Managing Native Hip Protrusio: Simplified Classification and Surgical Recommendations
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Protrusio Acetabuli Classification System
3.2. Managing Protrusio Acetabuli
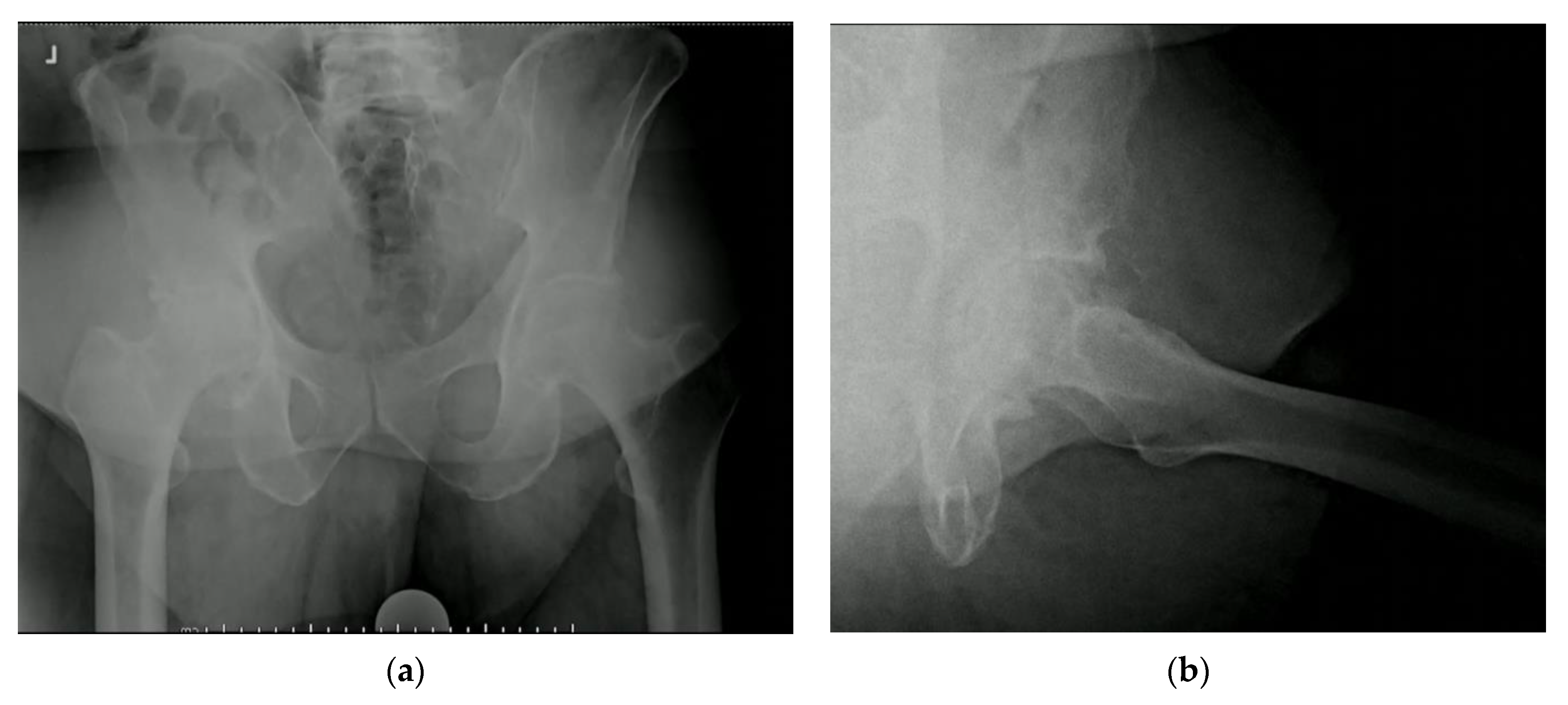
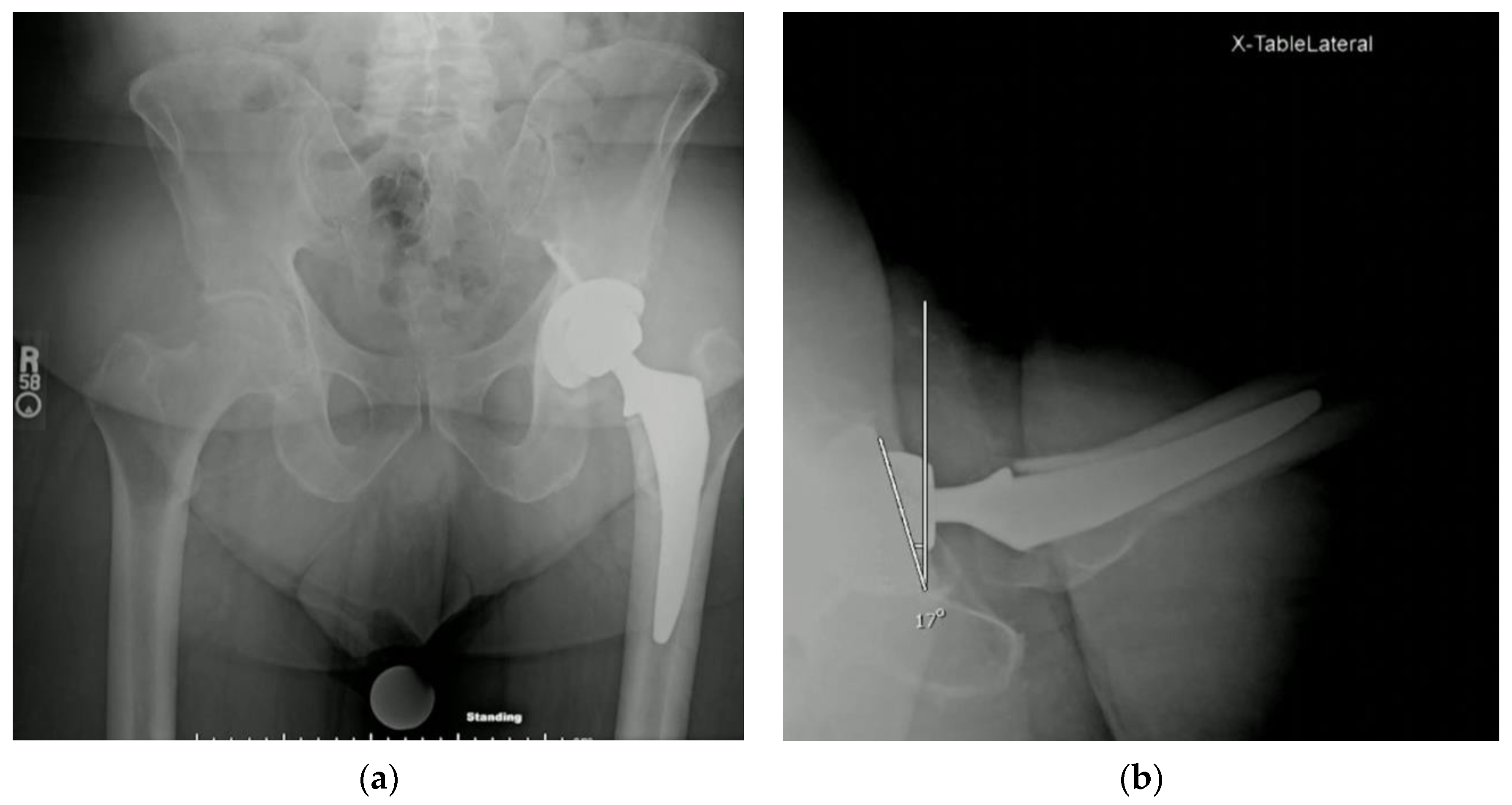
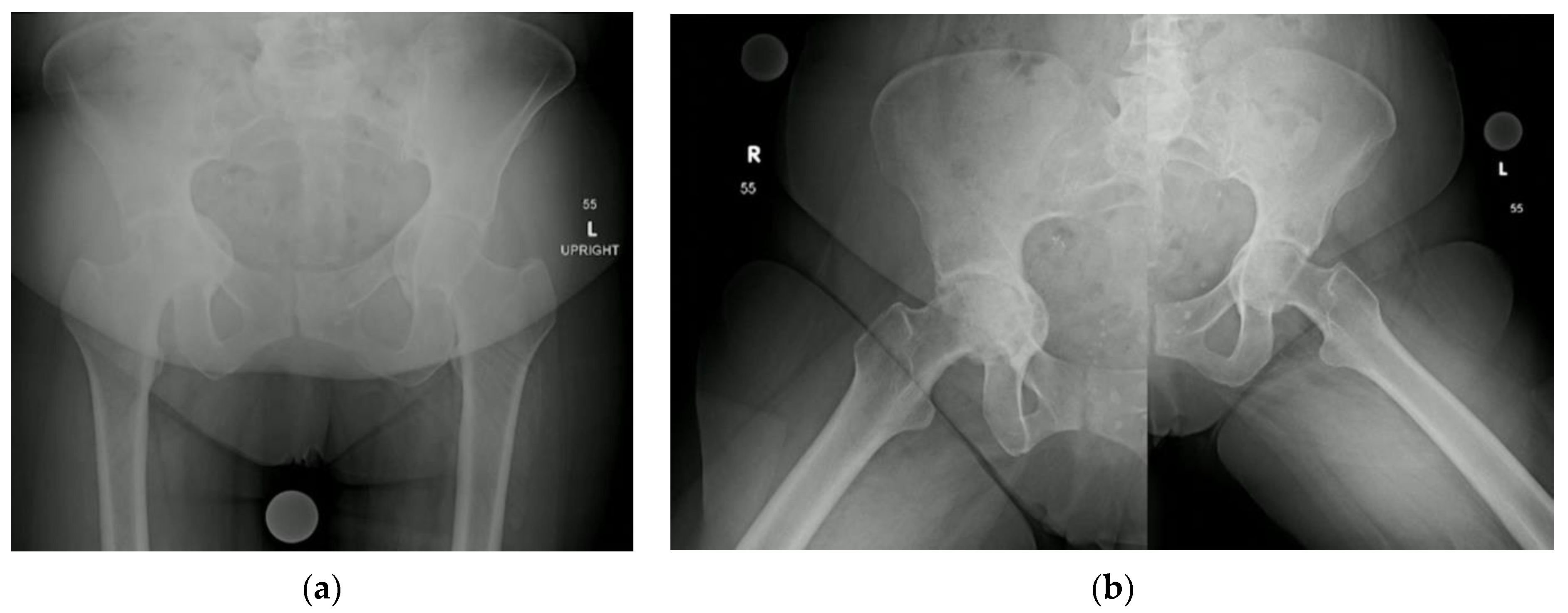
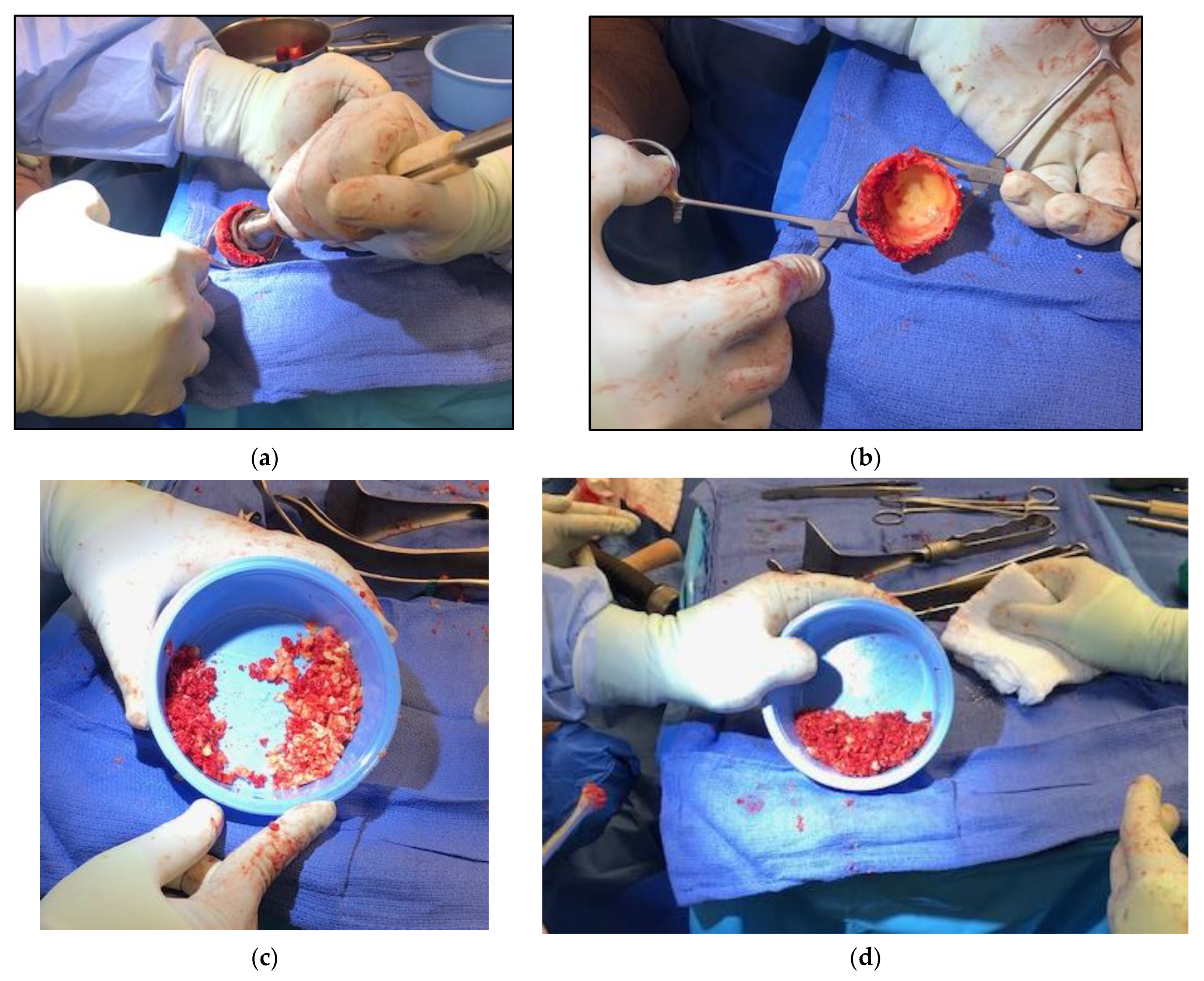
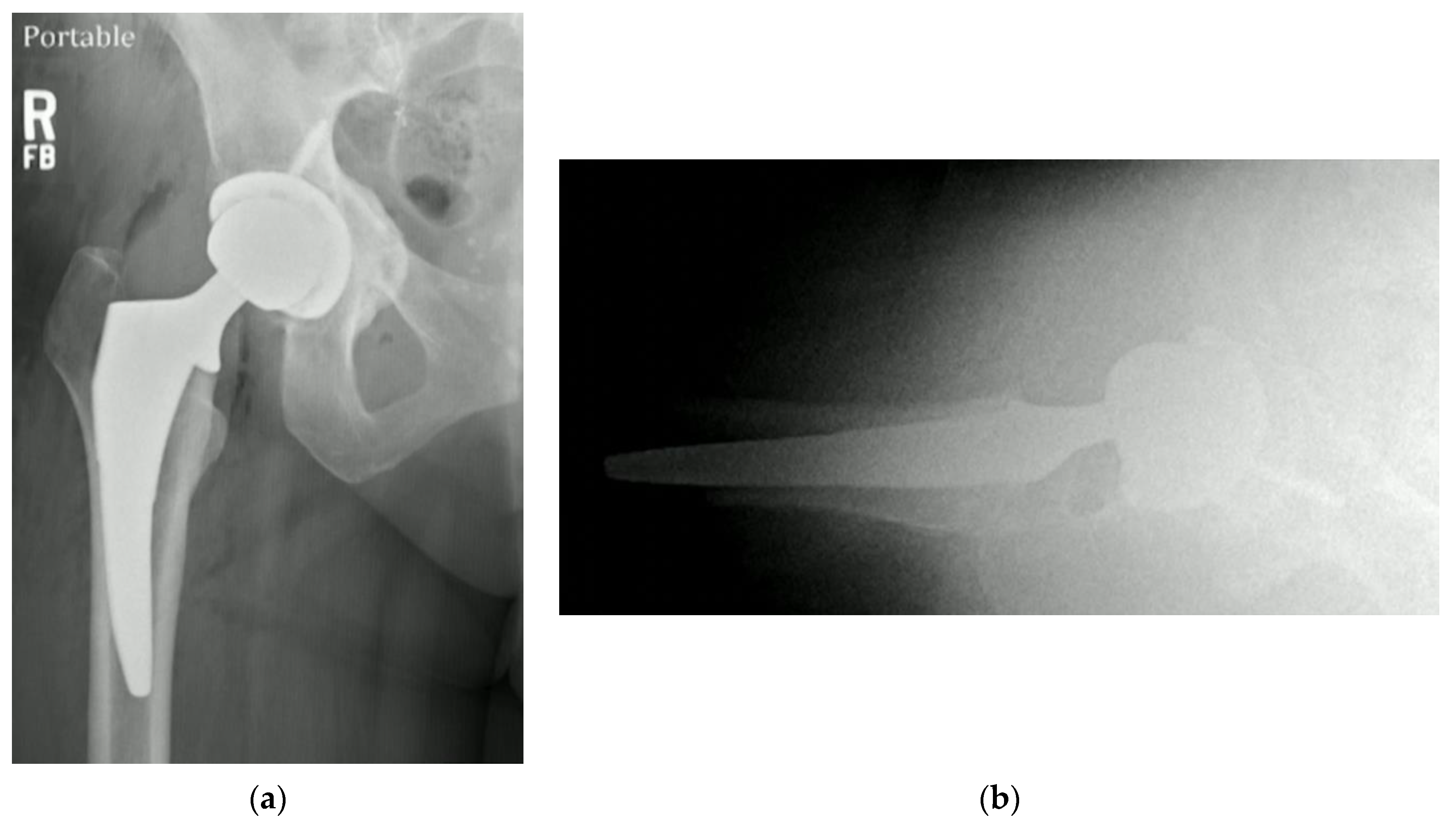
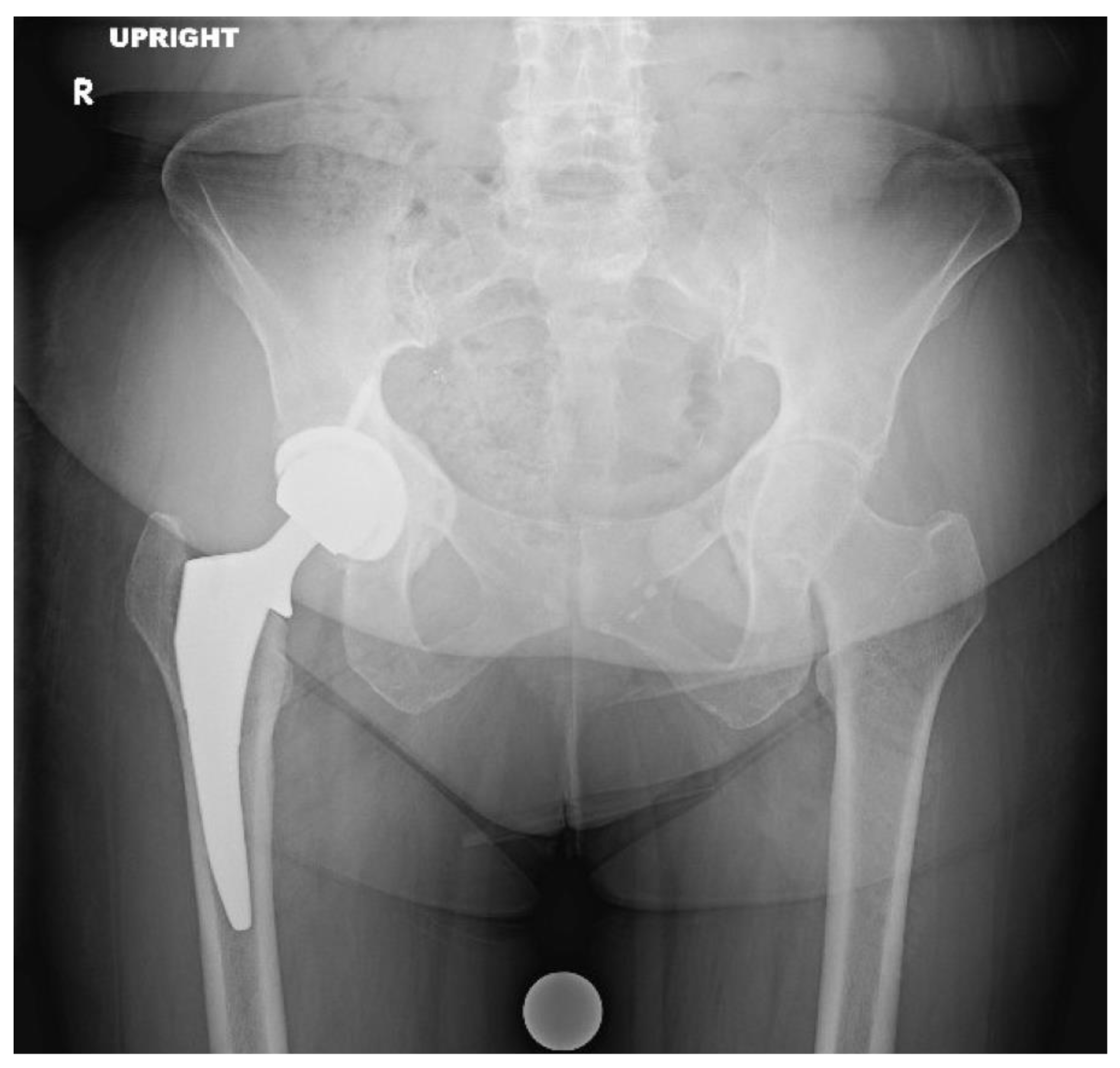
3.3. Protrusio Cases
3.4. Technical Pearls
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pomeranz, M. Intrapelvic Protrusion of the Acetabulum (Otto Pelvis). J. Bone Jt. Surg. Am. 2007, 465, 6–15. [Google Scholar]
- McBride, M.; Muldoon, M.; Santore, R.; Trousdale, R.; Wenger, D. Protrusio Acetabuli: Diagnosis and Treatment. J. Am. Acad. Orthop. Surg. 2001, 9, 79–88. [Google Scholar] [CrossRef] [PubMed]
- Armbuster, T.; Guerra, J.; Resnick, D.; Goergen, T.; Feingold, M.; Niwayama, G.; Danzig, L. The Adult Hip: An Anatomic Study. Part I: The bony landmarks. Radiology 1978, 128, 1–10. [Google Scholar] [CrossRef]
- Kindynis, P.; Garcia, J. Protrusio acetabuli. An update on the primary and secondary acetabular protrusion. J. Radiol. 1990, 71, 415–424. [Google Scholar]
- Levin, W. Intrapelvic Protrusion of the Acetabulum (Otto Pelvis). JAMA 1935, 105, 112. [Google Scholar] [CrossRef]
