Association Between Bone Mineral Density Around the Stem, Morphology of the Proximal Femur, and Effects of Osteoporosis Treatment in Patients with Femoral Neck Fracture
Abstract
1. Introduction
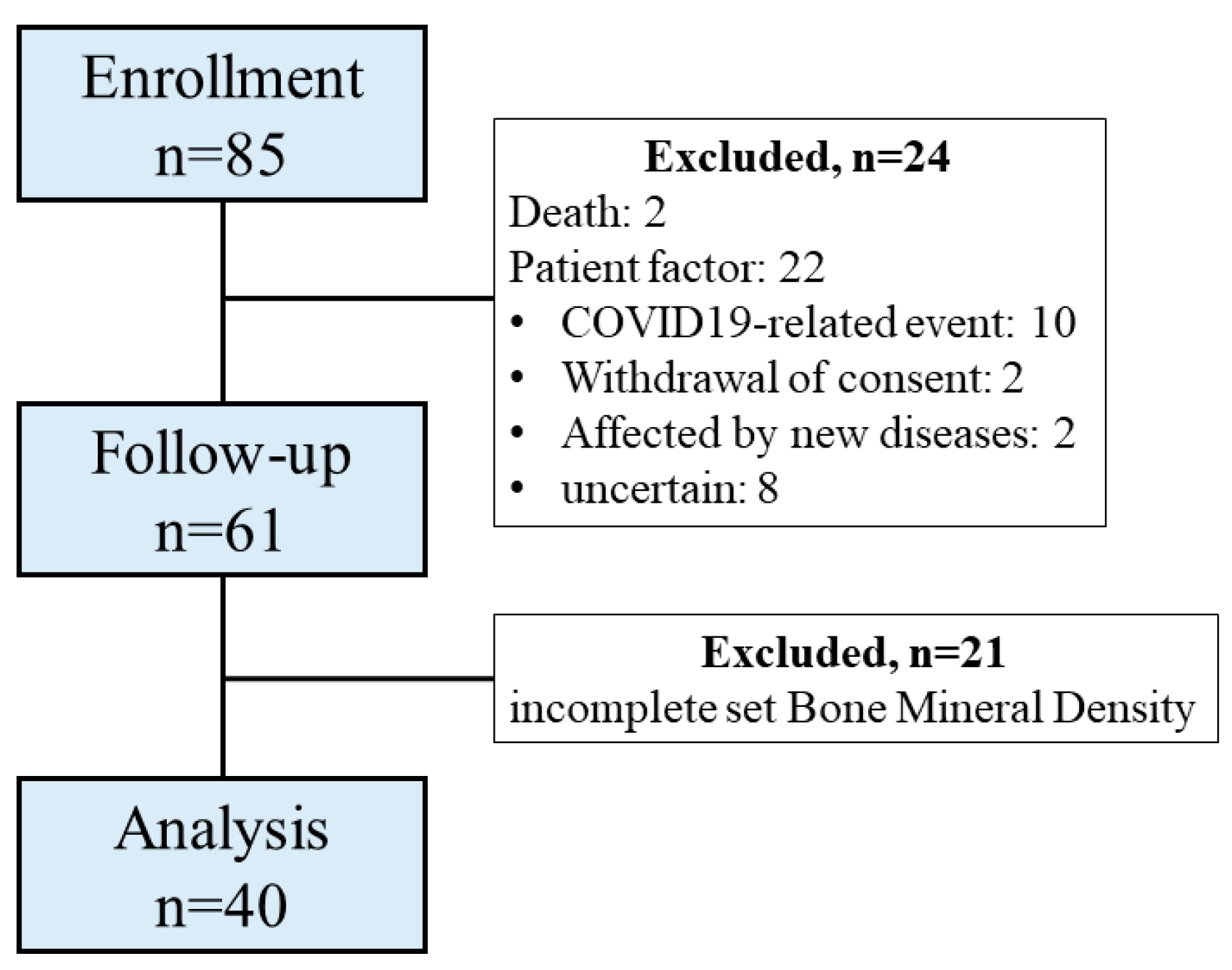
2. Materials and Methods
2.1. Study Design
2.2. Sample Size Estimation
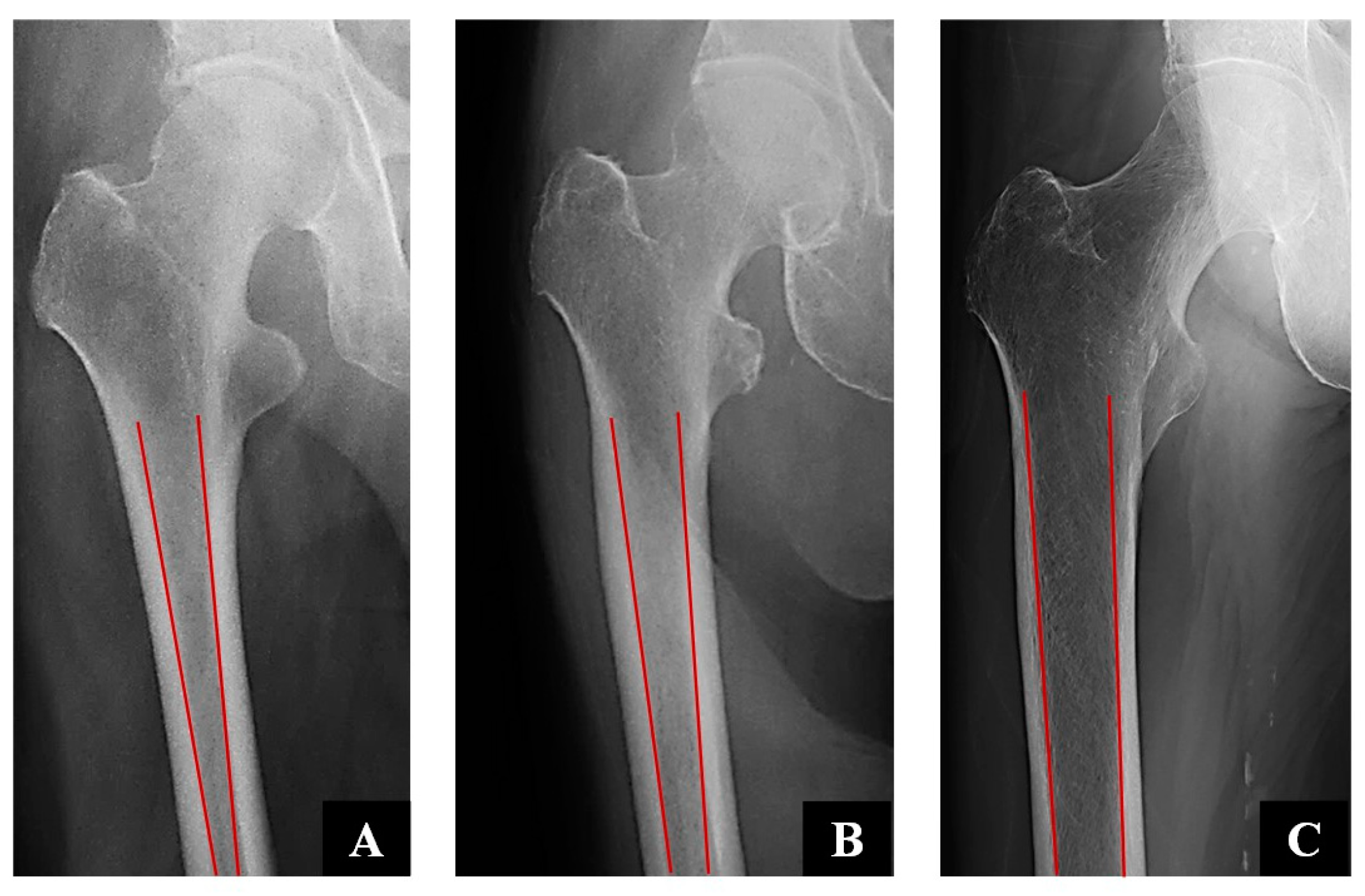
2.3. Clinical and Radiographical Assessment
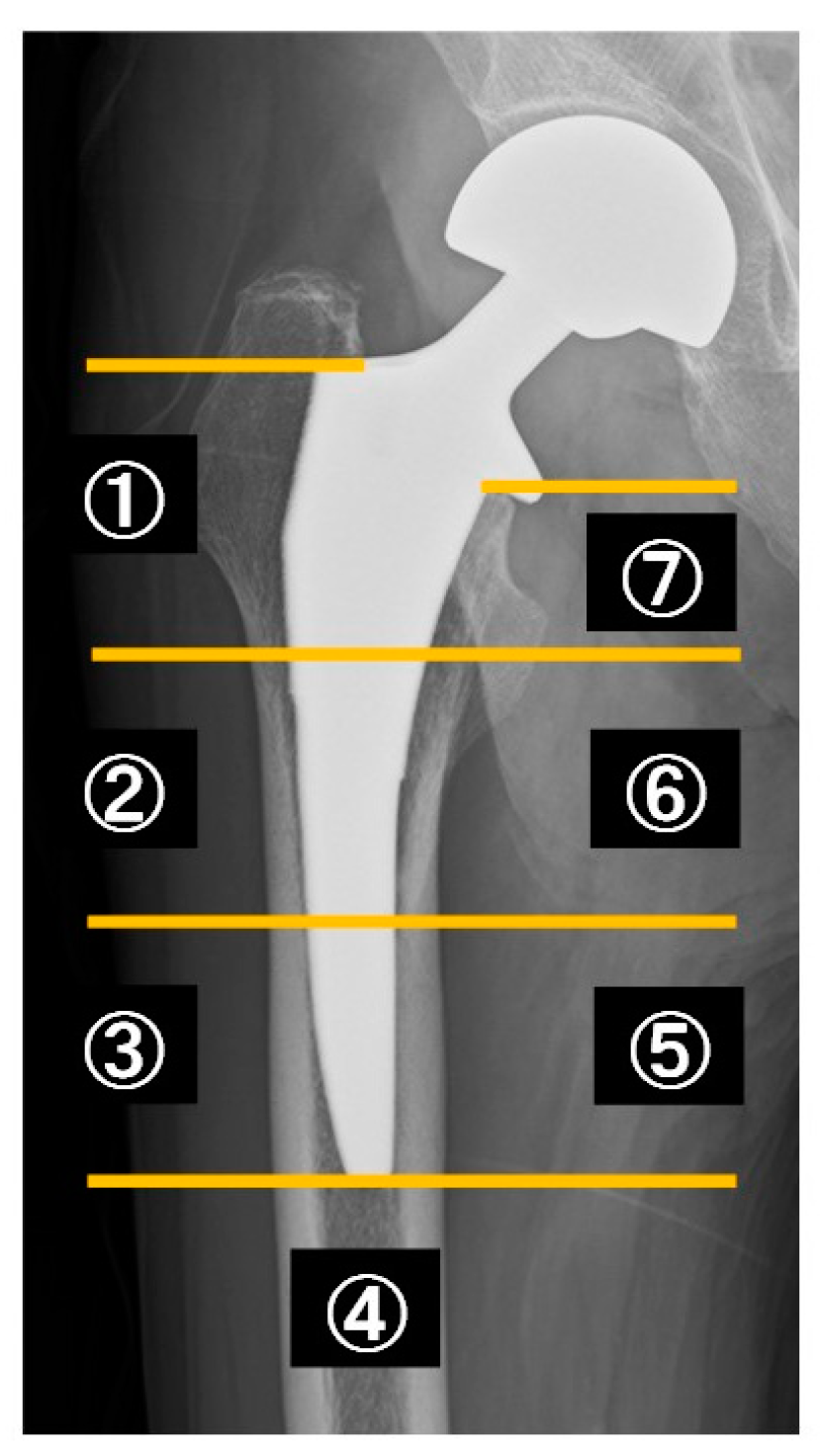
2.4. DEXA Measurements
2.5. Osteoporosis Treatment
2.6. Statistical Analysis
2.7. Ethical Statement
3. Results
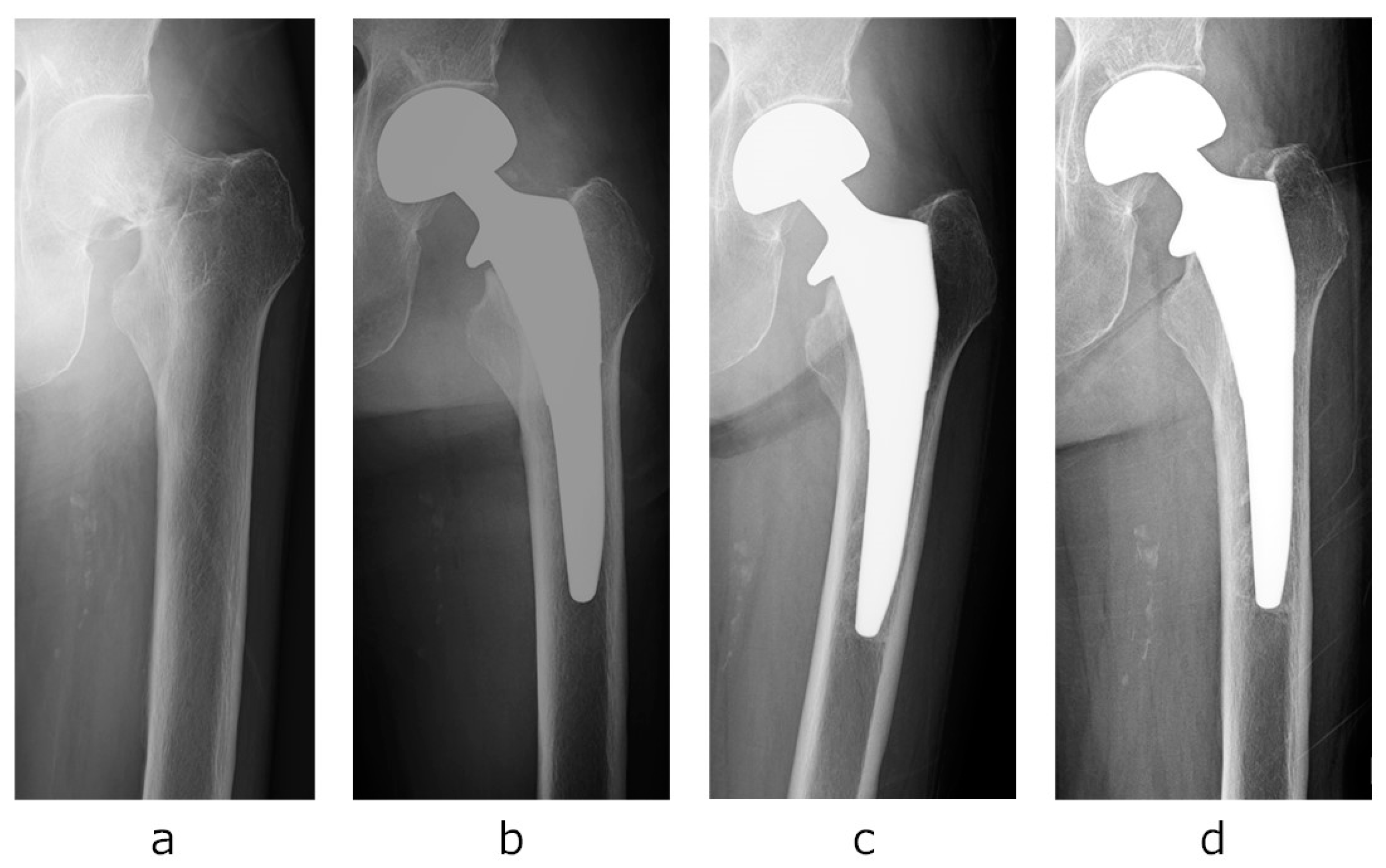
- Case presentation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BHA | Bipolar hip arthroplasty |
| BMD | Bone mineral density |
| BMI | Body mass index |
| DEXA | Dual-energy X-ray absorptiometry |
| EQ5D-5L | EuroQoL 5-Dimension 5-Level |
| HHS | Harris Hip Score |
| ROI | Region of interest |
| THA | Total hip arthroplasty |
| SERM | Selective estrogen receptor modulator |
References
- Vidovic, D.; Matejcic, A.; Punda, M.; Ivica, M.; Tomljenovic, M.; Bekavac-Beslin, M.; Mijic, A.; Bakota, B. Periprosthetic bone loss following hemiarthroplasty: A comparison between cemented and cementless hip prosthesis. Injury 2013, 44, S62–S66. [Google Scholar] [CrossRef]
- Burgers, P.T.P.W.; Van Geene, A.R.; Van Den Bekerom, M.P.J.; Van Lieshout, E.M.M.; Blom, B.; Aleem, I.S.; Bhandari, M.; Poolman, R.W. Total hip arthroplasty versus hemiarthroplasty for displaced femoral neck fractures in the healthy elderly: A meta-analysis and systematic review of randomized trials. Int. Orthop. 2012, 36, 1549–1560. [Google Scholar] [CrossRef] [PubMed]
