or there could be local variations in the density or structure of the bone block used in the different tests. These variations could affect ISQ measurements, hindering the observation of a positive trend between the two groups.
In general, observing Table 2, we can notice that no implant was found to be at risk of failure, both considering the literature, which deems 45 ISQ as the minimum threshold for implant success, and considering Osstell® guidelines, which set the minimum threshold at 60 ISQ [11,13].
However, the investigation revealed that primary stability in soft bone can be enhanced by preferring implants with deeper threads. Makary et al. also found that implants with larger diameters tend to have higher ISQ values compared with those with smaller diameters when observed during healing phases after 3 and 6 weeks [22].
Tözüm et al.’s results are also in line with ours, as they demonstrated how 12 implants with different diameters, inserted into acrylic resin blocks simulating the mandible, generated positive and significant results considering the relationship between implant width and ISQ [23].
On the other hand, Ohta et al. noticed a positive correlation between these factors, but not one that was truly significant [24].
4.3. Discussion of the IT and ISQ Correlation Results
The question of whether there is a correlation between IT and ISQ values remains a matter of debate [20,22]. The presented IT values, when compared with ISQ values, showed a directly proportional relationship, whereby when the former increased, the latter also increased.
According to Lages et al., the two parameters have no correlation and cannot be used in conjunction [25]. Ito et al. also stated that the lack of correlation is understandable, as the two tests examine different aspects: while IT is a mechanical factor influenced by the entire rotational insertion of the implant, ISQ relates more to the contact between the implant’s collar and the bone [26].
However, other studies revealed data supporting a positive correlation between IT test values and RFA values, possibly due to more standardized research, such as in the study conducted by Farronato et al. on polyurethane blocks [7,12,15,20]. Makary et al., in their comparative study of standard and ultrasonic drilling protocols, also observed a relationship between IT and ISQ, as well as bone quality [22].
Turkyilmaz et al., by placing 230 implants in surgical sites with known bone density, observed a positive correlation among the following examined factors: IT and bone density, ISQ and bone density, and IT and ISQ, thus confirming their previous studies [27].
A favorable aspect of our investigation was the adoption of a surgical protocol tailored to soft bone types. The implants we used were placed in accordance with the manufacturer’s instructions, which recommended a final drilling diameter of 3.3 mm for low-density bone (implant core diameter), which is smaller than the diameter of the implant to be inserted. Therefore, we created an undersized or “misfit” surgical site, which actually allows for a better bone–implant interface [28]. According to Degidi et al., adequate undersizing should not be less than 10%, which aligns with our protocol [29].
This study is subject to limitations because the bone blocks, although commercially standardized, did not have perfectly identical bone densities among them; the implants were tested on only one type of density (D3). We experimented with only one drilling protocol and not multiple protocols for comparison. In addition, we did not use a standardized SmartPeg screwing system but rather a manual one, and one calibrated operator was involved. Finally, the external validity of the presented results should be observed with care because of the use of a limited sample size.
Future research should include cadaveric or clinical samples of different bone types to further assess the subject from a more clinical perspective. Also, different implant geometry and drilling protocols are of interest to this topic.
The presented results support the notion that the primary stability of a dental implant, and thus, its long-term clinical success, can be improved and made more predictable, even in delicate situations, such as the ones with low density or otherwise compromised bone, by selecting an appropriate implant design that can improve clinical outcomes.
5. Conclusions
Taking into consideration the results of this in vitro study and the observed limitations, deeper implant thread depths seem to significantly increase the primary stability of dental implants placed in low-density bone. A positive correlation was found between IT and ISQ variables. Clinically, our results suggest that, in the presence of soft bone, a deeper threaded implant can result in an increased IT and ISQ score, increasing the chance of osseointegration.
Author Contributions
Conceptualization: M.S.P., T.B. and B.L.-A.; methodology: B.L.-A.; investigation: C.C.; writing—original draft: C.C.; writing—review and editing: T.B., R.F. and B.L.-A.; supervision: B.L.-A. All authors have read and agreed to the published version of the manuscript.
Funding
Non-financial logistical support was provided by MegaGen Portugal and CIIS (Center for Interdisciplinary Research in Health)—Precision Dental Medicine Platform, and Universidade Católica Portuguesa School of Dentistry, Viseu, Portugal.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on request.
Acknowledgments
The authors wish to thank Celeste Morais for statistical support.