- Verrall, P. An unusual bilateral condition of the acetabula. J. Bone Jt. Surg. 1929, 11, 39. [Google Scholar]
- McEwen, C.; Poppel, M.; Poker, N.; Jacobson, H. Protrusio Acetabuli in Rheumatoid Arthritis. Radiology 1956, 66, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Gates, H.; Poletti, S.; Callaghan, J.; McCollum, D. Radiographic measurements in protrusio acetabuli. J. Arthroplast. 1989, 4, 347–351. [Google Scholar] [CrossRef]
- Alexander, C. The Aetiology of Primary Protrusio Acetabuli. Br. J. Radiol. 1965, 38, 567–580. [Google Scholar] [CrossRef]
- Hooper, J.; Jones, E. Primary protrusion of the acetabulum. J. Bone Jt. Surg Br. 1971, 53, 23–29. [Google Scholar] [CrossRef]
- Sponseller, P.; Jones, K.; Ahn, N.; Erkula, G.; Foran, J.; Dietz, H. Protrusio acetabuli in Marfan syndrome: Age-related prevalence and associated hip function. J. Bone Joint Surg. Am. 2006, 88, 486–495. [Google Scholar] [CrossRef] [PubMed]
- Ahn, J.; Carter, E.; Raggio, C.; Green, D. Acetabular protrusio in patients with osteogenesis imperfecta: Risk factors and progres-sion. J. Pediatr Orthop. 2019, 39, e750–e754. [Google Scholar] [CrossRef] [PubMed]
- Violas, P.; Fassier, F.; Hamdy, R.; Duhaime, M.; Glorieux, F. Acetabular Protrusion in Osteogenesis Imperfecta. J. Pediatr. Orthop. 2002, 22, 622–625. [Google Scholar] [CrossRef]