- Bhandari, M.; Devereaux, P.; TornettaIII, P.; Swiontkowski, M.F.; Berry, D.J.; Haidukewych, G.; Schemitsch, E.H.; Hanson, B.P.; Koval, K.; Dirschl, D.; et al. Operative management of displaced femoral neck fractures in elderly patients. J. Bone Jt. Surg. 2005, 87, 2122–2130. [Google Scholar] [CrossRef] [PubMed]
- Iwamoto, Y.; Kijima, H.; Tazawa, H.; Konishi, N.; Kubota, H.; Yamada, S.; Tani, T.; Kamo, K.; Suzuki, N.; Okudera, Y.; et al. Initial rotational instability of the tapered wedge-shaped type cementless stem. Adv. Orthop. 2020, 2020, 2180260. [Google Scholar] [CrossRef]
- Fujii, M.; Kitamura, K.; Ikemura, S.; Hamai, S.; Motomura, G.; Nakashima, Y. Pneumatic femoral broaching decreases post-operative subsidence of a cementless taper-wedge stem. Int. Orthop. 2022, 46, 233–240. [Google Scholar] [CrossRef] [PubMed]
- Leiss, F.; Goetz, J.S.; Schindler, M.; Reinhard, J.; Müller, K.; Grifka, J.; Greimel, F.; Meyer, M. Influence of bone mineral density on femoral stem subsidence after cementless THA. Arch. Orthop. Trauma Surg. 2024, 144, 451–458. [Google Scholar] [CrossRef]
- Bunyoz, K.I.; Malchau, E.; Malchau, H.; Troelsen, A. Has the use of fixation techniques in THA changed in this decade? The uncemented paradox revisited. Clin. Orthop. Relat. Res. 2020, 478, 697–704. [Google Scholar] [CrossRef]
- Springer, B.D.; Etkin, C.D.; Shores, P.B.; Gioe, T.J.; Lewallen, D.G.; Bozic, K.J. Perioperative periprosthetic femur fractures are strongly correlated with fixation method: An analysis from the american joint replacement registry. J. Arthroplast. 2019, 34, S352–S354. [Google Scholar] [CrossRef]
