Consensus-Based Recommendations for Comprehensive Clinical Assessment in Prosthetic Care: A Delphi Study
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Participants
2.3. Focus Groups
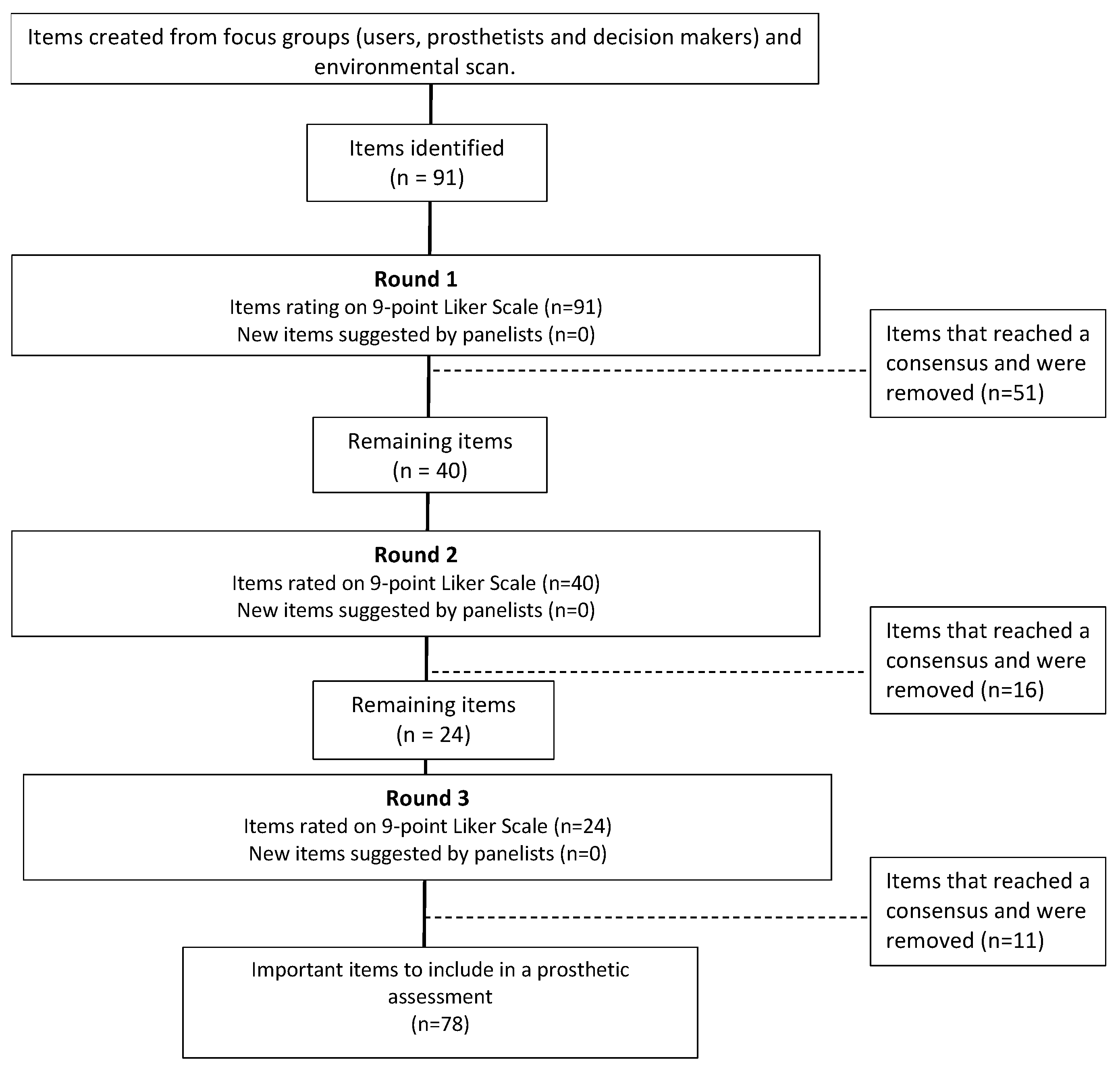
2.4. The Delphi Process
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ACCORD | Accurate Consensus Reporting Document. |
| LLA | Low limb amputation. |
| PROMS | Patient-reported outcome measures. |
Appendix A. Results Round 1
| Elements | Prosthetists and Decision Makers Mean Score (Median) | Prosthetic Users Mean Score (Median) | % Prosthetists and Decision Makers Who Voted ≥ 7 | % Prosthetic Users Who Voted ≥ 7 |
| General information of prosthetic users | ||||
| Name | 8.9 (9.0) | 7.47 (9.0) | 100 | 70.6 |
| Date of birth | 8.3 (9.0) | 7.18 (7.0) | 88.9 | 64.7 |
| Sex | 5.8 (6.0) | 4.8 (4.0) | 44.4 | 29.4 |
| Healthcare insurance number | 7.9 (9.0) | 6.82 (8.0) | 77.8 | 70.6 |
| Address | 7.9 (9.0) | 5.82 (6.0) | 77.8 | 47.1 |
| Phone number | 8.2 (9.0) | 7.2 (8.0) | 94.4 | 82.4 |
| E-mail address | 6.7 (7.0) | 7.3 (7.0) | 61.1 | 76.5 |
| Paying agent | 8.7 (9.0) | 7.2 (7.0) | 100 | 76.5 |
| Shoe size | 8.0 (9.0) | 7.3 (7.0) | 83.3 | 76.5 |
| Reason for consultation | 8.7 (9.0) | 7.8 (8.0) | 100 | 82.4 |
| Client’s goals | 7.8 (8.0) | 8.6 (9.0) | 88.9 | 100 |
| Client’s motivation | 7.7 (8.0) | 8.1 (9.0) | 77.8 | 88.8 |
| Medical and rehabilitation information | ||||
| Deterioration history of the amputated limb | 7.3 (7.0) | 8.5 (9.0) | 77.8 | 94.1 |
| Date of last amputation | 7.5 (7.0) | 8.3 (9.0) | 88.9 | 94.1 |
| Amputation hospital | 4.3 (4.0) | 6.1 (6.0) | 16.7 | 41.2 |
| Referring physician | 6.4 (7.0) | 7.2 (7.0) | 61.1 | 82.4 |
| Family doctor | 4.8 (4.5) | 6.7 (7.0) | 27.8 | 64.7 |
| Cause of amputation | 8.2 (9.0) | 8.4 (9.0) | 94.4 | 88.8 |
| Level of amputation | 8.4 (9.0) | 8.7 (9.0) | 100 | 94.1 |
| Amputation side | 8.2 (9.0) | 8.2 (9.0) | 88.9 | 88.8 |
| Smoking status | 5.8 (6.0) | 6.4 (7.0) | 33.3 | 64.7 |
| Alcohol use | 5.5 (6.0) | 6.2 (7.0) | 33.3 | 58.8 |
| Drug use (including cannabis) | 5.4 (5.0) | 6.0 (7.0) | 33.3 | 58.8 |
| Presence of intermittent claudication | 7.2 (7.0) | 7.8 (8.0) | 83.3 | 88.8 |
| Visual or hearing impairment | 7.1 (7.00) | 8.1 (8.0) | 72.2 | 94.1 |
| Patient weight without prosthesis | 7.7 (8.0) | 7.8 (8.0) | 94.4 | 88.8 |
| Patient height | 7.1 (7.0) | 7.3 (7.0) | 72.2 | 76.5 |
| Common comorbidities (e.g., vascular disease, diabetes, hypertension, etc.) | 7.8 (8.0) | 8.2 (9.0) | 88.9 | 94.1 |
| Allergies | 7.2 (7.0) | 7.4 (8.0) | 77.8 | 82.4 |
| Follow-up(s) with other health care professionals | 6.9 (7.0) | 7.7 (8.0) | 66.7 | 82.4 |
| Current medications | 6.9 (7.0) | 7.8 (9.0) | 61.1 | 70.6 |
| Place of rehabilitation | 5.5 (6.0) | 7.8 (8.0) | 33.3 | 82.4 |
| Date of rehabilitation admission | 5.8 (6.0) | 7.8 (9.0) | 44.4 | 82.4 |
| Date of rehabilitation discharge | 5.8 (6.0) | 7.5 (9.0) | 38.9 | 82.4 |
| Treating physiatrist | 7.2 (7.5) | 8.4 (9.0) | 66.7 | 82.4 |
| Environmental context | ||||
| Type of housing | 5.6 (6.0) | 7.9 (9.0) | 33.3 | 82.4 |
| Stairs in the home | 7.1 (7.0) | 8.2 (9.0) | 77.8 | 94.1 |
| Living alone or not | 6.8 (7.0) | 7.7 (8.0) | 66.7 | 88.8 |
