Nasal Floor Elevation—An Option of Premaxilla Augmentation: A Case Report
Abstract
1. Introduction
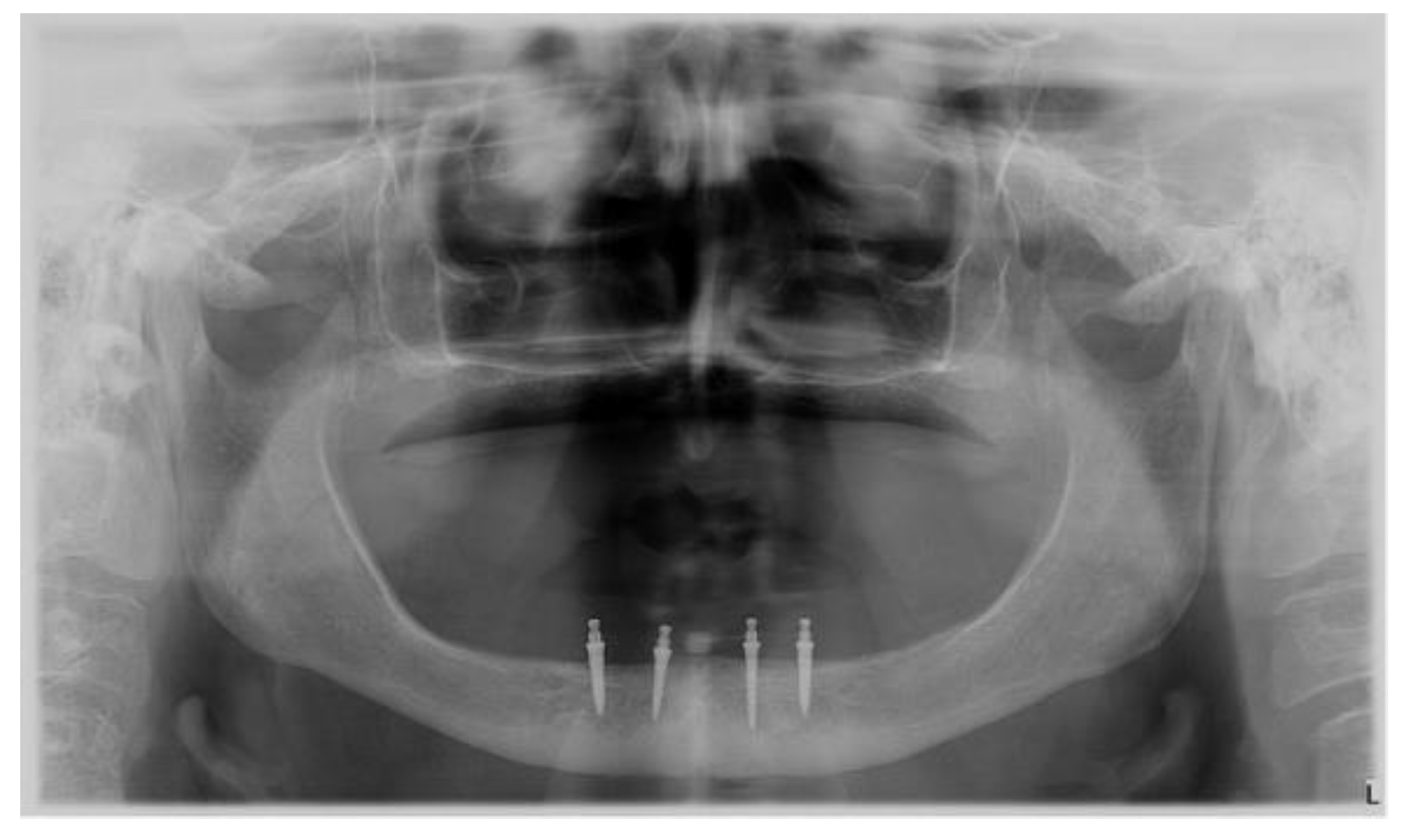
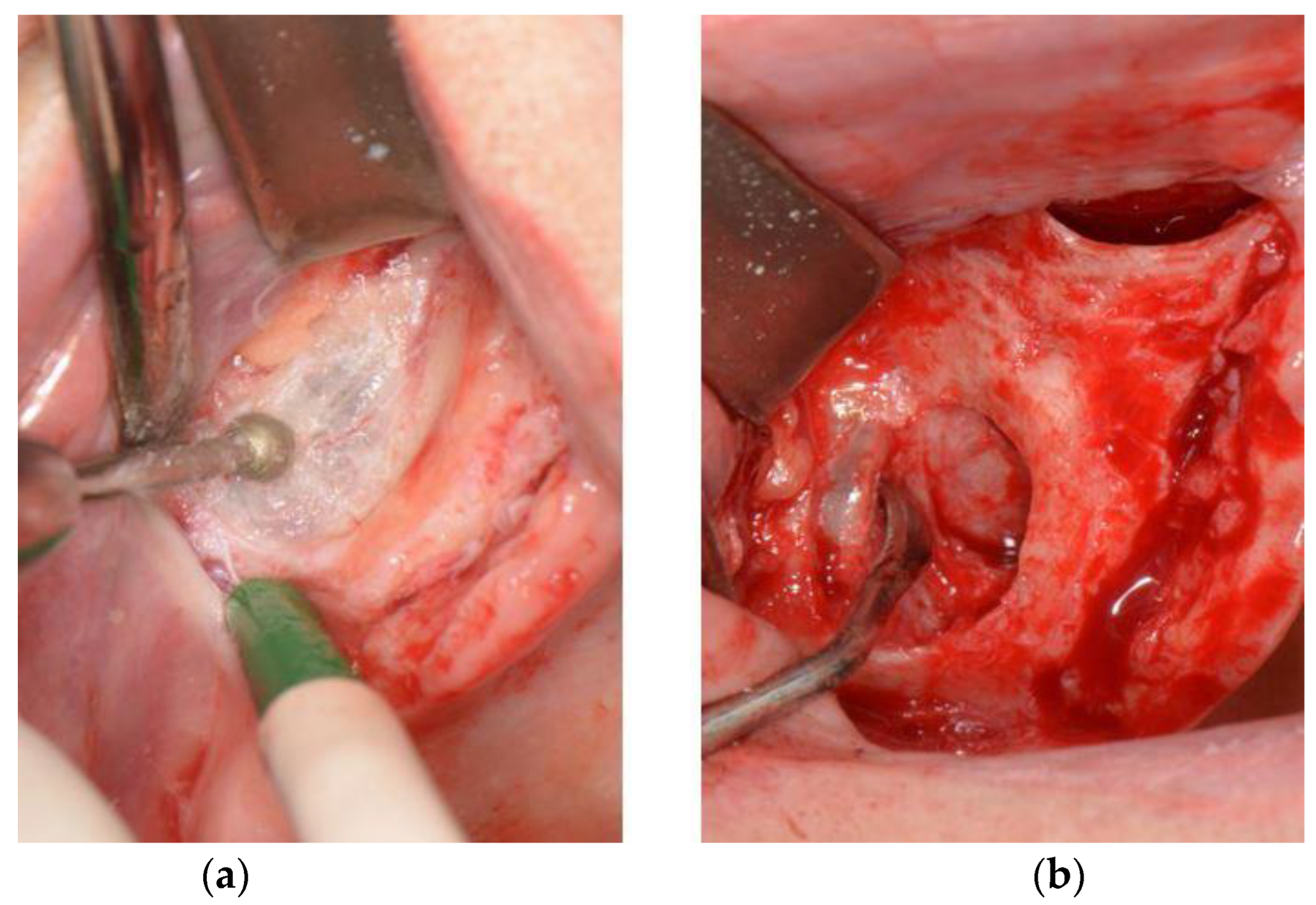
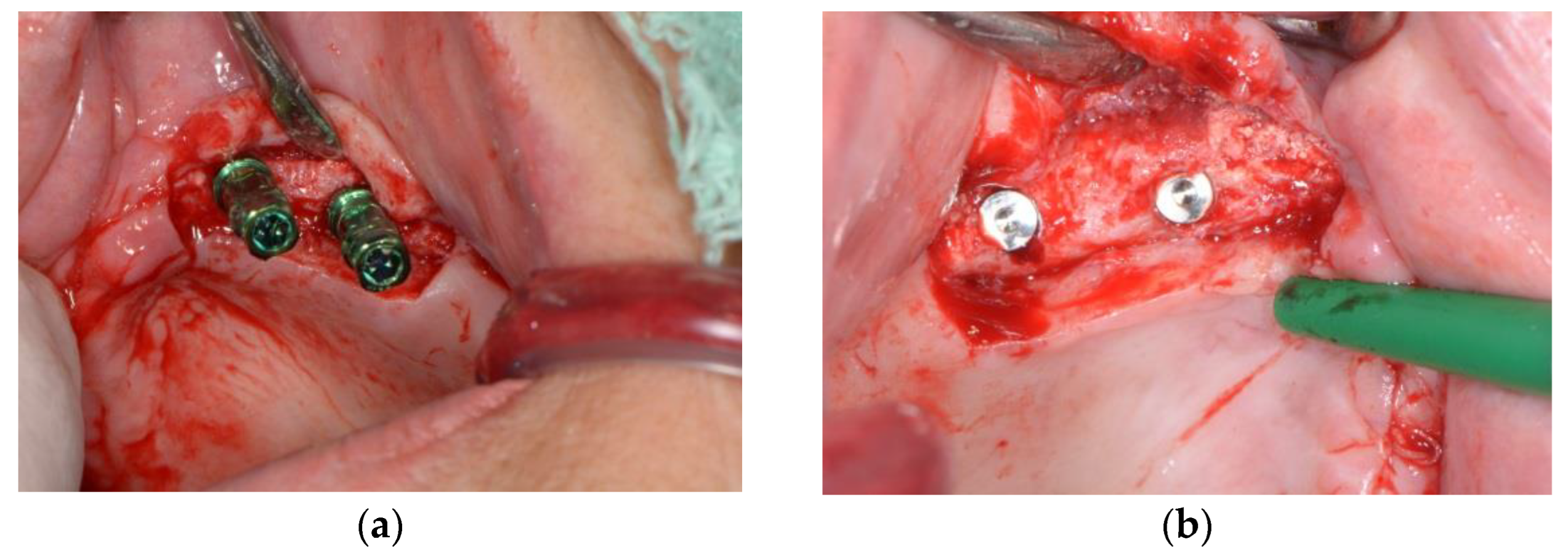
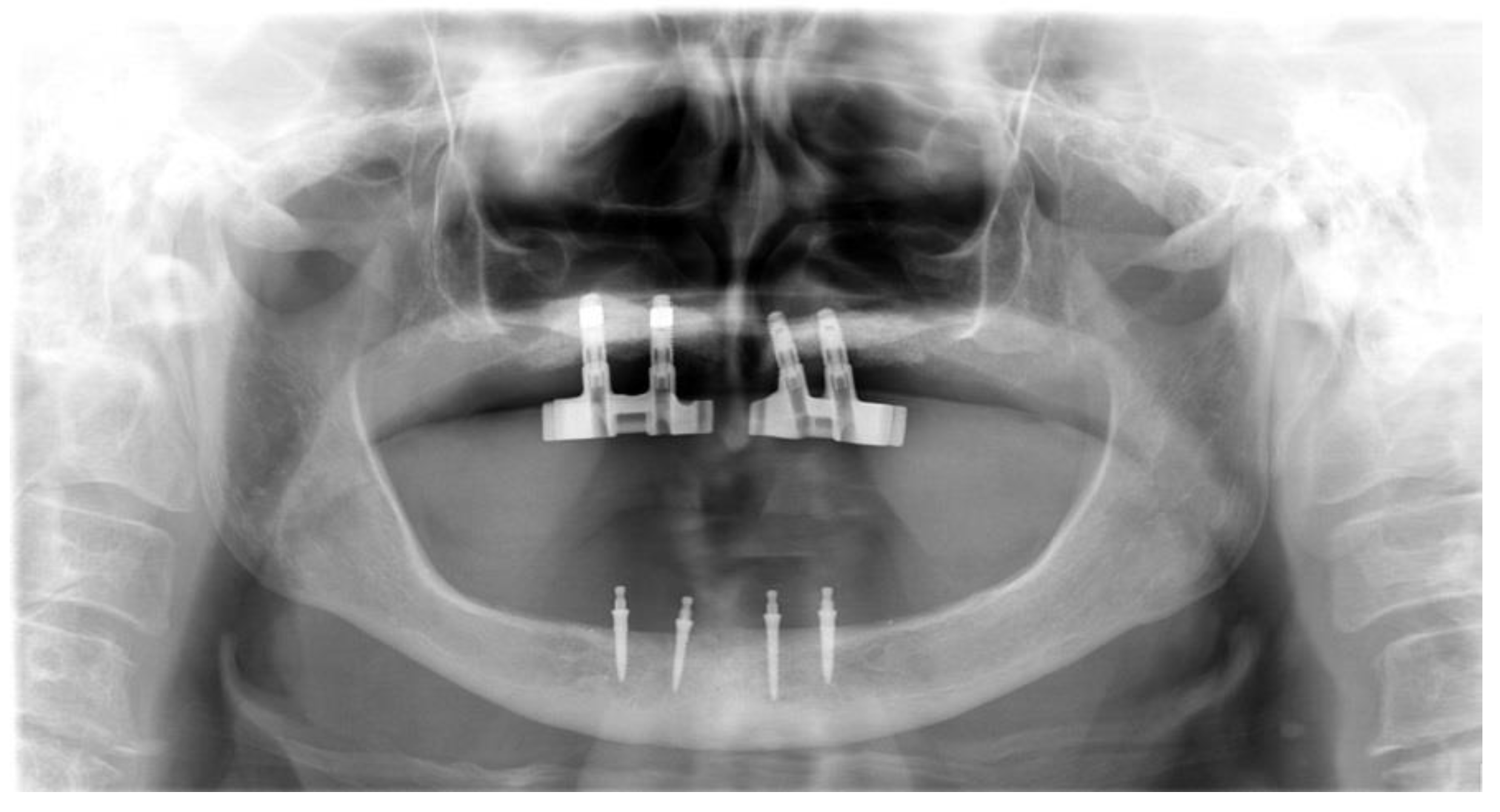
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- AL-Omiri, M.K.; Karasneh, J.A.; Lynch, E.; Lamey, P.J.; Clifford, T.J. Impacts of missing upper anterior teeth on daily living. Int. Dent. J. 2009, 59, 127–132. [Google Scholar] [PubMed]
- Gerritsen, A.E.; Allen, P.F.; Witter, D.J.; Bronkhorst, E.M.; Creugers, N.H. Tooth loss and oral health-related quality of life: A systematic review and meta-analysis. Health Qual. Life Outcomes 2010, 8, 126–137. [Google Scholar] [CrossRef]
- Messias, A.; Nicolau, P.; Guerra, F. Different Interventions for Rehabilitation of the Edentulous Maxilla with Implant-Supported Prostheses: An Overview of Systematic Reviews. Int. J. Prosthodont. 2021, 34, 63–84. [Google Scholar] [CrossRef]
- Aghaloo, T.L.; Misch, C.; Lin, G.H.; Iacono, V.J.; Wang, H.L. Bone Augmentation of the Edentulous Maxilla for Implant Placement: A Systematic Review. Int. J. Oral Maxillofac. Implant. 2016, 31, 19–30. [Google Scholar] [CrossRef]
