Can We Trust Them? FAST and DPA in Assessing Unstable Patients Following Blunt Abdominal Trauma
Abstract
1. Introduction
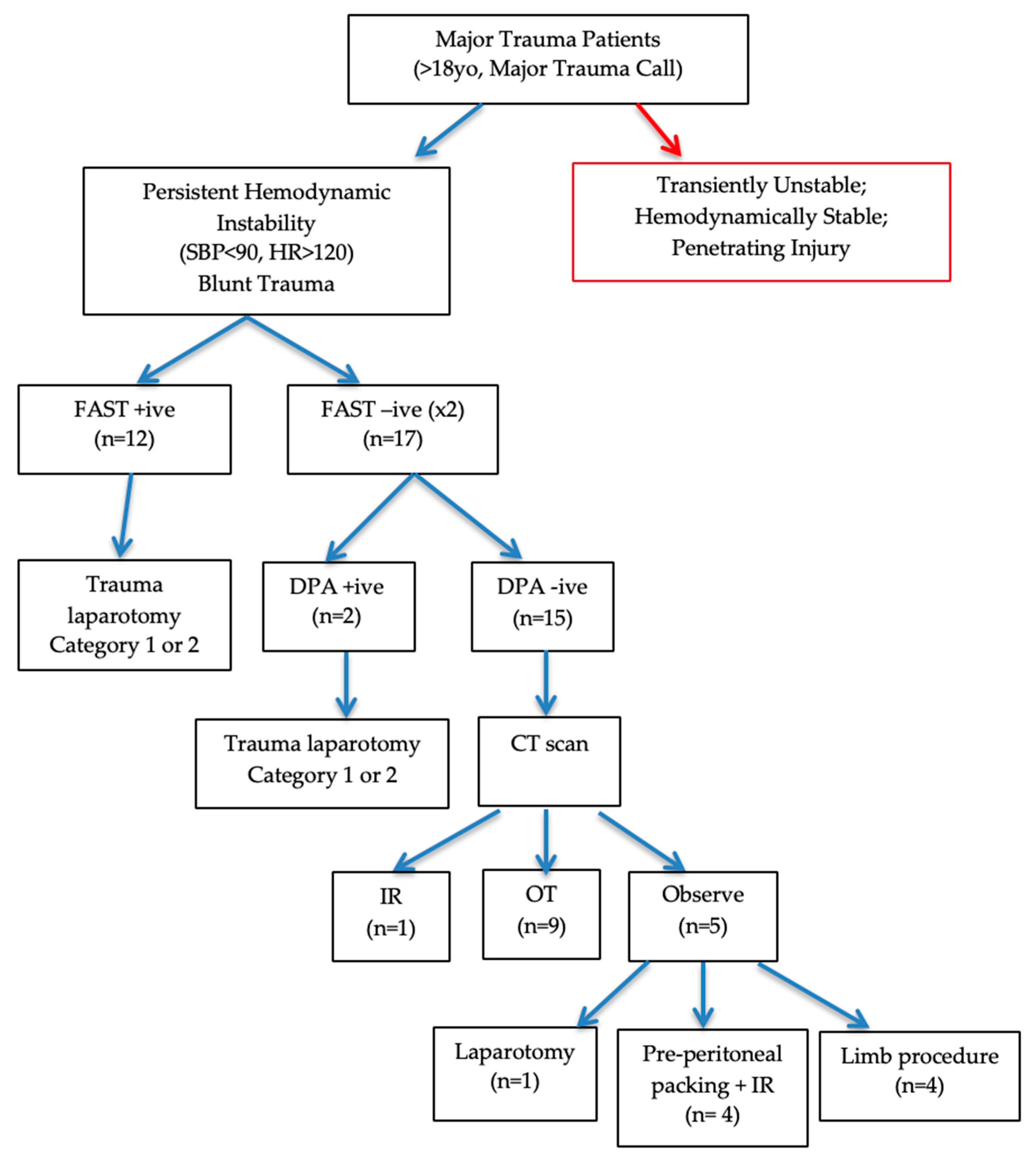
2. Materials and Methods
2.1. Patient Selection
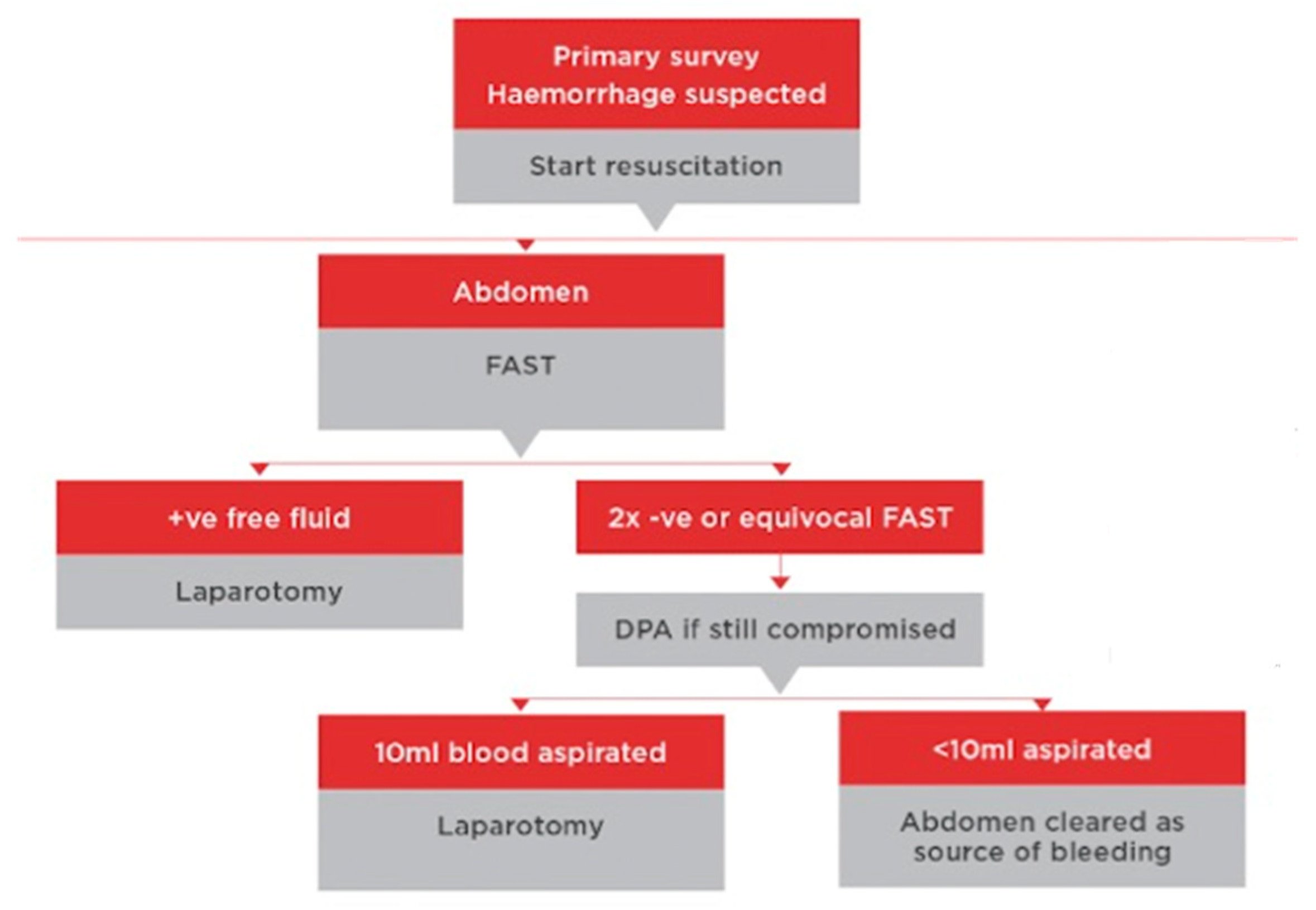
2.2. Clinical Management and Definitions
2.3. Data Collection and Analysis
3. Results
3.1. Basic Characteristics
3.2. DPA Confirmed No Additional Patients with Abdominal Sources of Instability in the Context of Negative FAST
3.3. Non-Hypovolaemic Shock Is Prevalent in FAST Negative Patient Group
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Root, H.D.; Hauser, C.W.; McKinley, C.T. Diagnostic peritoneal lavage. Surgery 1965, 57, 633. [Google Scholar]
- Chereau, N.; Wagner, M.; Tresallet, C.; Lucidarme, O.; Raux, M.; Menegaux, F. CT scan and Diagnostic Peritoneal Lavage: Towards a better diagnosis in the area of nonoperative management of blunt abdominal trauma. Injury 2016, 47, 2006–2011. [Google Scholar] [CrossRef] [PubMed]
- Akoglu, H.; Celik, O.F.; Celik, A.; Ergelen, R.; Onur, O.; Denizbasi, A. Diagnostic accuracy of the Extended Focused Abdominal Sonography for Trauma (E-FAST) performed by emergency physicians compared to CT. Am. J. Emerg. Med. 2018, 36, 1014–1017. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.H.; Shin, S.D.; Song, K.J.; Park, C.B. Diagnostic accuracy of focused assessment with sonography for trauma (FAST) examinations performed by emergency medical technicians. Prehosp. Emerg. Care Off. J. Natl. Assoc. EMS Physicians Natl. Assoc. State EMS Dir. 2012, 16, 400–406. [Google Scholar] [CrossRef] [PubMed]
- Smith, J. Focused assessment with sonography in trauma (FAST): Should its role be reconsidered? Postgrad. Med. J. 2010, 86, 285–291. [Google Scholar] [CrossRef] [PubMed]