| Presence of current support (social services, family and/or friends) | 7.0 (7.0) | 7.9 (8.0) | 77.8 | 88.8 |
| Availability of help from a relative for donning and removing the prosthesis | 7.4 (7.0) | 8.4 (9.0) | 83.3 | 100 |
| Prosthetic history | ||||
| Description of prosthetic components (socket, suspension, knee, foot, etc.) | 7.9 (8.0) | 7.7 (8.0) | 94.4 | 82.4 |
| Integrity of prosthetic components (to be replaced or not) | 7.6 (8.0) | 7.9 (8.0) | 83.3 | 82.4 |
| Hygiene of the sleeve and prosthesis | 7.4 (7.0) | 8.1 (9.0) | 72.2 | 88.8 |
| Prosthetic history, if applicable (what worked and what didn’t work with previous prostheses) | 8.0 (8.0) | 8.7 (9.0) | 94.4 | 94.1 |
| Problems (current and known recurring) with current prosthesis | 8.4 (9.0) | 8.9 (9.0) | 100 | 100 |
| Prosthesis use (h/day, number of days/week) | 7.6 (8.0) | 8.7 (9.0) | 83.3 | 94.1 |
| Reasons for not using prosthesis (if applicable) | 7.8 (7.5) | 8.7 (9.0) | 94.4 | 100 |
| Satisfaction and comfort with prosthesis | 7.9 (8.0) | 8.9 (9.0) | 100 | 100 |
| Pain | ||||
| Phantom pain (e.g., intensity, frequency, interference with activities, factors that increase or decrease pain) | 7.2 (8.0) | 8.4 (9.0) | 72.2 | 94.1 |
| Pain in residual limb (e.g., intensity, frequency, interference with activities, factors that increase or decrease pain) | 8.0 (8.0) | 8.7 (9.0) | 94.4 | 100 |
| Pain in contralateral limb (e.g., intensity, frequency, interference with activities, factors that increase or decrease pain) | 7.3 (7.0) | 8.5 (9.0) | 83.3 | 194.1 |
| Low back pain (e.g., intensity, frequency, interference with activities, factors that increase or decrease pain) | 6.7 (7.0) | 8.5 (9.0) | 66.7 | 100 |
| Other pain with description of intensity, frequency, interference with activities, factors that increase or decrease pain, etc. | 6.9 (7.0) | 8.4 (9.0) | 72.2 | 94.1 |
| Pain when walking without prosthesis (residual limb, contralateral limb) | 7.4 (8.0) | 8.5 (9.0) | 77.8 | 100 |
| Pain while walking with prosthesis (residual limb, contralateral limb) | 7.7 (7.5) | 8.5 (9.0) | 83.3 | 100 |
| Activities and participation (other than mobility) | ||||
| Number of falls in the past month | 7.6 (8.0) | 8.4 (9.0) | 83.3 | 100 |
| Autonomy to donn and doff prosthesis | 8.1 (8.0) | 8.7 (9.0) | 100 | 100 |
| Driving | 6.7 (7.0) | 8.1 (9.0) | 72.2 | 100 |
| Independence in activities of daily living | 7.8 (8.0) | 8.4 (9.0) | 77.8 | 94.1 |
| Use of technical mobility aids before amputation | 6.9 (7.5) | 8.2 (9.0) | 61.1 | 82.4 |
| Type(s) of technical mobility aid(s) used | 7.6 (8.0) | 8.6 (9.0) | 94.4 | 94.1 |
| Current main occupation | 7.8 (7.5) | 8.3 (7.0) | 94.4 | 70.6 |
| Physical activities and main leisure activities | 7.6 (7.0) | 7.7 (8.0) | 100 | 88.8 |
| Autonomy to manage finances, bills, etc. (cognitive skills) | 5.6 (6.0) | 6.4 (7.0) | 38.9 | 58.8 |
| Autonomy with activities of daily living (ADLs) (e.g., cooking, housework/laundry, shopping, transportation) | 7.1 (7.0) | 7.9 (9.0) | 77.8 | 82.4 |
| Physical examination and measures | ||||
| Skin integrity (wounds, scar tissue/skin grafts/skin problems on residual limb and non-amputee limb, scar mobility) | 8.3 (9.0) | 8.8 (9.0) | 100 | 100 |
| Assessment of color/temperature of residual limb and non-amputee limb | 7.4 (7.5) | 8.5 (9.0) | 72.2 | 94.1 |
