Abstract
Background/Objectives: Aging is associated with a progressive decline in biological function due to a complex interplay of physical, psychological, and social factors. This randomized controlled trial aimed to evaluate the effects of a functional health education program on functional capacity in older adults. Methods: Twenty participants (mean age: 80.70 ± 5.992 years) were randomized to either an experimental group that received a 12-week exercise program or a control group. The exercise program included aerobic, flexibility, strength, and cognitive components. Outcomes were assessed using the Timed Up and Go (TUG) test, Falls Efficacy Scale (FES), and Visual Analog Scale (VAS) for pain. Results: In the population studied, 80% of the older adults indicated some type of back pain. The experimental group results showed a significant reduction in back pain (p = 0.032) and risk of falling (p = 0.013). Additionally, the experimental group demonstrated significant improvements in functional capacity (p = 0.016) and cognitive capacity (p = 0.023). Conclusions: This study demonstrated that a specific activity significantly improved participants’ perceived risk of falls, functionality, cognitive function, and reduced back pain complaints in the experimental group.
1. Introduction
Aging is a natural process characterized by the progressive decline of biological components, but it is also a dynamic balance between physical, psychological, and social factors [1].
The aging process is irreversible and leads to various physiological, psychological, and functional changes [2]. As age increases, there is a higher prevalence of multi-pathological conditions, with chronic diseases such as metabolic, vascular, respiratory, oncological, neurological, and musculoskeletal disorders accounting for 80% of mortality in European countries [3].
Physical inactivity is a significant contributor to morbidity and mortality, with an estimated 14% of deaths in Portugal and 10% globally linked to sedentary behavior [4]. The Portuguese Ministry of Health’s National Health Plan 2020 emphasizes increasing life expectancy with quality health for those over 65 years of age by promoting active aging [5]. The goal of active aging is to develop individuals’ ability to maintain autonomy for as long as possible [6,7,8].
To achieve these goals, it is crucial for older adults to adopt healthy lifestyles, which include regular physical activity, healthy eating habits, and abstaining from tobacco and alcohol. Engaging in such practices facilitates the main objective of active aging: enabling individuals to preserve autonomy for as long as possible [9].
Evidence suggests that adults over 65 should engage in at least 150 min of moderate activity or 75 min of vigorous activity per week. For those with chronic conditions or frailty, recommendations suggest 45 min of moderate activity or 20 to 30 min of moderate-to-vigorous interval training [10,11,12].
When planning exercise programs for older adults, several factors should be considered, including cardiorespiratory capacity, strength, flexibility, agility, and coordination. These physical attributes act as predictors of functional capacity and are essential for performing activities of daily living (ADLs). Individual health conditions, such as medication use, risk factors, and personal preferences, must also be taken into account [8,13].
Functional activities that focus on grip strength, flexibility, endurance, balance, alternating loads, neuromotor exercises, and compensatory strategies have proven effective in reducing frailty and preventing falls while enhancing cognitive and psychological capacities [14,15,16,17,18,19].
Considering that more than one-third of older adults experience at least one fall annually, physiotherapy plays a crucial role in improving functionality, maintaining autonomy, and enhancing quality of life [20,21,22].
This study targeted a population with reduced mobility, introducing functional exercises in four key areas: aerobic training, balance training, strength training, and flexibility training. The goal was to provide an effective intervention for this population.
2. Materials and Methods
This study is a pilot, approved by the Australian New Zealand Clinical Trials Registry (ANZCTR) with number ACTRN12617001170314, pre-test and post-test evaluation aimed at assessing the implementation of an exercise protocol for older adults classified as pre-frail according to the Clinical Frailty Scale [23]. The study’s purpose was to verify improvements in balance, fear of falls, and frailty syndrome to increase functional independence. Participants were divided into experimental and control groups in a predictive–causal experimental quantitative approach [24].
Data collection involved a detailed questionnaire administered individually, gathering information on health problems and sociodemographic data.
Assessing older adults is crucial for verifying biopsychosocial components and classifying their physical, functional, and cognitive activity levels. To assess the clinical state of frailty [23], the Visual Analog Scale (VAS) for pain intensity [6,7,8], the Timed Up and Go (TUG) test for functional capacity [25], the Falls Efficacy Scale International (FES-I) for fear of falling [26], and the Mini-Mental State Examination (MMSE) for cognitive function [27].