- Veldman, H.D.; Heyligers, I.C.; Grimm, B.; Boymans, T.A.E.J. Cemented versus cementless hemiarthroplasty for a displaced fracture of the femoral neck: A systematic review and meta-analysis of current generation hip stems. Bone Jt. J. 2017, 99-B, 421–431. [Google Scholar] [CrossRef]
- Ekman, E.; Laaksonen, I.; Isotalo, K.; Liukas, A.; Vahlberg, T.; Mäkelä, K. Cementing does not increase the immediate postoperative risk of death after total hip arthroplasty or hemiarthroplasty: A hospital-based study of 10,677 patients. Acta Orthop. 2019, 90, 270–274. [Google Scholar] [CrossRef]
- Hayashi, S.; Hashimoto, S.; Kuroda, Y.; Nakano, N.; Matsumoto, T.; Kamenaga, T.; Niikura, T.; Kuroda, R. Hydroxyapatite-coated compaction short stem represents a characteristic pattern of peri-prosthetic bone remodelling after total hip arthroplasty. Arch. Orthop. Trauma Surg. 2022, 142, 2903–2910. [Google Scholar] [CrossRef] [PubMed]
- Kaszuba, S.V.; Cipparrone, N.; Gordon, A.C. The Actis and Corail femoral stems provide for similar clinical and radiographic outcomes in total hip arthroplasty. HSS J. 2020, 16, 412–419. [Google Scholar] [CrossRef] [PubMed]
- Chitnis, A.S.; Mantel, J.; Ruppenkamp, J.; Bourcet, A.; Holy, C.E. Survival analysis for all-cause revision following primary total hip arthroplasty with a medial collared, triple-tapered primary hip stem versus other implants in real-world settings. Curr. Med. Res. Opin. 2020, 36, 1839–1845. [Google Scholar] [CrossRef] [PubMed]
- Hatano, M.; Koizumi, Y.; Yamamoto, N.; Miyoshi, K.; Kawabata, K.; Tanaka, T.; Tanaka, S.; Shiroshita, A.; Kataoka, Y. Anti-osteoporotic drug efficacy for periprosthetic bone loss after total hip arthroplasty: A systematic review and network meta-analysis. J. Orthop. Sci. 2025, 30, 126–135. [Google Scholar] [CrossRef]