| Presence and location of neuroma on residual limb | 7.8 (8.0) | 8.7 (9.0) | 100 | 100 |
| Presence and measurement of contractures (especially hip and knee flexors) | 8.5 (9.0) | 8.2 (9.0) | 100 | 88.8 |
| Assessment of sensitivity of residual limb and non-amputee limb (e.g., light touch, prick sensation test) | 7.0 (7.0) | 7.9 (8.0) | 66.7 | 88.8 |
| Lower limb muscle strength | 7.7 (7.5) | 7.9 (9.0) | 88.9 | 82.4 |
| Upper limb muscle strength | 6.8 (6.5) | 6.7 (7.0) | 50 | 58.8 |
| Lower limb joint amplitude | 8.0 (8.0) | 7.9 (9.0) | 94.4 | 82.4 |
| Joint amplitude of upper limbs | 6.4 (6.0) | 6.7 (7.0) | 38.9 | 58.8 |
| Anthropometric measurements: residual limb length, edema | 7.9 (8.0) | 7.0 (9.0) | 100 | 82.4 |
| Type and use of compression method (e.g., elastic bandage) | 7.3 (7.0) | 7.7 (8.0) | 66.7 | 70.6 |
| Level of autonomy for compression method | 7.4 (7.5) | 7.3 (8.0) | 66.7 | 70.6 |
| Mobility without prosthesis | ||||
| Standing balance (static and dynamic) | 7.4 (8.0) | 8.1 (9.0) | 77.8 | 94.1 |
| Transfer autonomy (e.g., sit-stand; wheelchair-bed) | 6.8 (7.0) | 8.1 (9.0) | 72.2 | 82.4 |
| Unipodal walking autonomy | 8.2 (9.0) | 7.8 (9.0) | 66.7 | 70.6 |
| Technical aids used | 7.1 (7.0) | 8.3 (9.0) | 88.9 | 88.8 |
| Maximum walking distance | 5.9 (6.0) | 7.5 (9.0) | 55.6 | 70.6 |
| Mobility with prosthesis | ||||
| Standing balance (static and dynamic) | 7.4 (8.0) | 8.5 (9.0) | 77.8 | 94.1 |
| Transfer autonomy (e.g., sit-stand; wheelchair-bed) | 6.8 (7.0) | 8.2 (9.0) | 61.1 | 88.8 |
| Prosthetic alignment (static and dynamic) | 8.2 (9.0) | 8.7 (9.0) | 94.4 | 100 |
| Description of gait pattern | 7.1 (7.0) | 8.5 (9.0) | 66.7 | 100 |
| Walking speed | 5.9 (6.0) | 7.5 (8.0) | 27.8 | 70.6 |
| Technical mobility aids used | 7.4 (8.0) | 8.2 (9.0) | 83.3 | 88.8 |
| Autonomy in locomotor activities (e.g., stairs, slopes, sidewalks, transferring to and from the floor, walking on uneven surfaces, etc.). | 7.8 (7.5) | 8.4 (9.0) | 100 | 94.1 |
| List of priority problems | 8.0 (8.0) | 8.4 (9.0) | 94.4 | 100 |
| Prosthetic treatment plan | 8.4 (8.5) | 8.3 (9.0) | 100 | 94.1 |
 : inclusion consensus. : inclusion consensus.  : no consensus. : no consensus.  : Exclusion consensus (No item obtained an exclusion consensus for round 1). : Exclusion consensus (No item obtained an exclusion consensus for round 1). | ||||
Appendix B. Results, Round 2
| Elements | Prosthetists and Decision Makers Mean Score (Median) | Prosthetic Users Mean Score (Median) | % Prosthetists and Decision Makers Who Voted ≥ 7 | % Prosthetic Users Who Voted ≥ 7 |
| General information of prosthetic users | ||||
| Name | 8.8 (9.0) | 7.6 (9.0) | 100.0 | 82.4 |
| Date of birth | 8.5 (9.0) | 7.4 (8.0) | 100.0 | 70.6 |
| Sex | 5.7 (6.0) | 6.7 (8.0) | 42.1 | 52.9 |
| Healthcare insurance number | 8.5 (9.0) | 7.2 (9.0) | 94.7 | 76.5 |
| Address | 8.2 (9.0) | 6.1 (7.0) | 89.5 | 52.9 |
| E-mail address | 6.2 (6.0) | 7.2 (7.0) | 36.8 | 76.5 |
| Medical and rehabilitation information | ||||
| Amputation hospital | 4.1 (4.0) | 6.5 (6.0) | 0.0 | 47.1 |
| Referring physician | 7.0 (7.0) | 7.7 (8.0) | 73.7 | 76.5 |
| Family doctor | 5.5 (6.0) | 5.9 (6.0) | 31.6 | 41.2 |
| Smoking status | 5.7 (6.0) | 6.8 (7.0) | 36.8 | 58.8 |
