Cross-Cultural Review of Sexuality, Relationships, and Body Image after Burns: Analysis of the BSHS-B
Abstract
1. Introduction
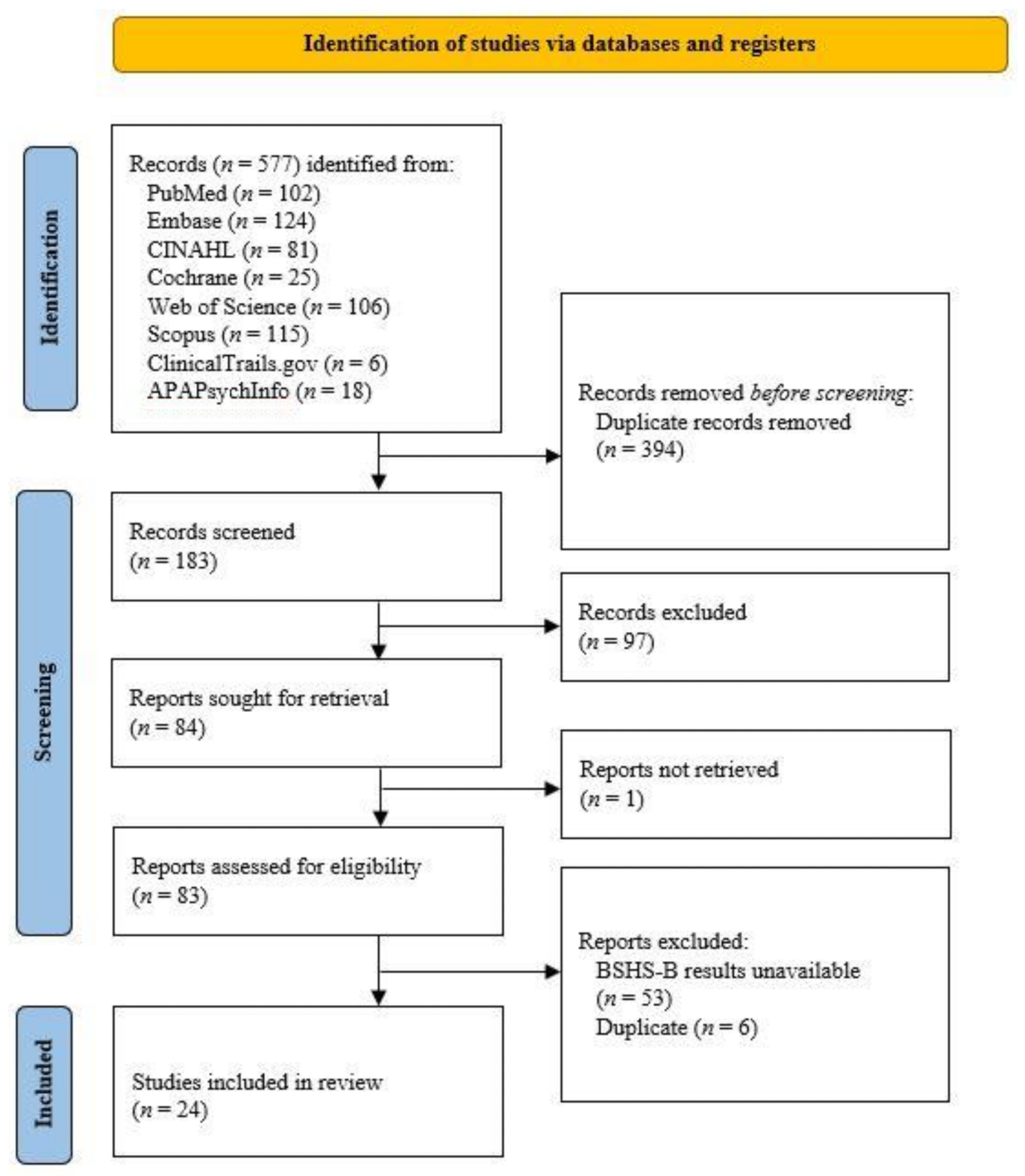
2. Materials and Methods
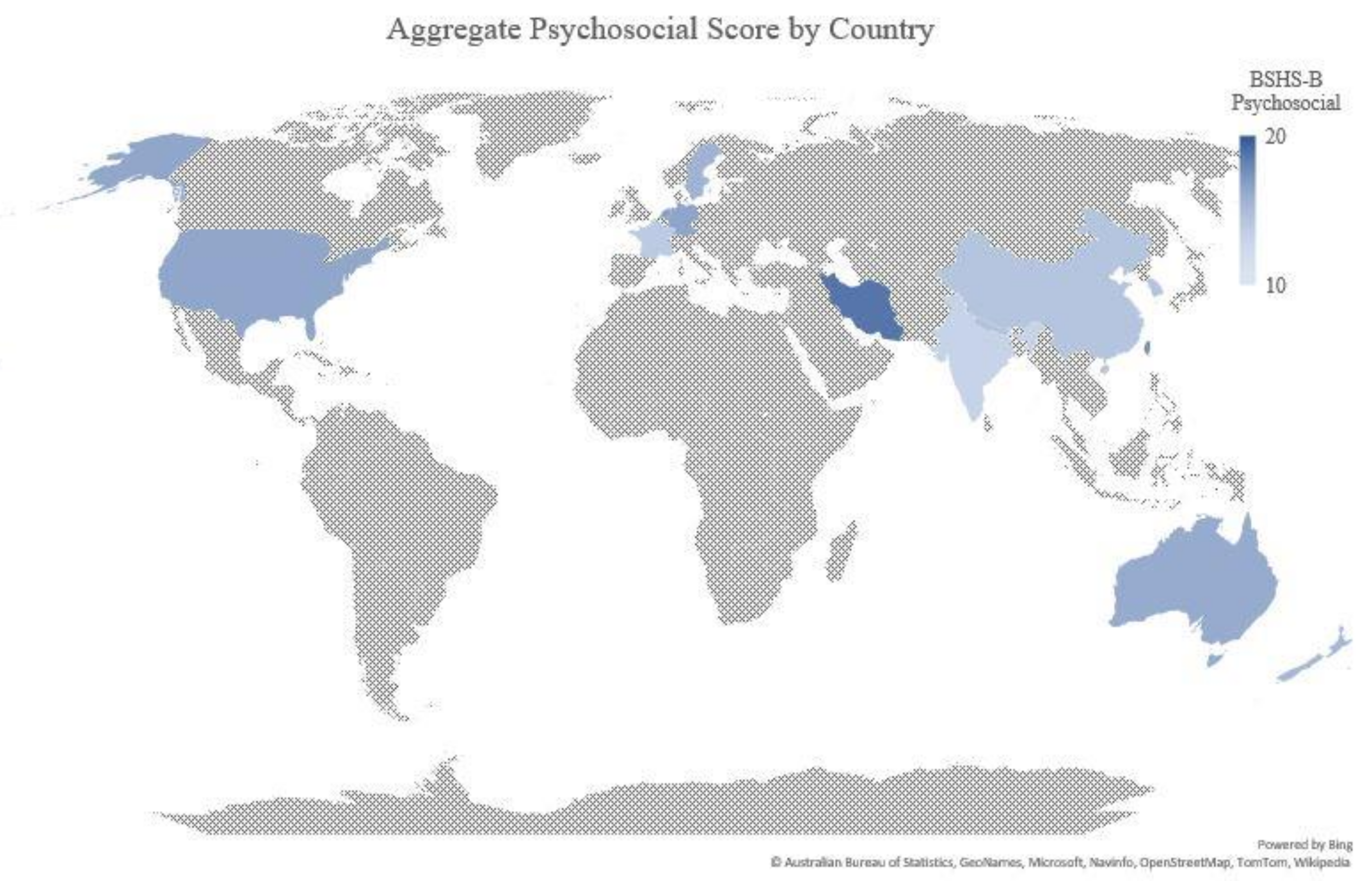
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Capek, K.; Sousse, L.E.; Hundeshagen, G.; Voigt, C.D.; Suman, O.E.; Finnerty, C.C.; Jennings, K.; Herndon, D.N. Contemporary Burn Survival. J. Am. Coll. Surg. 2018, 226, 453–463. [Google Scholar] [CrossRef]
- Bernstein, N.R. Objective bodily damage: Disfigurement and dignity. In Body Images: Development, Deviance, and Change; Cash, T.F., Pruzinsky, T., Eds.; Guilford Press: New York, NY, USA, 1990; pp. 131–148. [Google Scholar]
- Thombs, B.D.; Haines, J.M.; Bresnick, M.G.; Magyar-Russell, G.; Fauerbach, J.A.; Spence, R.J. Depression in burn reconstruction patients: Symptom prevalence and association with body image dissatisfaction and physical function. Gen. Hosp. Psychiatry 2007, 29, 14–20. [Google Scholar] [CrossRef]
- Kazemzadeh, J.; Rabiepoor, S.; Alizadeh, S. Satisfaction with appearance and sexual satisfaction in women with severe burn injuries. Int. J. Impot. Res. 2021, in press. [Google Scholar] [CrossRef] [PubMed]
- Fauerbach, J.A.; Heinberg, L.J.; Lawrence, J.W.; Munster, A.M.; Palombo, D.A.; Richter, D.; Spence, R.J.; Stevens, S.S.; Ware, L.; Muehlberger, T. Effect of Early Body Image Dissatisfaction on Subsequent Psychological and Physical Adjustment after Disfiguring Injury. Psychosom. Med. 2000, 62, 576–582. [Google Scholar] [CrossRef]
- Ajoudani, F.; Jasemi, M.; Lotfi, M. Social participation, social support, and body image in the first year of rehabilitation in burn survivors: A longitudinal, three-wave cross-lagged panel analysis using structural equation modeling. Burns 2018, 44, 1141–1150. [Google Scholar] [CrossRef] [PubMed]
- Fauerbach, J.A.; Pruzinsky, T.; Saxe, G.N. Psychological health and function after burn injury: Setting research priorities. J. Burn. Care Res. 2007, 28, 587–592. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, J.W.; Fauerbach, J.A.; Thombs, B.D. A test of the moderating role of importance of appearance in the relationship between perceived scar severity and body-esteem among adult burn survivors. Body Image 2006, 3, 101–111. [Google Scholar] [CrossRef]