2.1. Participants, Therapists, Centers
Data were collected from March to July 2018 from older adults in the Viseu region, Portugal, who participated in the Senior Activity program promoted by the Municipality of Viseu.
The sampling plan was non-probabilistic and based on convenience, with inclusion criteria including ages 65–90, participation in the “Senior Activity” program, voluntary consent, and ability to perform walking exercises. Exclusion criteria included recent surgical procedures, intellectual developmental disabilities, and ongoing physical rehabilitation.
2.2. Intervention
After the initial assessment, participants were randomly and conveniently distributed through the distribution of variables carried out by the Excel program into two groups, one control and one experimental. The control group (CG) served as a reference, which allowed us to evaluate whether the treatment carried out in the experimental group had an effect and, therefore, did not participate in the exercise plan. The experimental group (EG) performed a series of functional exercises focusing on the areas of aerobic training, balance, strength, flexibility, and cognitive training, which were introduced in the “Senior Activity” classes.
Functional exercises were applied, targeting flexibility, balance, global motor coordination, and global motor skills. Cognitive training was incorporated through exercises for memorizing sequences, locations, colors, and objects. Functional health education exercises were integrated into the exercise class every two weeks, alternating between two motor and two cognitive exercises. The total duration of the intervention with the EG was 12 consecutive weeks, with evaluations every 4 weeks.
The intervention was divided into three phases:
- Initial questionnaires (T0) and random group allocation.
- Implementation of functional exercises for the EG starting in the second month.
- Reassessment at four-week intervals (T1, T2, and T3) to evaluate the intervention’s effectiveness.
In the first phase, some questionnaires were carried out, and the EG and CG participants were randomly selected. From the 2nd month, in the 2nd phase, the individuals selected for the EG were given functional exercises.
In the end, in the 3rd phase, a reassessment was performed where the data were compared before (T0) and after the 4-week intervention (T1), after the 8-week intervention (T2), and after the 12-week intervention (T3), thus verifying its effectiveness.
2.3. Data Analysis
Ethical approval for the study was obtained from the Piaget Institute Ethics Committee (No. 03/2018), approval date is 15 January 2018, and it adhered to the Declaration of Helsinki principles.
Data were analyzed using IBM SPSS Statistics 26.0, with results compared across evaluation time points using the Mann–Whitney U non-parametric test after carrying out the homogeneity test, where it was verified that the sample does not follow a homogeneous distribution. A significance level of 0.05 was adopted for all analyses [28].
3. Results
A total of 20 older adults, aged between 67 and 90 years (mean age: 80.70 ± 5.992), were randomly assigned to the experimental group (EG, n = 10) and control group (CG, n = 10) [Figure 1]. The sample was predominantly female (78.9%), with 21.1% male participants. The majority were widowed (52.6%) and lacked basic education (63.2%).
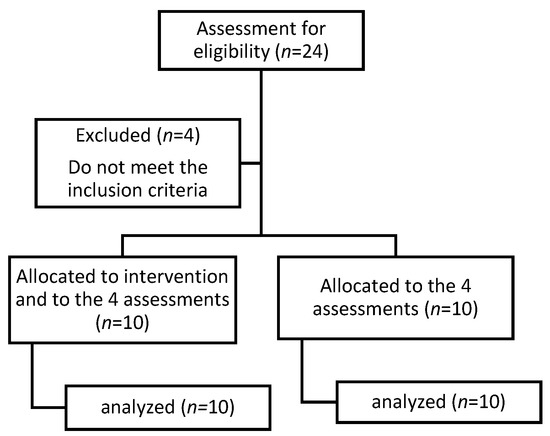
Figure 1.
Flowchart for the randomized controlled trial.
In the study, 80% of the population reported some form of back pain, of which 50% was chronic, with 81.2% localized in the lumbar region. At baseline, the mean pain level, assessed using the Visual Analog Scale (VAS), was 5.70 ± 3.672, with the EG reporting a mean of 7.10 ± 3.695 and the CG reporting 4.30 ± 3.234. First reassessment (4 weeks): The EG reported a mean of 5.00 ± 3.091 (p = 0.051), while the CG reported 3.20 ± 2.530 (p = 0.149). Third assessment (8 weeks): The EG reported 4.00 ± 1.944 (p = 0.022), and the CG reported 2.70 ± 2.11 (p = 0.217). Fourth assessment (12 weeks): A significant reduction in back pain was observed in the EG, with a mean of 3.88 ± 2.232 (p = 0.032), while the CG showed a mean of 3.70 ± 1.889 (p = 0.529) [Table 1].