| Alcohol use | 5.6 (6.0) | 6.5 (7.0) | 31.6 | 58.8 |
| Drug use (including cannabis) | 5.3 (6.0) | 6.7 (7.0) | 21.1 | 58.8 |
| Visual or hearing impairment | 7.7 (8.0) | 8.3 (8.0) | 94.7 | 94.1 |
| Patient height | 7.1 (7.0) | 7.3 (7.0) | 72.2 | 76.5 |
| Follow-up(s) with other health care professionals | 6.7 (7.0) | 7.7 (8.0) | 57.9 | 76.5 |
| Current medications | 7.0 (7.0) | 7.7 (8.0) | 73.7 | 76.5 |
| Place of rehabilitation | 6.3 (7.0) | 7.5 (8.0) | 52.6 | 76.5 |
| Date of rehabilitation admission | 6.5 (7.0) | 7.2 (7.0) | 57.9 | 70.6 |
| Date of rehabilitation discharge | 6.0 (6.0) | 7.3 (7.0) | 52.6 | 76.5 |
| Treating physiatrist | 7.6 (8.0) | 8.0 (8.0) | 84.2 | 88.2 |
| Environmental context | ||||
| Type of housing | 6.9 (7.0) | 7.3 (8.0) | 68.4 | 76.5 |
| Living alone or not | 6.9 (7.0) | 7.9 (8.0) | 68.4 | 100.0 |
| Pain | ||||
| Phantom pain (e.g., intensity, frequency, interference with activities, factors that increase or decrease pain) | 7.9 (8.0) | 8.1 (8.0) | 94.7 | 100.0 |
| Low back pain (e.g., intensity, frequency, interference with activities, factors that increase or decrease pain) | 7.5 (8.0) | 8.2 (8.0) | 89.5 | 94.1 |
| Other pain with description of intensity, frequency, interference with activities, factors that increase or decrease pain, etc. | 8.0 (8.0) | 8.2 (8.0) | 94.7 | 100.0 |
| Activities and participation (other than mobility) | ||||
| Current main occupation | 7.8 (8.0) | 8.1 (8.0) | 100.0 | 94.1 |
| Driving | 7.1 (7.0) | 7.9 (8.0) | 63.2 | 100.0 |
| Autonomy to manage finances, bills, etc. (cognitive skills) | 6.4 (7.0) | 6.4 (6.0) | 52.6 | 47.1 |
| Use of technical mobility aids before amputation | 7.5 (7.0) | 8.0 (8.0) | 84.2 | 88.2 |
| Physical examination and measures | ||||
| Assessment of color/temperature of residual limb and non-amputee limb | 8.2 (8.0) | 8.4 (8.0) | 100.0 | 100.0 |
| Assessment of sensitivity of residual limb and non-amputee limb (e.g., light touch, prick sensation test) | 7.9 (8.0) | 8.1 (8.0) | 94.7 | 94.1 |
| Upper limb muscle strength | 7.4 (7.0) | 7.4 (7.0) | 84.2 | 64.7 |
| Joint amplitude of upper limbs | 6.7 (7.0) | 7.2 (7.0) | 57.9 | 64.7 |
| Type and use of compression method (e.g., elastic bandage) | 7.8 (8.0) | 7.8 (8.0) | 100.0 | 94.1 |
| Level of autonomy for compression method | 7.5 (8.0) | 7.7 (7.0) | 94.7 | 94.1 |
| Mobility without prosthesis | ||||
| Transfer autonomy (e.g., sit-stand; wheelchair-bed) | 7.4 (7.0) | 8.0 (8.0) | 84.2 | 88.2 |
| Unipodal walking autonomy | 7.3 (8.0) | 7.7 (8.0) | 78.9 | 88.2 |
| Maximum walking distance | 6.9 (7.0) | 8.0 (8.0) | 73.7 | 88.2 |
| Mobility with prosthesis | ||||
| Transfer autonomy (e.g., sit-stand; wheelchair-bed) | 7.1 (7.0) | 7.7 (8.0) | 73.7 | 88.2 |
| Description of gait pattern | 5.5 (6.0) | 7.4 (8.0) | 57.9 | 70.6 |
| Walking speed | 7.7 (8.0) | 8.3 (9.0) | 89.5 | 94.1 |
 : inclusion consensus. : inclusion consensus.  : no consensus. : no consensus.  : Exclusion consensus (No item obtained an exclusion consensus for round 2). : Exclusion consensus (No item obtained an exclusion consensus for round 2). | ||||
Appendix C. Results, Round 3
| Elements | Prosthetists and Decision Makers Mean Score (Median) | Prosthetic Users Mean Score (Median) | % Prosthetists and Decision Makers Who Voted ≥ 7 | % Prosthetic Users Who Voted ≥ 7 |