- Thombs, B.D.; Notes, L.D.; Lawrence, J.W.; Magyar-Russell, G.; Bresnick, M.G.; Fauerbach, J.A. From survival to socialization: A longitudinal study of body image in survivors of severe burn injury. J. Psychosom. Res. 2008, 64, 205–212. [Google Scholar] [CrossRef]
- Thompson, J.K.; Heinberg, L.J.; Altabe, M.; Tantleff-Dunn, S. Exacting Beauty: Theory, Assessment, and Treatment of Body Image Disturbance; American Psychological Association: Washington, DC, USA, 1999. [Google Scholar]
- Grabe, S.; Hyde, J.S. Ethnicity and body dissatisfaction among women in the United States: A meta-analysis. Psychol. Bull. 2006, 132, 622–640. [Google Scholar] [CrossRef]
- Wildes, J.E.; Emery, R.E.; Simons, A.D. The roles of ethnicity and culture in the development of eating disturbance and body dissatisfaction: A meta-analytic review. Clin. Psychol. Rev. 2001, 21, 521–551. [Google Scholar] [CrossRef]
- Schooler, D. Real Women Have Curves: A Longitudinal Investigation of TV and the Body Image Development of Latina Adolescents. J. Adolesc. Res. 2008, 23, 132–153. [Google Scholar] [CrossRef]
- Kildal, M.; Andersson, G.; Fugl-Meyer, A.R.; Lannerstam, K.; Gerdin, B. Development of a brief version of the Burn Specific Health Scale (BSHS-B). J. Trauma 2001, 51, 740–746. [Google Scholar] [CrossRef] [PubMed]
- Gandolfi, S.; Auquit-Auckbur, I.; Panunzi, S.; Mici, E.; Grolleau, J.L.; Chaput, B. Validation of the French version of the Burn Specific Health Scale-Brief (BSHS-B) questionnaire. Burns 2016, 42, 1573–1580. [Google Scholar] [CrossRef] [PubMed]
- Müller, A.; Smits, D.; Jasper, S.; Berg, L.; Claes, L.; Ipaktchi, R.; Vogt, P.M.; de Zwaan, M. Validation of the German version of the Burn Specific Health Scale-Brief (BSHS-B). Burns 2015, 41, 1333–1339. [Google Scholar] [CrossRef] [PubMed]
- Pishnamazi, Z.; Rejeh, N.; Heravi-Karimooi, M.; Vaismoradi, M. Validation of the Persian version of the Burn Specific Health Scale—Brief. Burns 2013, 39, 162–167. [Google Scholar] [CrossRef]