- Roberts, T.; Cepela, D.; Uhl, R.; Lozman, J. Orthopaedic Considerations for the Adult With Osteogenesis Imperfecta. J. Am. Acad. Orthop. Surg. 2016, 24, 298–308. [Google Scholar] [CrossRef]
- Hastings, D.; Parker, S. Protrusio Acetabuli in Rheumatoid Arthritis. Clin. Orthop. Relat. Res. 1975, 108, 76–83. [Google Scholar] [CrossRef]
- Samanta, J.; Chattopadhyay, A.; Sharma, A. Protrusio acetabuli. J. Clin. Rheumatol. 2021, 27, S786. [Google Scholar] [CrossRef]
- Dwosh, I.; Resnick, D.; Becker, M. Hip involvement in ankylosing spondylitis. Arthritis Rheum. 1976, 19, 683–692. [Google Scholar] [CrossRef] [PubMed]
- Mullaji, A.; Shetty, G. Acetabular protrusio: Surgical technique of dealing with a problem in depth. Bone Jt. J. 2013, 95 (Suppl. A), 37–40. [Google Scholar] [CrossRef]
- Greig, D.; Hsiue, P.; Chen, C.; Trikha, R.; Khoshbin, A.; Stavrakis, A. Outcomes of Total Hip Arthroplasty in Patients with Acetabular Protrusio. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 2020, 4, e20.00121. [Google Scholar] [CrossRef]
- Baghdadi, Y.; Larson, N.; Sierra, R. Restoration of the Hip Center during THA Performed for Protrusio Acetabuli Is Associated with Better Implant Survival. Clin. Orthop. Relat. Res. 2013, 471, 3251–3259. [Google Scholar] [CrossRef]
- Leunig, M.; Nho, S.; Turchetto, L.; Ganz, R. Protrusio Acetabuli: New Insights and Experience with Joint Preservation. Clin. Orthop. Relat. Res. 2009, 467, 2241–2250. [Google Scholar] [CrossRef] [PubMed]