Conflicts of Interest
The authors declare non-financial support from MegaGen Portugal for this study. The authors would like to declare the following interests outside the work presented: B.L.-A. reports personal fees (sponsored lectures) and non-financial support from Megagen (Daegu, Republic of Korea). R.F. reports grants, personal fees, and non-financial support from MozoGrau (Valladolid, Spain), Avinent (Santpedor, Spain), Inibsa Dental (Lliçà de Vall, Spain), Dentaid SL (Cerdanyola del Vallés, Spain), non-financial support from Nobel Biocare (Zürich, Switzerland), personal fees from Geistlich Pharma AG (Wolhusen, Switzerland), BioHorizons Iberica (Madrid, Spain), Araguaney Dental (Barcelona, Spain), Septodont (Saint-Maur-des-fossés, France), Dentaid SL (Cerdanyola del Vallés, Spain), and Laboratorios Silanes (Mexico City, Mexico) outside the submitted work. Dr. Figueiredo has also participated as a principal investigator in a randomized clinical trial sponsored by Mundipharma (Cambridge, U.K.) and in another clinical trial as a sub-investigator for Menarini Richerche (Florence, Italy). The other authors do not report any potential conflicts of interest.
References
- Lozano-Carrascal, N.; Salomo-Coll, O.; Gilabert-Cerda, M.; Farre-Pages, N.; Gargallo-Albiol, J.; Hernandez-Alfaro, F. Effect of implant macro-design on primary stability: A prospective clinical study. Med. Oral Patol. Oral Cir. Bucal 2016, 21, e214–e221. [Google Scholar] [CrossRef] [PubMed]
- Makary, C.; Menhall, A.; Zammarie, C.; Lombardi, T.; Lee, S.Y.; Stacchi, C.; Park, K.B. Primary stability optimization by using fixtures with different thread depth according to bone density: A clinical prospective study on early loaded implants. Materials 2019, 12, 2398. [Google Scholar] [CrossRef]
- Stoilov, M.; Shafaghi, R.; Stark, H.; Marder, M.; Kraus, D.; Enkling, N. Influence of implant macro-design, -length, and -diameter on primary implant stability depending on different bone qualities using standard drilling protocols—An in vitro analysis. J. Funct. Biomater. 2023, 14, 469. [Google Scholar] [CrossRef] [PubMed]
- Bilhan, H.; Geckili, O.; Mumcu, E.; Bozdag, E.; Sünbüloğlu, E.; Kutay, O. Influence of surgical technique, implant shape and diameter on the primary stability in cancellous bone. J. Oral Rehabil. 2010, 37, 900–907. [Google Scholar] [CrossRef]
- Atieh, M.A.; Alsabeeha, N.; Duncan, W.J. Stability of tapered and parallel-walled dental implants: A systematic review and meta-analysis. Clin. Implant. Dent. Relat. Res. 2018, 20, 634–645. [Google Scholar] [CrossRef]
- Lee, S.-Y.; Kim, S.-J.; An, H.-W.; Kim, H.-S.; Ha, D.-G.; Ryo, K.-H.; Park, K.-B. The effect of the thread depth on the mechanical properties of the dental implant. J. Adv. Prosthodont. 2015, 7, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Sarfaraz, H.; Johri, S.; Sucheta, P.; Rao, S. Study to assess the relationship between insertion torque value and implant stability quotient and its influence on timing of functional implant loading. J. Indian Prosthodont. Soc. 2018, 18, 139–146. [Google Scholar] [CrossRef]
- Mavrogenis, A.F.; Dimitriou, R.; Parvizi, J.; Babis, G.C. Biology of implant osseointegration. J. Musculoskelet. Neuronal Interact. 2009, 9, 61–71. [Google Scholar]
- Smeets, R.; Stadlinger, B.; Schwarz, F.; Beck-Broichsitter, B.; Jung, O.; Precht, C.; Kloss, F.; Gröbe, A.; Heiland, M.; Ebker, T. Impact of dental implant surface modifications on osseointegration. Biomed Res. Int. 2016, 2016, 6285620. [Google Scholar] [CrossRef]
- Falco, A.; Berardini, M.; Trisi, P. Correlation between implant geometry, implant surface, insertion torque, and primary stability: In vitro biomechanical analysis. Int. J. Oral Maxillofac. Implant. 2018, 33, 824–830. [Google Scholar] [CrossRef]
- Dos Santos, M.V.; Elias, C.N.; Cavalcanti Lima, J.H. The effects of superficial roughness and design on the primary stability of dental implants. Clin. Implant. Dent. Relat. Res. 2011, 13, 215–223. [Google Scholar] [CrossRef] [PubMed]
- do Vale Souza, J.P.; de Moraes Melo Neto, C.L.; Piacenza, L.T.; Freitas da Silva, E.V.; de Melo Moreno, A.L.; Penitente, P.A.; Brunetto, J.L.; dos Santos, D.M.; Goiato, M.C. Relation between insertion torque and implant stability quotient: A clinical study. Eur. J. Dent. 2021, 15, 618–623. [Google Scholar] [CrossRef]