- Latif, N.A.A.; Emam, Z.M.; Awady, M.A.E. Validity and reliability of translated Arabic version of the burn specific health scale-brief. Curr. Sci. Int. 2019, 8, 168–177. [Google Scholar]
- Ling-Juan, Z.; Jie, C.; Jian, L.; Xiao-Ying, L.; Ping, F.; Zhao-Fan, X.; Jian-Ling, H.; Juan, H.; Feng, Z.; Tao, L. Development of quality of life scale in Chinese burn patients: Cross-cultural adaptation process of burn-specific health scale-brief. Burns 2012, 38, 1216–1223. [Google Scholar] [CrossRef]
- Mulay, A.M.; Ahuja, A.; Ahuja, R.B. Modification, cultural adaptation and validation of burn specific health scale-brief (BSHS-B) for Hindi speaking population. Burns 2015, 41, 1543–1549. [Google Scholar] [CrossRef]
- Mendez-Romero, D.; Clark, A.T.; Christie, A.; Wolf, S.E. Weight changes and patterns of weight measurements in hospitalized burn patients: A contemporary analysis. Burn. Trauma 2018, 6, 30. [Google Scholar] [CrossRef]
- Altman, D.G.; Machin, D.; Bryant, T.N.; Gardner, M.J. Statistics with Confidence, 2nd ed.; BMJ Books: London, UK, 2000; pp. 28–31. [Google Scholar]
- Sindi, R.; Dos Reis, C.S.; Bennett, C.; Stevenson, G.; Sun, Z. Quantitative Measurements of Breast Density Using Magnetic Resonance Imaging: A Systematic Review and Meta-Analysis. J. Clin. Med. 2019, 8, 745. [Google Scholar] [CrossRef]
- Spronk, I.; Van Loey, N.E.E.; van der Vlies, C.H.; Haagsma, J.A.; Polinder, S.; van Baar, M.E.; Nieuwenhuis, M.K.; Middelkoop, E.; Pijpe, A.; Stoop, M.M.; et al. Activity Impairment, Work Status, and Work Productivity Loss in Adults 5–7 Years after Burn Injuries. J. Burn Care Res. 2021, 43, 256–262. [Google Scholar] [CrossRef]
- Hsu, K.C.; Lu, H.F.; Chen, Y.C.; Chen, L.F. Differences in parent-perceived and patient-reported quality of life among young adult burn patients: A prospective longitudinal study. Burns 2021, 47, 1878–1889. [Google Scholar] [CrossRef] [PubMed]
- Tehranineshat, B.; Mohammadi, F.; Mehdizade Tazangi, R.; Sohrabpour, M.; Parviniannasab, A.M.; Bijani, M. A Study of the Relationship Among Burned Patients’ Resilience and Self-Efficacy and Their Quality of Life. Patient Prefer. Adherence 2020, 14, 1361–1369. [Google Scholar] [CrossRef] [PubMed]