Table 1.
Mean back pain scores (VAS) between groups across all phases of evaluation.
Functional performance was assessed using the Timed Up and Go (TUG) test: EG baseline: Mean time of 21.10 ± 10.064 s (minimum: 13.94; maximum: 48.88), indicating significant difficulties in mobility and dynamic balance during activities of daily living (ADLs). CG baseline: Mean time of 18.38 ± 4.492 s (minimum: 14.01; maximum: 27.33), suggesting a functional condition consistent with frail older adults with impaired dynamic balance. First reassessment (4 weeks): The EG achieved a mean of 17.05 ± 6.483 (p = 0.174), and the CG recorded 16.94 ± 3.434 (p = 0.496). Third assessment (8 weeks): The EG reported 18.31 ± 9.143 (p = 0.326), while the CG showed 17.07 ± 4.144 (p = 0.597). Fourth assessment (12 weeks): The EG demonstrated significant improvements in functional capacity, with a mean of 14.18 ± 4.797 (p = 0.016), while the CG showed 17.33 ± 6.655 (p = 0.406) [Table 2].

Table 2.
Analysis of the difference between the assessment phases in relation to functionality by group.
Regarding the program in the assessment of cognitive function, according to the Mini-Mental State Examination (MMSE) scale, it allowed us to have an idea of the cognitive function of our sample; having 55% of illiterate individuals, MMSE values greater than 15 means that there is no cognitive deficit. Baseline: Overall mean of 21.00 ± 3.866 with a minimum value of 12 and a maximum of 27. The EG obtained the initial average of 20.10 ± 4.149, and the CG reported 21.90 ± 3.542. First reassessment: the EG reported an average of 22.10 ± 4.306 (p = 0.223); in the case of the CG, at the same time, they had an average of 23.40 ± 4.351 (p = 0.361). Third assessment: the EG had an average of 23.50 ± 3.837 (p = 0.057), in the CG, the average was 23.20 ± 4.442 (p = 0.569). Fourth assessment (12 weeks): the EG showed improvements in functional capacity with an average of 24.88 ± 3.227 (p = 0.023), and the control group also increased to 21.70 ± 3.802 (p = 0.820) [Table 3].

Table 3.
Analysis of MMSE averages by group.
The Falls Efficacy Scale (FES) revealed the following outcomes. Baseline: Overall mean of 58.35 ± 20.531, with a minimum of 32 and a maximum of 100. The EG reported 49.50 ± 18.934, while the CG reported 67.20 ± 18.902, which means that in the control group, there is greater self-confidence and less risk of falling. With the introduction of exercises, the first reassessment: the EG had an average of 55.60 ± 19.357 (p = 0.342), and the CG had an average of 70.80 ± 23.593 (p = 0.579). Third assessment: EG had an average of 62.43 ± 19.156 (p = 0.158); in the CG, the average was 72.50 ± 25.176 (p = 0.850). Fourth assessment (12 weeks): EG showed a significant increase in self-efficacy, with a mean of 77.75 ± 14.964 (p = 0.013). The CG showed a mean of 73.90 ± 27.851, with no significant differences between the first and the last evaluation moments (p = 0.705) [Table 4].

Table 4.
Analysis of the difference between the assessment phases in relation to the risk of falls by group.
The experimental group demonstrated statistically significant improvements over the 12 weeks in reduction in lumbar pain (p = 0.032); improved functional performance (p = 0.016); enhanced cognitive function (p = 0.023); increased self-efficacy and reduced fall risk (p = 0.013) [Figure 2].
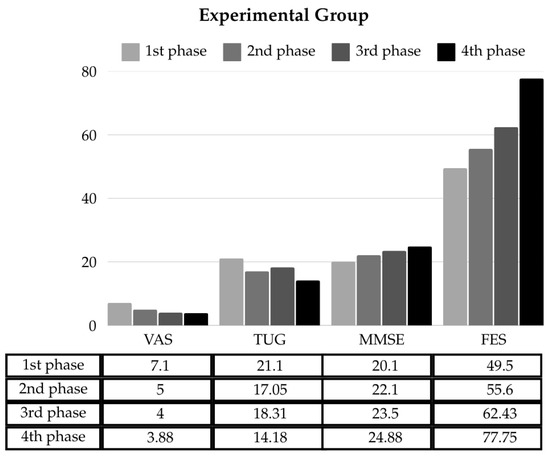
Figure 2.