| General information of prosthetic users | ||||
| Date of birth | 8.3 (8.0) | 7.1 (8.0) | 100.0 | 82.4 |
| Sex | 4.5 (5.0) | 6.2 (7.0) | 26.7 | 52.9 |
| Address | 7.9 (8.0) | 6.6 (7.0) | 87.1 | 52.9 |
| E-mail address | 5.7 (6.0) | 6.7 (7.0) | 26.7 | 76.5 |
| Medical and rehabilitation information | ||||
| Amputation hospital | 4.0 (4.0) | 5.5 (5.0) | 13.3 | 23.5 |
| Referring physician | 7.5 (7.0) | 7.2 (7.0) | 86.7 | 82.4 |
| Family doctor | 5.2 (5.0) | 6.6 (6.0) | 26.7 | 47.1 |
| Smoking status | 5.2 (5.0) | 6.8 (7.0) | 33.3 | 70.6 |
| Alcohol use | 4.7 (5.0) | 6.5 (6.0) | 13.3 | 41.2 |
| Drug use (including cannabis) | 5.0 (5.0) | 6.6 (6.0) | 20.0 | 47.1 |
| Patient height | 7.1 (7.0) | 7.3 (7.0) | 72.2 | 76.5 |
| Follow-up(s) with other health care professionals | 7.3 (7.0) | 7.5 (7.0) | 86.7 | 88.2 |
| Current medications | 6.9 (7.0) | 7.8 (7.0) | 80.0 | 100.0 |
| Place of rehabilitation | 5.3 (6.0) | 7.3 (7.0) | 26.7 | 82.4 |
| Date of rehabilitation admission | 5.5 (6.0) | 7.0 (7.0) | 33.3 | 64.7 |
| Date of rehabilitation discharge | 5.4 (6.0) | 6.6 (7.0) | 33.3 | 52.9 |
| Environmental context | ||||
| Type of housing | 7.5 (8.0) | 7.3 (7.0) | 87.1 | 88.2 |
| Living alone or not | 7.7 (8.0) | 7.8 (7.0) | 100.0 | 94.1 |
| Driving | 6.9 (7.0) | 7.9 (8.0) | 73.3 | 100.0 |
| Activities and participation (other than mobility) | ||||
| Autonomy to manage finances, bills, etc. (cognitive skills) | 6.2 (6.0) | 6.6 (7.0) | 40.0 | 64.7 |
| Physical examination and measures | ||||
| Upper limb muscle strength | 7.3 (7.0) | 8.1 (8.0) | 87.1 | 94.1 |
| Joint amplitude of upper limbs | 7.1 (7.0) | 7.7 (8.0) | 66.7 | 88.2 |
| Mobility without prosthesis | ||||
| Maximum walking distance | 6.6 (7.0) | 7.6 (8.0) | 66.7 | 88.2 |
| Mobility with prosthesis | ||||
| Transfer autonomy (e.g., sit-stand; wheelchair-bed) | 7.6 (7.0) | 7.9 (8.0) | 100.0 | 100.0 |
| Description of gait pattern | 4.9 (5.0) | 6.6 (7.0) | 20.0 | 64.7 |
 : inclusion consensus. : inclusion consensus.  : Exclusion consensus. : Exclusion consensus. | ||||
References
- Rommers, G.M.; Vos, L.D.W.; Groothoff, J.W.; Eisma, W.H. Clinical rehabilitation of the amputee: A retrospective study. Prosthet. Orthot. Int. 1996, 20, 72–78. [Google Scholar] [CrossRef] [PubMed]
- Raichle, K.A.; Hanley Ma Fau-Molton, I.; Molton I Fau-Kadel, N.J.; Kadel Nj Fau-Campbell, K.; Campbell K Fau-Phelps, E.; Phelps E Fau-Ehde, D.; Ehde D Fau-Smith, D.G.; Smith, D.G. Prosthesis use in persons with lower- and upper-limb amputation. J. Rehabil. Res. Dev. 2008, 45, 7. [Google Scholar] [CrossRef] [PubMed]
- Pezzin, L.E.; Dillingham, T.R.; MacKenzie, E.J.; Ephraim, P.; Rossbach, P. Use and satisfaction with prosthetic limb devices and related services. Arch. Phys. Med. Rehabil. 2004, 85, 723–729. [Google Scholar] [CrossRef] [PubMed]
- Resnik, L.; Borgia, M. Reliability of Outcome Measures for People With Lower-Limb Amputations: Distinguishing True Change From Statistical Error. Phys. Ther. 2011, 91, 555–565. [Google Scholar] [CrossRef] [PubMed]