- Sotelo-Garza, A.; Charnley, J. The Results of Charnley Arthroplasty of the Hip Performed for Protrusio Acetabuli. Clin. Orthop. Relat. Res. 1978, 132, 12–18. [Google Scholar] [CrossRef]
- Ranawat, C.; Zahn, M. Role of bone grafting in correction of protrusio acetabuli by total hip arthroplasty. J. Arthroplast. 1986, 1, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Hirst, P.; Esser, M.; Murphy, J.; Hardinge, K. Bone grafting for protrusio acetabuli during total hip replacement. A review of the Wrightington method in 61 hips. J. Bone Jt. Surg. 1987, 69, 229–233. [Google Scholar] [CrossRef] [PubMed]
- Clohisy, J.; Carlisle, J.; Trousdale, R.; Kim, Y.; Beaule, P.; Morgan, P.; Steger-May, K.; Schoenecker, P.; Millis, M. Radiographic Evaluation of the Hip has Limited Reliability. Clin. Orthop. Relat. Res. 2008, 467, 666–675. [Google Scholar] [CrossRef]
- Saleh, K.; Holtzman, J.; Gafni, A.; Saleh, L.; Jaroszynski, G.; Wong, P.; Woodgate, I.; Davis, A.; Gross, A. Development, test reliability and validation of a classification for revision hip arthroplasty. J. Orthop. Res. 2001, 19, 50–56. [Google Scholar] [CrossRef]
- Paprosky, W.; Perona, P.; Lawrence, J. Acetabular defect classification and surgical reconstruction in revision arthroplasty: A 6-year follow-up evaluation. J. Arthroplast. 1994, 9, 33–44. [Google Scholar] [CrossRef]