Analysis of the difference between the assessment phases in relation to the average of pain (VAS), functionality (TUG), cognitive function (MMSE), and risk of falls (FES) in the experimental group.
These results allow for analysis and comparison with the existing bibliography.
4. Discussion
The evidence highlights numerous studies on interventions for frail older adults; however, correlating these studies remains challenging due to the dispersed methods of assessing frailty, as each investigator employs different assessment mechanisms [29].
In the present study, overall, our sample showed slight improvements, but only the experimental group presented statistically significant improvements, which aligns with numerous studies that emphasize the benefits of physical exercise for older adults [10,30].
The implementation of effective strategies to reduce falls in the elderly population has become a global challenge, given the continuous aging process [24].
In this regard, the authors state that falls are the main cause of hospitalization in older adults, highlighting the importance of physical exercise in recovering and maintaining functional capacity, as well as preserving physical and mental abilities. This approach aims to reduce limitations and promote the maintenance of independence and autonomy in this population.
Despite the global improvements observed, the introduction of the functional health education program in the experimental group resulted in a significant reduction in lower back pain (p = 0.032), improved self-confidence regarding the risk of falling (p = 0.013), enhanced functional capacity (p = 0.016), and better cognitive function (p = 0.023). In the control group, improvements in the means were also observed, although they did not reach statistical significance. Once again, these findings are consistent with the literature, which recommends physical exercise as an effective means of relieving pain symptoms. The implemented program led to significant improvements by incorporating global exercises that promote greater body awareness [31].
The implementation of balance-challenging exercises proves promising in reducing the risk of falls, and fostering adaptive abilities and strategies to respond to changes in stability points. This enhances independence related to functional capacity, demonstrating that a specific exercise program can offer sufficient benefits to reverse or reduce frailty syndrome, maximize the functional capacity of older adults, and improve their independence in activities of daily living [29,32].
Study Limitation
Although numerous interventions have been developed to improve the outcomes of frail older adults’ people, a major obstacle encountered is the difficulty of comparing inter-studies due to differences in the diagnosis of frailty.
The fact that the sample distribution was not homogeneous requires a careful analysis of the data presented.
The study was carried out randomly and for convenience, and the places where the collections and interventions with the elderly were carried out were defined by the “Senior Activity” program of the municipal council of Viseu, which generated a major limitation on access to participants and the consequent small number of participants.
This limitation, the small sample size due to the low availability of elderly care centers in the region, which prevents extrapolation of the results.
5. Conclusions
In view of the progressive aging of the population, which occurs mainly in developed countries, current societies have a new concern and a new way of facing aging and older adults. This fact is confirmed by the introduction of a new concept, active aging, aiming for older adults to age actively, independently, and successfully.
The present study proved that the application of a specific activity, in the functional components allowed, in the experimental group, improvements in the self-perception of risk of falling, functionality, cognitive function, and decreased back pain complaints, with all factors showing statistically significant differences. These data should be interpreted with caution, given the small sample size. Nevertheless, the findings warrant further investigation in larger studies.
Funding
This research received no external funding.
Institutional Review Board Statement
All data collection was authorized by the participant through a consent form and all procedures in this project is in line with national and international guidelines for scientific research involving human subjects and including the Declaration of Helsinki in 2013 on Ethical Principles for Medical Research Involving Human Subjects, and the 1997 Convention on Human Rights and Biomedicine (the “Oviedo Convention”). The study was conducted in accordance with the Declaration of Helsinki, and the study is approved by Piaget Institute Ethics Committee (No. 03/2018), on 15 January 2018.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the author.
Acknowledgments
The author would like to thank those responsible for the senior activity program of the Municipal Council of Viseu, as well as the local promoters and day centres participating in this study and the participants of it, without them it would not be possible to achieve this. The author would also like to thank the collaboration of students Cristina Farias and Ana Rita Mesquita for their support in data collection.