- Hsu, J.M.; Joseph, A.P.; Tarlinton, L.J.; Macken, L.; Blome, S. The accuracy of focused assessment with sonography in trauma (FAST) in blunt trauma patients: Experience of an Australian major trauma service. Injury 2007, 38, 71–75. [Google Scholar] [CrossRef]
- Bode, P.; Niezen, R.; van Vugt, A.; Schipper, J. Abdominal Ultrasound as a Reliable Indicator for Conclusive Laparotomy in Blunt Abdominal Trauma. J. Trauma 1993, 34, 27–31. [Google Scholar] [CrossRef] [PubMed]
- Rothlin, M.; Naf, R.; Amgwerd, M.; Candinas, D.; Frick, T.; Trentz, O. Ultrasound in Blunt Abdominal and Thoracic Trauma. J. Trauma 1993, 34, 488–495. [Google Scholar] [CrossRef]
- Rafaqat, W.; Lagazzi, E.; Abiad, M.; Velmahos, G.C. Diagnostic peritoneal lavage is dead: Long live diagnostic peritoneal aspiration. J. Trauma Acute Care Surg. 2024, 96, e24. [Google Scholar] [CrossRef] [PubMed]
- Western Sydney Local Health District. Westmead Trauma Algorithm; Version 1.2.4; [Mobile App]; Western Sydney Local Health District: Sydney, Australia, 2022. [Google Scholar]
- Hoff, W.; Holevar, M.; Nagy, K.; Patterson, L.; Young, J.; Arrillaga, A.; Najarian, M.P.; Valenziano, C.P. Practice Management Guidelines for the Evaluation of Blunt Abdominal Trauma: The EAST Practice Management Guidelines Work Group. J. Trauma 2002, 53, 602–615. [Google Scholar] [CrossRef] [PubMed]
- American College of Surgeons. Advanced Trauma Life Support (ATLS) Course Manual; American College of Surgeons: Chicago, IL, USA, 2012. [Google Scholar]
- Branney, S.W.; Wolfe, R.E.; Moore, E.E.; Albert, N.P.; Heinig, M.; Mestek, M.; Eule, J. Quantitative Sensitivity of Ultrasound in Detecting Free Intraperitoneal Fluid. J. Trauma Acute Care Surg. 1995, 39, 375–380. [Google Scholar] [CrossRef] [PubMed]
- Miller, M.T.; Pasquale, M.D.; Bromberg, W.J.; Wasser, T.E.; Cox, J. Not So Fast. J. Trauma Acute Care Surg. 2003, 54, 52–60. [Google Scholar] [CrossRef] [PubMed]
- Paajanen, H.; Lahti, P.; Nordback, I. Sensitivity of transabdominal ultasonography in detection of intraperitoneal fluid in humans. Eur. Radiol. 1999, 9, 1423–1425. [Google Scholar] [CrossRef] [PubMed]