- Ferri, J.; Dujoncquoy, J.P.; Carneiro, J.M.; Raoul, G. Maxillary reconstruction to enable implant insertion: A retrospective study of 181 patients. Head Face Med. 2008, 4, 31–40. [Google Scholar] [CrossRef] [PubMed]
- Lorean, A.; Mazor, Z.; Barbu, H.; Mijiritsky, E.; Levin, L. Nasal floor elevation combined with dental implant placement: A long-term report of up to 86 months. Int. J. Oral Maxillofac. Implant. 2014, 29, 705–708. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Denche, J.T.; Abbushi, A.; Hernandez, G.; Fernandez-Tresguerres, I.; Lopez-Cabarcos, E.; Tamimi, F. Nasal floor elevation for implant treatment in the atrophic premaxilla: A within-patient comparative study. Clin. Implant Dent. Relat. Res. 2015, 17, 520–530. [Google Scholar] [CrossRef]
- Anitua, E.; Anitua, B.; Alkhraisat, M.H.; Piñas, L.; Eguiad, A. Transalveolar nasal floor elevation and implant placement: Long term follow-up case report and description of the technique. Oral Maxillofac. Surg. Cases 2021, 7, 1–6. [Google Scholar] [CrossRef]
- Mazor, Z.; Lorean, A.; Mijiritsky, E.; Levin, L. Nasal floor elevation combined with dental implant placement. Clin. Implant Dent. Relat. Res. 2012, 14, 768–771. [Google Scholar] [CrossRef]