- Shakya, R.; Manandhar, M.; Dangol, R.; Shrestha, A. Cross cultural adaptation and validation of burn specific health scale- brief in Nepali (BSHS-B-Np). J. Patient-Rep. Outcomes 2020, 4, 25. [Google Scholar] [CrossRef] [PubMed]
- Bourgi, J.; Sleiman, Z.; Fazaa, E.; Maasarani, D.; Chahine, Y.; Nassif, E.; Youssef, E.; Chami, J.; Mikhael, R.; Ghanime, G. Predictors of generic and burn-specific quality of life among adult burn patients admitted to a Lebanese burn care center: A cross-sectional single-center study. Int. J. Burn. Trauma 2020, 10, 81–89. [Google Scholar]
- Zhang, X.; Liu, Y.; Deng, X.; Deng, C.; Pan, Y.; Hu, A. The Correlation Between Quality of Life and Acceptability of Disability in Patients with Facial Burn Scars. Front. Bioeng. Biotechnol. 2019, 7, 329. [Google Scholar] [CrossRef]
- Gojowy, D.; Kauke, M.; Ohmann, T.; Homann, H.-H.; Mannil, L. Early and late-recorded predictors of health-related quality of life of burn patients on long-term follow-up. Burns 2019, 45, 1300–1310. [Google Scholar] [CrossRef] [PubMed]
- Gandolfi, S.; Carloni, R.; Bertheuil, N.; Grolleau, J.; Auquit-Auckbur, I.; Chaput, B. Assessment of quality-of-life in patients with face-and-neck burns: The Burn-Specific Health Scale for Face and Neck (BSHS-FN). Burns 2018, 44, 1602–1609. [Google Scholar] [CrossRef]
- Chin, T.L.; Carrougher, G.J.; Amtmann, D.; McMullen, K.; Herndon, D.N.; Holavanahalli, R.; Meyer, W.; Ryan, C.M.; Wong, J.N.; Gibran, N.S. Trends 10 years after burn injury: A Burn Model System National Database study. Burns 2018, 44, 1882–1886. [Google Scholar] [CrossRef] [PubMed]
- Oh, H.; Boo, S. Quality of life and mediating role of patient scar assessment in burn patients. Burns 2017, 43, 1212–1217. [Google Scholar] [CrossRef]
- Berg, L.; Meyer, S.; Ipaktchi, R.; Vogt, P.M.; Müller, A.; de Zwaan, M. Psychosocial Distress at Different Time Intervals after Burn Injury. Psychother. Psychosom. Med. Psychol. 2017, 67, 231–239. (In German) [Google Scholar] [CrossRef] [PubMed]