- Chen, X.; Shen, Y.; Ye, C.; Mumingjiang, Y.; Lu, J.; Yu, Y. Prophylactic efficacy on periprosthetic bone loss in calcar region after total hip arthroplasty of antiosteoporotic drugs: A network meta-analysis of randomised controlled studies. Postgrad. Med. J. 2021, 97, 150–155. [Google Scholar] [CrossRef]
- Arabmotlagh, M.; Rittmeister, M.; Hennigs, T. Alendronate prevents femoral periprosthetic bone loss following total hip arthroplasty: Prospective randomized double-blind study. J. Orthop. Res. 2006, 24, 1336–1341. [Google Scholar] [CrossRef]
- Zeng, Y.; Lai, O.; Shen, B.; Yang, J.; Zhou, Z.; Kang, P.; Pei, F. A systematic review assessing the effectiveness of alendronate in reducing periprosthetic bone loss after cementless primary THA. Orthopedics 2011, 34. [Google Scholar] [CrossRef]
- Dorr, L.D.; Faugere, M.-C.; Mackel, A.M.; Gruen, T.A.; Bognar, B.; Malluche, H.H. Structural and cellular assessment of bone quality of proximal femur. Bone 1993, 14, 231–242. [Google Scholar] [CrossRef]
- Söderman, P.; Malchau, H. Is the Harris hip score system useful to study the outcome of total hip replacement? Clin. Orthop. Relat. Res. 2001, 384, 189–197. [Google Scholar] [CrossRef]
- Shiroiwa, T.; Ikeda, S.; Noto, S.; Igarashi, A.; Fukuda, T.; Saito, S.; Shimozuma, K. Comparison of value set based on DCE and/or TTO data: Scoring for EQ-5D-5L health states in Japan. Value Health 2016, 19, 648–654. [Google Scholar] [CrossRef]
- Greene, M.E.; Rader, K.A.; Garellick, G.; Malchau, H.; Freiberg, A.A.; Rolfson, O. The EQ-5D-5L improves on the EQ-5D-3L for health-related quality-of-life assessment in patients undergoing total hip arthroplasty. Clin. Orthop. Relat. Res. 2015, 473, 3383–3390. [Google Scholar] [CrossRef]