Conflicts of Interest
The author declares no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| ANZCTR | Australian New Zeeland Clinical Trial |
| VAS | Visual Analog Scale |
| TUG | Timed up and Go |
| FES | Falls Efficacy Scale International |
| MMSE | Mini Mental State Examination |
| CG | control group |
| EG | experimental group |
References
- Christensen, U.; Støvring, N.; Schultz-Larsen, K.; Schroll, M.; Avlund, K. Functional ability at age 75: Is there an impact of physical inactivity from middle age to early old age? Scand. J. Med. Sci. Sports 2006, 16, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Sherrington, C.; Tiedemann, A. Physiotherapy in the prevention of falls in older people. J. Physiother. 2015, 61, 54–60. [Google Scholar] [CrossRef]
- DGS M da S. Estratégia Nacional para a Qualidade na Saúde. DGS. 2015. Available online: https://diariodarepublica.pt/dr/detalhe/despacho/5613-2015-67324029 (accessed on 26 December 2024).
- WHO. Physical Activity and Older Adults; WHO: Geneva, Switzerland, 2011; pp. 1–58. [Google Scholar]
- Nunes, A.M. A Recuperação Do Serviço Nacional De Saúde Português: Novas Perspectivas Para A Política De Saúde. Rev. Gestão Sist. Saúde 2018, 7, 16–28. [Google Scholar] [CrossRef]
- Desouzart, G.; Matos, R.; Melo, F.; Filgueiras, E. Effects of sleeping position on back pain in physically active seniors: A controlled pilot study. Work 2016, 53, 235–240. [Google Scholar] [CrossRef] [PubMed]
- Taylor, A.H.; Cable, N.T.; Faulkner, G.; Hillsdon, M.; Narici, M.; Van Der Bij, A.K. Physical activity and older adults: A review of health benefits and the effectiveness of interventions. J. Sports Sci. 2004, 22, 703–725. [Google Scholar] [CrossRef]
- Tribess, S.; Virtuoso, J.S., Jr. Prescription of physical exercises for elderly. Rev. Saude Com 2005, 1, 163–172. [Google Scholar]
- Maciel, M.G. Atividade física e funcionalidade do idoso. Mot. Rev. Educ. Física 2010, 16, 1024–1032. [Google Scholar] [CrossRef]
- American College of Sports Medicine. ACSM’s Exercise Testing and Prescription; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2017. [Google Scholar]
- Theou, O.; Stathokostas, L.; Roland, K.P.; Jakobi, J.M.; Patterson, C.; Vandervoort, A.A.; Jones, G.R. The effectiveness of exercise interventions for the management of frailty: A systematic review. J. Aging Res. 2011, 2011, 569194. [Google Scholar] [CrossRef]
- Trudelle-Jackson, E.; Jackson, A.W. Do older adults who meet 2008 Physical Activity Guidelines have better physical performance than those who do not meet? J. Geriatr. Phys. Ther. 2018, 41, 180–185. [Google Scholar] [CrossRef]
- Shubert, T.E. Evidence-based exercise prescription for balance and falls prevention: A current review of the literature. J. Geriatr. Phys. Ther. 2011, 34, 100–108. [Google Scholar] [CrossRef]
- Serra-Rexach, J.A.; Bustamante-Ara, N.; Hierro, V.M.; González Gil, P.; Sanz Ibáñez, M.J.; Blanco Sanz, N.; Ortega Santamaría, V.; Gutiérrez Sanz, N.; Marín Prada, A.B.; Gallardo, C.; et al. Short-term, light-to moderate-intensity exercise training improves leg muscle strength in the oldest old: A randomized controlled trial. J. Am. Geriatr. Soc. 2011, 59, 594–602. [Google Scholar] [CrossRef]
- Tsai, J.C.; Chan, P.; Wang, C.-H.; Jeng, C.; Hsieh, M.H.; Kao, P.F.; Chen, Y.J.; Liu, J.C. The effects of exercise training on walking function and perception of health status in elderly patients with peripheral arterial occlusive disease. J. Intern. Med. 2002, 252, 448–455. [Google Scholar] [CrossRef] [PubMed]
- Windle, G.; Hughes, D.; Linck, P.; Russell, I.; Woods, B. Is exercise effective in promoting mental well-being in older age? A systematic review. Aging Ment. Health 2010, 14, 652–669. [Google Scholar] [CrossRef] [PubMed]