- Wasiak, J.; Lee, S.J.; Paul, E.; Shen, A.; Tan, H.; Cleland, H.; Gabbe, B. Female patients display poorer burn-specific quality of life 12 months after a burn injury. Injury 2017, 48, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Rothman, D.J.; Sutter, M.; Perrin, P.B.; LiBrandi, H.; Feldman, M.J. Coping styles and quality of life in adults with burn. Burns 2016, 42, 1105–1110. [Google Scholar] [CrossRef] [PubMed]
- Ahuja, R.B.; Mulay, A.M.; Ahuja, A. Assessment of quality of life (QoL) of burn patients in India using BSHS-RBA scale. Burns 2016, 42, 639–647. [Google Scholar] [CrossRef]
- Hwang, Y.F.; Chen-Sea, M.J.; Chen, C.L.; Hsieh, C.S. Validation of a Taiwanese Version of the Burn-Specific Health Scale-Brief. J. Burn. Care Res. 2016, 37, e310–e316. [Google Scholar] [CrossRef] [PubMed]
- Murphy, M.E.; Holzer, C.E., III.; Richardson, L.M.; Epperson, K.; Ojeda, S.; Martinez, E.M.; Suman, O.E.; Herndon, D.N.; Meyer, W.J. Quality of Life of Young Adult Survivors of Pediatric Burns Using World Health Organization Disability Assessment Scale II and Burn Specific Health Scale-Brief: A Comparison. J. Burn. Care Res. 2015, 36, 521–533. [Google Scholar] [CrossRef][Green Version]
- Dowda, D.J.; Li, F. Major concerns and issues in burn survivors in Australia. Burn. Trauma 2014, 2, 84–87. [Google Scholar] [CrossRef]
- Xie, B.; Xiao, S.C.; Zhu, S.H.; Xia, Z.F. Evaluation of long term health-related quality of life in extensive burns: A 12-year experience in a burn center. Burns 2012, 38, 348–355. [Google Scholar] [CrossRef]
- Roh, Y.S.; Chung, H.S.; Kwon, B.; Kim, G. Association between depression, patient scar assessment and burn-specific health in hospitalized burn patients. Burns 2012, 38, 506–512. [Google Scholar] [CrossRef]
- Reeve, J.; James, F.; McNeill, R.; Brown, P.; Cameron, L.; Mills, S. Functional and psychological outcomes following burn injury: Reduced income and hidden emotions are predictors of greater distress. J. Burn Care Res. 2011, 32, 468–474. [Google Scholar] [CrossRef]
- Sgroi, M.I.; Willebrand, M.; Ekselius, L.; Gerdin, B.; Andersson, G. Fear-avoidance in Recovered Burn Patients: Association with Psychological and Somatic Symptoms. J. Health Psychol. 2005, 10, 491–502. [Google Scholar] [CrossRef]