- Gruen, T.A.; McNeice, G.M.; Amstutz, H.C. “Modes of failure” of cemented stem-type femoral components: A radiographic analysis of loosening. Clin. Orthop. Relat. Res. 1979, 141, 17–27. [Google Scholar] [CrossRef]
- Kilgus, D.; Shimaoka, E.; Tipton, J.; Eberle, R. Dual-energy X-Ray absorptiometry measurement of bone mineral density around porous-coated cementless femoral implants. Methods and preliminary results. J. Bone Jt. Surgery. Br. Vol. 1993, 75-B, 279–287. [Google Scholar] [CrossRef] [PubMed]
- Kröger, H.; Miettinen, H.; Arnala, I.; Koski, E.; Rushton, N.; Suomalainen, O. Evaluation of periprosthetic bone using dual-energy X-ray absorptiometry: Precision of the method and effect of operation on bone mineral density. J. Bone Miner. Res. 1996, 11, 1526–1530. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, S.; Nishiyama, T.; Fujishiro, T.; Kanzaki, N.; Hashimoto, S.; Kurosaka, M. Periprosthetic bone mineral density with a cementless triple tapered stem is dependent on daily activity. Int. Orthop. 2012, 36, 1137–1142. [Google Scholar] [CrossRef]
- Murat, M.; Ermutlu, C.; Unkar, E.A.; Topalhafızoglu, S.; Şenel, A.; Öztürkmen, Y. Bone loss following cementless hemiarthroplasty for the treatment of femoral neck fracture. Indian J. Orthop. 2020, 54, 454–462. [Google Scholar] [CrossRef]
- Damborg, F.; Nissen, N.; I Jørgensen, H.R.; Abrahamsen, B.; Brixen, K. Changes in bone mineral density (BMD) around the cemented Exeter stem: A prospective study in 18 women with 5 years follow-up. Acta Orthop. 2008, 79, 494–498. [Google Scholar] [CrossRef]