- Cha, J.Y.; Kashuk, J.L.; Sarin, E.L.; Cothren, C.C.; Johnson, J.L.; Biffl, W.L.; Moore, E.E. Diagnostic peritoneal lavage remains a valuable adjunct to modern imaging techniques. J. Trauma 2009, 67, 330–334; discussion 4–6. [Google Scholar] [CrossRef]
- Schellenberg, M.; Owattanapanich, N.; Emigh, B.; Karavites, L.; Clark, D.H.; Lam, L.; Inaba, K. Contemporary utility of diagnostic peritoneal aspiration in trauma. J. Trauma Acute Care Surg. 2021, 91, 814–819. [Google Scholar] [CrossRef] [PubMed]
- Menegaux, F.; Tresallet, C.; Gosgnach, M.; Nguyen-Thanh, Q.; Langeron, O.; Riou, B. Diagnosis of bowel and mesenteric injuries in blunt abdominal trauma: A prospective study. Am. J. Emerg. Med. 2006, 24, 19–24. [Google Scholar] [CrossRef]
| FAST Negative, Leading to DPA (n = 17) | FAST Positive, Leading to Trauma Laparotomy (n = 12) | p-Values | |
|---|---|---|---|
| Sex, Male | 14 (82%) | 8 (67%) | 0.403 |
| Age, Mean Years (±SD) | 54.5 (±22.2) | 38.3 (±14.9) | 0.019 |
| Mechanism of Injury, n (%) | 0.255 | ||
| MVC | 5 (29%) | 6 (50%) | |
| MBC | 3 (18%) | 4 (33%) | |
| Pedestrian/Bicycle vs. vehicle | 6 (35%) | 1 (8%) | |
| Other | 3 (18%) | 1 (8%) | |
| Injury Severity Score, Median [IQR] | 29 [17–33.5] | 28 [22–42.5] | 0.594 |
| Initial systolic blood pressure | 0.348 | ||
| <90 | 9 (53%) | 8 (66%) | |
| 90–100 | 2 (12%) | - | |
| 100–140 | 4 (24%) | 4 (33%) | |
| >140 | 2 (12%) | - | |
| Initial heart rate | 0.108 | ||
| 50–100 | 5 (29%) | 1 (8%) | |
| 100–120 | 5 (29%) | 1 (8%) | |
| 120–140 | 6 (35%) | 5 (42%) | |
| >140 | 1 (6%) | 4 (33%) | |
| Positive DPA | 2 (12%) | n/a | |
| Operative Management | <0.001 | ||
| Laparotomy | 3 (18%) | 12 (100%) | |
| Pre-peritoneal packing | 4 (24%) | - | |
| Other procedure | 4 (24%) | - | |
| Interventional Radiology | 0.944 | ||