- World Bank. World List of Economies. Available online: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (accessed on 21 December 2021).
- McMahon, H.A.; Ndem, I.; Gampper, L.; Gampper, T.J.; DeGeorge, B.R. Quantifying Burn Injury–Related Disability and Quality of Life in the Developing World: A Primer for Patient-Centered Resource Allocation. Ann. Plast. Surg. 2019, 82, S433–S436. [Google Scholar] [CrossRef] [PubMed]
- Ren, Z.; Zhang, P.; Wang, H.; Wang, H. Qualitative research investigating the mental health care service gap in Chinese burn injury patients. BMC Health Serv. Res. 2018, 18, 902. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.M.; Ban, M.S. Rebuilding Life after Burn Injuries in Korea: Using Photovoice. J. Burn Care Res. 2019, 40, 913–922. [Google Scholar] [CrossRef] [PubMed]
- Jang, M.H.; Park, J.; Chong, M.K.; Sok, S.R. Factors Influencing Resilience of Burn Patients in South Korea. J. Nurs. Sch. 2017, 49, 478–486. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Hu, Y.; Hu, A. Stigma and illness uncertainty among patients with visible burn scars: A cross-sectional study. Burns 2021, in press. [Google Scholar] [CrossRef]
- Hemmati Maslakpak, M.; Ajoudani, F.; Lotfi, M.; Alinejad, V. Burn self-stigma: A hybrid concept analysis. Burns 2021, in press. [Google Scholar] [CrossRef]


| Author Name | Year | Country | Follow-Up | Age | Sex (% Women) | TBSA | n | Affect | Body Image | Interpersonal Relationships | Sexuality |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Spronk et al. [24] | 2021 | Netherlands | 67.2 ± 6 months | 42.8 ± 13.5 | 37.1% | 9.8 ± 12.7 | 155 | 3.7 ± 0.6 | 3.5 ± 0.8 | 3.9 ± 0.3 | 3.8 ± 0.5 |
| Hsu et al. [25] | 2021 | Taiwan | 36 months | 21.35 ± 2.71 | 62.9% | 61.12 ± 15.38 | 27 | 3.08 ± 0.54 | 2.11 ± 0.95 | 3.37 ± 0.75 | 3.45 ± 0.48 |
| Tehranineshat et al. [26] | 2020 | Iran | 80% in 6–12 months | 34.48 ± 8.4 | 60.3% | 36.1% ± 8.19 | 305 | 4.5 ± 0.27 | 3.8 ± 0.37 | 4.45 ± 0.79 | 4.98 ± 0.14 |
| Shakya et al. [27] | 2020 | Nepal | 39.9 ± 81.2 months | 28.9 ± 10.6 | 57.7% | 16.6 ± 8.3 | 111 | 2.96 ± 1.0 | 2.10 ± 1.3 | 3.63 ± 0.8 | 3.53 ± 0.9 |