| Stem Size | Number |
|---|---|
| 1 | 1 |
| 2 | 3 |
| 3 | 9 |
| 4 | 8 |
| 5 | 8 |
| 6 | 7 |
| 7 | 3 |
| 8 | 1 |
| Dorr A | Dorr B | Dorr C | p Value | X2 Value | ||
|---|---|---|---|---|---|---|
| Number of Patients | 6 | 24 | 10 | - | - | |
| Female, n (%) | 3 (50%) | 16 (66.7%) | 9 (90%) | 0.204 | 3.175 | |
| Age (years) | 81.8 ± 4.5 | 80.0 ± 6.6 | 80.1 ± 7.3 | 0.173 | - | |
| BMI (kg/m2) | 21.9 ± 3.1 | 20.8 ± 2.7 | 19.9 ± 1.8 | 0.338 | - | |
| HHS (points) | 93.5 ± 6.0 | 81.9 ± 15.6 | 75.9 ± 19.0 | 0.087 | - | |
| EQ-5D-5L (score) | 0.88 ± 0.11 | 0.76 ± 0.21 | 0.75 ± 0.18 | 0.287 | - | |
| Zone area | Time | BMD change rate | ||||
| Zone 1 | 6 m | 0.90 ± 0.09 | 0.89 ± 0.11 | 0.88 ± 0.12 | 0.218 | - |
| 12 m | 0.86 ± 0.12 | 0.86 ± 0.15 | 0.85 ± 0.13 | 0.943 | - | |
| Zone 2 | 6 m | 0.91 ± 0.05 | 0.90 ± 0.12 | 0.83 ± 0.15 | 0.200 | - |
| 12 m | 0.88 ± 0.07 | 0.88 ± 0.16 * | 0.77 ± 0.09 * | 0.036 * | - | |
| Zone 3 | 6 m | 0.98 ± 0.03 | 0.96 ± 0.06 | 0.96 ± 0.09 | 0.673 | - |
| 12 m | 0.96 ± 0.02 | 0.95 ± 0.08 | 0.97 ± 0.07 | 0.771 | - | |
| Zone 4 | 6 m | 0.99 ± 0.02 | 0.98 ± 0.05 | 0.97 ± 0.05 | 0.769 | - |
| 12 m | 0.98 ± 0.02 | 0.97 ± 0.05 | 0.97 ± 0.06 | 0.985 | - | |
| Zone 5 | 6 m | 0.98 ± 0.03 | 0.97 ± 0.08 | 0.97 ± 0.08 | 0.948 | - |
| 12 m | 0.96 ± 0.03 | 0.92 ± 0.21 | 0.98 ± 0.09 | 0.429 | - | |
| Zone 6 | 6 m | 0.91 ± 0.08 | 0.91 ± 0.12 | 0.88 ± 0.15 | 0.911 | - |
| 12 m | 0.90 ± 0.13 | 0.94 ± 0.10 | 0.82 ± 0.15 | 0.169 | - | |
| Zone 7 | 6 m | 0.86 ± 0.15 | 0.78 ± 0.13 | 0.71 ± 0.16 | 0.298 | - |
| 12 m | 0.86 ± 0.21 | 0.80 ± 0.16 | 0.67 ± 0.10 | 0.113 | - | |