- Telleria, J.; Gee, A. Classifications In Brief: Paprosky Classification. Clin. Orthop. Relat. Res. 2013, 471, 3725–3730. [Google Scholar] [CrossRef]
- Campbell, D.; Garbuz, D.; Masri, B.; Duncan, C. Reliability of acetabular bone defect classification systems in revision total hip arthroplasty. J. Arthroplast. 2001, 16, 83–86. [Google Scholar] [CrossRef]
- Van Praet, F.; Mulier, M. To cement or not to cement acetabular cups in total hip arthroplasty: A systematic review and re-evaluation. SICOT J. 2019, 5, 35. [Google Scholar] [CrossRef]
- Boisgard, S.; Descamps, S.; Bouillet, B. Complex primary total hip arthroplasty. Orthop. Traumatol. Surg. Res. 2013, 99, S34–S42. [Google Scholar] [CrossRef]
- Ries, M. Total Hip Arthroplasty in Acetabular Protrusio. Orthopedics 2009, 32, 666. [Google Scholar]
- Zhao, X.; Zhu, Z.; Zhao, J.; Li, M.; Wang, G.; Yu, D.; Yu, B. The utility of digital templating in Total Hip Arthroplasty with Crowe type II and III dysplastic hips. Int. Orthop. 2010, 35, 631–638. [Google Scholar] [CrossRef] [PubMed]
- Lass, R.; Olischar, B.; Kubista, B.; Waldhoer, T.; Giurea, A.; Windhager, R. Total Hip Arthroplasty Using Imageless Computer-Assisted Navigation—2-Year Follow-Up of a Prospective Randomized Study. J. Clin. Med. 2020, 9, 1620. [Google Scholar] [CrossRef] [PubMed]