- Walton, M.K.; Powers, J.H., III; Hobart, J.; Patrick, D.; Marquis, P.; Vamvakas, S.; Isaac, M.; Molsen, E.; Cano, S.; Burke, L.B. Clinical Outcome Assessments: Conceptual Foundation-Report of the ISPOR Clinical Outcomes Assessment—Emerging Good Practices for Outcomes Research Task Force. Value Health 2015, 18, 741–752. [Google Scholar] [CrossRef] [PubMed]
- Schaffalitzky, E.; Gallagher, P.; MacLachlan, M.; Wegener, S.T. Developing consensus on important factors associated with lower limb prosthetic prescription and use. Disabil. Rehabil. 2012, 34, 2085–2094. [Google Scholar] [CrossRef] [PubMed]
- Hall, N.; Parker, D.; Williams, A. An exploratory qualitative study of health professional perspectives on clinical outcomes in UK orthotic practice. J. Foot Ankle Res. 2020, 13, 49. [Google Scholar] [CrossRef] [PubMed]
- Robinson, C.; Fatone, S. You’ve heard about outcome measures, so how do you use them? Integrating clinically relevant outcome measures in orthotic management of stroke. Prosthet. Orthot. Int. 2012, 37, 30–42. [Google Scholar] [CrossRef] [PubMed]
- Parker, K.; Kirby, R.L.; Adderson, J.; Thompson, K. Ambulation of People With Lower-Limb Amputations: Relationship Between Capacity and Performance Measures. Arch. Phys. Med. Rehabil. 2010, 91, 543–549. [Google Scholar] [CrossRef] [PubMed]
- Gaunaurd, I.; Spaulding, S.E.; Amtmann, D.; Salem, R.; Gailey, R.; Morgan, S.J.; Hafner, B.J. Use of and confidence in administering outcome measures among clinical prosthetists: Results from a national survey and mixed-methods training program. Prosthet. Orthot. Int. 2014, 39, 314–321. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Morgan, S.J.; Rowe, K.; Fitting, C.C.; Gaunaurd, I.A.; Kristal, A.; Balkman, G.S.; Salem, R.; Bamer, A.M.; Hafner, B.J. Use of Standardized Outcome Measures for People With Lower Limb Amputation: A Survey of Prosthetic Practitioners in the United States. Arch. Phys. Med. Rehabil. 2022, 103, 1786–1797. [Google Scholar] [CrossRef] [PubMed]
- Ostler, C.; Scott, H.; Sedki, I.; Kheng, S.; Donovan-Hall, M.; Dickinson, A.; Metcalf, C. From outcome measurement to improving health outcomes following lower limb amputation—A Narrative review exploring outcome measurement from a clinical practice perspective. Prosthet. Orthot. Int. 2021, 46, e341–e350. [Google Scholar] [CrossRef] [PubMed]
- Young, J.; Rowley, L.; Lalor, S. Use of Outcome Measures Among Prosthetists and Orthotists in the United Kingdom. J. Prosthet. Orthot. 2018, 30, 152–157. [Google Scholar] [CrossRef]
- Spaulding, S.; Yamane, A.; McDonald, C.; Spaulding, S. A conceptual framework for orthotic and prosthetic education. Prosthet. Orthot. Int. 2019, 43, 369–381. [Google Scholar] [CrossRef]
- Field, J.; Holmes, M.M.; Newell, D. PROMs data: Can it be used to make decisions for individual patients? A narrative review. Patient Relat. Outcome Meas. 2019, 10, 233–241. [Google Scholar] [CrossRef] [PubMed]
- Calvert, M.; Kyte, D.; Price, G.; Valderas, J.M.; Hjollund, N.H. Maximising the impact of patient reported outcome assessment for patients and society. BMJ 2019, 364, k5267. [Google Scholar] [CrossRef] [PubMed]
- Innovation Canada. Innovation Canada—Technology Readiness Levels; Innovation, Science and Economic Development Canada: Ottawa, ON, Canada, 2018; Available online: https://ised-isde.canada.ca/site/innovation-canada/en/technology-readiness-levels (accessed on 10 March 2025).