- Sentineri, R.; Lombardi, T.; Celauro, A.; Stacchi, C. Nasal floor elevation with transcrestal hydrodynamic approach combined with dental implant placement: A case report. Int. J. Periodontics Restor. Dent. 2016, 36, 357–361. [Google Scholar] [CrossRef]
- El-Ghareeb, M.; Pi-Anfruns, J.; Khosousi, M.; Aghaloo, T.; Moy, P. Nasal floor augmentation for the reconstruction of the atrophic maxilla: A case series. J. Oral Maxillofac. Surg. 2012, 70, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Ning, B.; Pei, X. Tantalum and its derivatives in orthopedic and dental implants: Osteogenesis and antibacterial properties. Colloids Surf. B Biointerfaces 2021, 208, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Ore, A.; Gerónimo, D.; Huaman, M.; Calsin, N.; Mendoza, R.; Mayta-Tovalino, F. Uses and applications of tantalum in oral implantology: A literature review. J. Int. Oral Health 2021, 13, 331–335. [Google Scholar]
- Al-Rafee, M.A. The epidemiology of edentulism and the associated factors: A literature Review. J. Fam. Med. Prim. Care 2020, 9, 1841–1843. [Google Scholar] [CrossRef] [PubMed]
- Sharka, R.; Abed, H.; Hector, M. Oral health-related quality of life and satisfaction of edentulous patients using conventional complete dentures and implant-retained overdentures: An umbrella systematic review. Gerodontology 2019, 36, 195–204. [Google Scholar] [CrossRef] [PubMed]