- James, C.; Peterson, B.; Crim, J.; Cook, J.; Crist, B. The Use of Fluoroscopy During Direct Anterior Hip Arthroplasty: Powerful or Misleading? J. Arthroplast. 2018, 33, 1775–1779. [Google Scholar] [CrossRef]
- Zhen, P.; Li, X.; Zhou, S.; Lu, H.; Chen, H.; Liu, J. Total hip arthroplasty to treat acetabular protrusions secondary to rheumatoid arthritis. J. Orthop. Surg. Res. 2018, 13, 92. [Google Scholar] [CrossRef]
- Sarpong, N.; Herndon, C.; Shah, R. Acetabular “up-and-in” defect treated with in-situ femoral head autograft technique during total hip arthroplasty. Arthroplast. Today 2019, 5, 301–305. [Google Scholar] [CrossRef]
- Krishnan, H.; Patel, N.; Skinner, J.; Muirhead-Allwood, S.; Briggs, T.; Carrington, R.; Miles, J. Primary and revision total hip ar-throplasty in osteogenesis imperfecta. Hip Int. 2013, 23, 303–309. [Google Scholar] [CrossRef]
- Bengoa, F.; Lopez, A.; Dabed, D.; Rojas, N.; Diaz-Ledezma, C. Total hip arthroplasty in protrusio acetabuli: Ten tips to improve surgical outcomes. Rev. Chil. Ortop. Traumatol. 2021, 62, e127–e135. [Google Scholar]
- Sathappan, S.; Ginat, D.; Patel, V.; Walsh, M.; Jaffe, W.; Cesare, P. Effect of Anesthesia Type on Limb Length Discrepancy After Total Hip Arthroplasty. J. Arthroplast. 2008, 23, 203–209. [Google Scholar] [CrossRef]
- Chughtai, M.; Samuel, L.; Acuna, A.; Kamath, A. Algorithmic soft tissue femoral release in anterior approach total hip arthroplasty. Arthroplast. Today 2019, 5, 471–476. [Google Scholar] [CrossRef] [PubMed]