- Gattrell, W.; Logullo, P.; van Zuuren, E.; Price, A.; Hughes, E.; Blazey, P.; Winchester, C.C.; Tovey, D.; Goldman, K.; Hungin, A.P.; et al. ACCORD (ACcurate COnsensus Reporting Document): A reporting guideline for consensus methods in biomedicine developed via a modified Delphi. PLoS Med. 2024, 21, e1004326. [Google Scholar] [CrossRef] [PubMed]
- Barrett, D.; Heale, R. What are Delphi studies? Evid. Based Nurs. 2020, 23, 68. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, H.-F.; Shannon, S.E. Three Approaches to Qualitative Content Analysis. Qual. Health Res. 2005, 15, 1277–1288. [Google Scholar] [CrossRef] [PubMed]
- Nasa, P.; Jain, R.; Juneja, D. Delphi methodology in healthcare research: How to decide its appropriateness. World J. Methodol. 2021, 11, 116–129. [Google Scholar] [CrossRef] [PubMed]
- Boulkedid, R.; Abdoul, H.; Loustau, M.; Sibony, O.; Alberti, C. Using and Reporting the Delphi Method for Selecting Healthcare Quality Indicators: A Systematic Review. PLoS ONE 2011, 6, e20476. [Google Scholar] [CrossRef] [PubMed]
- Hasson, F.; Keeney, S.; McKenna, H. Research guidelines for the Delphi survey technique. J. Adv. Nurs. 2000, 32, 1008–1015. [Google Scholar] [CrossRef] [PubMed]
- Kahle, J.T.; Highsmith, M.J.; Schaepper, H.; Johannesson, A.; Orendurff, M.S.; Kaufman, K. Redicting walking ability following lower limb amputation: An updated systematic literature review. Technol. Innov. 2016, 18, 125–137. [Google Scholar] [CrossRef] [PubMed]
- Shunmuga Sundaram, C.; Campbell, R.; Ju, A.; King, M.T.; Rutherford, C. Patient and healthcare provider perceptions on using patient-reported experience measures (PREMs) in routine clinical care: A systematic review of qualitative studies. J. Patient-Rep. Outcomes 2022, 6, 122. [Google Scholar] [CrossRef] [PubMed]
- Foster, A.; Croot, L.; Brazier, J.; Harris, J.; O’Cathain, A. The facilitators and barriers to implementing patient reported outcome measures in organisations delivering health related services: A systematic review of reviews. J. Patient-Rep. Outcomes 2018, 2, 46. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Prosthetists and Decision Makers n = 18 | Prosthetic Users n = 17 |
|---|---|---|
| Age, mean (SD) | 44 (7) | 60 (10) |
| Gender, % | ||
| Men | 2 (11) | 9 (53) |
| Women | 16 (89) | 8 (47) |
| Years of clinical experience, mean (SD) | 21 (9) | - |
| Amputation, % | ||
| Unilateral | - | 16 (94) |
| Bilateral | - | 1 (6) |
| Level of amputation | ||
| Transfemoral | - | 5 (29) |
| Transtibial | - | 11 (65) |
| Other | - | 1 (6) |
| Time since amputation (years), mean (SD) | 22 (19) | |
| Cause of amputation, n (%) | ||
| Infection | - | 1 (6) |
| Dysvascular | - | 2 (12) |
| Trauma | - | 11 (64) |
| Cancer | - | 1 (6) |
| Other | - | 2 (12) |
| Highest certificate, diploma or degree obtained, n (%) | ||
| Highschool or equivalent | 0 (0) | 5 (29) |
| Professional degree or college | 15 (83) | 5 (29) |
| Bachelor | 2 (11) | 4 (24) |
| Master or doctorate | 1 (6) | 3 (18) |
| Elements | |
|---|---|
| 1. General information of prosthetic users | Not included |
| Name | Sex |
| Date of birth | Adress |
| Healthcare insurance number | Email address |
| Phone number | |
| Paying agent | |
| Shoe size | |
| Reason of consultation | |
| Client’s goals | |
| Client’s motivation | |
| 2. Medical and rehabilitation information | Not included |
| Deterioration history of the amputated limb | Amputation hospital |
| Date of last amputation | Referring physician |
| Referring physician | Smoking status |
| Cause of amputation | Alcohol use |
| Level of amputation | Drug use (including cannabis) |
| Amputation side | Date of rehabilitation admission |
| Presence of intermittent claudication | Date of rehabilitation discharge |
| Visual or auditory impairment | |
| Patient weight without prosthesis | |
| Patient height | |
| Comorbidities (e.g., vascular, diabetes, hypertension, etc.) | |
| Allergies | |
| Follow-up(s) with other healthcare professionals | |
| Current medications | |
| Place of rehabilitation | |
| Treating physiatrist | |
| 3. Environmental context | |
| Type of housing | |
| Stairs in the home | |
| Living alone or not | |
| Presence of current support (social services, family and/or friends) | |
| Availability of help from a relative for donning and removing the prosthesis | |
| 4. Current prosthesis and prosthetic history | |