| No Angiography | 10 (59%) | 7 (58%) | |
| Angiography + Intervention | 5 (29%) | 4 (33%) | |
| Angiography (no intervention) | 2 (12%) | 1 (8%) | |
| Laparotomy Findings | <0.001 | ||
| Solid organ injury | 1 (6%) | 6 (50%) | |
| Mesenteric/viscus injury | - | 5 (42%) | |
| No significant intra-abdominal injuries | 16 (94%) | 1 (8%) | |
| Findings on laparotomy | 2 (12%) | 1 (8%) | |
| Implied by no need for laparotomy | 14 (82%) | 0 (0%) | |
| Source of Instability | <0.001 | ||
| Hypovolaemic cause | |||
| Abdomen | - | 11 (92%) | |
| Pelvis | 7 (41%) | - | |
| Long bone/Limb | 4 (23%) | - | |
| External | - | - | |
| Chest | 2 (12%) | - | |
| Distributive cause | 2 (12%) | 1 (8%) | |
| Cardiogenic cause | 1 (6%) | - | |
| Length of Stay, Median Days [IQR] | 22 [4.5–37] | 17 [7–62.5] | 0.739 |
| FAST | DPA | |
|---|---|---|
| True positive | 11 | 0 |
| False negative | 0 | 0 |
| True negative | 17 | 15 |
| False positive | 1 | 2 |
| Sensitivity | - | |
| Specificity | 94% | 88.2% |
| PPV | 91.6% | |
| NPV | 100% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Quinn, R.; Hsu, J.; Pang, T. Can We Trust Them? FAST and DPA in Assessing Unstable Patients Following Blunt Abdominal Trauma. Surgeries 2024, 5, 674-681. https://doi.org/10.3390/surgeries5030053
Quinn R, Hsu J, Pang T. Can We Trust Them? FAST and DPA in Assessing Unstable Patients Following Blunt Abdominal Trauma. Surgeries. 2024; 5(3):674-681. https://doi.org/10.3390/surgeries5030053
Chicago/Turabian StyleQuinn, Rakesh, Jeremy Hsu, and Tony Pang. 2024. "Can We Trust Them? FAST and DPA in Assessing Unstable Patients Following Blunt Abdominal Trauma" Surgeries 5, no. 3: 674-681. https://doi.org/10.3390/surgeries5030053
APA StyleQuinn, R., Hsu, J., & Pang, T. (2024). Can We Trust Them? FAST and DPA in Assessing Unstable Patients Following Blunt Abdominal Trauma. Surgeries, 5(3), 674-681. https://doi.org/10.3390/surgeries5030053