- Piovesan, A.C.; Pivetta, H.M.F.; Peixoto., J.M.d.B. Fatores que predispõem a quedas em idosos residentes na região oeste de Santa Maria, RS. Rev. Bras. Geriatr. E Gerontol. 2011, 14, 75–83. [Google Scholar] [CrossRef]
- WHO. A Policy Framework. Em: Active Aging; World Health Organization: Geneva, Switzerland, 2002. [Google Scholar]
- Duarte de Queiroz Brito, T.; de Oliveira, A.R.; do Carmo Eulálio, M. Disability and Aging: Study of Social Representations of the Elderly from Physical Therapy Rehabilitation. Av. Psicol. Latinoam. 2015, 33, 121–133. [Google Scholar]
- Gschwind, Y.J.; Kressig, R.W.; Lacroix, A.; Muehlbauer, T.; Pfenninger, B.; Granacher, U. A best practice fall prevention exercise program to improve balance, strength/power, and psychosocial health in older adults: Study protocol for a randomized controlled trial. BMC Geriatr. 2013, 13, 105. [Google Scholar] [CrossRef] [PubMed]
- Dutra, M.O.M.; Coura, A.S.; de França, I.S.X.; Enders, B.C.; Rocha, M.A. Sociodemographic factors and functional capacity of elderly affected by stroke. Rev. Bras. Epidemiol. 2017, 20, 124–135. [Google Scholar] [CrossRef]
- Costa, L.O.P.; Maher, C.G.; Latimer, J.; Hodges, P.W.; Herbert, R.D.; Refshauge, K.M.; McAuley, J.H.; Jennings, M.D. Motor control exercise for chronic low back pain: A randomized placebo-controlled trial. Phys. Ther. 2009, 89, 1275–1286. [Google Scholar] [CrossRef]
- Rockwood, K. What would make a definition of frailty successful? Age Ageing 2005, 34, 432–434. [Google Scholar] [CrossRef]
- Nakagawa, K.; Inomata, N.; Nakazawa, R.; Sakamoto, M. The effect of a health promotion program consisting of easy and simple exercises for community living elderly people. J. Phys. Ther. Sci. 2007, 19, 235–242. [Google Scholar] [CrossRef][Green Version]
- Nunciato, A.C.; Pereira, B.C.; Borghi-Silva, A. Métodos de avaliação da capacidade física e qualidade de vida em idosos: Revisão de literatura. Saúde Rev. 2012, 12, 41–48. [Google Scholar] [CrossRef]
- Camargos, F.F.O.; Dias, R.C.; Dias, J.; Freire, M.T.F. Cross-cultural adaptation and evaluation of the psychometric properties of the Falls Efficacy Scale-International Among Elderly Brazilians (FES-I-BRAZIL). Braz. J. Phys Ther. 2010, 14, 237–243. [Google Scholar] [CrossRef]
- Santana, I.; Duro, D.; Lemos, R.; Costa, V.; Pereira, M.; Simões, M.R.; Freitas, S. Mini-Mental State Examination: Avaliação dos Novos Dados Normativos no Rastreio e Diagnóstico do Défice Cognitivo. Acta Med. Port. 2016, 29, 240–248. Available online: https://www.actamedicaportuguesa.com/revista/index.php/amp/article/view/6889 (accessed on 26 December 2024). [CrossRef] [PubMed]
- Maroco, J. Análise Estatística com o SPSS Statistics, 7th ed.; ReportNumber: Lisboa, Portugal, 2018. [Google Scholar]
- de Labra, C.; Guimaraes-Pinheiro, C.; Maseda, A.; Lorenzo, T.; Millán-Calenti, J.C. Effects of physical exercise interventions in frail older adults: A systematic review of randomized controlled trials. BMC Geriatr. 2015, 15, 154. [Google Scholar] [CrossRef] [PubMed]
- Petry, N.M.; Andrade, L.F.; Barry, D.; Byrne, S. A randomized study of reinforcing ambulatory exercise in older adults. Psychol. Aging 2013, 28, 1164. [Google Scholar] [CrossRef] [PubMed]
- Castro, D.C.; Nunes, D.P.; Pagotto, V.; Pereira, L.V.; Bachion, M.M.; Nakatani, A.Y.K. Incapacidade funcional para atividades básicas de vida diária de idosos: Estudo populacional/Functional disability for basic activities of daily lives of the elderly: A population study. Ciência Cuid. E Saúde 2016, 15, 109–117. [Google Scholar] [CrossRef]
- Siegrist, M.; Freiberger, E.; Geilhof, B.; Salb, J.; Hentschke, C.; Landendoerfer, P.; Linde, K.; Halle, M.; Blank, W.A. Fall prevention in a primary care setting: The effects of a targeted complex exercise intervention in a cluster randomized trial. Dtsch. Ärzteblatt Int. 2016, 113, 365. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).