- Honcharuk, E.; Kayiaros, S.; Rubin, L. The direct anterior approach for acetabular augmentation in primary total hip arthroplasty. Arthroplast. Today 2018, 4, 33–39. [Google Scholar] [CrossRef] [PubMed]



| Grade | Distance between Acetabulum and Ilioischial Line |
|---|---|
| I | 1–5 mm (mild protrusio) |
| II | 6–15 mm (moderate protrusio) |
| III | 16+ mm (severe protrusio) |
| Grade | Distance between Acetabular and Ilioischial Lines (Men) | Distance between Acetabular and Ilioischial Lines (Women) |
|---|---|---|
| I | 3–8 mm | 6–11 mm |
| II | 8–13 mm | 12–17 mm |
| III | Over 13 mm with fragmentation | Over 17 mm with fragmentation |
| Class | Ilioischial Line | Iliopectineal Line | Recommended Treatment |
|---|---|---|---|
| I | Intact (femoral head medialized) | Intact | Implant Placement: Lateralization of acetabular component to match native rim. Standard component needed, no need for screw augmentation. Bone graft: Not likely required. |
| II | Violated | Intact | Implant Placement: Lateralization of acetabular component to rim, consider use of larger or jumbo component. Screw fixation optional. Consider lateralized acetabular liner. Bone Graft: Likely required medially with impaction grafting. |