| Description of prosthetic components (socket, suspension, knee, foot, etc.) | |
| Integrity of prosthetic components (to be replaced or not) | |
| Hygiene of the sleeve and prosthesis | |
| Prosthetic history, if applicable (what worked and what didn’t with previous prostheses) | |
| Problems (current and known recurring) with current prosthesis | |
| Prosthesis use (h/day, no. of days/week) | |
| Reasons for not using the prosthesis (if applicable) | |
| Satisfaction and comfort with the prosthesis | |
| 5. Pain | |
| Phantom pain (e.g., intensity, frequency, interference with activities, factors that increase or decrease pain) | |
| Residual limb pain (e.g., intensity, frequency, interference with activities, factors that increase or decrease pain) | |
| Pain in contralateral limb (e.g., intensity, frequency, interference with activities, factors increasing or decreasing pain) | |
| Low back pain (e.g., intensity, frequency, interference with activities, factors that increase or decrease pain) | |
| Other pain with description of intensity, frequency, interference with activities, factors increasing or decreasing pain, etc. | |
| Pain when walking with or without prosthesis (residual limb, contralateral limb) | |
| 6. Activities and participation (other than mobility) | Not included |
| Number of falls in the last month | Autonomy to manage finances, bills, etc. |
| Driving | |
| Independence in activities of daily living | |
| Use of technical mobility aids before amputation | |
| Type(s) of technical mobility aid(s) used | |
| Current main occupation | |
| Physical activities and main leisure activities | |
| Autonomy to don and doff the prosthesis | |
| Autonomy in activities of daily living (ADLs) (e.g., cooking, housework/laundry, shopping, transportation) | |
| 7. Physical examination and measures | |
| Skin integrity (wounds, scar tissue/skin grafts/skin problems on residual limb and non-amputee limb, scar mobility) | |
| Assessment of color/temperature of residual limb and non-amputee limb | |
| Presence and location of neuroma on residual limb | |
| Presence and measurement of contractures (especially hip and knee flexors) | |
| Assessment of sensitivity of residual limb and non-amputee limb (e.g., light touch, prick sensation test) | |
| Lower limb muscle strength | |
| Upper limb muscle strength | |
| Lower limb joint amplitude | |
| Joint amplitude of upper limbs | |
| Anthropometric measurements: residual limb length, edema | |
| Type and use of compression method (e.g., elastic bandage) | |
| Level of autonomy for compression method | |
| 7.1 Mobility without prosthesis | Not included |
| Standing balance (static and dynamic) | Maximum walking distance |
| Transfer autonomy (e.g., sit-stand; wheelchair-bed) | |
| Unipodal walking autonomy | |
| Technical mobility aids used | |
| 7.2 Mobility with prosthesis | Not included |
| Standing balance (static and dynamic) | Description of gait pattern |
| Transfer autonomy (e.g., sit-stand; wheelchair-bed) | |
| Prosthesis alignment (static and dynamic) | |
| Walking speed | |
| Technical mobility aids used | |
| Autonomy in locomotor activities (e.g., stairs, slopes, sidewalks, transferring to and from the ground, walking on uneven ground, etc.). | |
| 8. List of priority problems | |
| 9. Prosthetic treatment plan |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dupuis, F.; Pichette, M.; Swaine, B.; Auger, C.; Zidarov, D. Consensus-Based Recommendations for Comprehensive Clinical Assessment in Prosthetic Care: A Delphi Study. Prosthesis 2025, 7, 92. https://doi.org/10.3390/prosthesis7040092
Dupuis F, Pichette M, Swaine B, Auger C, Zidarov D. Consensus-Based Recommendations for Comprehensive Clinical Assessment in Prosthetic Care: A Delphi Study. Prosthesis. 2025; 7(4):92. https://doi.org/10.3390/prosthesis7040092
Chicago/Turabian StyleDupuis, Frédérique, Marion Pichette, Bonnie Swaine, Claudine Auger, and Diana Zidarov. 2025. "Consensus-Based Recommendations for Comprehensive Clinical Assessment in Prosthetic Care: A Delphi Study" Prosthesis 7, no. 4: 92. https://doi.org/10.3390/prosthesis7040092
APA StyleDupuis, F., Pichette, M., Swaine, B., Auger, C., & Zidarov, D. (2025). Consensus-Based Recommendations for Comprehensive Clinical Assessment in Prosthetic Care: A Delphi Study. Prosthesis, 7(4), 92. https://doi.org/10.3390/prosthesis7040092