- Mishra, S.K.; Chowdhary, R. Patient’s oral health-related quality of life and satisfaction with implant supported overdentures -a systematic review. J. Oral Biol. Craniofac. Res. 2019, 9, 340–346. [Google Scholar] [CrossRef]
- Torres, Y.; Raoul, G.; Lauwers, L.; Ferri, J. The use of onlay bone grafting for implant restoration in the extremely atrophic anterior maxilla. A case series. Swiss. Dent. J. 2019, 129, 274–285. [Google Scholar]
- Kahnberg, K.E.; Nilsson, P.; Rasmusson, L. Le Fort I osteotomy with interpositional bone grafts and implants for rehabilitation of the severely resorbed maxilla: A 2-stage procedure. Int. J. Oral Maxillofac. Implant. 1999, 14, 571–578. [Google Scholar]
- Batas, L.; Tsalikis, L.; Stavropoulos, A. PRGF as adjunct to DBB in maxillary sinus floor augmentation: Histological results of a pilot split-mouth study. Int. J. Implant Dent. 2019, 5, 1–7. [Google Scholar] [CrossRef]
- Ozçakır Tomruk, C.; Sençift, M.K.; Duygu Capar, G. Prevalence of sinus floor elevation procedures and survival rates of implants placed in the posterior maxilla. Biotechnol. Biotechnol. Equip. 2016, 30, 134–139. [Google Scholar] [CrossRef]
- Fraser, D.; Funkenbusch, P.; Ercoli, C.; Meirelles, L. Biomechanical analysis of the osseointegration of porous tantalum implants. J. Prosthet. Dent. 2020, 123, 811–820. [Google Scholar] [CrossRef] [PubMed]