| Bourgi et al. [28] | 2020 | Lebanon | 36.8 ± 16.1 months | 44.6 ± 17.2 | 26.9% | 24.5 | 130 | 3.17 ± 1.05 | 2.49 ± 1.41 | 3.55 ± 0.86 | 3.43 ± 0.81 |
| Zhang et al. [29] | 2019 | China | 116.72 days (15–427) | 42.77 ± 13.82 | 36.4% | n/a | 121 | 3.64 ± 0.62 | 3.08 ± 0.63 | 3.57 ± 0.49 | 3.81 ± 0.5 |
| Gojowy et al. [30] | 2019 | Germany | 170.4 ± 40.8 months | 51 ± 17 | 26% | 39 ± 17 | 42 | 3.8 ± 0.5 | 3.3 ± 0.8 | 4.0 ± 0.2 | 3.8 ± 0.6 |
| Gandolfi et al. [31] | 2018 | France | >24 months | 46.4 ± 15.9 | 34% | 26.9 ± 15.9 | 53 | 4.33 ± 1.68 | 1.99 ± 1.18 | 3.56 ± 0.69 | 1.84 ± 0.76 |
| Chin et al. [32] | 2018 | USA | 120 ± 12 months | 26 (12–44) | 33.9% | 22 (11–43) | 221 | 3.6 (2.8–4.0) | 3.0 (2.0–3.8) | 4.0 (3.5–4.0) | 4.0 (3.0–4.0) |
| Oh et al. [33] | 2017 | South Korea | 0 (day of discharge) | 44.52 ± 13.23 | 31% | 14.94 ± 13.23 | 100 | 3.19 ± 0.90 | 2.72 ± 1.34 | 3.57 ± 0.71 | 3.28 ± 1.00 |
| Berg et al. [34] | 2017 | Germany | 11+ months | 49.9 ± 15.2 | 35.6% | 13.2 ± 11 | 141 | 3.53 ± 0.87 | 3.18 ± 0.98 | 3.83 ± 0.58 | 3.6 |
| Wasiak et al. [35] | 2017 | Australia | 12 months | M: 39.9 ± 17.6; F: 42.8 ± 13.6 | 75.4% | M: 18.5 (13–25); F: 14 (9–25) | 114 | 3.53 ± 0.11 | 3.10 ± 0.14 | 3.68 ± 0.09 | 3.61 ± 0.10 |
| Rothman et al. [36] | 2016 | USA | 4.25 ± 6.72 months | 41.32 ± 14.32 | 28.9% | 87% with <30% TBSA | 83 | 3.35 ± 0.78 | 3.1 ± 0.94 | 3.66 ± 0.55 | 3.48 ± 0.85 |
| Ahuja et al. [37] | 2016 | India | 10 months (8–12) | 28 (23.75–32.25) | 60% | 30 (19.38–40.63) | 60 | 2.22 | 3.92 ± 1.43 | 3.08 ± 1.29 | 2.29 |
| Hwang et al. [38] | 2016 | Taiwan | 18.6 ± 32.2 months | 42.1 ± 13.3 | 36.1% | 23.3 ± 25.4 | 108 | 3.85 (3.28–4) | 4 (3.25–4) | 4 (4–4) | 4 (3.33–4) |
| Murphy et al. [39] | 2015 | USA | 30–150 months | 17.9 ± 1.7 | 44% | 49.6 ± 12.5 | 50 | 3.4 ± 0.1 | 3.1 ± 0.1 | 3.7 ± 0.1 | 3.6 ± 0.1 |
| Mulay et al. [20] | 2015 | India | 6–12 months | 30.95 (20–55) | 60% | 39.75 (20–60) | 20 | 2.27 ± 1.38 | 1.61 ± 1.28 | 3.21 ± 1.24 | 2.63 ± 1.32 |
| Dowda & Li [40] | 2014 | Australia | 12 months | 43 (21–81) | 4% | 21 (10–68) | 13 | 2.94 ± 0.55 | 3.03 ± 0.81 | 4.71 ± 0.43 | 3.43 ± 0.59 |