| Pre-Injury Intervention | Post-Injury Intervention | No Intervention | p Value | X2 Value | ||
|---|---|---|---|---|---|---|
| Number of Patients | 6 | 19 | 15 | - | - | |
| Dorr type | A, 2; B, 3; C, 1 | A, 1; B, 13; C, 5 | A, 3; B, 8; C, 4 | 0.523 | - | |
| Female, n (%) | 5 (83.3%) | 13 (68.4%) | 10 (66.7%) | 0.737 | 0.610 | |
| Age (years) | 84.2 ± 3.3 | 79.9 ± 6.8 | 79.2 ± 6.6 | 0.129 | - | |
| BMI (kg/m2) | 21.1 ± 2.1 | 21.5 ± 2.7 | 19.7 ± 2.3 | 0.902 | - | |
| HHS (points) | 83.7 ± 16.3 | 79.6 ± 18.3 | 85.2 ± 12.9 | 0.832 | - | |
| EQ-5D-5L (score) | 0.82 ± 0.18 | 0.77 ± 0.22 | 0.77 ± 0.16 | 0.743 | - | |
| Zone area | Time | BMD change rate | ||||
| Zone 1 | 6 m | 0.94 ± 0.10 | 0.86 ± 0.11 | 0.87 ± 0.11 | 0.351 | - |
| 12 m | 0.95 ± 0.11 + | 0.88 ± 0.13 | 0.80 ± 0.14 + | 0.039 + | - | |
| Zone 2 | 6 m | 0.93 ± 0.08 | 0.86 ± 0.16 | 0.89 ± 0.07 | 0.699 | - |
| 12 m | 0.92 ± 0.09 | 0.86 ± 0.18 | 0.83 ± 0.10 | 0.357 | - | |
| Zone 3 | 6 m | 1.01 ± 0.04 | 0.95 ± 0.06 | 0.97 ± 0.06 | 0.920 | - |
| 12 m | 0.98 ± 0.03 | 0.96 ± 0.09 | 0.94 ± 0.05 | 0.336 | - | |
| Zone 4 | 6 m | 1.00 ± 0.04 | 0.97 ± 0.04 | 0.98 ± 0.05 | 0.446 | - |
| 12 m | 0.99 ± 0.02 | 0.97 ± 0.05 | 0.97 ± 0.04 | 0.552 | - | |
| Zone 5 | 6 m | 0.98 ± 0.08 | 0.97 ± 0.07 | 0.96 ± 0.08 | 0.974 | - |
| 12 m | 0.97 ± 0.04 | 0.96 ± 0.08 | 0.89 ± 0.26 | 0.700 | - | |
| Zone 6 | 6 m | 0.98 ± 0.10 | 0.90 ± 0.13 | 0.87 ± 0.10 | 0.076 | - |
| 12 m | 0.94 ± 0.10 | 0.92 ± 0.15 | 0.89 ± 0.09 | 0.387 | - | |
| Zone 7 | 6 m | 0.94 ± 0.09 #+ | 0.73 ± 0.14 # | 0.76 ± 0.12 + | 0.003 #, 0.005 + | - |
| 12 m | 0.93 ± 0.11 #+ | 0.74 ± 0.19 # | 0.78 ± 0.14 + | 0.004 #, 0.029 + | - | |
| Type of Drug | Number of Patients (n = 39) |