- Bencharit, S.; Byrd, W.C.; Altarawneh, S.; Hosseini, B.; Leong, A.; Reside, G.; Morelli, T.; Offenbacher, S. Development and applications of porous tantalum trabecular metal-enhanced titanium dental implants. Clin. Implant Dent. Relat. Res. 2014, 16, 817–826. [Google Scholar] [CrossRef] [PubMed]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jordan, A.; Vuletić, M.; Sušić, M.; Stojić, L.; Gabrić, D. Nasal Floor Elevation—An Option of Premaxilla Augmentation: A Case Report. Surgeries 2022, 3, 306-313. https://doi.org/10.3390/surgeries3040033
Jordan A, Vuletić M, Sušić M, Stojić L, Gabrić D. Nasal Floor Elevation—An Option of Premaxilla Augmentation: A Case Report. Surgeries. 2022; 3(4):306-313. https://doi.org/10.3390/surgeries3040033
Chicago/Turabian StyleJordan, Ante, Marko Vuletić, Mato Sušić, Luka Stojić, and Dragana Gabrić. 2022. "Nasal Floor Elevation—An Option of Premaxilla Augmentation: A Case Report" Surgeries 3, no. 4: 306-313. https://doi.org/10.3390/surgeries3040033
APA StyleJordan, A., Vuletić, M., Sušić, M., Stojić, L., & Gabrić, D. (2022). Nasal Floor Elevation—An Option of Premaxilla Augmentation: A Case Report. Surgeries, 3(4), 306-313. https://doi.org/10.3390/surgeries3040033