| Xie et al. [41] | 2012 | China | 24–48 months | 42.6 ± 13.0 | 30% | 83.5 ± 9.7 | 20 | 3.0 ± 1.2 | 1.4 ± 1.1 | 3.6 ± 1.0 | 2.7 ± 2.5 |
| Roh et al. [42] | 2012 | South Korea | 2 ± 2 months | 38.4 ± 10.8 | 29.2% | 25.9 ± 15.9 | 113 | 2.61 ± 1.20 | 2.03 ± 1.33 | 3.29 ± 0.85 | 3.64 ± 0.68 |
| Ling-Juan et al. [19] | 2012 | China | 37.1 ± 35.4 months | 40.42 ± 13.16 | 22.6% | 40.05 ± 27.35 | 208 | 3.02 ± 1.09 | 2.11 ± 1.38 | 3.12 ± 1.15 | 2.65 ± 0.90 |
| Reeve et al. [43] | 2011 | New Zealand | 61 months | 43.2 ± 12.3 | 36% | >1/2 10–20% | 50 | 3.32 ± 1.01 | 2.65 ± 1.41 | 3.69 ± 0.72 | 3.34 ± 1.78 |
| Sgroi et al. [44] | 2005 | Sweden | 42 ± 14 months | 43.7 ± 17.2 | 26.2% | 16.7 ± 14.3 | 84 | 3.17 ± 0.92 | 2.64 ± 0.17 | 3.69 ± 0.64 | 3.40 ± 0.90 |
| Kildal et al. [14] | 2001 | Sweden | 111.6 ± 57.6 months | 46.1 ± 15.5 | 19.8% | 23.1 ± 16.2 | 248 | 3.36 ± 0.77 | 3.05 ± 1.00 | 3.67 ± 0.68 | 3.53 ± 0.77 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Puthumana, J.S.; Ross, E.S.; Keller, P.R.; Drogt, C.S.; Khoo, K.H.; Duraes, E.F.; Hultman, C.S.; Lerman, S.F. Cross-Cultural Review of Sexuality, Relationships, and Body Image after Burns: Analysis of the BSHS-B. Eur. Burn J. 2022, 3, 197-206. https://doi.org/10.3390/ebj3010017
Puthumana JS, Ross ES, Keller PR, Drogt CS, Khoo KH, Duraes EF, Hultman CS, Lerman SF. Cross-Cultural Review of Sexuality, Relationships, and Body Image after Burns: Analysis of the BSHS-B. European Burn Journal. 2022; 3(1):197-206. https://doi.org/10.3390/ebj3010017
Chicago/Turabian StylePuthumana, Joseph S., Emily S. Ross, Patrick R. Keller, Carolyn S. Drogt, Kimberly H. Khoo, Eliana F. Duraes, Charles S. Hultman, and Sheera F. Lerman. 2022. "Cross-Cultural Review of Sexuality, Relationships, and Body Image after Burns: Analysis of the BSHS-B" European Burn Journal 3, no. 1: 197-206. https://doi.org/10.3390/ebj3010017
APA StylePuthumana, J. S., Ross, E. S., Keller, P. R., Drogt, C. S., Khoo, K. H., Duraes, E. F., Hultman, C. S., & Lerman, S. F. (2022). Cross-Cultural Review of Sexuality, Relationships, and Body Image after Burns: Analysis of the BSHS-B. European Burn Journal, 3(1), 197-206. https://doi.org/10.3390/ebj3010017