- Heimes, D.; Becker, P.; Pabst, A.; Smeets, R.; Kraus, A.; Hartmann, A.; Sagheb, K.; Kämmerer, P.W. How does dental implant macrogeometry affect primary implant stability? A narrative review. Int. J. Implant. Dent. 2023, 9, 20. [Google Scholar] [CrossRef] [PubMed]
- Möhlhenrich, S.C.; Heussen, N.; Elvers, D.; Steiner, T.; Hölzle, F.; Modabber, A. Compensating for poor primary implant stability in different bone densities by varying implant geometry: A laboratory study. Int. J. Oral Maxillofac. Surg. 2015, 44, 1514–1520. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.; Wu, G.; Hunziker, E. The clinical significance of implant stability quotient (ISQ) measurements: A literature review. J. Oral Biol. Craniofacial Res. 2020, 10, 629–638. [Google Scholar]
- Javed, F.; Ahmed, H.B.; Crespi, R.; Romanos, G.E. Role of primary stability for successful osseointegration of dental implants: Factors of influence and evaluation. Interv. Med. Appl. Sci. 2013, 5, 162–167. [Google Scholar] [CrossRef]
- Herrero-Climent, M.; Lemos, B.F.; Herrero-Climent, F.; Falcao, C.; Oliveira, H.; Herrera, M.; Gil, F.J.; Ríos-Carrasco, B.; Ríos-Santos, J.V. Influence of implant design and under-preparation of the implant site on implant primary stability. An in vitro study. Int. J. Environ. Res. Public Health 2020, 17, 4436. [Google Scholar] [CrossRef]
- Gaviria, L.; Salcido, J.P.; Guda, T.; Ong, J.L. Current trends in dental implants. J. Korean Assoc. Oral Maxillofac. Surg. 2014, 40, 50–60. [Google Scholar] [CrossRef]
- Molly, L. Bone density and primary stability in implant therapy. Clin. Oral Implant. Res. 2006, 17, 124–135. [Google Scholar] [CrossRef]
- Farronato, D.; Manfredini, M.; Stocchero, M.; Caccia, M.; Azzi, L.; Farronato, M. Influence of bone quality, drilling protocol, implant diameter/length on primary stability: An in vitro comparative study on insertion torque and resonance frequency analysis. J. Oral Implant. 2020, 46, 182–189. [Google Scholar] [CrossRef]
- Fischer, K.R.; Büchel, J.; Gubler, A.; Liu, C.C.; Sahrmann, P.; Schmidlin, P.R. Nonsurgical cleaning potential of deep-threaded implants and titanium particle release: A novel in vitro tissue model. Clin. Oral Implant. Res. 2023, 34, 416–425. [Google Scholar] [CrossRef] [PubMed]
- Makary, C.; Rebaudi, A.; Sammartino, G.; Naaman, N. Implant primary stability determined by resonance frequency analysis: Correlation with insertion torque, histologic bone volume, and torsional stability at 6 weeks. Implant. Dent. 2012, 21, 474–480. [Google Scholar] [CrossRef] [PubMed]
- Tözüm, T.F.; Turkyilmaz, I.; McGlumphy, E.A. Relationship between dental implant stability determined by resonance frequency analysis measurements and peri-implant vertical defects: An in vitro study. J. Oral Rehabil. 2008, 35, 739–744. [Google Scholar] [CrossRef] [PubMed]
- Ohta, K.; Takechi, M.; Minami, M.; Shigeishi, H.; Hiraoka, M.; Nishimura, M.; Kamata, N. Influence of factors related to implant stability detected by wireless resonance frequency analysis device. J. Oral Rehabil. 2010, 37, 131–137. [Google Scholar] [CrossRef]
- Lages, F.S.; Douglas-de Oliveira, D.W.; Costa, F.O. Relationship between implant stability measurements obtained by insertion torque and resonance frequency analysis: A systematic review. Clin. Implant Dent. Relat. Res. 2018, 20, 26–33. [Google Scholar] [CrossRef]
- Ito, Y.; Sato, D.; Yoneda, S.; Ito, D.; Kondo, H.; Kasugai, S. Relevance of resonance frequency analysis to evaluate dental implant stability: Simulation and histomorphometrical animal experiments. Clin. Oral Implant. Res. 2008, 19, 9–14. [Google Scholar] [CrossRef]
- Turkyilmaz, I.; Tumer, C.; Ozbek, E.N.; Tözüm, T.F. Relations between the bone density values from computerized tomography, and implant stability parameters: A clinical study of 230 regular platform implants. J. Clin. Periodontol. 2007, 34, 716–722. [Google Scholar] [CrossRef]
- Bandela, V.; Munagapati, B.; Komala, J.; Basany, R.B.; Patil, S.R.; Kanaparthi, S. Comparison of primary stability of implants installed by two different methods in D3 and D4 bone types: An in vitro study. J. Int. Soc. Prev. Community Dent. 2020, 10, 620–626. [Google Scholar] [CrossRef]
- Degidi, M.; Daprile, G.; Piattelli, A. Influence of underpreparation on primary stability of implants inserted in poor quality bone sites: An in vitro study. J. Oral Maxillofac. Surg. 2015, 73, 1084–1088. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).