|---|---|
| Vitamin D | 17 (44%) |
| Bisphosphonate | 16 (41%) |
| Denosumab | 3 (8%) |
| Teriparatide | 2 (5%) |
| SERM | 1 (2%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oe, K.; Hayashi, S.; Fukui, T.; Sakai, Y.; Takahara, S.; Iwakura, T.; Sakurai, A.; Shoda, E.; Kuroda, R.; Niikura, T. Association Between Bone Mineral Density Around the Stem, Morphology of the Proximal Femur, and Effects of Osteoporosis Treatment in Patients with Femoral Neck Fracture. Osteology 2025, 5, 9. https://doi.org/10.3390/osteology5010009
Oe K, Hayashi S, Fukui T, Sakai Y, Takahara S, Iwakura T, Sakurai A, Shoda E, Kuroda R, Niikura T. Association Between Bone Mineral Density Around the Stem, Morphology of the Proximal Femur, and Effects of Osteoporosis Treatment in Patients with Femoral Neck Fracture. Osteology. 2025; 5(1):9. https://doi.org/10.3390/osteology5010009
Chicago/Turabian StyleOe, Keisuke, Shinya Hayashi, Tomoaki Fukui, Yoshitada Sakai, Shunsuke Takahara, Takashi Iwakura, Atsushi Sakurai, Etsuo Shoda, Ryosuke Kuroda, and Takahiro Niikura. 2025. "Association Between Bone Mineral Density Around the Stem, Morphology of the Proximal Femur, and Effects of Osteoporosis Treatment in Patients with Femoral Neck Fracture" Osteology 5, no. 1: 9. https://doi.org/10.3390/osteology5010009
APA StyleOe, K., Hayashi, S., Fukui, T., Sakai, Y., Takahara, S., Iwakura, T., Sakurai, A., Shoda, E., Kuroda, R., & Niikura, T. (2025). Association Between Bone Mineral Density Around the Stem, Morphology of the Proximal Femur, and Effects of Osteoporosis Treatment in Patients with Femoral Neck Fracture. Osteology, 5(1), 9. https://doi.org/10.3390/osteology5010009