| III | Violated | Violated | Implant Placement: Lateralization of acetabular component, consider use of jumbo, deep profile, revision, or multi-hole component. Screw fixation is strongly recommended in multiple planes to augment construct stability. Consider lateralized acetabular liner. Bone Graft: Universally required. Autograft reamings and morselized cortical bone from native head is recommended, consider use of additional allograft bone to fill large defects. Powdered antibiotic can be added to graft mixture to reduce risk of prosthetic joint infection. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ani, L.; Radford, Z.; Rubin, L.E. Managing Native Hip Protrusio: Simplified Classification and Surgical Recommendations. Osteology 2023, 3, 33-46. https://doi.org/10.3390/osteology3010005
Ani L, Radford Z, Rubin LE. Managing Native Hip Protrusio: Simplified Classification and Surgical Recommendations. Osteology. 2023; 3(1):33-46. https://doi.org/10.3390/osteology3010005
Chicago/Turabian StyleAni, Lidia, Zachary Radford, and Lee E. Rubin. 2023. "Managing Native Hip Protrusio: Simplified Classification and Surgical Recommendations" Osteology 3, no. 1: 33-46. https://doi.org/10.3390/osteology3010005
APA StyleAni, L., Radford, Z., & Rubin, L. E. (2023). Managing Native Hip Protrusio: Simplified Classification and Surgical Recommendations. Osteology, 3(1), 33-46. https://doi.org/10.3390/osteology3010005






